Abstract
Objective
Major health disparities exist in pregnancy among young people. Although social determinant of health (SDH) approaches in interventions are promoted to reduce these disparities, little research exists that synthesizes empirical links between SDHs and pregnancy among young people. This systematic literature review utilized the Healthy People 2020 SDH framework to analyze and synthesize the empirical associations between SDHs and pregnancy among young people.
Methods
We included studies that were published in the past 25 years from PubMed, PsycINFO®, and Academic Search” Premier databases. Twenty-two studies met all inclusion criteria and, following the Matrix Method, were assessed for methodological quality and empirical links between determinant areas and pregnancy.
Results
Seventeen studies reported an empirical association between at least one SDH and pregnancy among young people. Areas most represented were poverty and family structure. No studies examined the relationship between pregnancies among young people and quality of housing, access to healthy foods, access to health-care services and primary care, health technology, social cohesion, perceptions of discrimination/equity, access to employment, employment status, school policies that support health promotion, safe school environments, or higher education enrollment.
Conclusion
This research indicates a need to expand the range of SDHs that are analyzed with pregnancy among young people and to focus interventions on areas that have been determined to have an empirical link with pregnancy.
Although recent reports indicate a historic decline in pregnancy among young people in the United States, pregnancy rates in the United States are still higher than in other developed countries, and marked racial/ethnic, geographic, and socioeconomic disparities persist. Reducing health disparities in pregnancies among young people is a path toward achieving health equity in the United States.1
Research regarding pregnancy prevention among young people is often geared toward individual and interpersonal levels, including a heavy focus on knowledge, beliefs, attitudes, skills, and personal decision making.2–6 Based on this individual-level research, the majority of currently recommended and evidence-based pregnancy prevention programs are designed to intervene at these levels.7,8 However, current public health research and interventions are less focused on how the social determinants of health (SDHs) influence unintended pregnancy among adolescents and young adults.
The exploration of SDHs to address health disparities in pregnancy among young people is promoted by the Centers for Disease Control and Prevention.1 An SDH approach may identify and address issues that are not feasibly addressed through individual or interpersonal behavior change approaches. SDHs can be defined as the conditions in which people are born, grow, live, work, and age.9 Healthy People 2020 created a framework for understanding SDHs that consists of five determinant areas: economic stability, education, social and community context, health and health care, and neighborhood and built environment.10 Within the SDH framework, a number of critical issues are listed in each of the five determinant areas.
Research links pregnancy among young people with various SDHs that fall under a wide array of topics, including exposure to incarceration, community violence, and socioeconomic disadvantage.11–13 In addition, survey data provide insight into SDHs and pregnancy among young people, especially in the area of socioeconomics. For example, children from families of lower socioeconomic status are more likely than children of families from higher socioeconomic status to experience pregnancy as an adolescent.14
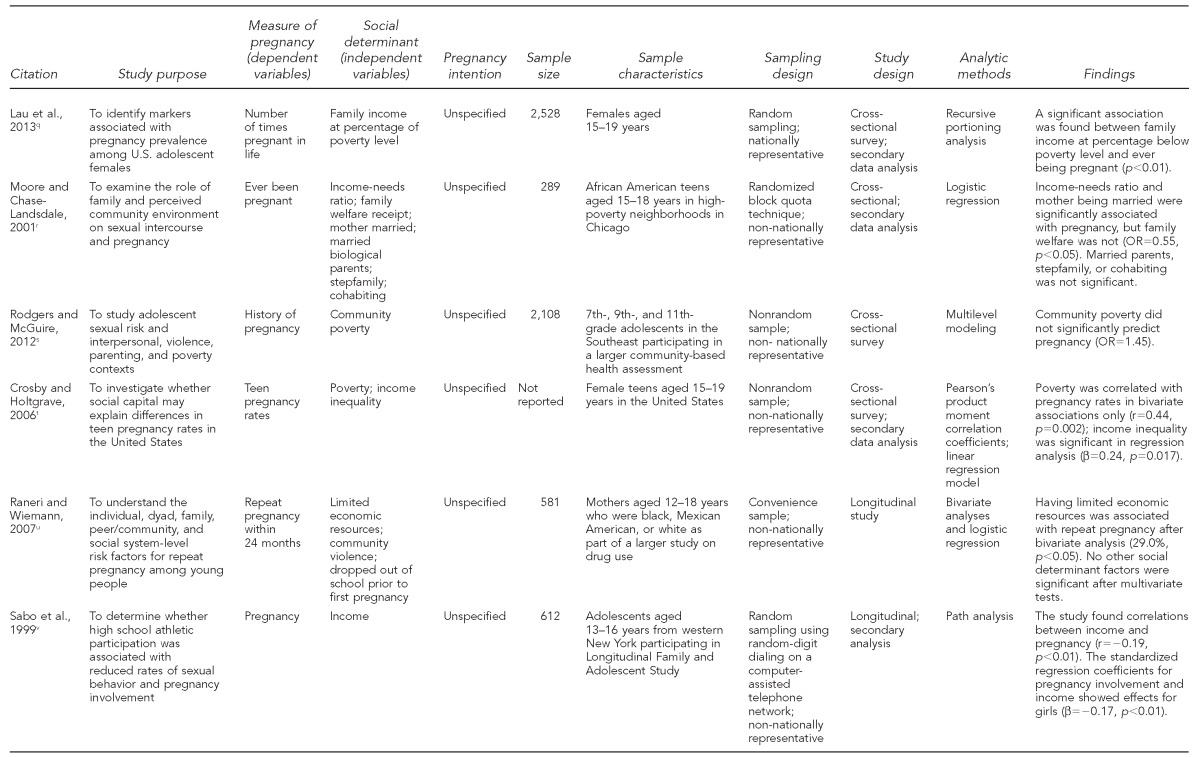
We conducted a systematic review of the literature to understand whether or not SDHs influence pregnancy among young people. This study employed the Healthy People 2020 framework for SDHs to examine links between determinants and pregnancy among young people, as well as to explore reasons why these relationships may exist. The Healthy People 2020 framework for SDHs was developed as a place-based organizing framework that distinguishes five key areas of social determinants and identifies critical components within each area that are an initial set of objectives to address for the decade (Table 1).15 Models that include elements of SDHs, such as the Healthy People 2020 Framework, are recommended to guide public health practice.16
Table 1.
