Abstract
Bone fracture resistance is determined by the amount of bone present (“bone quantity”) and by a number of other geometric and material factors grouped under the term “bone quality.” In May 2013, a workshop was convened among a group of clinicians and basic science investigators to review the current state of the art in Bone Quality and Fracture Prevention and to make recommendations for future directions for research. The AAOS/ORS/OREF workshop was attended by 64 participants, including two representatives of the National Institutes of Arthritis and Musculoskeletal and Skin Diseases and 13 new investigators whose posters stimulated additional interest. A key outcome of the workshop was a set of recommendations regarding clinically relevant aspects of both bone quality and quantity that clinicians can use to inform decisions about patient care and management. The common theme of these recommendations was the need for more education of clinicians in areas of bone quality and for basic science studies to address specific topics of pathophysiology, diagnosis, prevention, and treatment of altered bone quality. In this report, the organizers with the assistance of the speakers and other attendees highlight the major findings of the meeting that justify the recommendations and needs for this field.
Keywords: bone quality, fragility fracture, fracture prevention, workshop
In May, 2013, the AAOS, OREF, and ORS convened a group of basic scientists and clinicians to review the current understanding of bone quality and to create a dialogue between basic scientists and clinicians about the significance of bone quality parameters and their affect on patient management. The meeting combined sessions with breakout groups to define future research directions (Table 1). This report summarizes the findings with suggestions for future basic science and clinical research.
Table 1.
Recommendations for Bone Quality Studies
| Goal | Recommendations |
|---|---|
| Improving understanding of the pathophysiology of altered bone quality | Plan more comprehensive studies. Use collaborators to increase breadth and minimize narrowly focused studies. Subgroup patients by disease type to assess pathophysiology of different conditions leading to fracture |
| Improve access to rare samples by expanding existing registries and developing new registries | |
| Improve access to normal human controls (for comparison with age-matched specimens of altered bone quality) by partnering with trauma centers or medical examiners | |
| Improving diagnosis of altered bone quality | In patients at high risk for or with history of fragility fracture, consider bone biopsy in addition to DEXA, labs, FRAX. Biopsy allows direct assessment of histology and tissue properties, and assessment of treatment outcomes |
| Noninvasive finite element modeling studies based on patient-specific imaging data can be used to complement studies of bone matrix properties | |
| Improving prevention of fragility fractures in patients with altered bone quality | Educate providers and patients about the risk of fragility fractures |
| Communicate relative risks and benefits of preventive drug treatment to patients at high risk of fragility fracture to increase patient acceptance of pharmaceutical intervention | |
| Improving treatment of altered bone quality | Utilize non-rodent animal models exhibiting intracortical remodeling to examine the effects of drug treatments on the bone matrix and to optimize combination therapy and drug holidays |
| Address lost opportunities from current drug trials: implement longer-term tracking of participants and incident follow-up; incentivize sharing of data with academia |
Session I: Bone Quality: What is It? (Presenters: Eve Donnelly, PhD; Joseph M. Lane, MD)
Bone fracture resistance is determined by bone quantity and bone quality, defined broadly as all geometric, microarchitectural, and material factors (e.g., trabecular architecture, collagen crosslinking, mineralization, microcracks) that contribute to whole-bone fracture resistance.1 Bone mineral density (BMD, g/cm2), clinically determined by dual photon absorptiometry (DXA), provides a combined measure of quantity and quality, because areal BMD (aBMD) cannot distinguish between thicker bones (greater quantity) and more highly mineralized bones (altered quality). BMD assessed by DXA has moderate ability to predict fracture risk in untreated patients and to predict the reduction in risk in patients treated with antiresorptive therapies.2 In addition, fracture risk increases with age independently of BMD.3 These examples suggest that bone quality factors in addition to BMD contribute to fracture risk. For example, changes in collagen structure and advanced glycation end products (AGEs) that increase with age4 may contribute to age-related changes in fracture risk. Bisphosphonates alter tissue composition and decrease the heterogeneity of the collagen matrix and the mineral crystallinity,5 which may make bone stiffer and stronger but more brittle over time. Clinicians prescribing therapeutic regimens will benefit from understanding how to modulate bone turnover using existing and new bone-active agents to restore the trabecular network and tissue compositional heterogeneity and to limit AGEs.
Clinically, individuals with osteoporotic fragility fractures, for example, low energy fractures that occur from a standing height or less, must be distinguished from individuals with low BMD-associated diseases other than osteoporosis. A major clinical challenge is identifying the subset of osteoporotic patients with low BMD who require treatment. Conversely, patients with Paget’s disease, osteopetrosis, early Cushing’s syndrome, and osteogenesis imperfecta all fracture, but in these cases bone quality, not bone density, are abnormal. Thus, appropriately addressing the full spectrum of clinical bone disorders requires a thorough understanding of bone quality.
Session II: Contributions of Microarchitecture and Microstructure to Bone Quality (Presenters: Karl Jepsen, PhD; Adele Boskey, PhD; Deepak Vashishth, PhD; Christopher Hernandez, PhD; Oran Kennedy, PhD)
Advances in diagnostic and treatment regimens to reduce fracture incidence will benefit from a better understanding of how bone morphology and tissue quality together define whole-bone mechanical properties. These measures include commonly reported properties such as stiffness and failure load, and more complex properties such as toughness, creep, and fatigue life.6,7 Not all bones are constructed the same way; the same tissue-level matrix constituents exist in everyone’s bones, but they vary in morphology. Though slight, these variations are clinically meaningful. Bone “robustness,” a measure of transverse size relative to length, varies among individuals and parallels increases in porosity.8 Whole-bone stiffness increases with the 4th power of bone diameter, and increases in diameter are accompanied by concomitant variations in mineralization and porosity so that tissue-level stiffness (modulus) is greatest in slender bones and lowest in the wider robust bones. The slender bones achieve high tissue-level stiffness (which contributes to whole-bone stiffness) by limiting turnover, which may come at the expense of reduced toughness. The effects of these natural variations in tissue-level material properties and geometry on clinical measures such as BMD are unknown.
