Abstract
We report the case of a 36 year-old man with relapsing undifferentiated nasopharyngeal carcinoma treated with a re-irradiation Cyberknife, who subsequently developed tension pneumocephalus due to a cerebrospinal fluid leakage located at the clivus. The fistula was caused by osteonecrosis of the skull base secondary to the tumor invasion and to the sequelae of the radiotherapy. An endoscopic endonasal technique was used in order to repair the defect, with a peduncolated nasoseptal flap harvested to perform the skull base reconstruction. In this paper, we discuss the importance of identifying this possible complication related to radiotherapy in the management of neoplasm along the skull base; moreover, the role of endoscopy in the diagnosis and treatment of skull base fistulas is also described and commented.
Keywords: Tension pneumocephalus (TP), Nasopharyngeal carcinoma (NPC), Skull-base fistula, Endoscopic endonasal approach
1. Introduction
Nasopharyngeal carcinoma (NPC) is an uncommon malignant tumor, often locally advanced at diagnosis. In these cases, especially in the presence of skull-base metastasis, the standard treatment consists of high doses of conformal radiotherapy with chemiotherapy.1 Pneumocephalus is defined as the presence of gas within any of intracranial compartments, mainly based on a valve mechanism. Tension pneumocephalus (TP) is a rare and important neurosurgical emergency which is known to occur after trauma, nitrous oxide anesthesia and craniotomy. It is rarely observed with tumor and can be correlated with skull base defects due to tumor invasion, tumor change after chemotherapy or osteoradionecrosis of the skull base.2
We report the case of a 36 year-old patient diagnosed with relapsing undifferentiated NPC, treated with Cyberknife, who subsequently developed TP due to a clival fistula. The fistula was caused by osteonecrosis of the skull base and was repaired with an endoscopic endonasal technique, using a peduncolated nasoseptal flap.
2. Case report
In December 2010, due to the development of a laterocervical adenopathy, a 36 years-old man was diagnosed with an undifferentiated NPC (cT3N2bM0). In January 2011, the patient underwent a left-side modified radical neck dissection (levels I–V) and elective chemo-radiotherapy consisting in Cisplatin + RT (66 Gy) followed by Cisplatin/5-FU. Due to the relapse of the disease on the clivus and sphenoidal bone, in June 2013 a second line stereotactic radiotherapy (Cyberknife) was performed at a dose of 27 Gy in 3 fractions (isodose 66%).
In July 2014, Patient was admitted to the E.D. of our hospital because of general disorientation, progressive tendency to drowsiness, cephalea, fever and aqueous rhinorrhea. At the time of evaluation, physical and neurological examination revealed disorientation, tendency to drowsiness, no cranial nerve deficits and no other significative findings. Nasal endoscopy revealed the presence of necrotic bone over the clival area, in the paramedian portion of the nasopharynx, with an active cerebrospinal fluid rhinorrhea. A Computed Tomography (CT) scan revealed the presence of massive tension pneumocephalus with erosion of infero-posterior parts of sphenoidal sinus and possible radionecrosis of the clivus (Fig. 1, Fig. 2). In emergency, after somministrating antibiotic therapy consisting of IV Linezolid (at a dose of 600 mg two times a day) and Meropenem (at a dose of 1 g three times a day), which was also maintained in the post-operative period, the patient underwent endoscopic endonasal repair of the clival fistula with a peduncolated nasoseptal (Hadad) flap.3 During the operation, several mucosal biopsies were made in the sphenoidal sinus, clivus and nasopharynx; the pathological examination revealed radionecrosis with signs of infiltration by infiltrating undifferentiated non-keratinising squamocellular carcinoma (Fig. 3). Because of the persistence of aqueous rhinorrhea, four days after the first intervention, the patient underwent a new endoscopic endonasal repair of the fistula (Fig. 4) with a controlateral nasoseptal flap. The patient was then transferred to the intensive care unit (ICU) where he underwent a percutaneous tracheostomy for the assisted ventilation.
Fig. 1.
