Abstract
Objective
The Enhanced Comprehensive HIV Prevention Planning project was the first initiative of the Centers for Disease Control and Prevention (CDC) to address the goals of the National HIV/AIDS Strategy (NHAS). Health departments in 12 U.S. cities with a high prevalence of AIDS conducted comprehensive program planning and implemented cost-effective, scalable HIV prevention interventions that targeted high-risk populations. We examined trends in health department HIV prevention programs in these cities during the project.
Methods
We analyzed the number of people who received partner services, condoms distributed, and people tested for HIV, as well as funding allocations for selected HIV prevention programs by year and by site from October 2010 through September 2013. We assessed trends in the proportional change in services and allocations during the project period using generalized estimating equations. We also conducted thematic coding of program activities that targeted people living with HIV infection (PLWH).
Results
We found significant increases in funding allocations for HIV testing and condom distribution. All HIV partner services indicators, condom distribution, and HIV testing of African American and Hispanic/Latino populations significantly increased. HIV tests associated with a new diagnosis increased significantly among those self-identifying as Hispanic/Latino but significantly decreased among African Americans. For programs targeting PLWH, health department activities included implementing new program models, improving local data use, and building local capacity to enhance linkage to HIV medical care, retention in care, and treatment adherence.
Conclusions
Overall, these findings indicate that health departments in areas with a high burden of AIDS successfully shifted their HIV prevention resources to scale up important HIV programs and make progress toward NHAS goals.
The National HIV/AIDS Strategy (NHAS), established in 2010, set clear priorities for public health officials to refocus their response to human immunodeficiency virus (HIV) and realign prevention resources for high-impact prevention.1 Four main goals of the NHAS are to reduce new HIV infections, increase access to care and optimal health outcomes for people living with HIV infection (PLWH), reduce HIV-related health disparites, and achieve a more coordinated response to the HIV/acquired immunodeficiency syndrome (AIDS) epidemic. Health departments have an important role in NHAS implementation because they are responsible for implementing publicly funded prevention programs and making decisions about the optimal combination of programs for their jurisdictions.
In support of the NHAS, the U.S. Department of Health and Human Services provided funding to the Centers for Disease Control and Prevention (CDC) to implement the Enhanced Comprehensive HIV Prevention Planning (ECHPP) project (2010–2013) in 12 U.S. metropolitan statistical areas with a high prevalence of AIDS.2 Through the ECHPP project, health departments engaged in comprehensive planning to reprioritize their HIV-related activities across all funding sources and leverage existing resources to align programs with NHAS goals. Where appropriate, these health departments scaled up selected activities in their HIV prevention programs to attain NHAS goals for 2015.
We describe trends in HIV program funding allocations and services implemented by ECHPP-funded health departments during the ECHPP project period and after the release of the NHAS. We report data on program outcomes related to NHAS goals: partner services, condom distribution among high-risk populations, and HIV testing (to prevent new infections); HIV testing among African Americans and those self-identifying as Hispanic/Latino (to reduce HIV-related disparities); and linkage to HIV medical care, retention and reengagement in care, and treatment adherence (to increase access to care and improve health outcomes for PLWH).
METHODS
Twelve health departments participated in the ECHPP project: Chicago Department of Public Health (Chicago, Illinois); District of Columbia Department of Health (Washington, D.C.); Florida Department of Health (Miami, Florida); Georgia Department of Public Health (Atlanta, Georgia); Houston Health Department (Houston, Texas); Los Angeles County Department of Public Health (Los Angeles, California); Maryland Department of Health and Mental Hygiene (Baltimore, Maryland); New York City Department of Health and Mental Hygiene (New York, New York); Philadelphia Department of Public Health (Philadelphia, Pennsylvania); Puerto Rico Department of Health (San Juan, Puerto Rico); San Francisco Department of Public Health (San Francisco, California); and Texas Department of State Health Services (Dallas, Texas). We used the term ECHPP “site” for the geographic area in which the health department implemented its programs in its metropolitan statistical area. Four health departments implemented programs in their entire metropolitan statistical area; eight health departments implemented programs in selected counties in their metropolitan statistical area (according to disease burden and local resources).