Remodeling is the primary process that modifies bone volume and structure in adults. Bone remodeling is responsible for removing and replacing old or damaged bone tissue from the skeleton. The amount of remodeling throughout the skeleton can be measured by blood and urinary markers that can predict fracture risk independent of measures of bone size and mass, suggesting that remodeling itself influences fracture risk. Remodeling creates microscale cavities in bone, which can lead to microdamage, and the size of these cavities is altered by anti-osteoporotic therapies.9,10
Bone mineral is an important contributor not only to bone quantity, but also to quality, for example, tissue composition and crystal size. Bone composition varies with age, health, and disease, as well as pharmacologic therapies. Spectroscopic methods have sufficient resolution to describe microscale heterogeneity in composition, which is decreased by bisphosphonate treatment.5 This decrease may ease propagation of microcracks that contribute to fracture.
The collagen network is another contributor to quality, providing toughness and fracture resistance. The crosslinks stabilizing the collagen vary in composition with aging, disease, and drug therapies. Bone contains two types of collagen crosslinks, those that form enzymatically through the action of lysyl oxidase and those that form non-enzymatically as the result of glycation of the protein,4 the AGEs. The accumulation of AGEs is associated with increased fracture risk.11
Associated with the collagen network are noncollagenous proteins (NCPs) that also vary in amount and expression with age, disease, and treatment.12 Animal studies in which an NCP is knocked out or in provide insight into the function of NCPs. However, only for dentin matrix protein-1, a major product of osteocytes, has a human disease, hypophosphatemic rickets, been linked to a mutation in any of these proteins.13 The fibromodulin/biglycan double knockout mouse14 has a severe osteoporotic phenotype, and could provide a good model for assessing therapies for osteoporosis.
The contribution of microdamage accumulation in the extracellular matrix to the reduction of fracture resistance is challenging to assess, but several important variables have been evaluated. Damage increases with age and varies with tissue aging. Bone can sustain small areas of damage, which helps dissipate energy and make further propagation of that damage difficult. Bone remodeling is responsible for removing and replacing damaged tissue. The relevance of this issue becomes clinically evident when the remodeling process is suppressed, such as with the use of bisphosphonates.15 Bisphosphonates reduce fracture risk; however, many animal and two postmortem studies showed that microdamage accumulation occurred when bone remodeling was inhibited.16,17 Furthermore, toughness is reduced with bisphosphonate treatment.18
Session III: Noninvasive Assessment of Bone Quality (Presenters: Eve Donnelly, PhD; Sharmilla Majumdar, PhD; X. Sherry Liu, PhD; X. Edward Guo, PhD; Brian Snyder, MD, PhD)
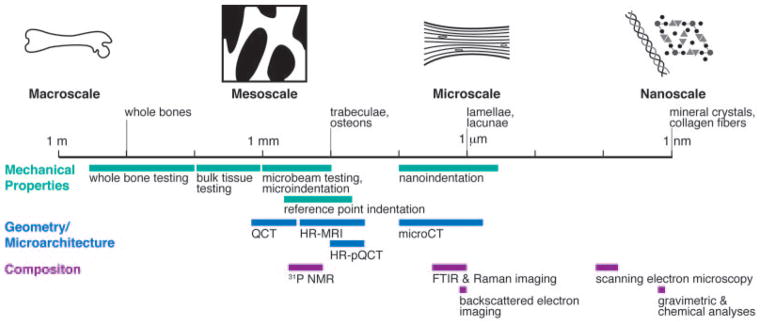
Noninvasive methods for characterizing bone geometry and microarchitecture include quantitative CT, high resolution peripheral quantitative CT (HR-pQCT), high resolution MRI and microCT (Fig. 1). Outcomes include 3D whole-bone geometry and trabecular morphology. Advantages include the ability to make many geometric measurements in clinical scanners; disadvantages include the ability to image only superficial and peripheral sites. Noninvasive methods for measuring tissue composition include in vivo Raman spectroscopy and nuclear magnetic resonance imaging and spectroscopy. Outcomes include mineral density, crystallinity, and bone water content. Advantages of these methods include detailed material characterization; disadvantages include long acquisition times Instrumented gait analysis and finite element (FE) analysis are noninvasive methods for assessing loading, but noninvasive assessment of the load-carrying capacity of bone in different individuals remains an critical unsolved problem.
Figure 1.
Hierarchical structure of bone depicted schematically on a logarithmic scale. Techniques for mechanical (dark gray bars), geometric/microarchitectural (medium gray bars), and compositional (light gray bars) are shown according to their approximate length scale of analysis. (QCT = quantitative computed tomography, HR-MRI = high-resolution magnetic resonance imaging, pQCT = peripher-al QCT, NMR = nuclear magnetic resonance imaging, FTIR = Fourier transform infrared). Adapted with permission from Donnelly.56
High resolution MRI is technically demanding and often expensive in assessing bone quality, but with a resolution of 190 μm, trabecular distribution and connectivity can be assessed.19 Newer technology and higher field strength will reduce imaging time and permit imaging sites such as the proximal femur. The marrow surrounding the trabecular bone, when imaged at high resolution, provides structural details that can be compared with measurements from other modalities.
HR-pQCT yields 3D measurements of geometric parameters and cortical and trabecular microarchitecture that correlate with bone strength. HR-pQCT also achieves sufficient resolution for generation of FE meshes to create models to assess bone strength, enabling prediction of failure loads.20 HR-pQCT is the only clinical CT modality that provides in vivo 3D microarchitectural imaging with an effective dose equivalent <1/100 of yearly natural background radiation dose.
