Abstract
We reviewed news reports of hepatitis A virus (HAV)-infected food handlers in the United States from 1993 to 2011 using the LexisNexis® search engine. Using U.S. news reports, we identified 192 HAV-infected food handlers who worked while infectious; of these HAV-infected individuals, 34 (18%) transmitted HAV to restaurant patrons. News reports of HAV-infected food handlers declined from 1993 to 2011. This analysis suggests that universal childhood vaccination contributed to the decrease in reports of HAV-infected food handlers, but mandatory vaccination of this group is unlikely to be cost-effective.
Reported acute hepatitis A cases in the United States have declined substantially from more than 13,000 cases in 2000 to fewer than 2,000 cases in 2013.1 According to a publication of population-based surveillance data collected from 2005 to 2007, approximately 46% of hepatitis A virus (HAV) cases reported in the United States were among people who reported recent international travel.2 Hepatitis A is a vaccine-preventable disease.3 The Advisory Committee on Immunization Practices (ACIP) recommended universal infant vaccination for 17 HAV “endemic” states (defined as ≥10 hepatitis A cases per 100,000 population per year in the state during 1987–1997) in 1999,4 with expanded recommendations for all states in 2006, regardless of hepatitis A case rates.5 Postexposure prophylaxis (PEP) with either HAV vaccine or immunoglobulin administered within 14 days of exposure can prevent HAV disease.
The Centers for Disease Control and Prevention (CDC) receives occasional reports of investigations of HAV-infected food handlers preparing food for customers, thereby putting them at risk for infection.1 It also requires extensive public notification to provide PEP to exposed patrons and significant resources, including staff time and the direct costs of vaccine and immunoglobulin.6–8 Although individual HAV cases are reported to CDC by state health departments, investigations of HAV-infected food handlers that could have exposed restaurant patrons might not be reported to CDC; however, these events might be reported in local newspapers. To assess the number of these incidents, we used a media search engine to collect news articles reporting such incidents to the public. We confirmed all reported incidents identified through the media search with the involved state and local health departments.
METHODS
We used the LexisNexis® news archive search engine (Lexis Research System, Dayton, Ohio) for 569 U.S. newspapers and wire services to retrieve newspaper articles reporting incidents in which HAV-infected food handlers worked while infectious, potentially exposing other food handlers and patrons to HAV, in the United States from January 1993 through December 2011. We used the following keywords: hepatitis A, food, food handler, case, outbreak, and investigation. All articles describing situations involving a food handler with hepatitis A were confirmed with state or local health departments by calling and asking for confirmation of details, such as total number of cases linked to the outbreak and which of the cases were among patrons and other food handlers.
The information extracted from all sources included state, county, year of exposure or event, type of food establishment (chain or local), number of potentially exposed people, number of doses of vaccine or immunoglobulin administered, and whether or not secondary cases among patrons were identified, suggesting that transmission occurred.
We compared numbers of episodes in which HAV-infected food handlers worked while infectious in the period before (1993–1999) and after (2000–2011) the 1999 ACIP universal childhood hepatitis A vaccination recommendations,3–5 and in 17 U.S. states with HAV infection incidence ≥10 cases per 100,000 population during 1987–1997 (Alaska, Arizona, Arkansas, California, Colorado, Idaho, Missouri, Montana, Nevada, New Mexico, Oklahoma, Oregon, South Dakota, Texas, Utah, Washington, and Wyoming) compared with the remaining 33 U.S. states, which did not receive the universal childhood hepatitis A vaccination recommendation until 2006.5
RESULTS
The LexisNexis search yielded 4,932 newspaper articles that included the relevant search terms, from which 192 distinct episodes in which HAV-infected food handler(s) worked while infectious were identified from 37 states in the 19-year period. HAV transmission to patrons was reported in 34 (18%) of these episodes, with a median of 19 infected patrons per episode (range: 1–110). If more than one food handler was reported as infected during the same episode, it was still only counted as one episode.