Health department ECHPP plans included HIV testing in clinical and community settings, condom distribution among high-risk populations, and programs that targeted PLWH. Programs that targeted PLWH included HIV partner services (confidential, voluntary services to help PLWH notify their sex and drug-injecting partners of possible HIV exposure so partners can receive testing for HIV and sexually transmitted diseases [STDs] and related services), linkage to HIV medical care within three months of new diagnosis, retention and reengagement in HIV medical care for previously diagnosed people not in care, and treatment adherence activities. Details of the ECHPP project and its evaluation are provided in this issue of Public Health Reports.2,3
Data collection
The ECHPP project represents the first time that CDC requested that health department grantees consider their entire portfolio of HIV programs during project planning and implementation and report programmatic information for both CDC and non-CDC funding sources. Thus, no comparable data for the pre- or post-ECHPP years are available. Although comprehensive planning and integration of HIV prevention and HIV care activities by health departments have been encouraged by CDC and other federal agencies in recent years, data on integrated programs or programs funded by non-CDC sources are not routinely shared with CDC. Each ECHPP health department reported quantitative and qualitative data on programs and funding allocation annually to CDC using standardized ECHPP progress reports, unless otherwise noted. The Health Resources and Services Administration (HRSA) provided CDC with allocation data for Ryan White Part A Programs implemented by health departments in these metropolitan areas. Ryan White Part A Program -allocations are reported annually by the seven city or county ECHPP health departments and represent programs that target PLWH.4 For the five state ECHPP health departments, Part A allocations are allocations made by a local county health department that partnered with the state health department to conduct ECHPP activities. Allocation data for all other funding (i.e., other federal agency, state, local, or private sources) were submitted directly to CDC. Other federal agencies included the Substance Abuse and Mental Health Services Administration and the Department of Housing and Urban Development. Funding allocations were defined as the amount of money health departments planned to spend on ECHPP programs. Allocation data were used as a proxy for actual funds spent because data on actual expenditures were not available. Data on allocations and HIV testing data were reported by calendar year. Other data were reported by project year (i.e., year 1, October 2010–September 2011; year 2, October 2011–September 2012; and year 3, October 2012–September 2013).
Data on partner services reported in aggregate by health departments in progress reports included the following: the number of newly diagnosed HIV-positive people interviewed for partner services, the number of notified partners tested for HIV, the number of previously undiagnosed partners who tested HIV-positive, and the number of people who received their test results. Data on partner services for two sites (Atlanta and Los Angeles) were excluded from analysis because the local data systems could not distinguish between new and previously diagnosed HIV-positive people. Data on condom distribution reported in aggregate by health departments in progress reports included the number of condoms distributed when targeting high-risk populations at specific venues (i.e., distribution at venues frequented by PLWH and high-risk people who are HIV-negative or do not know their HIV status).
For each calendar year and each ECHPP site, we examined the number of HIV tests and number of HIV-positive tests that indicated a new diagnosis of HIV infection (hereinafter referred to as “newly diagnosed”), overall and separately for African Americans and those self-identifying as Hispanic/Latino. HIV testing data were obtained from two sources: CDC's National HIV Prevention Program Monitoring and Evaluation system for CDC-funded HIV testing5 and ECHPP progress reports for HIV testing activities funded by other sources. Using ZIP Code of testing venue, we extracted testing data for the 12 ECHPP sites from the National HIV Prevention Program Monitoring and Evaluation system, which included HIV testing data from all health department testing programs funded by CDC. Previous self-reported HIV test results and current HIV test results were used to calculate the number of newly diagnosed people (i.e., those who did not report a previous HIV-positive test). Six health departments reported data in aggregate on tests supported by other funding sources in progress reports (Washington, D.C., Houston, Los Angeles, New York, Philadelphia, and San Francisco). For all testing data for each year, we computed the percentage of tests resulting in a new HIV diagnosis (i.e., positivity). Health departments also described activities that enhanced linkage to care, retention or reengagement in care, and treatment adherence among PLWH in their progress reports.
Data analysis
We reviewed ECHPP plans and local objectives to identify health departments that planned to scale up program activities. To assess trends in allocations and program outcomes for all 12 ECHPP sites, we generated weights to treat each site equally. We assessed trends for numerators and not proportions (e.g., number of named partners tested instead of proportion of named partners tested) because we wanted to assess the extent to which these health departments scaled up their programs to increase the overall number of people reached. Weights serve to estimate the trend using data from each site equally without the results being disproportionately influenced by the few ECHPP sites that have higher populations of people at risk for and living with diagnosed HIV. For each outcome, weights were calculated by dividing the mean first-year value by the first-year value for each site. For example, a site with half the HIV tests during 2011 than the average would be assigned a weight of 2 to compensate for the smaller number of observations. We analyzed trends during the three years using generalized estimating equations with a negative binomial distribution,6 producing rate ratios (RRs). This test for trends assessed the average proportional change from 2011 to 2012 to 2013 for funding allocation and HIV testing data, and project year 1 to project year 2 to project year 3 data for all other data; it did not assess whether the total number increased or decreased. Empirical (robust) standard errors and 95% confidence intervals (CIs) were applied.7
Two ECHPP sites (New York and Washington, D.C.) participated in the HIV Prevention Trials Network (HPTN) 065 Study during our assessment. To account for the additional programmatic activities of HPTN 065, we assessed trends in partner services, condom distribution, and HIV testing after omitting data from these two sites from analysis. San Juan data on race/ethnicity were excluded from analyses because data were not uniformly available, and data on funding allocations, partner services, and condom distribution were excluded from analyses because final data were not available.
Two coders conducted a content analysis for linkage to care, retention or reengagement in care, and treatment adherence activities. Each coder reviewed progress reports for half of the health departments, summarized activities, and created broad activity categories. Next, they discussed all categories and agreed on a final set. We focused on the five most frequently reported activity categories for each intervention.
RESULTS
Among 11 ECHPP sites in 2010 (Table 1), 45% of PLWH were African American (range 13% in San Francisco to 78% in Baltimore) and 27% self-identified as Hispanic/Latino (range 3% in Baltimore to 41% in Los Angeles); African American and Hispanic/Latino participants constituted the majority of PLWH in all ECHPP sites except in San Francisco, where 62% of PLWH were white.