Computational methods can be used for noninvasive prediction of structural properties such as whole-bone stiffness and strength. CT-based rigidity analysis predicts fracture risk in bones with osteolytic metastases more accurately than current clinical or radiographic algorithms based on symptoms, anatomic locations of the fracture, and the lesion size and location. The moment of inertia of the least rigid cross section through a beam of cancellous bone with a lytic defect is better correlated with the beam’s load-bearing capacity than the average material or geometric properties of the entire beam. In patients with meta-static cancer of the appendicular skeleton, pain was the most important clinical factor influencing the initial treatment plan; treatment was significantly benefited by including CT-based rigidity analysis of the fracture risk.21
Finite element analysis (FEA) is a computational method for solving engineering mechanics problems. Carefully constructed FE models provide precise predictions of stiffness and strength of structures with complex geometry, including whole bones or cancellous biopsies. Advanced 3D imaging modalities such as QCT-based FEA22 allow development of patient-specific models for determining bone structural properties. An advantage of these computational techniques is that the effects of altered bone quality on structural properties can be explored by varying the material properties assigned to each voxel.
Session IV: Animal Models of Altered Bone Quality (Presenters: Peter Byers, MD; Cliff Rosen, MD, Mark Johnson, PhD; Eileen Shore, PhD)
Understanding human bone quality requires better knowledge of how bone is made, turned over, and removed; thus animal models are needed to provide information about the causes of altered bone quality in humans and to enable investigation of the effects of therapies on bone quality (Table 2). For example, osteogenesis imperfecta (OI) is mostly due to defects in type I collagen synthesis or processing.23 In humans, heterozygous mutations in three genes (COL1A1, COL1A2, and intermembrane inducible protein 5) give rise to dominantly inherited forms of OI mutations in type I collagen genes and account for ~95% of all mutations recognized. The most common form, OI type I (mild), is modeled by the MOV13 mouse (Table 2), while type IV OI (moderately severe) is modeled by the Brtl mouse. The most studied mouse model of OI is the oim/oim mouse, which is homozygous for a frameshift deletion in COL1A2 (Table 2). Only two patients worldwide are reported with this mutation, yet this model is used for a large number of pre-clinical studies because its phenotype is highly reproducible. Recent studies examining the toughness of oim/oim and oim/+ bone suggest that the oim/oim bones lose toughness due to a decrease in stabilizing enzymatic crosslinks and an increase in non-enzymatic crosslinks.24 At the tissue level, high vascular canal density reduces the stable crack growth phase, and extensive woven bone limits crack-deflection toughening during crack growth in oim/oim animals. The important lesson from these studies of multiple OI mouse models is that the same phenotype can exist for different mutations.
Table 2.
Mouse and Rat Models of Altered Bone Quality
| Human Disease | Mouse Phenotype | Basis for Phenotype | Ref |
|---|---|---|---|
| Osteogenesis Imperfecta | Brittle bones altered mineralization | Several models with defects in type I collagen genes or genes for processing molecules, for example: MOV13: heterozygous null mutations in COL1A1 oim/oim: homozygous for a frameshift deletion in COL1A2, leading to a failure to integrate the protein into the procollagen trimer Brtl: targeted substitution of a glycine by cysteine in the triple helical domain Cartilage associated protein knockouts provide models of type VII OI |
23 |
| Osteopetrosis | High bone mass/altered osteoclast function | Knockouts of: c-SRC, cathepsin K, carbonic anhydrase II, CLCN7, Ostm1 Naturally occurring mutants: oc/oc and grey lethal mice, ia/ia rat |
26 |
| High bone mass | Increased bone mass | Knockouts of: Sclerostin, glycogen synthase kinase 3beta; secreted Frizzled-related protein 1; Dickkopf 1; myostatin | 27 |
| Low bone mass | Decreased bone formation | WNT-signaling protein knockouts; biglycan knockout | 28 |
| Osteoporosis | Decreased bone density | Fibromodulin/biglycan double knockout | 14 |
| Hypophosphatemic rickets | Poorly mineralized bone | Dentin matrix protein-1 knockout | 13 |
Naturally occurring inbred mouse strains are evolving into models for bone mass and strength. More than a dozen strains have been phenotyped for macro- and micro-architectural traits that are heritable and can be mapped through various genetic strategies. Differences may occur by strain (e.g., C3H has high bone mass, DBA low bone mass) or by sex. Recently the “collaborative cross” developed >150 strains and >300 inbred lines from 8 founder lines,25 capturing 90% of the genetic variation in the mouse genome and providing insight into the significant heritability associated with bone strength.
Identification of causal genes for rare human conditions that give rise to extreme bone mass phenotypes has revealed critical insights into bone biology, including several that give rise to a high bone mass phenotype. Osteoclast-targeted or osteopetrotic conditions have distinct effects on bone quality compared to those that target osteoblasts and result in osteosclerotic diseases. The lessons from studies using these models are that: High bone mass does not always result in increased strength or improved quality; too much of an increase in mass, even when accompanied by enhanced strength, is not necessarily desirable due to other comorbidities; and although several new drug targets have emerged from studies of high bone mass genes, achieving bone selective effects remains a major challenge.
A group of studies help elucidate the role of bone morphogenetic protein (BMP) in normal bone formation, removal, and quality. Heterotopic ossification is most commonly associated with severe tissue trauma. BMP signaling is active during skeletal development and repair as well as in a wide range of non-skeletal tissues. BMP implant experiments in mice demonstrated that increased BMP signaling induces ectopic bone formation. However, transgenic mouse models of BMP ligand or receptor overexpression that could lead to increased BMP signaling did not cause extra-skeletal bone formation. Fibrodysplasia ossificans progressiva (FOP), a human genetic disorder in which heterotopic bone forms in soft connective tissues, is also associated with altered skeletal formation, most characteristically malformation of the great toes. This rare disorder provides an opportunity to identify cellular pathways and mechanisms of misregulated and normal bone formation. All FOP patients have mutations in ACVR1, the gene encoding the ALK2 BMP type I receptor, and the mutations induce mild constitutive activation of the BMP pathway. A knock-in mouse model with the most common FOP mutation30 recapitulates clinical features of the human disease and is providing an increased understanding of the cellular and molecular mechanisms regulating skeletal development.31 While bone quality has not been assessed in patients with FOP because any surgery, for example, a biopsy, triggers further proliferation of ectopic bone, this mouse model provides an outstanding opportunity for determining bone quality in this condition.