Healthy People 2020 social determinants of health framework key issuesa
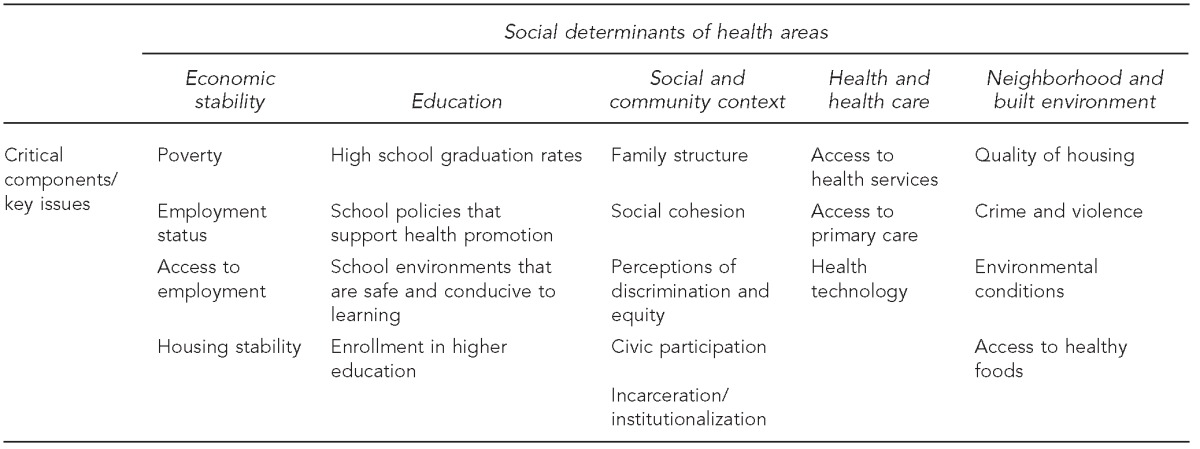
Department of Health and Human Services (US), Office of Disease Prevention and Health Promotion. Healthy People 2020: social determinants of health [cited 2014 Oct 9]. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39
The analysis included empirical research studies that linked pregnancy among young people and SDHs in the following areas: economic stability, social and community context, neighborhood and built environment, health and health care, and education. Each of the five key areas included critical components used for the review based on the conceptual framework developed by Healthy People 2020.10
METHODS
Literature search
We searched the scholarly databases PsycINFO®, PubMed, and Academic Search” Premier following guidelines of the Matrix Method,17 which provides guidelines to collect, organize, and analyze information in a systematic manner. When possible, medical subject heading terms were used for social determinant search terms.18 Search terms included a combination of the use of words from each key area of the SDH. (A list of keywords is available upon request.)
Inclusion and exclusion criteria
We included studies that focused on an empirical relationship between pregnancy among young people and one or more SDHs, based on the Healthy People 2020 SDH framework. Other criteria for inclusion included studies that were published during the past 25 years, from January 1988 to August 2013, and involved participants aged 13–25 years. This wide age range was selected to include a breadth of literature due to a lack of consistency in previous research of what age range defines young people.19,20 The date range was more than 10 years to address the rise of popularity and recognition of SDHs in the early 2000s.21–23 Measures for the dependent variable of pregnancy must have measured pregnancy itself rather than birth. Additional inclusion criteria were that studies were U.S.-based, peer reviewed, quantitative, and published in an English-language journal.
Studies were excluded if they did not analyze an empirical link between SDHs and pregnancy. As such, all qualitative studies, studies without a focus on links between SDHs and pregnancy among young people (e.g., management of existing pregnancy), and studies examining participants >25 years of age were excluded. In addition, studies with an outcome variable of birth or fathering a child were excluded because articles not measuring pregnancy itself violated the inclusion criteria of pregnancy as the outcome variable. Birth does not fully capture the measure of pregnancy because not all pregnancies result in birth.24 Letters to the editor and other non-peer-reviewed documents were also excluded.
Data extraction
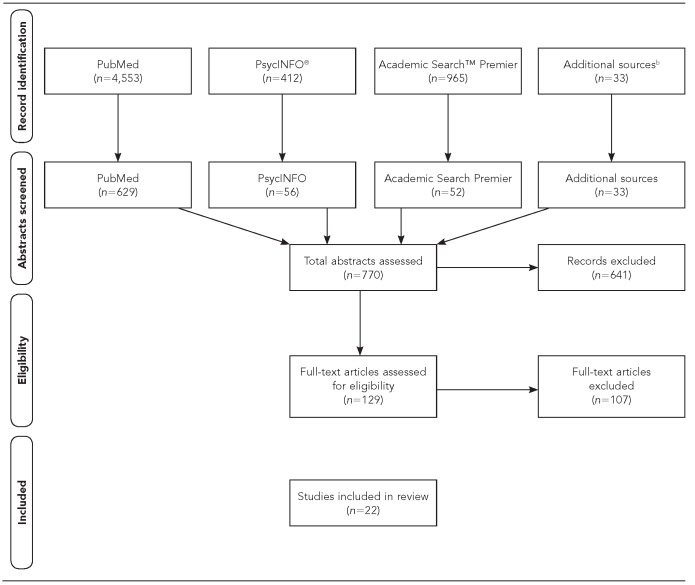
The initial search identified 5,963 studies—reviewed by a single reviewer based on title and keywords—of which 770 abstracts were reviewed. Twenty-two articles met all inclusion criteria and were abstracted for the findings matrix (Figure). The selected articles were assessed for significant and nonsignificant empirical relationships between pregnancy among young people and one or more SDHs in the Healthy People 2020 SDH framework.10 A single study could contribute multiple findings to the review.
Figure.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram of studies empirically analyzing associations between social determinants of health and pregnancy among young peoplea
aAdapted from Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med 2009;151:264-9.
bAdditional sources include articles included from the reference sections of other identified articles.