Table 1.
Adults and adolescents living with diagnosed HIV infection at year-end 2010, by race/ethnicity, 12 Enhanced Comprehensive HIV Prevention Planning project sitesa
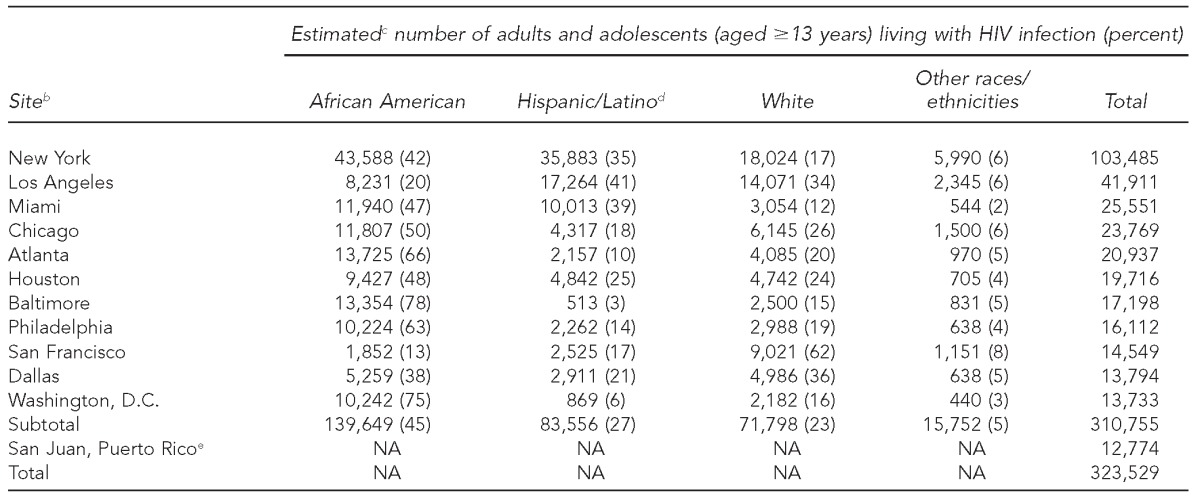
Data include people aged ≥13 years living with a diagnosed HIV infection, regardless of stage of disease at diagnosis, at year-end 2010, reported to the Centers for Disease Control and Prevention as of June 30, 2014. Age is based on the person's age as of December 31, 2010. Percentages may not total to 100 because of rounding.
bSites are listed in order of HIV prevalence (number of people living with a diagnosed HIV infection at year-end 2010), from high to low.
cEstimated numbers resulted from statistical adjustment that accounted for reporting delays but not for incomplete reporting.
dHispanic/Latino people can be of any race.
eRace/ethnicity data are not provided for San Juan, Puerto Rico, because these data were not uniformly available.
HIV = human immunodeficiency virus
NA = not available
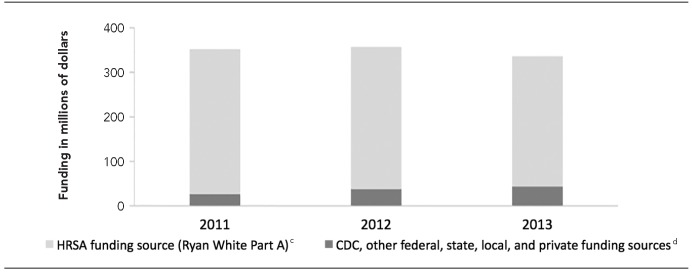
Among 11 ECHPP sites from 2011 to 2013, HIV testing allocations increased from $45.2 million to $59.0 million (RR=1.29; 95% CI 1.07, 1.55), and allocations for condom distribution to high-risk groups increased from $2.7 million to $3.8 million (RR=1.81; 95% CI 1.53, 2.14). Overall allocations for programs that target PLWH did not significantly change (Figure). However, Ryan White Part A Program funding allocations decreased from $325.1 million to $292.8 million (RR=0.97; 95% CI 0.94, 0.99), and other allocations for programs that target PLWH (e.g., HIV partner services programs, activities that connect clients to HIV medical care) increased from $26.8 million to $43.5 million (RR=1.36; 95% CI 1.14, 1.61).
Figure.