Session V: Measurement of Bone Quality: Direct Assessment (Presenters: Marjolein van der Meulen, PhD; Hart Malluche, MD; Virginia Ferguson, PhD)
A fractured bone reflects a failure of skeletal function and results when the loads applied to the skeleton exceed its capacity. Hence, understanding the contributions to whole bone strength is critical for characterizing the normal and diseased skeleton and for developing treatments to improve bone quality and prevent fractures. Whole-bone structural behavior is determined by three structural characteristics: The total tissue mass, the geometric distribution of the tissue, and the tissue material properties. Whole-bone mechanical properties can be measured in different loading modes: Compression/tension, bending, and torsion.32 The key outcomes include whole-bone stiffness, failure load, and energy absorbed to failure. Because the geometry and material properties vary throughout the structure, these properties depend on bone size and shape. In contrast, tissue material properties represent the intrinsic behavior of the constituent material, and are independent of the size and shape of the whole bone (Fig. 1). The tissue material properties include the elastic modulus, ultimate stress, and toughness and are measured from homogenous samples with known geometry. Extrinsic factors that contribute to mechanical performance include age, sex, diet, and disease.
Mineralized tissues are hierarchical, biological, nanocomposite materials consisting of a collagenous organic matrix stiffened by calcium phosphate mineral and plasticized by water. These constituents combine to form lamellae or layers at length scales of multiple micrometers. Nanoindentation and small probing technologies are ideal tools for mechanical assessment at the micrometer to nanometer levels (Fig. 1). The new reference point indentation-based technologies are appealing because they have been adapted for in vivo use in the clinic, but uncertainty remains as to whether the measured outcomes relate to conventional mechanical properties, such as tissue toughness, or to damage.33
Histomorphometry provides information regarding structural, mineralization, cellular activity and other turnover parameters that contribute to bone quality. Tetracycline double labeling administered before biopsy provides information on bone formation and resorption. Histomorphometry can also be used to examine micro-damage accumulation, osteoid accumulation as an index of mineralization defects, and collagen alignment.34 The limitation is that biopsies are required, but currently there are no noninvasive methods for obtaining data on cellular activity or dynamic bone parameters. Micro-CT or HRpQCT provides 3D microarchitectural measures of trabecular structure that complements histomorphometric data.
Session VI: Human disease models of altered bone quality (Presenters: Joseph Lane, MD; John Healey, MD; Susan Schiavi, PhD)
Fractures occur in patients with two forms of osteoporosis, the usual postmenopausal type in which excessive bone remodeling is present, and the less common type with diminished osteoblastic bone formation. Fractures also occur in patients with cancer, osteopetrosis, and kidney disease. All of these diseases can alter bone quality.
Radiation, chemotherapy, and bisphosphonate treatments inhibit bone remodeling and may alter bone quality. In the 1990’s, bisphosphonates were shown to prevent fractures in patients with multiple myeloma.35 Bisphosphonates are also anti-angiogenic.36 Bisphosphonates reduce fracture incidence by 50–70%; however, bisphosphonate treatment for prolonged periods (>5 years) is associated with atypical femoral fractures. While early anti-neoplastic treatments may prevent fracture, after fracture all chemotherapy agents retard or block bone healing. Radiation, for example, prevents healing in a dose-dependent fashion >20 Gy, with complete inhibition reported at doses >50 Gy.37 A study using Raman spectroscopy found that local radiation (4 × 5 Gy) of mouse bones altered bone quality—particularly the amount of collagen cross-links—starting 1 week after the radiation and continuing for 12–26 weeks.38 The authors suggest that the increased brittleness of irradiated bone is due to the damaged collagen scaffold. Conventional chemotherapy is not immediately deleterious to bone, but like radiation, it has long-term detrimental effects. Because metastatic cancers are becoming chronic diseases, the long-term effects on bone quality of cancer, radiation, and chemotherapy are becoming increasingly important. The clinical challenge is selecting the particular bisphosphonate to administer and the duration of treatment that is optimal for maximizing bone quality.
Individuals with chronic kidney disease (CKD) suffer from bone disease with increased fracture incidence prior to dialysis, but the mechanisms responsible for early changes in bone quality leading to fracture are incompletely understood. Genetic models with progressive CKD and clinical biopsies were used to identify mechanisms contributing to these early bone changes39 and showed that increased sclerostin expression was associated with the repression of β-catenin signaling. Consistent with evidence from the conditional β-catenin knockout in which osteocytes do not produce β-catenin,30 this reduction of WNT/β-catenin signaling is associated with altered RANK/OPG ratios and increased osteoclast activity. These data suggest that mechanisms other than the observed parathyroid hormone (PTH) elevation may contribute to the pathogenesis of renal osteodystrophy.
Session VII: Effects of Pharmacological Treatments on Bone Quality (Presenters: Elise Morgan, PhD; Nancy Lane, MD; David Burr, PhD)
Among FDA-approved pharmacologic treatments for osteoporosis (Fig. 2), injectable forms of recombinant human PTH (Teriparatide) is currently the lone anabolic option. Intermittent treatment with PTH is a classic anabolic therapy in the sense of increased bone remodeling coupled with a positive bone balance. Evidence also exists that intermittent PTH induces “renewed modeling” particularly on periosteal and trabecular surfaces.40 The effects of PTH on bone quality include alterations in tissue mineralization, cortical porosity, trabecular architecture, microdamage accumulation, and potentially material properties. PTH-induced increase in bone turnover allows for improvements in bone microarchitecture. Key areas for study include defining the effects of PTH on the microscale mechanical properties of bone tissue, the role of PTH in bone mechanotransduction, and the mechanism by which PTH affects fracture prevention.
Figure 2.
