Abstract
Giant fibrovascular polyps of the oesophagus are rare benign tumours originating from the upper oesophagus. A 58-year-old woman presented with a 6-week history of a sore throat, odynophagia and progressive dysphagia, managing only a soft diet. CT of the neck and thorax, and barium swallow, both demonstrated a giant fibrovascular polyp measuring approximately 7 cm in length arising from the proximal oesophagus. The patient underwent endoscopic resection of the polyp with the assistance of ultrasonic shears. We present the case of a giant fibrovascular polyp and describe our novel technique for successful endoscopic resection using ultrasonic shears.
Background
Giant fibrovascular polyps of the oesophagus are rare, comprising <2% of all benign oesophageal tumours.1 They commonly originate from the proximal oesophagus, and often present with non-specific symptoms associated with oesophageal and respiratory obstruction, which may progress to potentially fatal airway complications. Traditional excision commonly involves a transcervical vertical oesophagotomy and there are only a few reports of endoscopic resection. In this report, we present a case of a giant fibrovascular polyp that was successfully removed endoscopically with the assistance of ultrasonic shears.
Case presentation
A 58-year-old woman presented to clinic, with a 6-week history of a sore throat, odynophagia and progressive dysphagia, managing only a soft diet. She also described the feeling of a lump in her throat. Examination of the neck was unremarkable and there was no cervical lymphadenopathy. Examination of the oral cavity revealed evidence of a previous tonsillectomy but no other abnormalities. Flexible transnasal video laryngoscopy demonstrated a distorted, rotated larynx with swelling and erythaema of the right aryepiglottic fold and a possible right piriform mass. Further visualisation of this area was not possible because of the patient's sensitive gag reflex. Her medical history was unremarkable and she did not take regular medications. She was a non-smoker with moderate alcohol consumption.
Investigations
CT of the neck and thorax demonstrated a large pedunculated polyp measuring approximately 7 cm in length in the proximal oesophagus, with appearances suggestive of a giant benign fibrovascular polyp (figure 1). Barium swallow revealed a large oesophageal polyp with its cranial attachment approximately at the level of the cricopharyngeus, with a smooth and lobulated surface (figure 2). Blood tests were within the normal range. The patient underwent an examination under anaesthesia, which revealed a large polyp arising from the pedicle in the piriform sinus and passing through the cricopharyngeal sphincter into the oesophagus. Biopsy of the lesion did not show any evidence of malignancy.
Figure 1.

Sagittal CT showing the giant fibrovascular polyp in the proximal oesophagus.
Figure 2.

Anteroposterior contrast swallow radiograph.
Treatment
The patient subsequently underwent oesophagoscopy and excision of the polyp. During removal, the polyp was exposed using a Dedo pharyngoscope with suspension arm (figure 3). The lower extent of the polyp could not be visualised as the lesion completely filled the oesophagus. The polyp was grasped at the apex and the pedicle divided with ultrasonic shears (Harmonic ACE, Ethicon, UK; figure 4). This freed the polyp while ensuring haemostasis at the same time. The polyp was too large to be removed through the pharyngoscope, so polyp and endoscope were removed simultaneously with the polyp held by two separate grasping forceps. Prior to removal, 20 mg of atracurium was administered to relax the cricopharyngeal sphincter. Oesophagoscopy was performed following the removal of the polyp and showed a dilated upper oesophagus but no bleeding or perforation (figure 5). Macroscopically, the polyp measured 6.5×3.2×0.8 cm (figure 6). Histological examination revealed a large polyp with an ulcerated surface consisting of oedematous stratified squamous epithelium overlying a loose myxoid stroma with variably sized ectatic thick and thin-walled vessels. There was a lymphoplasmacytic inflammatory infiltrate with scattered lymphoid aggregates containing a few small germinal centres but no evidence of malignancy. These histological appearances were consistent with a giant fibrovascular polyp.
Figure 3.

Endoscopic view of hypopharynx showing pedicle of polyp passing through the upper oesophageal sphincter.
Figure 4.