RESULTS
Summary of findings
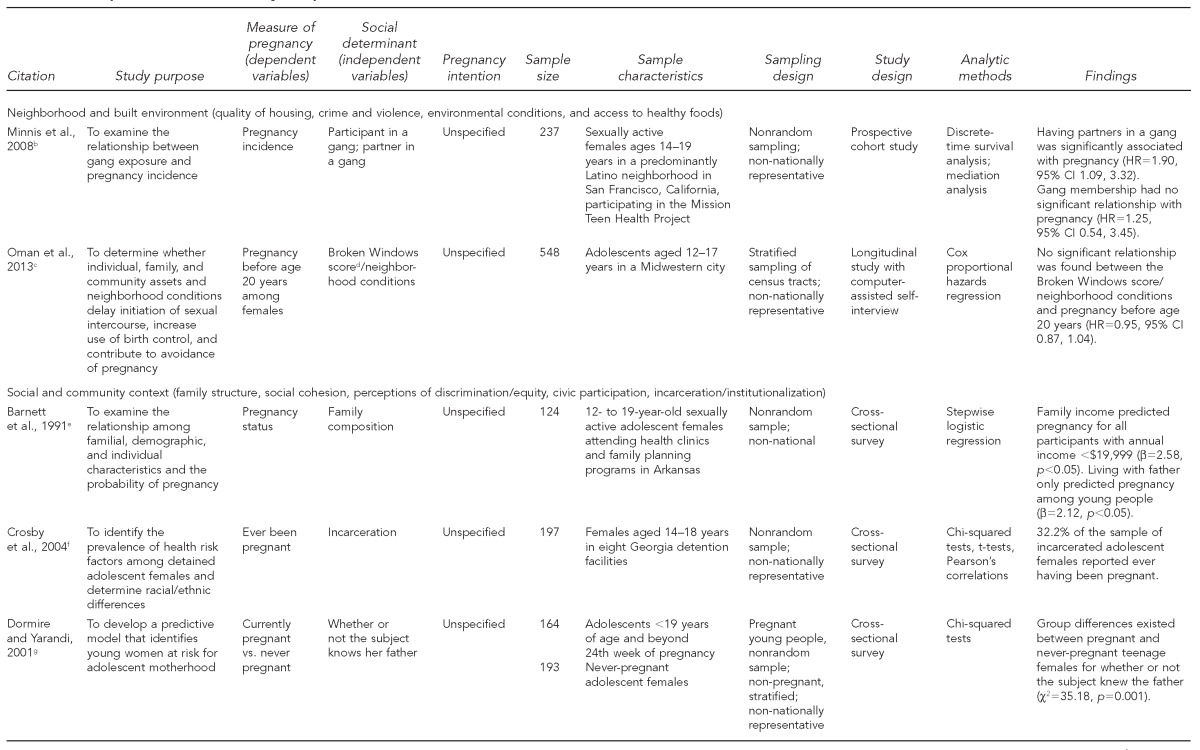
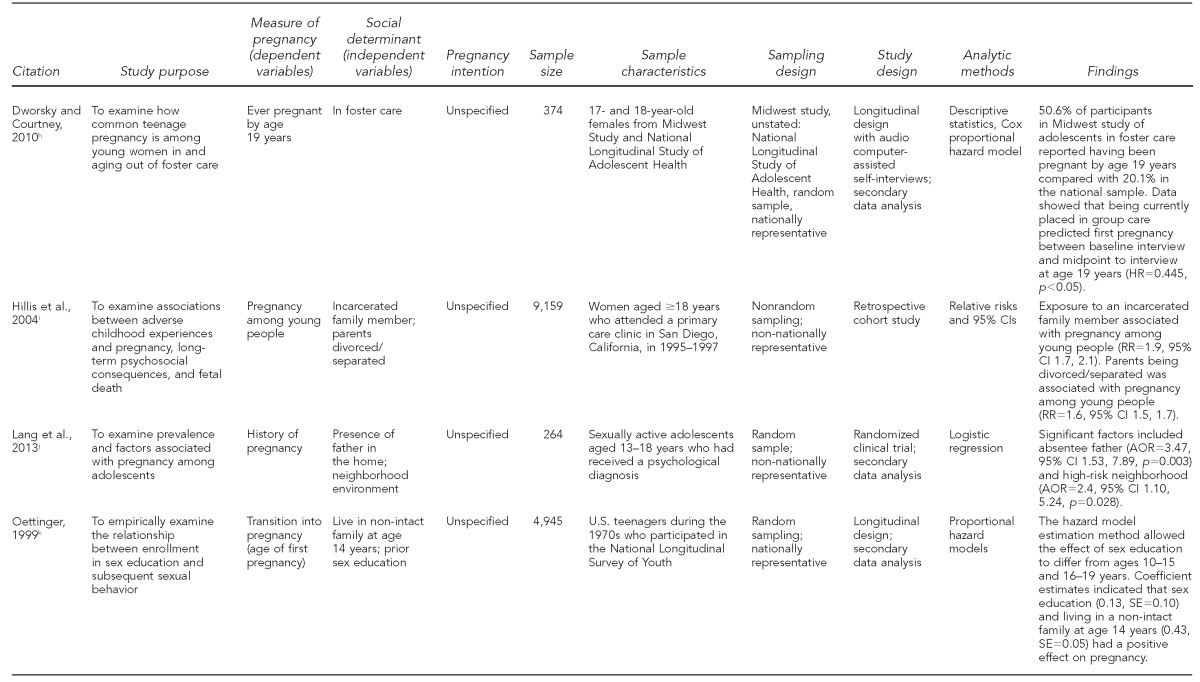
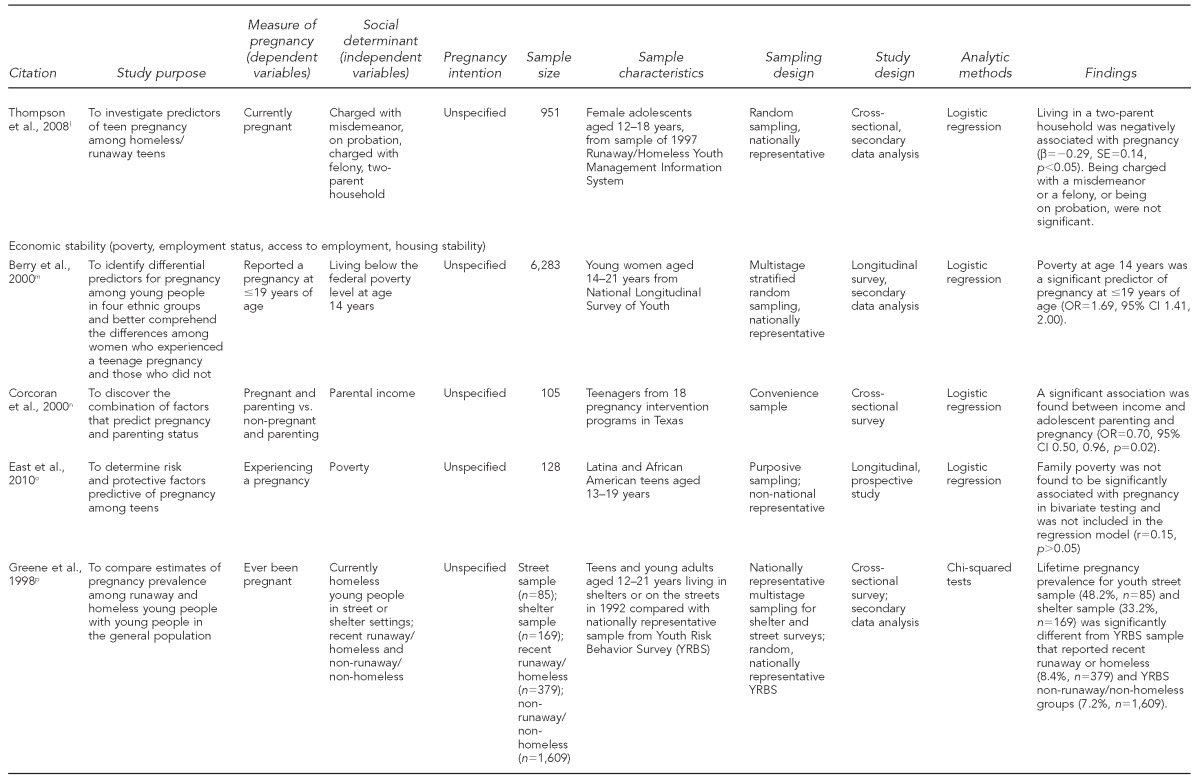
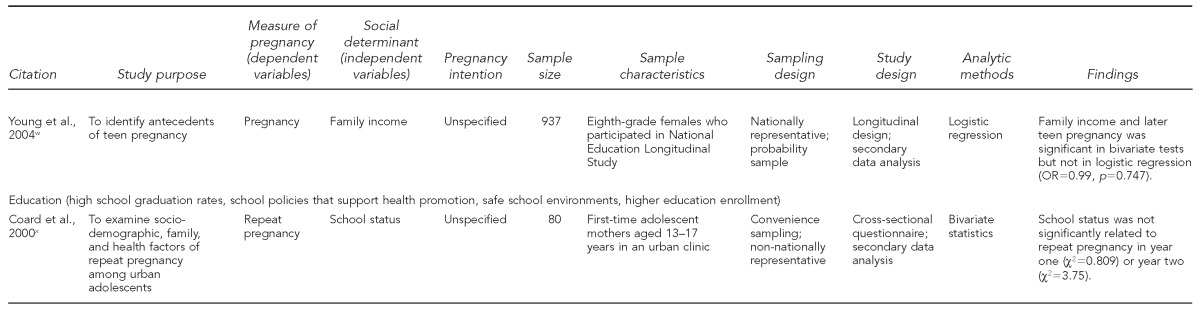
Twenty-two articles covered four of the five determinant areas of the Healthy People 2020 SDH framework. The majority of articles were in the areas of economic stability (n=11) and social and community context (n=9). No articles were identified in the determinant area of health and health care. Only eight of the 20 critical components within the five determinant areas were represented in abstracted articles. These critical components included crime and violence, environmental conditions, family structure, incarceration/institutionalization, poverty, housing stability, and high school graduation rates (Table 2). If a study analyzed more than one social determinant, it is listed in Table 2 under primary research area.
Table 2.
Methodological quality and findings of articles examining associations between social determinants of health and pregnancy among young people, based on components of the Healthy People 2020 Social Determinants of Health Framework, 2010a
No articles identified a link between pregnancy and the social determinant of health (SDH) health and health care. As such, only four SDHs from the Healthy People 2020 SDH framework are listed along with articles showing a link between those SDHs and pregnancy. Source: Department of Health and Human Services (US). The Secretary's Advisory Committee on National Health Promotion and Disease Prevention objectives for 2020: phase I report: recommendations for the framework and format of Healthy People 2020. 2008 [cited 2015 Sep 24]. Available from: URL: http://www.healthypeople.gov/sites/default/files/phaseI_0.pdf