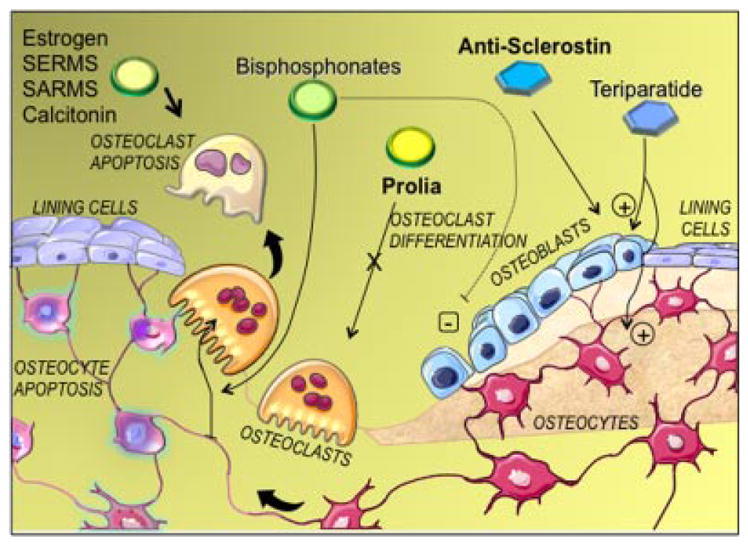
Cartoon showing the different classes of drugs in use to treat osteoporosis, and the cell pathways they affect. Drugs with green shapes affect osteoclasts and are considered anti-catabolic agents. Drugs with blue shapes stimulate osteoblasts and are considered anabolic. Arrows show the actions of the drugs, plus and minus symbols indicate whether effects are positive or negative. Modified with permission, from Gennari and Bilezikian.57
Glucocorticoid-induced osteoporosis or bone loss is common, and nearly 30% of individuals treated chronically with glucocorticoids (GCs) experience a fracture. GC-induced osteoporosis differs from postmenopausal osteoporosis: GC-treated individuals fracture at higher bone mass, and GC-induced bone loss can be recovered. The threshold GC dose that causes osteoporosis is debated, but prednisone doses >7.5 mg/day appear associated with bone loss and fracture. Mouse studies41 show that GCs alter trabecular architecture, increase turnover, decrease mineral content, and decrease compressive strength. One possible mechanism is the increase in sclerostin, which would inhibit new bone formation, altering bone quality. Low-dose GCs induce osteocyte autophagy in cortical bone, and higher doses induce apoptosis. These two forms of cell death likely impact material and mechanical properties of the tissue. Further study of the responsible pathways could lead to effective treatments to prevent bone loss.
Five classes of antiresorptive medications to treat osteoporosis are approved in the US. The anti-catabolic (antiresorptive) agents that affect bone quality include bisphosphonates, selective estrogen modulators (SERMs), calcitonin, estrogen, and RANKL-antibodies. All suppress bone remodeling, but have variable or unknown effects on tissue material properties. Bisphosphonates tend to increase microdamage accumulation and AGE content, and decrease toughness.4,9 The bisphosphonates suppress remodeling from 50% to 90% or more, leading to a fourfold increase in vertebral microcrack density when given to estrogen-replete dogs at clinical doses.42 Although RANKL antibodies (Denosumab) initially suppress bone remodeling even more than many bisphosphonates, the bone turnover gradually recovers over 6 months until the next injection. Over a 3-year treatment period, nearly 50% of treated patients had remodeling rates within the normal premenopausal range. Thus, Denosumab may not have the same long-term consequences as bisphosphonates. Denosumab did not reduce bone toughness in an ovariectomized monkey model. Raloxifene is one of several SERMs approved in the US, but the only one for which bone material property data exist. Raloxifene increases post-yield displacement and toughness of canine femoral cortical bone by 60–100%.43 Crack length, but not crack density increased significantly compared to vehicle-treated controls.44 Its positive effects on bone toughness may be the result of sequestering water in the bound water fraction of the tissue.
Session VIII: Strategies for Managing Patients with Altered Bone Quality (Presenters: Susan Bukata, MD; Thomas Einhorn, MD; Marc Swiontkowski, MD; Jay Lieberman, MD; David Burr, PhD)
More than half of women and one third of men over age 50 in the US will suffer a fragility fracture in their lifetime. Medical interventions can decrease the risk of spine fracture by 50–77% and hip fracture by 20–40%. However, many patients, including those at high risk, remain untreated. A repeatedly asked question is, “Why is there such resistance to bone health screening?” Despite recognition that adult patients who have suffered a fragility fracture are among the high risk patients for additional fractures,45 only 20% of these patients receive osteoporosis medication after their fragility fracture care. Patients identified as at risk for osteoporosis who do begin taking medications have low adherence rates.46 Failure of physicians to identify high-risk patients, poor patient acceptance of osteoporosis medications,47 and lack of adherence all contribute to the low rate of treatment. Several strategies to identify patients needing treatment, including the FRAX algorithm48 and fracture liaison services49 have been developed. Recently, questions regarding side effects of long-term usage of osteoporosis medications, particularly bisphosphonates, have led to confusion regarding appropriate breaks in therapy, re-initiation of therapy, and personal benefits of medications compared to risks of rare events. Further research is needed to provide this treatment guidance for patients at risk of fragility fracture.
Enhancement of skeletal repair and perhaps bone quality by implantable and injectable substances has been the subject of substantial research. Fracture calluses that heal through endochondral ossification normally progress from poor quality new bone to more mature, higher quality bone. Current clinical assessment of healing is based on radiographic measures of union at the callus, but clinicians lack information on callus tissue quality. The goal of enhancing fracture repair has been elusive, but observations suggest that repair is enhanced by systemic treatment. PTH was used in at least one clinical trial to enhance fracture healing50 and in others to reduce fracture risk51; however, the positive effects of PTH on accelerating healing and reducing fracture risk must be confirmed in other studies. Other pathways that might be targeted to enhance fracture repair include the wnt signaling pathway,26,29 particularly lipoprotein-related protein 5 (LRP5), which is required for this pathway and acts as a coreceptor. Antagonism of wnt signaling by the dickkopf (dkk) family prevents activation of LRP5 and thus modulates bone mass.52 Similarly, sclerostin, the SOST gene product, is a circulating inhibitor of LRP5 and thus inhibits wnt signaling. Phase I and II clinical trials are underway to test the efficacy of inhibitors of wnt signaling for their ability to systemically enhance skeletal repair.