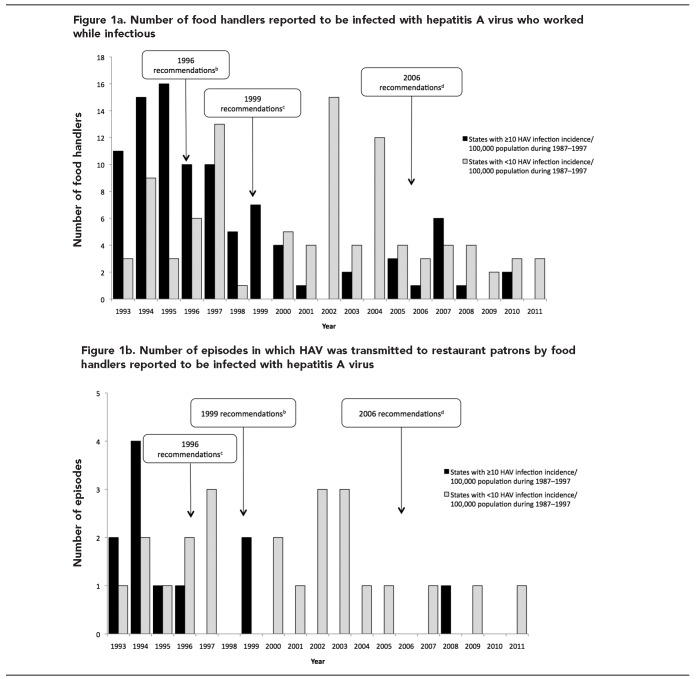
The total number of HAV-infected food handler episodes declined in all states during the study period: 109 episodes were reported in 1993–1999 (average of 16 per year), 58 episodes were reported in 2000–2006 (average of eight per year), and 25 episodes were reported in 2007–2011 (average of five per year) (Figure 1a). The biggest decline occurred in states with HAV infection incidence ≥10 cases per 100,000 population (during 1987–1997) and where vaccination recommendations were made earlier (1999). In those states, 74 (mean: 11 per year) episodes occurred during 1993–1999 compared with 11 episodes (mean: two per year) during 2000–2006 and 10 episodes (mean: two per year) during 2007–2011. However, in all other states in which universal HAV vaccination was not adopted until 2006, the number of episodes increased from 35 reports (mean: five per year) during 1993–1999 to 47 reports (mean: seven per year) during 2000–2006, and then decreased to 15 reports (mean: three per year) during 2007–2011.
Figure.
Number of episodes in which food handlers reported to be infected with hepatitis A virus worked while infectious and transmitted the virus to restaurant patrons, United States, 1993–2011a
a“States with ≥10 HAV infections per 100,000 population per year during 1987–1997” includes Alaska, Arizona, Arkansas, California, Colorado, Idaho, Missouri, Montana, Nevada, New Mexico, Oklahoma, Oregon, South Dakota, Texas, Utah, Washington, and Wyoming. “States with <10 HAV infections per 100,000 population per year” includes all other states.
bRecommendations refer to the guidelines for immunization of high-risk groups in 1996. Source: Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP) [published erratum appears in MMWR Morb Mortal Wkly Rep 1997;46:588]. MMWR Recomm Rep 1996;45(RR-15):1-3.
cRecommendations refer to the guidelines for infant vaccination made in 1999 for states with ≥10 cases of hepatitis A virus per 100,000 population. Source: Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 1999;48(RR-12):1-37.
dRecommendations refer to the guidelines for infant hepatitis A vaccination in all states in 2006. Source: Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2006;55(RR-7):1-23.
HAV = hepatitis A virus
The total number of episodes of HAV transmission to patrons as a result of an infected food handler also declined during the study period, with 19 episodes (mean: three per year) occurring in 1993–1999, 11 episodes (mean: two per year) occurring in 2000–2006, and four episodes (mean: one per year) occurring in 2007–2011 (Figure 1b). The biggest decline in episodes occurred in states with HAV infection incidence ≥10 cases per 100,000 population (during 1987–1997), where 10 episodes (mean: one per year) were identified in 1993–1999 compared with only one episode (mean: <1 per year) identified during 2000–2011. All other states had nine episodes (mean: one per year) during 1993–1999 compared with 14 episodes (mean: two per year) during 2000–2006, which was a slight increase. The number of such episodes declined again during 2007–2011, when three episodes (mean: one per year) were identified.