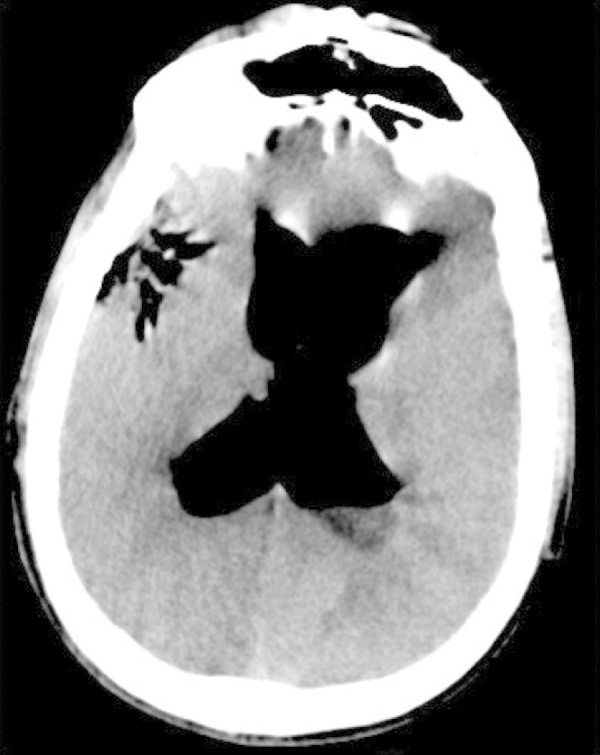
Preoperative axial head CT scan showing the pneumocephalus.
Fig. 2.
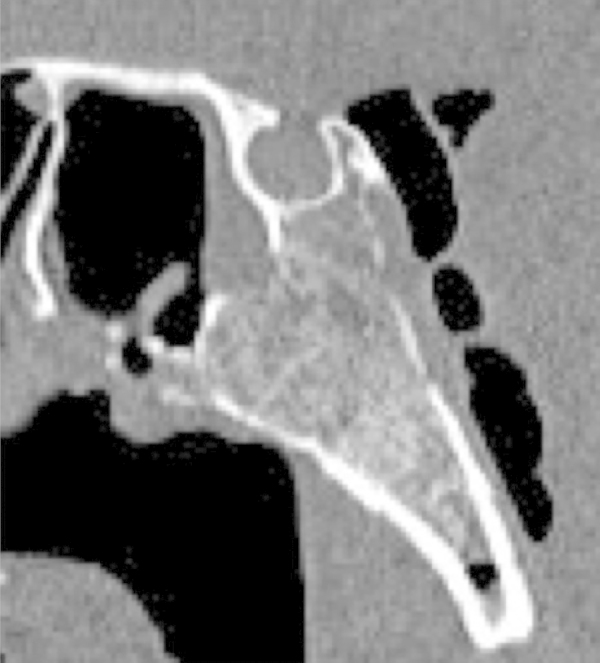
Preoperative sagittal head CT scan showing the necrotic bone of the clivus.
Fig. 3.
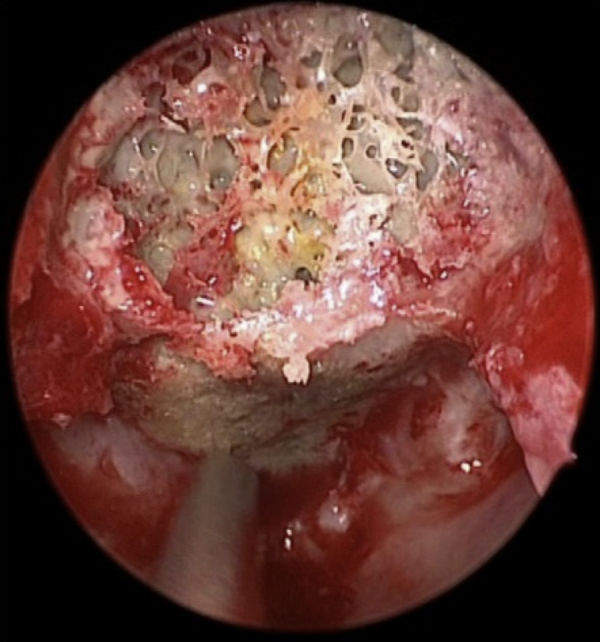
Intraoperative view of the necrotic bone of the clivus.
Fig. 4.