Clinical trials in hip fractures are active in three areas that might address bone quality: Internal fixation for femoral neck fractures, arthroplasty for femoral neck fractures, and internal fixation for intertrochanteric hip fractures. With the aging population, these areas may reflect optimal care to preserve function and prevent readmissions for the best value for patients, families, and payors. A meta analysis53 of femoral neck fractures suggested early (<4 month) mortality may be lower for patients treated with internal fixation. Fractures fixed with sliding hip screws had a significantly lower revision rate than those fixed with multiple screw implants. Further work is underway in the FAITH RCT in which 1,500 patients are being recruited. These differences in fracture fixation might be related to both the quality of the callus and the amount of bone formation allowed by the fixation device.
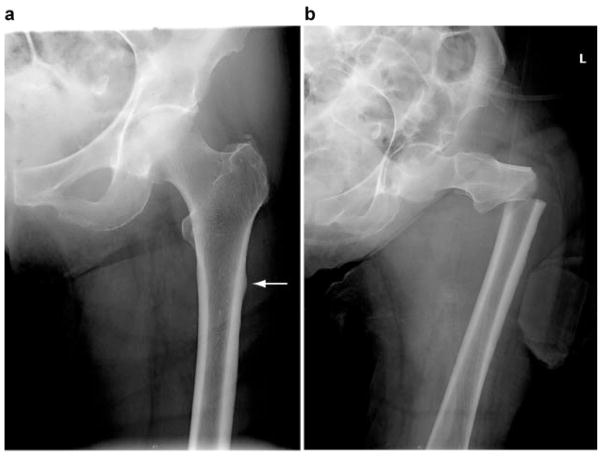
An unresolved problem that requires an understanding of bone quality and is needed for fracture prevention is the atypical femoral fracture (AFF).47 These unique transverse fractures (Fig. 3), initiating on the lateral side of the femur (either subtrochanteric or shaft) have been identified in bisphosphonate and Denosumab users. Although relatively uncommon, the incidence may increase with duration of bisphosphonate therapy. Initiating factors include microcrack and AGE accumulations, and documented loss of mineral and matrix heterogeneity. Dog rib studies simulating prolonged bisphosphonate therapy demonstrated marked loss of toughness. In a systemic review and meta-analysis, subgroup analysis of studies using the ASBMR criteria to define AFF suggests a higher risk of AFF with bisphosphonates use with RR of 11.78 (95% CI, 0.39–359.69) as compared to studies using mainly diagnostic codes (RR 1.62, 95% CI, 1.18–2.22).47,54 The conundrum arises because these drugs are extremely effective in preventing fractures, yet overuse may be associated with increased fracture risk.55 Additional knowledge of the effects of such drugs on bone quality is needed to resolve this dilemma.
Figure 3.
Radiographs showing (a1) a stress reaction (arrow) on the lateral proximal femoral cortex and (a2) an atypical subtrochanteric fracture sustained atraumatically in the same patient 48 h later and (b) a typical spiral subtrochanteric fracture. Adapted with permission from Donnelly and Saleh.58
RECOMMENDATIONS
Breakout groups focused on clinical topics and discussed future research and treatment directions, with results summarized in Table 1. A common theme was the need for more education of clinicians in areas of bone quality and for basic science studies to address specific topics of pathophysiology, diagnosis, prevention, and treatment of altered bone quality.
Acknowledgments
The Bone Quality and Fracture Prevention symposium was supported by NIH (1R13AR063599) and grants from Lilly USA and Zimmer. The authors appreciate the assistance of Dr. Timothy Wright in editing this manuscript.
Grant sponsor: NIH; Grant number: 1R13AR063599; Grant sponsor: Lilly USA; Grant sponsor: Zimmer.
References
- 1.Bouxsein ML, Seeman E. Quantifying the material and structural determinants of bone strength. Best Pract Res Clin Rheumatol. 2009;23:741–753. doi: 10.1016/j.berh.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 2.McDonnell P, McHugh PE, O’Mahoney D. Vertebral osteoporosis and trabecular bone quality. Ann Biomed Eng. 2007;35:170–189. doi: 10.1007/s10439-006-9239-9. [DOI] [PubMed] [Google Scholar]
- 3.Cooper C, Cole ZA, Holroyd CR, et al. IOF CSA Working Group on Fracture Epidemiology. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22:1277–1288. doi: 10.1007/s00198-011-1601-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang SY, Zeenath U, Vashishth D. Effects of non-enzymatic glycation on cancellous bone fragility. Bone. 2007;40:1144–1151. doi: 10.1016/j.bone.2006.12.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donnelly E, Meredith DS, Nguyen JT, et al. Reduced cortical bone compositional heterogeneity with bisphosphonate treatment in postmenopausal women with intertrochanteric and subtrochanteric fractures. J Bone Miner Res. 2012;27:672–678. doi: 10.1002/jbmr.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jepsen KJ. Functional interactions among morphologic and tissue quality traits define bone quality. Clin Orthop Relat Res. 2011;469:2150–2159. doi: 10.1007/s11999-010-1706-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van der Meulen MC, Jepsen KJ, Mikić B. Understanding bone strength: size isn’t everything. Bone. 2001;29:101–104. doi: 10.1016/s8756-3282(01)00491-4. [DOI] [PubMed] [Google Scholar]
- 8.Schlecht SH, Jepsen KJ. Functional integration of skeletal traits: an intraskeletal assessment of bone size, mineralization, and volume covariance. Bone. 2013;56:127–138. doi: 10.1016/j.bone.2013.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allen MR, Reinwald S, Burr DB. Alendronate reduces bone toughness of ribs without significantly increasing microdamage accumulation in dogs following 3 years of daily treatment. Calcif Tissue Int. 2008;82:354–360. doi: 10.1007/s00223-008-9131-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allen MR, Erickson AM, Wang X, et al. Morphological assessment of basic multicellular unit resorption parameters in dogs shows additional mechanisms of bisphosphonate effects on bone. Calcif Tissue Int. 2010;86:67–71. doi: 10.1007/s00223-009-9315-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Viguet-Carrin S, Roux JP, Arlot ME, et al. Contribution of the advanced glycation end product pentosidine and of maturation of type I collagen to compressive biomechanical properties of human lumbar vertebrae. Bone. 2006;39:1073–1079. doi: 10.1016/j.bone.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 12.Boskey AL, Robery PG. The regulatory role of matrix proteins in mineralizaiton of bone. In: Marcus R, Feldman D, Dempster DW, Luckey M, Cauley JA, editors. Osteoporosis. 4. Vol. 1. Chapter 11. Waltham MA: Elsevier, Academic Press; 2013. pp. 235–258. [Google Scholar]