bMinnis AM, Moore JG, Doherty IA, Rodas C, Auerswald C, Shiboski S, et al. Gang exposure and pregnancy incidence among female adolescents in San Francisco: evidence for the need to integrate reproductive health with violence prevention efforts. Am J Epidemiol 2008;167:1102-9.
cOman RF, Vesely SK, Aspy CB, Tolma EL, Gavin L, Bensyl DM, et al. A longitudinal study of youth assets, neighborhood conditions, and youth sexual behaviors. J Adolesc Health 2013;52:779-85.
dCohen D, Spear S, Scribner R, Kissinger P, Mason K, Wildgen J. “Broken windows” and the risk of gonorrhea. Am J Public Health 2000;90:230-6.
eBarnett JK, Papini DR, Gbur E. Familial correlates of sexually active pregnant and nonpregnant adolescents. Adolescence 1991;26:457-72.
fCrosby R, Salazar LF, DiClemente RJ, Yarber WL, Caliendo AM, Staples-Horne M. Health risk factors among detained adolescent females. Am J Prev Med 2004;27:404-10.
gDormire SL, Yarandi H. Predictors of risk for adolescent childbearing. Appl Nurs Res 2001;14:81-6.
hDworsky A, Courtney ME. The risk of teenage pregnancy among transitioning foster youth: implications for extending state care beyond age 18. Child Youth Serv Rev 2010;32:1351-6.
iHillis SD, Anda RF, Dube SR, Felittie VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics 2004;113:320-7.
jLang DL, Rieckmann T, DiClemente RJ, Crosby RA, Brown LK, Donenberg GR. Multi-level factors associated with pregnancy among urban adolescent women seeking psychological services. J Urban Health 2013;90:212-23.
kOettinger GS. The effects of sex education on teen sexual activity and teen pregnancy. J Political Econ 1999;107:606-44.
lThompson SJ, Bender KA, Lewis CM, Watkins R. Runaway and pregnant: risk factors associated with pregnancy in a national sample of runaway/homeless female adolescents. J Adolesc Health 2008;43:125-32.