Health department funding allocationsa for programs that target people living with HIV infection, 11 Enhanced Comprehensive HIV Prevention Planning project sites,b January 2011–January 2013
aThe HRSA Funding Source (Ryan White Part A) data were provided by HRSA to CDC. The CDC, other federal, state, local, and private funding sources were reported to CDC by Enhanced Comprehensive HIV Prevention Planning (ECHPP) grantees through ECHPP grantee progress reports.
bThe sites were located in Chicago, Illinois; Washington, D.C.; Miami, Florida; Atlanta, Georgia; Houston, Texas; Los Angeles, California; Baltimore, Maryland; New York, New York; Philadelphia, Pennsylvania; San Francisco, California; and Dallas, Texas. San Juan, Puerto Rico, was excluded because of missing data.
cStatistically significant trend, p=0.01
dStatistically significant trend, p<0.001
HIV = human immunodeficiency virus
HRSA = Health Resources and Services Administration
CDC = Centers for Disease Control and Prevention
Trends for all indicators for partner services from year 1 to year 3 were significant for the nine sites included in analysis (Table 2). The number of people newly diagnosed with HIV interviewed for partner services increased from 3,294 to 5,063 (RR=1.70; 95% CI 1.29, 2.24). The number of named partners tested increased from 1,664 to 1,778 (RR=1.27; 95% CI 1.15, 1.40). The number of newly diagnosed HIV-positive partners who received their test results increased from 117 to 195 (RR=1.68; 95% CI 1.14, 2.47). The number of condoms distributed also increased from 19,159,054 to 41,708,387 (RR=2.24; 95% CI 1.89, 2.67).
Table 2.
Number of people newly diagnosed with HIV and interviewed for partner services, named partners tested for HIV, and newly diagnosed HIV-positive partners who received their test results, Enhanced Comprehensive HIV Prevention Planning (ECHPP) project sites,a October 2010–September 2013
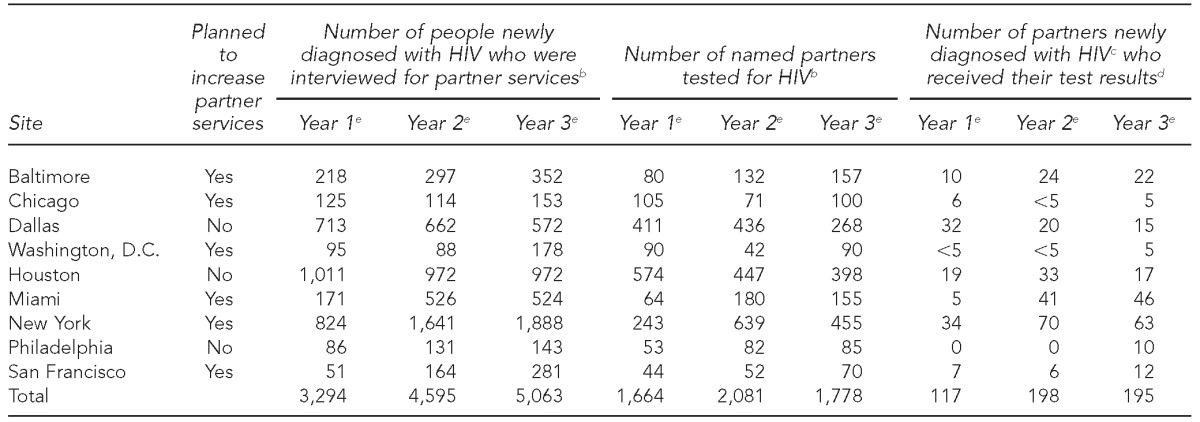
Three sites (Atlanta, Los Angeles, and San Juan, Puerto Rico) were excluded from analysis; Atlanta and Los Angeles lacked data on the number of newly diagnosed people interviewed for partner services, and San Juan lacked final data. Data were obtained from ECHPP grantee progress reports.
bSignificant trend during three years, p<0.001
cAcross these nine sites, among those tested for HIV, the number of partners who were newly diagnosed with HIV was 145 (9%) in year 1, 214 (10%) in year 2, and 202 (11%) in year 3.
dSignificant trend during three years, p=0.009
eReporting periods represent ECHPP project years: year 1, October 1, 2010–September 30, 2011; year 2, October 1, 2011–September 30, 2012; and year 3, October 1, 2012–September 30, 2013.
HIV = human immunodeficiency virus
Overall HIV testing trends were not significant (Table 3). A total of 1,018,135 HIV tests were conducted in 2011 and 1,135,421 HIV tests were conducted in 2013. People newly diagnosed with HIV through testing events totaled 7,474 in 2011 and 7,053 in 2013. The number of HIV tests among African Americans increased from 494,849 to 524,057 (RR=1.04; 95% CI 1.01, 1.07) from 2011 to 2013, but the number of African Americans who were newly diagnosed decreased from 3,917 to 3,627 (RR=0.94; 95% CI 0.90, 0.98). The number of HIV tests among those self-identifying as Hispanic/Latino increased from 287,848 to 309,497 (RR=1.10; 95% CI 1.03, 1.17) during this time period. Although the trend for newly diagnosed Hispanic/Latino participants increased (RR=1.15; 95% CI 1.04, 1.28), the number of newly diagnosed Hispanic/Latino participants decreased slightly, from 1,770 in 2011 to 1,692 in 2013. This discrepancy occurred because the trend test assessed average proportional change for all sites, rather than change in the number.
Table 3.