Endoscopic view showing the pedicle grasped with forceps.
Figure 5.
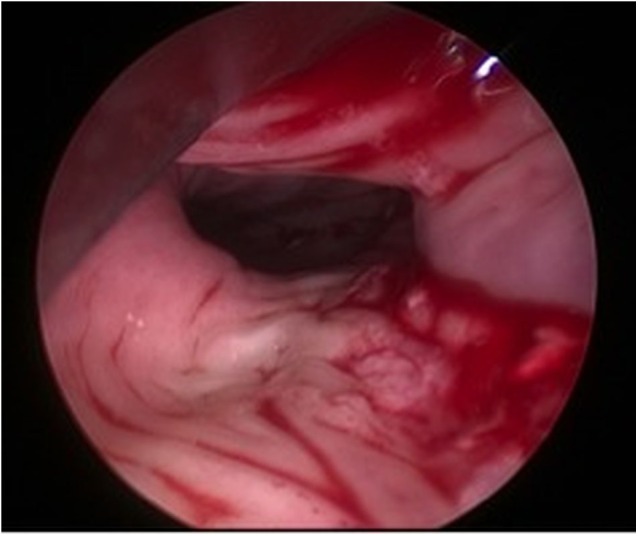
Endoscopic view of dilated upper oesophagus following removal of polyp.
Figure 6.