mBerry EH, Shillington AM, Peak T, Hohman MM. Multi-ethnic comparison of risk and protective factors for adolescent pregnancy. Child Adolesc Soc Work J 2000;17:79-96.
nCorcoran J, Franklin C, Bennett P. Ecological factors associated with adolescent pregnancy and parenting. Soc Work Res 2000;24:29-39.
oEast PL, Khoo ST, Reyes BT. Risk and protective factors predictive of adolescent pregnancy: a longitudinal, prospective study. Appl Dev Sci 2006;10:188-99.
pGreene JM, Ringwalt CL. Pregnancy among three national samples of runaway and homeless youth. J Adolesc Health 1998;23:370-7.
qLau M, Lin H, Flores G. Clusters of markers identify high and low prevalence of adolescent pregnancy in the U.S. J Pediatr Adolesc Gynecol 2013;26:40-6.
rMoore MR, Chase-Lansdale PL. Sexual intercourse and pregnancy among African American girls in high-poverty neighborhoods: the role of family and perceived community environment. J Marriage Fam 2001; 63:1146-57.
sRodgers KB, McGuire JK. Adolescent sexual risk and multiple contexts: interpersonal violence, parenting, and poverty. J Interpers Violence 2012;27:2091-107.
tCrosby RA, Holtgrave DR. The protective value of social capital against teen pregnancy: a state-level analysis. J Adolesc Health 2006;38:556-9.
uRaneri LG, Wiemann CM. Social ecological predictors of repeat adolescent pregnancy. Perspect Sex Reprod Health 2007;39:39-47.
vSabo DF, Miller KE, Farrell MP, Melnick MJ, Barnes GM. High school athletic participation, sexual behavior and adolescent pregnancy: a regional study. J Adolesc Health 1999;25:207-16.
wYoung T, Turner J, Denny G, Young M. Examining external and internal poverty as antecedents of teen pregnancy. Am J Health Behav 2004;28:361-73.
xCoard SI, Nitz K, Felice ME. Repeat pregnancy among urban adolescents: sociodemographic, family, and health factors. Adolescence 2000;35:193-200.
HR = hazard ratio
CI = confidence interval
RR = relative risk
AOR = adjusted odds ratio
OR = odds ratio
Neighborhood and built environment
Four studies included evidence in the area of neighborhood and built environment.25–28 Under the study framework, this area could have included studies analyzing quality of housing, crime and violence, environmental conditions, or access to healthy foods.10 Of these four critical components, crime and violence as well as environmental conditions were assessed25–28 (Table 2).
One study examined the relationship between gang exposure and pregnancy incidence and found that gang membership did not have a significant relationship with pregnancy (hazard ratio [HR]=1.25, 95% confidence interval [CI] 0.54, 3.45), but having a partner in a gang was associated with pregnancy incidence (HR=1.90, 95% CI 1.09, 3.32).26 Additional studies related to neighborhood and built environment found that community violence was not related to a repeat pregnancy within 24 months,28 and there was no significant relationship between the Broken Windows assessment—an instrument that examines neighborhood disorganization based on the condition of buildings, amount of trash, graffiti, and abandoned cars—and pregnancy before 20 years of age (HR=0.95, 95% CI 0.87, 1.04).27 However, the fourth study included in the review found that a history of pregnancy was associated with living in a high-risk neighborhood environment (adjusted odds ratio [AOR] = 2.40, 95% CI 1.10, 5.24, p=0.028)25 (Table 2).
Social and community context
Eight studies analyzed social and community context,25,29–35 while one study analyzed social and community context only as a secondary variable. Under the Healthy People 2020 SDH framework, these types of articles could have included family structure, social cohesion, perceptions of discrimination/equity, civic participation, or incarceration/institutionalization.10 Of these critical components, the most commonly researched SDHs were family structure (reported in seven articles) and incarceration (reported in three articles)25,29–32,34–36 (Table 2).
Family structure was measured by six studies in nine different ways, including knowing one's father, father living in the home, a two-parent household, mother married, married biological parents, stepfamily (defined as biological parent married to nonbiological parent), cohabiting (defined as biological parent living with partner but unmarried), parental separation or divorce, or living in group foster care. All associations were significant except for the study that examined married biological parents, stepfamily, and cohabitation33 (Table 2).
Of studies examining young people living with one or both biological parents, one found that living with the father only predicted pregnancy status (p<0.05).29 However, another study indicated a positive association between a father not living in the home and adolescent pregnancy (AOR=3.47, 95% CI 1.53, 7.89, p=0.003).25 Another study found group differences between pregnant and never-pregnant adolescent females by whether or not they knew their father (c2=35.18, p=0.001).31 Additional findings reported a negative association between living in a two-parent household and pregnancy (b=0.29, standard error = 0.14, p<0.05)35 as well as a significant positive association between divorced or separated parents and pregnancy among young people (relative risk [RR] = 1.6, 95% CI 1.5, 1.7).32 A study that examined family structure in greater detail indicated that the mother being married was negatively associated with pregnancy among young people, while having married biological parents, a stepfamily, or a parent cohabiting with a partner were not associated with pregnancy in the full model.33
A study examining family structure by researching adolescents in foster care found that 50.6% of foster care participants had ever been pregnant by 19 years of age in comparison with 20.1% of their peers in a national sample. In addition, data indicated that being currently in group care predicted a first pregnancy between the baseline interview and midpoint of the study36 (Table 2).
The critical component of incarceration was examined by both exposure to incarceration of a family member and incarceration of the young person. Exposure to an incarcerated family member was found to be positively associated with pregnancy among young people (RR=1.9, 95% CI 1.7, 2.1).32 One study found that 32.2% of a sample of incarcerated adolescent females reported ever having been pregnant, which is higher than the national average.30 However, a second study reported no associations between pregnancy and being charged with a misdemeanor, being on probation, or being charged with a felony35 (Table 2).
Economic stability
Economic stability was examined in 12 studies.28–30,33,37–44 Under the guiding framework, studies eligible to be included in this area would have examined key areas of poverty, employment status, access to employment, or housing stability.10 In abstracted articles where measures of income were utilized instead of poverty, these measures were included. Of these critical components, 11 studies examined poverty28–30,33,37–39,41–44 and only one study examined housing stability40 (Table 2).