Number of HIV tests and people newly diagnosed with HIV, Enhanced Comprehensive HIV Prevention Planning project sites, January 2011–December 2013
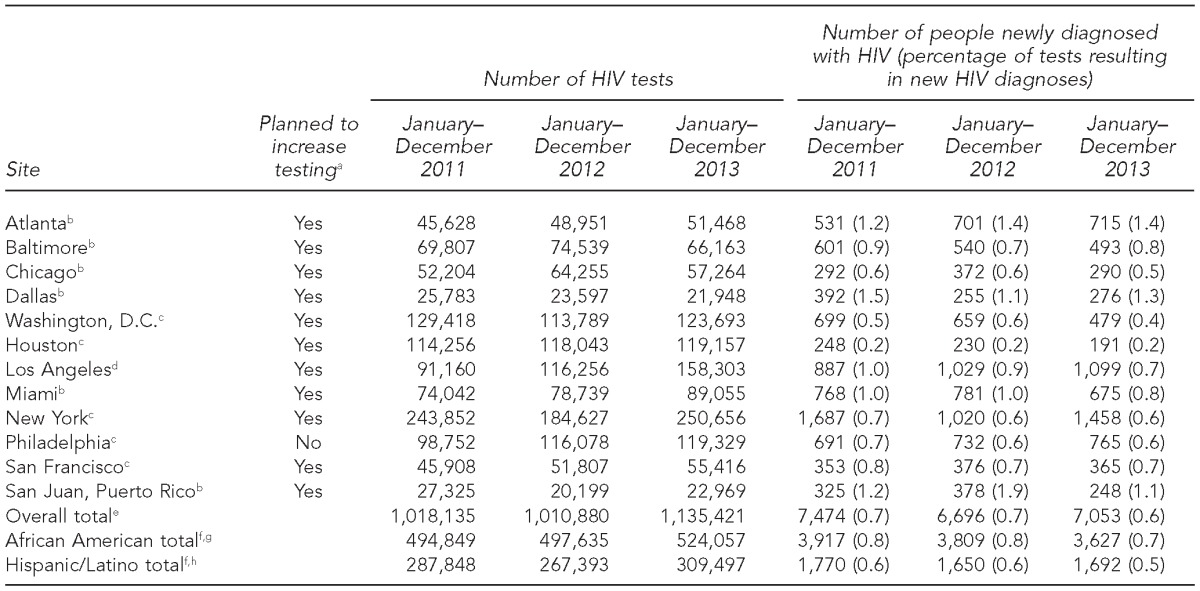
aPlanned to increase their HIV testing activities or increase the number of newly diagnosed HIV-positive people found through testing
bCDC-funded tests only
cBoth CDC-funded tests and tests funded by other sources (i.e., other federal, state, local, or private funds)
dFor Los Angeles, CDC-funded tests only are reported for 2011 and 2012. Both CDC-funded tests and privately funded tests are reported for 2013. In 2013, 59 of the 1,099 newly identified HIV-positive test results in Los Angeles represented newly diagnosed confirmed HIV-positive tests only (preliminary HIV-positive tests not included).
eTrend results for overall totals were not significant: number of HIV tests (p=0.47), number of people newly diagnosed with HIV (p=0.12)
fSan Juan, Puerto Rico, data were excluded from racial/ethnic totals because most HIV testing in San Juan is conducted among Hispanic/Latino people.
gSignificant increasing trend for number of HIV tests (p=0.008); significant decreasing trend for number of people newly diagnosed with HIV (p=0.009)
hSignificant increasing trends for number of HIV tests (p=0.004) and number of people newly diagnosed with HIV (p=0.009)
HIV = human immunodeficiency virus
CDC = Centers for Disease Control and Prevention
After removing data for New York and Washington, D.C., from our analysis because of the cities' participation in HPTN 065, the direction and significance of our results did not change. We also report on the top five most frequently reported activities for linkage to care, retention or reengagement in care, and treatment adherence activities (Table 4).
Table 4.