- 13.Feng JQ, Ward LM, Liu S, et al. Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet. 2006;38:1310–1315. doi: 10.1038/ng1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ameye L, Young MF. Mice deficient in small leucine-rich proteoglycans: novel in vivo models for osteoporosis, osteoarthritis, Ehlers-Danlos syndrome, muscular dystrophy, and corneal diseases. Glycobiology. 2002;12:107R–116R. doi: 10.1093/glycob/cwf065. [DOI] [PubMed] [Google Scholar]
- 15.Mashiba T, Turner CH, Hirano T, et al. Effects of suppressed bone turnover by bisphosphonates on microdamage accumulation and biomechanical properties in clinically relevant skeletal sites in beagles. Bone. 2001;28:524–531. doi: 10.1016/s8756-3282(01)00414-8. [DOI] [PubMed] [Google Scholar]
- 16.Chapurlat RD, Arlot M, Burt-Pichat B, et al. Micro-crack frequency and bone remodeling in postmenopausal osteoporotic women on long-term bisphosphonates: a bone biopsy study. J Bone Miner Res. 2007;22:1502–1509. doi: 10.1359/jbmr.070609. [DOI] [PubMed] [Google Scholar]
- 17.Stepan JJ, Burr DB, Pavo I, et al. Low bone mineral density is associated with bone microdamage accumulation in postmenopausal women with osteoporosis. Bone. 2007;41:378–385. doi: 10.1016/j.bone.2007.04.198. [DOI] [PubMed] [Google Scholar]
- 18.Allen MR, Burr DB. Bisphosphonate effects on bone turnover, microdamage, and mechanical properties: what we think we know and what we know that we don’t know. Bone. 2011;49:56–65. doi: 10.1016/j.bone.2010.10.159. [DOI] [PubMed] [Google Scholar]
- 19.Krug R, Carballido-Gamio J, Banerjee S, et al. In vivo ultra-high-field magnetic resonance imaging of trabecular bone microaritecture at 7 T. J Magn Reson Imaging. 2008;27:854–859. doi: 10.1002/jmri.21325. [DOI] [PubMed] [Google Scholar]
- 20.Liu XS, Zhang XH, Sekhon KK, et al. High-resolution peripheral quantitative computed tomography can assess microstructural and mechanical properties of human distal tibial bone. J Bone Miner Res. 2010;25:746–756. doi: 10.1359/jbmr.090822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hong J, Cabe GD, Tedrow JR, et al. Failure of trabecular bone with simulated lytic defects can be predicted non-invasively by structural analysis. J Orthop Res. 2004;22:479–486. doi: 10.1016/j.orthres.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Wang X, Sanyal A, Cawthon PM, et al. Prediction of new clinical vertebral fractures in elderly men using finite element analysis of CT scans. J Bone Miner Res. 2012;27:808–816. doi: 10.1002/jbmr.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marini JC, Blissett AR. New genes in bone development: what’s new in osteogenesis imperfecta. J Clin Endocrinol Metab. 2013;98:3095–3103. doi: 10.1210/jc.2013-1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carriero A, Zimmermann EA, Paluszny A, et al. How tough is brittle bone? investigating osteogenesis imperfecta in mouse bone. J Bone Miner Res. 2014 doi: 10.1002/jbmr.2172. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Valdar W, Flint J, Mott R. Simulating the collaborative cross: power of quantitative trait loci detection and mapping resolution in large sets of recombinant inbred strains of mice. Genetics. 2006;172:1783–1797. doi: 10.1534/genetics.104.039313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rossini M, Gatti D, Adami S. Involvement of WNT/β-catenin signaling in the treatment of osteoporosis. Calcif Tissue Int. 2013;93:121–132. doi: 10.1007/s00223-013-9749-z. [DOI] [PubMed] [Google Scholar]
- 27.Virk MS, Alaee F, Tang H, et al. Systemic administration of sclerostin antibody enhances bone repair in a critical-sized femoral defect in a rat model. J Bone Joint Surg Am. 2013;95:694–701. doi: 10.2106/JBJS.L.00285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baron R, Kneissel M. WNT signaling in bone homeostasis and disease: from human mutations to treatments. Nat Med. 2013;19:179–192. doi: 10.1038/nm.3074. [DOI] [PubMed] [Google Scholar]
- 29.Kramer I, Halleux C, Keller H, et al. Osteocyte Wnt/beta-catenin signaling is required for normal bone homeostasis. Mol Cell Biol. 2010;30:3071–3085. doi: 10.1128/MCB.01428-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chakkalakal SA, Zhang D, Culbert AL, et al. An Acvr1 R206H knock-in mouse has fibrodysplasia ossificans progressiva. J Bone Miner Res. 2012;27:1746–1756. doi: 10.1002/jbmr.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shore EM, Kaplan FS. Inherited human diseases of heterotopic bone formation. Nat Rev Rheumatol. 2010;6:518–527. doi: 10.1038/nrrheum.2010.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cole JH, van der Meulen MCH. Whole bone mechanics and bone quality. Clin Orthop Relat Res. 2011;469:2139–2149. doi: 10.1007/s11999-011-1784-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jepsen KJ, Schlecht SH. Individuals with type II diabetes show increased fracture incidence despite having normal BMD. J Bone Miner Res. 2014;28:784–786. doi: 10.1002/jbmr.2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Herman BC, Cardoso L, Majeska RJ, et al. Activation of bone remodeling after fatigue: differential response to linear microcracks and diffuse damage. Bone. 2010;47:766–772. doi: 10.1016/j.bone.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Berenson JR, Lichtenstein A, Porter L, et al. Efficacy of pamidronate in reducing skeletal events in patients with advanced multiple myeloma. Myeloma Aredia Study Group. N Engl J Med. 1996;334:488–493. doi: 10.1056/NEJM199602223340802. [DOI] [PubMed] [Google Scholar]