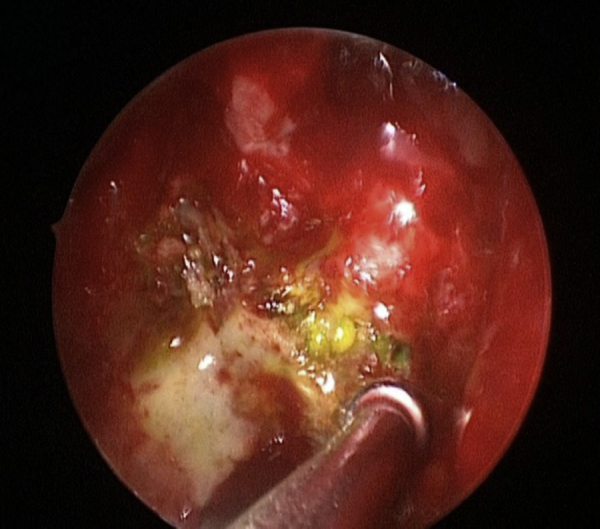
Intraoperative view of the bone defect which comes out of the fluorescein.
At two weeks from the first intervention, as a result of new episodes of rinoliquorrea and the persistence of tension pneumocephalus at control CT scans, the patient underwent a new endoscopic endonasal intervention, with the identification of a small dehisce at the level of the left nasal sept flap, which was repaired with some fibrin glue. After few days the patient returned to our unit and because of the new onset of fever and skin rash, he underwent blood and urine colture, bronchoalveolar lavage and dosage of inflammatory markers. A dermatological evaluation revealed a skin lichenoid eruption, probably related to drug and antibiotic assumption and the coltures of the airways resulted positive for colonization by Pseudomonas aeruginosa.
Further endoscopic endonasal controls showed no signs of fistula and a good healing process of the nasal flaps; patient no longer complained of rhinoliquorrea. Control CT and MRI cerebral scans showed a progressive resorption of the pneumocephalus in the absence of any signs of infection (Fig. 5). The tracheostomy tube was then removed and the patient was referred to rehabilitation, waiting a new oncologic multidisciplinary evaluation to define next treatments.
Fig. 5.
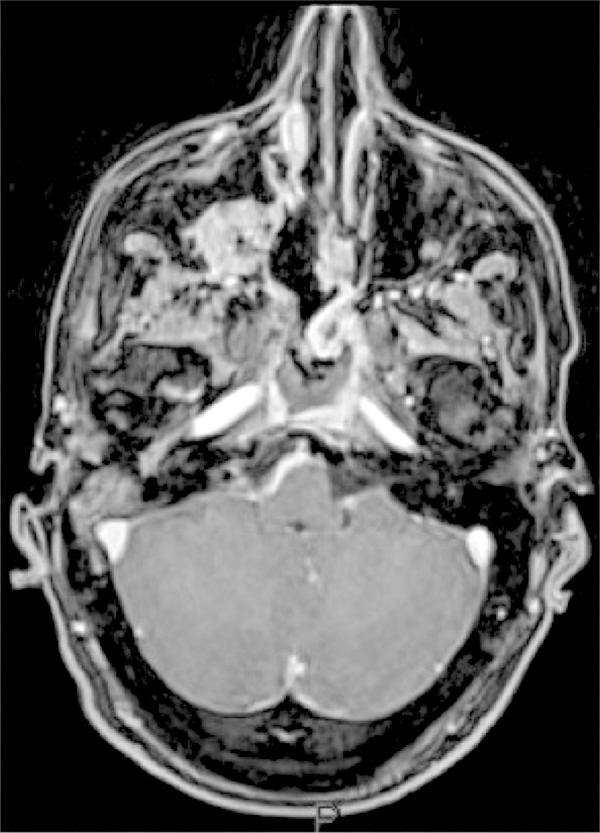
Postoperative T1 with gadolinium axial head MR showing the flap rotated on clivus.