The top five most frequently reported activities for each of three interventions, 12 Enhanced Comprehensive HIV Prevention Planning project sites,a October 2010–September 2013
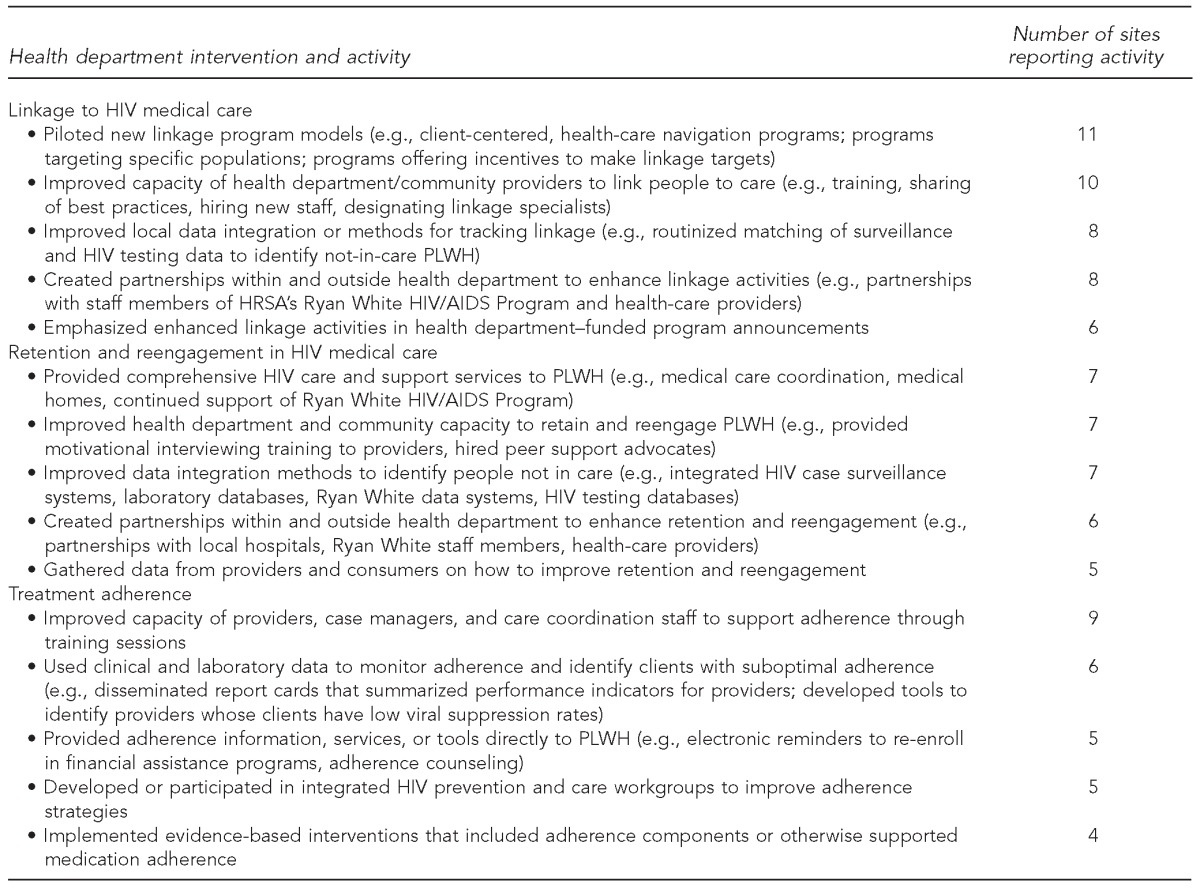
The sites were located in Chicago, Illinois; Washington, D.C.; Miami, Florida; Atlanta, Georgia; Houston, Texas; Los Angeles, California; Baltimore, Maryland; New York, New York; Philadelphia, Pennsylvania; San Juan, Puerto Rico; San Francisco, California; and Dallas, Texas.
HIV = human immunodeficiency virus
PLWH = people living with HIV infection
HRSA = Health Resources and Services Administration
AIDS = acquired immunodeficiency syndrome
DISCUSSION
The ECHPP project was the first CDC initiative to support health department implementation of NHAS and encourage high-impact prevention in areas with a high prevalence of AIDS. Funding allocation trends for 2011–2013 showed that health departments in 12 U.S. cities with the highest HIV burden increased program dollars to support HIV testing, condom distribution, and non-Ryan White Part A Programs that target PLWH. Trends showed that these health departments supported the goal to reduce new HIV infections by increasing the number of people served by partner services and condom distribution programs. Health departments supported the goal to reduce HIV-related disparities by increasing testing of African American and Hispanic/Latino populations. In support of improving service access and health outcomes for PLWH, health departments piloted new program models and enhanced their infrastructure, capacity, local partnerships, and data use, which should ultimately improve outcomes related to linkage, retention in care, and treatment adherence.
HIV partner services and condom distribution programs are important strategies to reduce new HIV infections.8,9 During the ECHPP project, all indicators of partner services increased, suggesting overall success at these health departments in expansion of services, program integration, building of staff capacity, and new partnerships. However, not all health departments reported increases for all indicators, which may reflect differences in local priorities and resources. The number of condoms distributed to PLWH and high-risk populations doubled from the first year to the last year of the ECHPP project, and nine sites reported increasing distribution. This shift is supported by evidence that shows condom distribution programs to be cost-effective, cost saving,9 and perhaps easier to implement than other programs.
Although these data do not directly address racial/ethnic disparities in HIV testing, the increased testing of African Americans and those self-identifying as Hispanic/Latino suggests that health department testing programs in high-burden areas are increasing their reach among racial/ethnic minority groups and increasing the proportion of people who know their status. An increasing trend in newly diagnosed people self-identifying as Hispanic/Latino is an important finding because this group is the largest ethnic minority population in the United States; although they comprise 16% of the population,10 they account for 21% of new HIV diagnoses.11 We found an overall decrease in new diagnoses among African Americans; several reasons may explain this decrease. HIV incidence among African American women has decreased in recent years (by 21% from 2008 to 201012) and, in some communities, incidence could be decreasing among men as well. We found increases in the number of newly diagnosed African Americans in some ECHPP sites but not in others; differences in local targeting efforts or levels of HIV infection in these communities may explain this variation. Nationally, the percentage of HIV-infected African Americans who are unaware of their HIV infection is decreasing,13 suggesting that current testing strategies are generally successful. However, more innovative strategies may be needed to reach the small percentage of African Americans who are still unaware of their HIV infection.