Giant fibrovascular polyp of the oesophagus after endoscopic removal.
Outcome and follow-up
The patient resumed a normal diet the following day and was subsequently discharged.
Discussion
Giant fibrovascular polyps of the oesophagus are rare and represent <2% of all oesophageal benign tumours.1 These polyps commonly arise from the upper oesophagus, near the level of the cricopharyngeus at the pharyngo-oesophageal junction. They consist of a core of fibroadipose connective tissue and blood vessels covered by stratified squamous epithelium. The polyps are thought to develop when the loose and relatively mobile submucosal tissue near Laimer's triangle is slowly stretched over time by oesophageal peristalsis traction and swallowing. Polyps measuring up to 26 cm have been described.2
The slow-growing nature of these polyps means that they can reach considerable sizes before becoming symptomatic. Symptoms are caused by intraluminal mass effect of the polyp and include dysphagia, odynophagia, regurgitation of food, chest or neck pain and the sensation of a lump. Regurgitation of the polyp into the mouth occurs occasionally and may, rarely, cause laryngeal obstruction leading to asphyxiation and death.3
Diagnosis may be challenging and often requires a combination of history, imaging and endoscopy. Barium studies are commonly used and show the typical appearance of a lobulated intraluminal sausage-shaped lesion with a bulbous tip.4 Endoscopic ultrasound can be used to demonstrate size, pedicle location and polyp vascularity, and has the advantage of providing a diagnostic histological sample via fine-needle aspiration cytology. CT is useful to identify feeding vessels while MRI provides multiple planes of section and high differentiation resolution of soft tissues.5
Surgical excision is the definitive treatment for giant fibrovascular polyps and is usually curative, with only a few reports of recurrence.6–8 Resection not only provides symptom control but also eliminates the risk of asphyxiation. Depending on polyp size and pedicle vascularity, an endoscopic or open approach may be used. Open excision via a transcervical/transthoracic incision is recommended for polyps longer than 8 cm or those with a thick vascular pedicle; in rare cases, thoracotomy6 or oesophagectomy9 10 may be required for very large lesions. Endoscopic resection is recommended for small polyps with a thin pedicle although lesions of up to 17 cm have been successfully removed endoscopically.11 To date, there are only five reports of endoscopic resection and techniques for removal include the use of an electrosurgical snare,11 12 Endoloop,13 14 Endo GIA stapler15 and Nd:YAG laser.16 In our case, we were able to remove the entire polyp endoscopically using a Harmonic ACE (Ethicon, UK) to divide the thick vascular pedicle, and muscle relaxant to aid delivery. By utilising this approach, we were able to avoid the complications and risks associated with open surgery.
Learning points.
Giant fibrovascular polyps of the oesophagus are rare benign tumours of the oesophagus.
Resection is indicated in all patients for symptom control as well as to eliminate the risk of asphyxiation.
Endoscopic resection is technically feasible and avoids the morbidity associated with a transcervical vertical oesophagotomy.
This report describes the novel use of ultrasonic shears to successfully facilitate endoscopic removal of a giant fibrovascular polyp.
Footnotes
Contributors: NL and AH wrote the first draft, which was revised by AM who also provided all images for the manuscript. JW provided all histopathological reports. All the authors approved the manuscript prior to submission.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Levine MS, Buck JL, Pantongrag-Brown L et al. Fibrovascular polyps of the oesophagus: clinical, radiographic and pathologic findings in 16 patients. AJR Am J Roentgenol 1996;166:781–7. 10.2214/ajr.166.4.8610549 [DOI] [PubMed] [Google Scholar]
- 2.Hoseok I, Kim JS, Shim YM. Giant fibrovascular polyp of the hypopharynx: surgical treatment with the biapproach. J Kor Med Sci 2006;21:749–51. 10.3346/jkms.2006.21.4.749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sargent RL, Hood IC. Asphyxiation caused by giant fibrovascular polyp of the oesophagus. Arch Pathol Lab Med 2006;130:725–7. [DOI] [PubMed] [Google Scholar]
- 4.Ridge C, Geoghegan T, Govender P et al. Giant oesophageal fibrovascular polyp (2005:12b). Eur Radiol 2006;16:764–6. 10.1007/s00330-005-0112-2 [DOI] [PubMed] [Google Scholar]
- 5.Ascenti G, Racchiusa S Mazzioti S et al. Giant fibrovascular polyp of the esophagus: CT and MR findings. Abdom Imaging 1999;24:109–10. 10.1007/s002619900455 [DOI] [PubMed] [Google Scholar]
- 6.Lee SY, Chan WH, Sivanandan R et al. Recurrent giant fibrovascular polyp of the esophagus. World J Gastroenterol 2009;15:3697–700. 10.3748/wjg.15.3697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Drenth JPH, Wobbes T, Bonenkamp JJ et al. Recurrent esophageal fibrovascular polyps: case history and review of the literature. Dig Dis Sci 2002;47:2598–604. 10.1023/A:1020592900552 [DOI] [PubMed] [Google Scholar]
- 8.Mufalli Behar P, Arena S, Marrangoni AG. Recurrent fibrovascular polyp of the esophagus. Am J Otolaryngol 1995;16:209–12. 10.1016/0196-0709(95)90106-X [DOI] [PubMed] [Google Scholar]
- 9.Palacios F, Contardo C, Guevara J et al. Giant oesophageal fibrovascular polyp. Rev Gastroenterol Peru 2003;23:213–16. [PubMed] [Google Scholar]
- 10.Kanaan S, DeMeester TR. Fibrovascular polyp of the esophagus requiring esophagectomy. Dis Esophagus 2007;20:453–4. 10.1111/j.1442-2050.2007.00710.x [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Hao JY, Li SWH et al. Successful endoscopic removal of a giant upper oesophageal inflammatory fibrous polyp. World J Gastroenterol 2009;15:5236–8. 10.3748/wjg.15.5236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pham AM, Rees CJ, Belafsky PC. Endoscopic removal of a giant fibrovascular polyp of the esophagus. Ann Otol Rhinol Laryngol 2008;117:587–90. 10.1177/000348940811700806 [DOI] [PubMed] [Google Scholar]
- 13.Alobid I, Vilaseca I, Fernandez J et al. Giant fibrovascular polyp of the esophagus causing sudden dyspnea: endoscopic treatment. Laryngoscope 2007;117:944–5. 10.1097/MLG.0b013e318033310f [DOI] [PubMed] [Google Scholar]
- 14.Murino A, Eisendrath P, Blero D et al. A giant fibrovascular esophageal polyp endoscopically resected using 2 gastroscopes simultaneously (with videos). Gastrointest Endosc 2014;79:834–5. 10.1016/j.gie.2014.01.001 [DOI] [PubMed] [Google Scholar]
- 15.McLean JN, DelGaudio JM. Endoscopic resection of a giant esophageal polyp: case report and review of the literature. Am J Otolaryng 2007;28:115–17. 10.1016/j.amjoto.2006.03.005 [DOI] [PubMed] [Google Scholar]
- 16.Naveau S, Bedossa P, Mallet L et al. Successful ablation of a large fibrovascular polyp of the esophagus by endoscopic Nd:YAG laser therapy. Gastrointest Endosc 1989;35:254–6. 10.1016/S0016-5107(89)72770-X [DOI] [PubMed] [Google Scholar]