3. Discussion
Pneumocephalus was first described by Chiari in 1884 at autopsy in patient who died of ethmoiditis.4 Since its early description, numerous models have been proposed to explain the mechanism of pneumocephalus formation, as presented in Davson's elastic model of the cerebrospinal fluid compartment.5, 6 According to its first radiological description, the most common cause of pneumocephalus was trauma, as considered in a series of 295 cases in which head injury and cranial surgery were considered to account for 74.5% and tumors, especially sinus osteomas and epidermoid and pituitary tumors, for 23%.7, 8, 9, 10, 11 Pneumocephalus is asymptomatic in almost all the cases and the postcraniotomy ones tend to solve spontaneously, with the air being reabsorbed. TP represents the only emergency in order to reduce intracranial pressure and to repair any cerebrospinal fluid leakage.12 Pneumocephalus has been rarely described in association with nasopharyngeal carcinoma, especially in association with radionecrosis and infiltration of the clivus after gamma-knife treatment.7
Nasopharyngeal carcinoma is highly endemic in certain regions including the People's Republic of China and Southeast Asia. Its etiology is unique and multifactorial, involving genetic background, epigenetic and environment factors, including Epstein–Barr virus (EBV) infection. EBV reactivation is supposed to be triggered by (co) carcinogenic agents, such as food, tobacco, smoke, alcohol consumption, occupational dust, inhalant. Standard treatment is based on radiotherapy with or without chemotherapy for early stage, concurrent chemoradiotherapy in locally advanced tumors, and palliative systemic chemotherapy in metastatic disease. However, recurrences and disease progression in a certain proportion of cases have been described, indicating that this standard care has some limitations.13 The grade of severity of complications after radiotherapy for NPC depends on the number of cycles, with only minor complications after one single course (xerostomia, trimus, fibrosis) to severe complications (myelitis, paralysis of nerves, osteoradionecrosis, temporal lobe injury and severe trimus) in patients treated with second salvage radiation.14 Radiation osteonecrosis is usually localized in the mandible and can be considered one of the most important complications.15 Esther Jimenez-Jimenez et al. recently reviewed the literature, identifying 5 cases of TP related to NPC and various localization of osteoradionecrosis of the skull base. In the presented cases, TP usually appeared between 2 and 4 years after the first radiotherapy course.12
In our case, the patient was diagnosed of a undifferentiated nasopharyngeal carcinoma (cT3N2bM0). The patient underwent in January 2011 a left-side modified radical neck dissection and elective radio-chemotherapy, with a total dose of 66 Gy. Due to the relapse of the disease on the clivus and sphenoidal bone, in June 2013 a second line stereotactic radiotherapy was performed at a dose of 27 Gy over the clivus and the sphenoid bone. He presented rhinoliquorrea 42 months after the first radiotherapic treatment, and 13 months after the Cyberknife re-irradiation. We think that this condition was secondary to both osteoradionecrosis of the clivus and of the infero-posterior parts of sphenoidal sinus and tumoral invasion of the clivus, as confirmed by the pathological examination.
It is not yet clear which predisposing factors can increase the risk to develop osteoradionecrosis and why some patients develop it and others do not, nor why there is a predisposition for certain areas under the same radiation exposition. Previously proposed explanations of the causes of this condition focused on hypoxia and vascular derangement, while most recent theories involve a fibroatrophic mechanism, with new possible medications that target this process.16 The vascular damage seems to be related to endothelial cell reaction to radiation therapy, which range from apoptosis to permanent phenotypic changes. These vascular dysfunctions help to generate the initial prefibrotic phase. A second fact is related to fibroblast stromal change which occurs as a result of reactive oxygen species’ deregulation of fibroblast proliferation and metabolism, suggesting the use of antioxidant or antifibrosis drugs for the treatment of osteoradionecrosis.17
Although TP and skull-base radionecrosis related to NPC is a rare entity, it can be very dangerous because of the risk of infection, cerebrospinal fluid leakage and rapid neurological worsening.2 A key point in order to get a better outcome is to support the patient during the critical period of illness, to perform an initially empirical antimicrobial therapy and to localize and repair the skull-base fistula to arrest the TP mechanism. Endoscopic endonasal approach, as in our case, can be considered a good and safe procedure to repair the cerebrospinal fluid leakage, and the nasoseptal (Hadad) flap is an effective option in order to perform an effective skull base repair.3
4. Conclusions
Nasopharyngeal carcinoma (NPC) is a relatively rare entity in United States and Europe, whose treatment is mainly based upon radiotherapy in primary or salvage treatment. Different complications has been described in association with radiotherapy, especially with high-dose treatment, necessary in advanced stages.
Tension pneumocephalus (TP) is a rare and serious complication related to radiotherapy in the treatment of NPC, which has to be considered especially when primary tumor involve the skull base and there is the necessity of treatment with radiosurgery such as gamma-knife technique.
Early identification and diagnosis of TP is mandatory to give the patient the best treatment and the repair of the skull base fistula can be successfully managed with the endoscopic endonasal approach and the use of the well-known peduncolated nasoseptal flap technique.
Conflict of interest
None declared.
Financial disclosure
None declared.