Our qualitative findings indicate these health departments are devoting considerable effort to implementing activities that support linkage, retention and reengagement in care, and medication adherence. Their programmatic strategies may serve as models for jurisdictions with a low or medium burden of HIV/AIDS; the health departments in these jurisdictions may need more time to scale up services to reach NHAS goals. The total number of PLWH in the ECHPP sites who have been linked and retained in care during the project period are not yet available from CDC's National HIV Surveillance System.14 However, health departments can compute these indicators by using their local surveillance data to assess the extent to which they are improving continuum-of-care outcomes.
At the start of the ECHPP project, health departments conducted a local analysis to identify service gaps and develop strategies to increase coordination of services, realign resources, and increase local impact, using existing resources where possible. CDC's largest HIV prevention cooperative agreement and HRSA's overall Ryan White HIV/AIDS Program represent a substantial proportion of health departments' existing resources and, thus, influence prevention program activity. Beginning in 2012, CDC required all CDC-funded health department grantees to direct 75% of their flagship funds to core HIV prevention programs—HIV testing, condom distribution among high-risk populations, programs that target PLWH, and policy and structural interventions.15 This change was the first time that CDC's flagship program required that dollars be allocated to programs that target PLWH. HRSA's Ryan White HIV/AIDS Program supports most of the publicly funded programs for PLWH, such as case management, pharmaceutical financial assistance, and treatment adherence counseling.4 Our findings indicate that some prevention programs, such as testing and condom distribution, can be scaled up with existing federal resources, but additional information is needed to understand how local resources can support scale-up of programs that target PLWH.
Many ECHPP plans involved development of new data systems, statistical modeling to identify optimal program combinations, creation of new partnerships, and implementation of new data and program protocols, all of which can be time-consuming and costly.2 Despite this investment, these health departments increased service delivery of important HIV prevention programs. Overall allocations for programs targeting PLWH were relatively flat from 2011 to 2013, despite growing emphasis at different levels of public health on “prevention for positives” and “treatment as prevention.” Total Ryan White HIV/AIDS Program awards decreased during this time period,16 which could have limited health departments' ability to increase allocations. On the other hand, some health departments reported leveraging other federal resources (e.g., Medicaid) to pay for programs and offset a decrease in funds. Also, additional monies may not have been needed if the number of new infections in the jurisdiction was declining or if the health department successfully shifted to higher-impact programs or policies at no additional cost.
Limitations
Several limitations should be noted. First, without additional years of data (for pre- and post-ECHPP periods) and without data from non-ECHPP comparison sites, it was difficult to draw inferences about the extent to which the ECHPP project contributed to the trends. However, because the ECHPP project focused on planning initially, we would expect some increase in services as sites began to implement new ECHPP strategies and program models. Second, although the overarching project goals were the same, local objectives, priorities, and program implementation varied. Thus, program scale-up may look different across cities, and broad interpretations about why trends exist should be limited. Third, causal inferences about the ECHPP project or any specific program and its impact are not appropriate, because results summarize programs funded across different sources, and other initiatives implemented during these years may have influenced findings. Fourth, the number of newly diagnosed people may be overestimated given that HIV testing program data, which rely on self-report rather than HIV case surveillance data, were analyzed. Finally, although the increasing trends are believed to be due to a true scale-up in services, changes in data systems could have contributed to some trends.
CONCLUSION
Overall, these data support the conclusion that ECHPP jurisdictions implemented large-scale shifts in HIV prevention programs to meet NHAS goals.
Footnotes
The authors acknowledge the hard work and commitment of the following members of the Enhanced Comprehensive HIV Prevention Planning Project team: David Amarathithada, Nanette Benbow, Debra Janiszewski, Griselle Torres, and Fikirte Wagaw (Chicago Department of Public Health); Michael Kharfen, Nestor Rocha, Benjamin Takai, and Tiffany West (District of Columbia Department of Health); Darline Candio, April Hogan, Marlene LaLota, Tamara McElroy, Janelle Taveras, Kira Villamizar, and Max Wilson (Florida Department of Health); Donato Clarke, Melanie Durley, William Lyons, Twalla Marshall, Leisha McKinley-Beach, and Vivian Momah (Georgia Department of Public Health); Hickmon Friday, Marlene McNeese, and Cathy Wiley (Houston Health Department); John Mesta, Mario J. Pérez, Jacqueline Rurangirwa, and Jennifer Sayles (Los Angeles County Department of Public Health); Hope Stewart-Cassidy, Claudia Gray, and Heather Hauck (Maryland Department of Health and Mental Hygiene); Blayne Cutler, Nana Mensah, Julie Myers, and Monica Sweeney (New York City Department of Health and Mental Hygiene); David Acosta, Jane Baker, Matthew McClain, Amy Nunn, Brad Shannon, and Coleman Terrell (Philadelphia Department of Public Health); Caroline Maldonado, Sandra Miranda de Leon, and Margaret Wolfe (Puerto Rico Department of Health); Grant Colfax, Moupali Das, Dara Geckeler, Nick Moss, Israel Nieves-Rivera, and Tracey Packer (San Francisco Department of Public Health); Donci Bardash, Jeff Hitt, Chris Mobley, and Ann Robbins (Texas Department of State Health Services); and Donna Alexander, Angie Alvarado-Cordero, Maria Ayala-Perales, Lisa Belcher, Janet Blair, Jeffrey Brock, Jim Carey, Stephanie Celestain, Pollyanna Chavez, Cari Courtenay-Quirk, Ken Dominguez, Frank Ebagua, Agatha Eke, Renata Ellington, Holly Fisher, Stephen Flores, Carla Galindo, Lytt Gardner, Cindy Getty, Marlene Glassman, Tamika Hoyte, Rhondette Jones, David Knapp Whittier, Andrew Margolis, Tricia Martin, DaDera Moore, Jasmin Minaya, Mary Spink Neumann, Angel Ortiz-Ricard, Stanley Phillip, Cynthia Prather, David Purcell, Shuenae Smith, Phyllis Stoll, Dale Stratford, Robert Swayzer, Eboni Taylor, Raekiela Taylor, Peter Thomas, Vasavi Thomas, and Melissa Thomas-Proctor (Centers for Disease Control and Prevention [CDC]). The authors also thank the members of CDC's Division of HIV/AIDS Prevention Steering Committee: Maria Alvarez, April Bankston, Janet Cleveland, Samuel Dooley, Erica Dunbar, Linda Koenig, Amy Lansky, Cynthia Lyles, Barbara Maciak, June Mayfield, Jonathan Mermin, Dale Stratford, Gary Uhl, and Rich Wolitski.