- 36.Tsai SH, Huang PH, Chang WC, et al. Zoledronate inhibits ischemia-induced neovascularization by impairing the mobilization and function of endothelial progenitor cells. PLoS ONE. 2012;7:e41065. doi: 10.1371/journal.pone.0041065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lehner B, Bauer J, Rödel F, et al. Radiation-induced impairment of osseous healing with vascularized bone transfer: experimental model using a pedicled tibia flap in rat. Int J Oral Maxillofac Surg. 2004;33:486–492. doi: 10.1016/j.ijom.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 38.Gong B, Oest ME, Mann KA, et al. Raman spectroscopydemonstrates prolonged alteration of bone chemical composition following extremity localized irradiation. Bone. 2013;57:252–258. doi: 10.1016/j.bone.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sabbagh Y, Graciolli FG, O’Brien S, et al. Repression of osteocytes Wnt/β-catenin signaling is an early event in the progression of renal osteodystrophy. J Bone Miner Res. 2012;27:1757–1772. doi: 10.1002/jbmr.1630. [DOI] [PubMed] [Google Scholar]
- 40.Easley SK, Jekir MG, Burghardt AJ, et al. Contribution of the intra-specimen variations in tissue mineralization to PTH- and raloxifene-induced changes in stiffness of rat vertebrae. Bone. 2010;46:1162–1169. doi: 10.1016/j.bone.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 41.Lane NE, Yao W, Balooch M, et al. Glucocorticoid-treated mice have localized changes in trabecular bone material properties and osteocyte lacunar size that are not observed in placebo-treated or estrogen-deficient mice. J Bone Miner Res. 2006;21:466–476. doi: 10.1359/JBMR.051103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Allen MR, Iwata K, Phipps R, et al. Alterations in canine vertebral bone turnover, microdamage accumulation, and biomechanical properties following 1-year treatment with clinical treatment of risedronate or alendronate. Bone. 2006;39:872–879. doi: 10.1016/j.bone.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 43.Allen MR, Hogan HA, Hobbs WA, et al. Raloxifene enhances material-level mechanical properties of femoral cortical and trabecular bone. Endocrinology. 2007;148:3908–3913. doi: 10.1210/en.2007-0275. [DOI] [PubMed] [Google Scholar]
- 44.Allen MR, Iwata K, Sato M, et al. Raloxifene enhances vertebral mechanical properties independent of density. Bone. 2006;39:1130–1135. doi: 10.1016/j.bone.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 45.Silman AJ. The patient with fracture: the risk of subsequent fractures. Am J Med. 1995;98:12S–16S. doi: 10.1016/s0002-9343(05)80039-7. [DOI] [PubMed] [Google Scholar]
- 46.Cramer JA, Gold DT, Silverman SL, et al. A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos Int. 2007;18:1023–1031. doi: 10.1007/s00198-006-0322-8. [DOI] [PubMed] [Google Scholar]
- 47.Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American society for bone and mineral research. J Bone Miner Res. 2014;29:1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 48.Kanis JA, Johnell O, Oden A, et al. FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19:385–397. doi: 10.1007/s00198-007-0543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mitchell PJ. Best practices in secondary fracture prevention: fracture liaison services. Curr Osteoporos Rep. 2013;11:52–60. doi: 10.1007/s11914-012-0130-3. [DOI] [PubMed] [Google Scholar]
- 50.Peichl P, Holzer LA, Maier R, et al. Parathyroid hormone 1-84 accelerates fracture-healing in pubic bones of elderly osteoporotic women. J Bone Joint Surg Am. 2011;93:1583–1587. doi: 10.2106/JBJS.J.01379. [DOI] [PubMed] [Google Scholar]
- 51.Nakamura T, Sugimoto T, Nakano T, et al. Randomized Teriparatide [human parathyroid hormone (PTH) 1-34] Once-Weekly Efficacy Research (TOWER) trial for examining the reduction in new vertebral fractures in subjects with primary osteoporosis and high fracture risk. J Clin Endocrinol Metab. 2012;97:3097–3106. doi: 10.1210/jc.2011-3479. [DOI] [PubMed] [Google Scholar]
- 52.Niehrs C. Function and biological roles of the Dickkopf family of Wnt modulators. Oncogene. 2006;25:7469–7481. doi: 10.1038/sj.onc.1210054. [DOI] [PubMed] [Google Scholar]
- 53.Bhandari M, Tornetta P, III, Hanson B, et al. Optimal internal fixation for femoral neck fractures: multiple screws or sliding hip screws? J Orthop Trauma. 2009;23:403–407. doi: 10.1097/BOT.0b013e318176191f. [DOI] [PubMed] [Google Scholar]
- 54.Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res. 2013;28:1729–1737. doi: 10.1002/jbmr.1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Diab DL, Watts NB. Bisphosphonates in the treatment of osteoporosis. Endocrinol Metab Clin North Am. 2012;41:487–506. doi: 10.1016/j.ecl.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 56.Donnelly E. Methods for assessing bone quality. Clin Orthop Relat Res. 2011;469:2128–2138. doi: 10.1007/s11999-010-1702-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gennari L, Bilezikian JP. Glucocorticoid-induced osteoporosis: hope on the HORIZON. Lancet. 2009;373:1225–1226. doi: 10.1016/S0140-6736(09)60704-2. [DOI] [PubMed] [Google Scholar]
- 58.Donnelly E, Saleh A, Unnanuntana A, Lane JM. Atypical femoral fractures: epidemiology, etiology, and patient management. Curr Opin Support Palliat Care. 2012;6:348–354. doi: 10.1097/SPC.0b013e3283552d7d. [DOI] [PMC free article] [PubMed] [Google Scholar]