Among studies examining poverty, seven studies found a significant association with pregnancy among young people,29,30,33,37,38,41,43 two studies found significant associations in bivariate testing only,28,44 and two studies found no relationship between poverty and pregnancy.39,42 The seven studies that found significant associations between poverty and pregnancy among young people included those living below the federal poverty level (FPL) at 14 years of age, family income, poverty, parental income, and income-needs ratio. One study indicated that poverty at 14 years of age was a significant predictor of pregnancy by age 19 years (odds ratio [OR] = 1.69, 95% CI 1.41, 2.00),37 and another study indicated that annual family income <$19,999 predicted pregnancy among young people (p<0.05).29 Additional studies supported these results, including one that associated income and adolescent parenting with pregnancy (OR=0.70, 95% CI 0.50, 0.96, p=0.02),38 one that associated parental income at percentage below FPL with number of times pregnant in life (p<0.01),41 and another associating income with pregnancy (b=–0.17, p<0.01)43 (Table 2).
Not all included studies found significant associations linking economic stability-related measures with adolescent pregnancy. A study including related measures reported that the income-needs ratio was significantly associated with ever having been pregnant, but family welfare receipt was not (OR=0.55, p<0.05).33 Another study found that poverty (r=0.44, p=0.002) and income equality (r=0.53, p<0.001) were positively associated with teen pregnancy rates in bivariate associations; however, only income equality was significant in the linear regression model (b=0.24, p=0.017).45 Two additional studies found significance between pregnancy and limited economic resources or family income only at bivariate levels.28,44 However, nonsignificant findings included that family poverty was not significantly associated with pregnancy39 and that poverty did not significantly predict a history of pregnancy (OR=1.45)42 (Table 2).
The one study that did not examine poverty within the economic determinant analyzed current homeless or runaway young people and pregnancy. The lifetime pregnancy prevalence for young people living on the street (48.2%, n=85) and in shelters (33.2%, n=169) was significantly higher than a national sample of runaway/homeless young people (8.4%, n=379) and non-runaway/non-homeless young people (7.2%, n=1,609)40 (Table 2).
Education
We identified two articles under the determinant of education, and neither article reported significant associations between pregnancy and education.28,46 In the Healthy People 2020 SDH framework, the social determinant of education encompasses high school graduation rates, school policies that support health promotion, safe school environments, and higher education enrollment.10 One study found that dropping out of school prior to first pregnancy was not associated with pregnancy rates,28 while the second study found that school status was not significantly related to repeat pregnancy within one year (c2=0.809) or two years (c2=3.75)46 (Table 2).
Methodological quality
Of the 22 studies included in the review, 11 employed cross-sectional designs,29–31,33,35,38,40–42,45,46 eight used longitudinal designs,27,28,34,36,37,39,43,44 one was a prospective cohort study,26 one was a retrospective cohort study,32 and one was a cross-sectional, randomized clinical trial.25 The sample sizes ranged from 80 participants46 to 9,159 participants.32 No studies reported reliability or validity for any measures related to SDHs or pregnancy. Twelve studies analyzed secondary data.25,33–37,40,41,43–46 Nine studies employed logistic regression analyses,25,28,29,33,35,37–39,44 four studies employed bivariate analyses,31,40,45,46 and three studies used Cox proportional hazards regression.27,34,36 Six studies reported 95% CIs25–27,32,37,38 (Table 2).
DISCUSSION
This study employed the Healthy People 2020 SDH framework to examine links between determinants and pregnancy among young people and explore reasons for these relationships. Although four of the five determinants were found in the included studies, many of the critical components within these determinants were not included. For example, no studies examined the relationship between pregnancies among young people and quality of housing, access to healthy foods, access to health-care services and primary care, health technology, social cohesion, perceptions of discrimination/equity, access to employment, employment status, school policies that support health promotion, safe school environments, or higher education enrollment.
The fact that 13 of the 20 critical components within the five determinant areas of health were not represented by studies in this review indicates a gap in the literature. Healthy People 2020 identified these critical components as areas in need of intervention in all aspects of health promotion this decade (i.e., 2010–2020); yet, without empirical evidence it is not prudent to begin interventions in areas that have not been linked to pregnancy among young people. Young people up to 25 years of age were included and those aged >25 years were excluded based on research indicating that brain development and decision-making processes do not reach full maturity until this age; however, this review did not provide information on the full age range of this population.47,48 Indications of brain development not reaching maturity until 25 years of age indicates a need for further research among young adults in their early to mid-20s.
We found studies of varying methodological quality and a body of literature that was largely stagnant in terms of analytic methods. For one, half of all research findings on pregnancy and social determinant areas of health were based on cross-sectional study designs. Future research should employ more sophisticated (i.e., longitudinal) designs in an effort to improve the ability to link social determinants to a later pregnancy, thereby enhancing causal inference. Second, no studies reported reliability or validity for any measures related to SDHs or pregnancy. This type of exclusion limited our ability to conduct meta-analytic studies and to assess evidence regarding appropriate measurement of constructs. Third, most studies employed very simple bivariate or, at best, multivariable analyses, such as logistic regression. Only one study employed path analysis, and no other research utilized structural equation modeling (SEM). More sophisticated analyses regarding linkages between SDHs and pregnancy are needed. For example, SEM of these data would be critical, as SEM maintains several advantages over simpler analytic techniques.49 SDH research would be best situated if its analytic techniques mirrored this reality of health and human behavior.
Strengths and limitations
Our study was unique in that it utilized a framework to tie together a wide array of SDHs and examine key areas within each determinant that have been identified as vital to address in 2010–2020.1 Previous systematic reviews in this area have not been limited to social determinants nor have they used a framework tied to ongoing action such as Healthy People 2020.8 And, as noted previously, this study revealed a gap in the literature: 13 of the 20 critical components within the five determinant areas of health were not represented by studies in this review. The findings of this study indicate the need to support interventions in pregnancy among young people based on many areas of SDHs.