References
- 1.Al-Sarraf M., LeBlanc M., Giri P.G. Chemoradiotherapy versus radiotherapy in patients with advanced nasopharyngeal cancer: phase III randomized Intergroup study 0099. J Clin Oncol. 1998;16:1310–1317. doi: 10.1200/JCO.1998.16.4.1310. [DOI] [PubMed] [Google Scholar]
- 2.Wu C.T., Lee S.T. Delayed spontaneous tension pneumocephalus caused by radionecrosis of the skull base. Br J Neurosurg. 1999;13:214–216. doi: 10.1080/02688699944032. [DOI] [PubMed] [Google Scholar]
- 3.Hadad G., Bassagasteguy L., Carrau R.L. A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope. 2006;116:1882–1886. doi: 10.1097/01.mlg.0000234933.37779.e4. [DOI] [PubMed] [Google Scholar]
- 4.Chiari H. Uber einen Fall von Luftansammlung in den Ventrikeln des menschlichen Gehirns. Ztschr f Heilk. 1884;5:383–390. [Google Scholar]
- 5.Davson H. Little Brown and Company; Boston: 1967. Physiology of the cerebrospinal fluid; pp. 337–432. [Google Scholar]
- 6.Walker F.O., Vern B.A. The mechanism of pneumocephalus formation in patients with CSF fistulas. J Neurol Neurosurg Psychiatry. 1986;49(February (2)):203–205. doi: 10.1136/jnnp.49.2.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Markham J.W. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir (Wien) 1967;16(1):1–78. doi: 10.1007/BF01401900. [DOI] [PubMed] [Google Scholar]
- 8.Clark J.B., Six E.G. Epidermoid tumor presenting as a tension pneumocephalus: case report. J Neurosurg. 1984;60:1312–1314. doi: 10.3171/jns.1984.60.6.1312. [DOI] [PubMed] [Google Scholar]
- 9.Isler R.J., Weber A.L. Pneumocephalus from paranasal sinus carcinoma. Ann Otol Rhinol Laryngol. 1978;87(January–February (1 (Pt 1))):142–143. doi: 10.1177/000348947808700123. [DOI] [PubMed] [Google Scholar]
- 10.Kinsley S., Dougherty J. Tension pneumocephalus related to an epidermoid tumor of ethmoid sinus origin. Ann Emerg Med. 1993;22(February (2)):259–261. doi: 10.1016/s0196-0644(05)80217-3. [DOI] [PubMed] [Google Scholar]
- 11.Wilson E.S., Jr., Sheft D.J. Epidermoid tumor of the skull with intracranial pneumatocele: case report. J Neurosurg. 1968;28:600–602. doi: 10.3171/jns.1968.28.6.0600. [DOI] [PubMed] [Google Scholar]
- 12.Jimenez-Jimenez E., Marti S.S., Villa M.V. Tension pneumocephalus related to radiotherapy for nasopharyngeal carcinoma. Case Rep Oncol Med. 2014:327380. doi: 10.1155/2014/327380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hutajulu S.H., Kurnianda J., Tan I.B., Middeldorp J.M. Therapeutic implications of Epstein-Barr virus infection for the treatment of nasopharyngeal carcinoma. Ther Clin Risk Manag. 2014;10(September):721–736. doi: 10.2147/TCRM.S47434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdel Razek A.A., Kamal E. Nasopharyngeal carcinoma: correlation of apparent diffusion coefficient value with prognostic parameters. Radiol Med. 2013;118(June (4)):534–539. doi: 10.1007/s11547-012-0890-x. [DOI] [PubMed] [Google Scholar]
- 15.Kiu M.C1, Wan Y.L., Ng S.H., Lee S.T., Hao S.P. Pneumocephalus due to nasopharyngeal carcinoma: case report. Neuroradiology. 1996;38(January (1)):70–72. doi: 10.1007/BF00593227. [DOI] [PubMed] [Google Scholar]
- 16.Teng M.S., Futran N.D. Osteoradionecrosis of the mandible. Curr Opin Otolaryngol Head Neck Surg. 2005;13(August (4)):217–221. doi: 10.1097/01.moo.0000170527.59017.ff. [DOI] [PubMed] [Google Scholar]
- 17.Delanian S., Lefaix J.L. The radiation-induced fibroatrophic process: therapeutic perspective via the antioxidant pathway. Radiother Oncol. 2004;73(November (2)):119–131. doi: 10.1016/j.radonc.2004.08.021. [DOI] [PubMed] [Google Scholar]