Portions of this manuscript (preliminary data) were presented at the 2014 U.S. Conference on AIDS Annual Meeting, San Diego, California, October 2–5, 2014. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.The White House (US), Office of National AIDS Policy. National HIV/AIDS strategy. 2010 [cited 2015 Jul 6] Available from: https://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf.
- 2.Flores SA, Purcell DW, Fisher HH, Belcher L, Carey JW, Courtenay-Quirk C, et al. Shifting resources and focus to meet the goals of the National HIV/AIDS Strategy: the Enhanced Comprehensive HIV Prevention Planning project, 2010–2013. Public Health Rep. 2016;131:52–8. doi: 10.1177/003335491613100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fisher HH, Hoyte T, Flores SA, Purcell DW, Dunbar E. Stratford D, Evaluation framework for HIV prevention and care activities in the Enhanced Comprehensive HIV Prevention Planning project, 2010–2013. Public Health Rep. 2016;131:67–75. doi: 10.1177/003335491613100113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Health Resources and Services Administration (US) Ryan White HIV/AIDS Program [cited 2015 Jul 6] Available from: http://hab.hrsa.gov/abouthab/aboutprogram.html.
- 5.Centers for Disease Control and Prevention (US) National HIV Prevention Program Monitoring and Evaluation System [cited 2015 Sep 9] Available from: http://www.cdc.gov/hiv/statistics/surveillance/index.html.
- 6.Gardner WI, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol Bull. 1995;118:392–404. doi: 10.1037/0033-2909.118.3.392. [DOI] [PubMed] [Google Scholar]
- 7.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 8.Hogben M, McNally T, McPheeters M, Hutchinson AB. The effectiveness of HIV partner counseling and referral services in increasing identification of HIV-positive individuals: a systematic review. Am J Prev Med. 2007;33(2 Suppl):S89–100. doi: 10.1016/j.amepre.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Cohen DA, Farley TA, Bedimo-Etame JR, Scribner R, Ward W, Kendall C, et al. Implementation of condom social marketing in Louisiana, 1993 to 1996. Am J Public Health. 1999;89:204–8. doi: 10.2105/ajph.89.2.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Census Bureau (US) The Hispanic population: 2010 [cited 2015 Jul 6] Available from: http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf.
- 11.Centers for Disease Control and Prevention (US) HIV surveillance report, 2013; vol. 25 [cited 2015 Jul 6] Available from: http://www.cdc.gov/hiv/library/reports/surveillance/2013/surveillance_report_vol_25.html.
- 12.Lansky A, Hall I, Mermin J. Declining HIV incidence among women in the United States. Women's Health Issues. 2014;24:581–3. doi: 10.1016/j.whi.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (US) Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2013. HIV Surveillance Supplemental Report [cited 2015 Jul 13] Available from: http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillancereport_vol20_no2.pdf.
- 14.Centers for Disease Control and Prevention (US) National HIV Surveillance System [cited 2015 Jul 6] Available from: http://www.cdc.gov/hiv/statistics/surveillance/index.html.
- 15.Centers for Disease Control and Prevention (US) Funding opportunity announcement (FOA) PS12-1201: comprehensive human immunodeficiency virus (HIV) prevention programs for health departments [cited 2015 Jul 6] Available from: http://www.cdc.gov/hiv/policies/funding/announcements/PS12-1201/index.html.
- 16.The AIDS Institute. The AIDS Institute Ryan White award analysis 2011–2013 [cited 2015 Jul 6] Available from: http://www.theaidsinstitute.org/sites/default/files/attachments/All%20Ryan%20White%20HH%20Analysis%20Graphs.pdf.