This study was also subject to several limitations. First, the Healthy People 2020 SDH framework includes critical components for the decade, but may not include an exhaustive compilation of elements of SDHs. Second, this review included study designs that were experimental as well as nonexperimental, which limited our ability to assess study findings uniformly. Utilizing the measure of pregnancy as inclusion criteria excluded similar studies that measured birth, fathering a child, or being a male involved in a pregnancy. Third, this review predominantly included studies that sampled teenagers and young adults up to 25 years of age. Therefore, the associations made in this review cannot be generalized to “older” young people. Fourth, pregnancy was measured in several different ways. Although no studies included in the final review had participants older than 21 years of age, differences in pregnancies among younger adolescents (aged 12–15 years) and older adolescents/young adults were found. Fifth, none of the included studies measured pregnancy intention, so we were not able to discuss this aspect. Sixth, this systematic review was conducted by a single reviewer rather than multiple reviewers, which may have introduced bias in assessing each study. Finally, the review included only published studies, which may have excluded information from studies in which the findings were not significant or were otherwise not published (i.e., the file drawer effect).
PUBLIC HEALTH IMPLICATIONS
We found evidence in the literature regarding the relationship between areas of SDHs and pregnancy among young people. SDHs have been indicated as a vital way to reduce health disparities in pregnancy among young people.1 To most effectively use information on SDHs to create interventions in this area, we must first base these interventions on empirical evidence. This review provides evidence of areas in which pregnancy among young people has been linked to such SDHs as measures of economic stability, education, social and community context, and neighborhood and built environment; however, more work is needed to envision the full picture of the relationship between SDHs and pregnancy among young people.
Footnotes
As an analysis of secondary data, this analysis was determined as exempt by the University of South Florida Institutional Review Board.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Disparities in teen birth rates. 2015 [cited 2015 Sep 28] Available from: http://www.cdc.gov/teenpregnancy/about/index.htm.
- 2.Crenshaw DA, Lee J. At-risk adolescents: self-esteem, youth violence, and teen pregnancy. In: Guindon MH, editor. Self-esteem across the lifespan: issues and interventions. New York: Routlege/Taylor & Francis Group; 2010. pp. 143–57. [Google Scholar]
- 3.Deptula DP, Henry DB, Schoeny ME. How can parents make a difference? Longitudinal associations with adolescent sexual behavior. J Fam Psychol. 2010;24:731–9. doi: 10.1037/a0021760. [DOI] [PubMed] [Google Scholar]
- 4.Finer LB, Philbin JM. Sexual initiation, contraceptive use, and pregnancy among young adolescents. Pediatrics. 2013;131:886–91. doi: 10.1542/peds.2012-3495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.House LD, Mueller T, Reininger B, Brown K, Markham CM. Character as a predictor of reproductive health outcomes for youth: a systematic review. J Adolesc Health. 2010;46(3 Suppl):S59–74. doi: 10.1016/j.jadohealth.2009.11.218. [DOI] [PubMed] [Google Scholar]
- 6.Reese BM, Haydon AA, Herring AH, Halpern CT. The association between sequences of sexual initiation and the likelihood of teenage pregnancy. J Adolesc Health. 2013;52:228–33. doi: 10.1016/j.jadohealth.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Department of Health and Human Services (US), Office of Adolescent Health. Evidence-based programs [cited 2015 Sep 24] Available from: http://www.hhs.gov/ash/oah/oah-initiatives/teen_pregnancy/db/tpp-searchable.html.
- 8.Kirby D. Washington: The National Campaign to Prevent Teen and Unplanned Pregnancy; 2007. Emerging answers 2007: research findings on programs to reduce teen pregnancy—full report. Also available from: http://www.thenationalcampaign.org/EA2007/EA2007_full.pdf [cited 2013 Oct 5] [Google Scholar]
- 9.World Health Organization. Social determinants of health [cited 2013 Aug 28] Available from: http://www.who.int/social_determinants/en.
- 10.Department of Health and Human Services (US), Office of Disease Prevention and Health Promotion. Healthy People 2020: social determinants of health [cited 2013 Aug 28] Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39.
- 11.Miller E, Levenson R, Herrera L, Kurek L, Stofflet M, Marin L. Exposure to partner, family, and community violence: gang-affiliated Latina women and risk of unintended pregnancy. J Urban Health. 2012;89:74–86. doi: 10.1007/s11524-011-9631-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Penman-Aguilar A, Carter M, Snead MC, Kourtis AP. Socioeconomic disadvantage as a social determinant of teen childbearing in the U.S. Public Health Rep. 2013;128(Suppl 1):5–22. doi: 10.1177/00333549131282S102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Whalen ML, Loper AB. Teenage pregnancy in adolescents with an incarcerated household member. West J Nurs Res. 2014;36:346–61. doi: 10.1177/0193945913496873. [DOI] [PubMed] [Google Scholar]
- 14.Singh S, Darroch JE, Frost JJ. Socioeconomic disadvantage and the adolescent women's sexual and reproductive behavior: the case of five developed countries. Fam Plann Perspect. 2001;33:251–8. 289. [PubMed] [Google Scholar]
- 15.Department of Health and Human Services (US) The Secretary's Advisory Committee on National Health Promotion and Disease Prevention objectives for 2020: phase I report: recommendations for the framework and format of Healthy People 2020. 2008 [cited 2015 Sep 24] Available from: http://www.healthypeople.gov/sites/default/files/phaseI_0.pdf.
- 16.Golden SD, Earp AL. Social ecological approaches to individuals and their contexts: twenty years of Health Education & Behavior health promotion interventions. Health Educ Behav. 2012;39:364–72. doi: 10.1177/1090198111418634. [DOI] [PubMed] [Google Scholar]
- 17.Garrard J. Sudbury (MA): Jones and Bartlett Publishers; 2004. Health sciences literature review made easy: the Matrix Method. [Google Scholar]
- 18.National Institutes of Health (US), National Library of Medicine. Medical subject headings [cited 2013 Mar 26] Available from: http://www.nlm.nih.gov/mesh.
- 19.World Health Organization. Adolescents: health risks and solutions. 2014 [cited 2014 Jul 8] Available from: http://www.who.int/mediacentre/factsheets/fs345/en.
- 20.Centers for Disease Control and Prevention (US) Sexually transmitted diseases: reportable STDs in young people 15–24 years of age, by state [cited 2014 Jul 8] Available from: http://www.cdc.gov/std/stats/by-age/15-24-all-stds/default.htm.