DISCUSSION
According to our study, HAV-infected food-handler episodes have declined substantially since 1993–1999, mirroring the decline observed nationally in the number of cases after implementation of childhood hepatitis A vaccination. Reports of HAV-infected food handlers and food-handler transmission episodes decreased earlier in states where universal vaccination of children was recommended in 1999 by ACIP (≥10 cases per 100,000 population during 1987–1997). It is likely that increases in vaccination coverage of young children led to reduced transmission, causing a herd immunity effect;9,10 children infected with HAV are frequently asymptomatic but still very contagious, causing outbreaks. These data support universal childhood vaccination policy by showing a decrease in the number of food-handler episodes coinciding with implementation of the policy in the various stages.3–5 Nonetheless, HAV-infected food handlers continue to pose a health risk and require follow-up by health departments.6
Limitations
Our study was subject to some limitations. LexisNexis is a news search engine, and newspaper reports might have had incomplete initial information regarding the final number of exposed patrons or the number of immunoglobulin or vaccinations given. The search might also have missed reports of HAV-infected food handlers that were not included in LexisNexis. These limitations would result in underreporting, but the trend would not change.
CONCLUSION
This analysis suggests that universal childhood vaccination contributed to the decrease in episodes in which HAV-infected food handlers worked while infectious and transmitted HAV to patrons.5 As such, mandatory food-handler vaccination is unlikely to be cost-effective.7 State and local health departments should make decisions about requiring vaccination for food handlers based on local needs.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Surveillance for viral hepatitis—United States, 2012 [cited 2015 Apr 14] Available from: URL: http://www.cdc.gov/hepatitis/statistics/2012surveillance/index.htm.
- 2.Klevens RM, Miller JT, Iqbal K, Thomas A, Rizzo EM, Hanson H, et al. The evolving epidemiology of hepatitis A in the United States. Incidence and molecular epidemiology from population-based surveillance, 2005–2007. Arch Intern Med. 2010;170:1811–8. doi: 10.1001/archinternmed.2010.401. [DOI] [PubMed] [Google Scholar]
- 3.Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP) [published erratum appears in MMWR Morb Mortal Wkly Rep 1997;46588] MMWR Recomm Rep. 1996;45(RR-15):1–30. [PubMed] [Google Scholar]
- 4.Prevention of hepatitis A through active or passive immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 1999;48(RR-12):1–37. [PubMed] [Google Scholar]
- 5.Fiore AE, Wasley A, Bell BP. Prevention of hepatitis A through active or passive immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006;55(RR-7):1–23. [PubMed] [Google Scholar]
- 6.Dalton CB, Haddix A, Hoffman RE, Mast EE. The cost of a food-borne outbreak of hepatitis A in Denver, Colo. Arch Intern Med. 1996;156:1013–6. [PubMed] [Google Scholar]
- 7.Meltzer MI, Shapiro CN, Mast EE, Arcari C. The economics of vaccinating restaurant workers against hepatitis A. Vaccine. 2001;19:2138–45. doi: 10.1016/s0264-410x(00)00396-0. [DOI] [PubMed] [Google Scholar]
- 8.Fiore AE. Hepatitis A transmitted by food. Clin Infect Dis. 2004;38:705–15. doi: 10.1086/381671. [DOI] [PubMed] [Google Scholar]
- 9.Armstrong GL, Billah K, Rein DB, Hicks KA, Wirth KE, Bell BP. The economics of routine childhood hepatitis A immunization in the United States: the impact of herd immunity. Pediatrics. 2007;119:e22–9. doi: 10.1542/peds.2006-1572. [DOI] [PubMed] [Google Scholar]
- 10.Klevens RM, Kruszon-Moran D, Wasley A, Gallagher K, McQuillan GM, Kuhnert W, et al. Seroprevalence of hepatitis A virus antibodies in the U.S.: results from the National Health and Nutrition Examination Survey. Public Health Rep. 2011;126:522–32. doi: 10.1177/003335491112600408. [DOI] [PMC free article] [PubMed] [Google Scholar]