- 21.Kindig DA. Understanding population health terminology. Milbank Q. 2007;85:139–61. doi: 10.1111/j.1468-0009.2007.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krieger N. A glossary for social epidemiology. J Epidemiol Community Health. 2001;55:693–700. doi: 10.1136/jech.55.10.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raphael D. Toronto: Canadian Scholar's Press; 2004. Social determinants of health: Canadian perspectives. [Google Scholar]
- 24.Ventura SJ, Curtin SC, Abma JC, Henshaw SK. Estimated pregnancy rates and rates of pregnancy outcomes for the United States, 1990–2008. Natl Vital Stat Rep. 2012 Jun 20;60(7):1–22. [PubMed] [Google Scholar]
- 25.Lang DL, Rieckmann T, DiClemente RJ, Crosby RA, Brown LK, Donenberg GR. Multi-level factors associated with pregnancy among urban adolescent women seeking psychological services. J Urban Health. 2013;90:212–23. doi: 10.1007/s11524-012-9768-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Minnis AM, Moore JG, Doherty IA, Rodas C, Auerswald C, Shiboski S, et al. Gang exposure and pregnancy incidence among female adolescents in San Francisco: evidence for the need to integrate reproductive health with violence prevention efforts. Am J Epidemiol. 2008;167:1102–9. doi: 10.1093/aje/kwn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oman RF, Vesely SK, Aspy CB, Tolma EL, Gavin L, Bensyl DM, et al. A longitudinal study of youth assets, neighborhood conditions, and youth sexual behaviors. J Adolesc Health. 2013;52:779–85. doi: 10.1016/j.jadohealth.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Raneri LG, Wiemann CM. Social ecological predictors of repeat adolescent pregnancy. Perspect Sex Reprod Health. 2007;39:39–47. doi: 10.1363/3903907. [DOI] [PubMed] [Google Scholar]
- 29.Barnett JK, Papini DR, Gbur E. Familial correlates of sexually active pregnant and nonpregnant adolescents. Adolescence. 1991;26:457–72. [PubMed] [Google Scholar]
- 30.Crosby R, Salazar LF, DiClemente RJ, Yarber WL, Caliendo AM, Staples-Horne M. Health risk factors among detained adolescent females. Am J Prev Med. 2004;27:404–10. doi: 10.1016/j.amepre.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 31.Dormire SL, Yarandi H. Predictors of risk for adolescent childbearing. Appl Nurs Res. 2001;14:81–6. doi: 10.1053/apnr.2001.22373. [DOI] [PubMed] [Google Scholar]
- 32.Hillis SD, Anda RF, Dube SR, Felittie VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004;113:320–7. doi: 10.1542/peds.113.2.320. [DOI] [PubMed] [Google Scholar]
- 33.Moore MR, Chase-Lansdale PL. Sexual intercourse and pregnancy among African American girls in high-poverty neighborhoods: the role of family and perceived community environment. J Marriage Fam. 2001;63:1146–57. [Google Scholar]
- 34.Oettinger GS. The effects of sex education on teen sexual activity and teen pregnancy. J Political Econ. 1999;107:606–44. [Google Scholar]
- 35.Thompson SJ, Bender KA, Lewis CM, Watkins R. Runaway and pregnant: risk factors associated with pregnancy in a national sample of runaway/homeless female adolescents. J Adolesc Health. 2008;43:125–32. doi: 10.1016/j.jadohealth.2007.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dworsky A, Courtney ME. The risk of teenage pregnancy among transitioning foster youth: implications for extending state care beyond age 18. Child Youth Serv Rev. 2010;32:1351–6. [Google Scholar]
- 37.Berry EH, Shillington AM, Peak T, Hohman MM. Multi-ethnic comparison of risk and protective factors for adolescent pregnancy. Child Adolesc Soc Work J. 2000;17:79–96. [Google Scholar]
- 38.Corcoran J, Franklin C, Bennett P. Ecological factors associated with adolescent pregnancy and parenting. Soc Work Res. 2000;24:29–39. [Google Scholar]
- 39.East PL, Khoo ST, Reyes BT. Risk and protective factors predictive of adolescent pregnancy: a longitudinal, prospective study. Appl Dev Sci. 2006;10:188–99. [Google Scholar]
- 40.Greene JM, Ringwalt CL. Pregnancy among three national samples of runaway and homeless youth. J Adolesc Health. 1998;23:370–7. doi: 10.1016/s1054-139x(98)00071-8. [DOI] [PubMed] [Google Scholar]
- 41.Lau M, Lin H, Flores G. Clusters of markers identify high and low prevalence of adolescent pregnancy in the U.S. J Pediatr Adolesc Gynecol. 2013;26:40–6. doi: 10.1016/j.jpag.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 42.Rodgers KB, McGuire JK. Adolescent sexual risk and multiple contexts: interpersonal violence, parenting, and poverty. J Interpers Violence. 2012;27:2091–107. doi: 10.1177/0886260511432148. [DOI] [PubMed] [Google Scholar]
- 43.Sabo DF, Miller KE, Farrell MP, Melnick MJ, Barnes GM. High school athletic participation, sexual behavior and adolescent pregnancy: a regional study. J Adolesc Health. 1999;25:207–16. doi: 10.1016/s1054-139x(99)00070-1. [DOI] [PubMed] [Google Scholar]
- 44.Young T, Turner J, Denny G, Young M. Examining external and internal poverty as antecedents of teen pregnancy. Am J Health Behav. 2004;28:361–73. doi: 10.5993/ajhb.28.4.8. [DOI] [PubMed] [Google Scholar]
- 45.Crosby RA, Holtgrave DR. The protective value of social capital against teen pregnancy: a state-level analysis. J Adolesc Health. 2006;38:556–9. doi: 10.1016/j.jadohealth.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 46.Coard SI, Nitz K, Felice ME. Repeat pregnancy among urban adolescents: sociodemographic, family, and health factors. Adolescence. 2000;35:193–200. [PubMed] [Google Scholar]
- 47.Giedd JN, Blumenthal J, Jeffries NO, Castellanos FX, Liu H, Zijdenbos A, et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nature Neurosci. 1999;2:861–3. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- 48.Johnson SB, Blum RW, Giedd JN. Adolescent maturity and the brain: the promise and pitfalls of neuroscience research in adolescent health policy. Adolesc Health. 2009;45:216–21. doi: 10.1016/j.jadohealth.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Buhi ER, Goodson P, Neilands TB, Blunt H. Adolescent sexual abstinence: a test of an integrative theoretical framework. Health Educ Behav. 2011;38:63–79. doi: 10.1177/1090198110375036. [DOI] [PubMed] [Google Scholar]