ABSTRACT
Objective
This study aimed to investigate the potential role of CAMK II pathway in the compression-regulated OPG expression in periodontal ligament cells (PDLCs).
Material and Methods
The PDL tissue model was developed by 3-D culturing human PDLCs in a thin sheet of poly lactic-co-glycolic acid (PLGA) scaffolds, which was subjected to static compression of 25 g/cm2 for 3, 6 and 12 h, with or without treatment of KN-93. After that, the expression of OPG, RANKL and NFATC2 was investigated through real-time PCR and western blot analysis.
Results
After static compression, the NFATC2 and RANKL expression was significantly up-regulated, while partially suppressed by KN-93 for 6 and 12 h respectively. The OPG expression was significantly down-regulated by compression in 3 h, started to elevate in 6 h, and significantly up-regulated in 12 h. The up-regulation after 12 h was significantly suppressed by KN-93.
Conclusions
Long-term static compression increases OPG expression in PDLCs, at least partially, via the CAMK II pathway.
Keywords: Osteogenesis, Periodontal ligament, Calcium-calmodulin-dependent Protein kinases, Mechanotransduction
INTRODUCTION
Mechanical loading has long been deciphered to regulate bone metabolism, and plays critical roles in orthodontic tooth movement (OTM) 4 , 10 , 22 . When teeth are subjected to orthodontic force, the remodeling of the adjacent periodontium is initiated. The static compression induces bone resorption at the pressure side, resulting in a “loose” tooth, followed by bone formation to complete a bone remodeling cycle, which restores the periodontium and strengthens the tooth again 29 . Lack of this recovery process may lead to alveolar bone loss followed by gingival recession and tooth removability.
The molecular mechanisms under bone remodeling in OTM has been extensively investigated. Numerous studies have focused on osteoclastogenesis, the rate-limiting step in OTM 1 , 12 , 16 . Particularly, COX-2 has been shown to induce up-regulation of receptor activator for nuclear factor-κ B ligand (RANKL), an essential pro-osteoclastogenic factor, in periodontal ligament cells (PDLCs) under compression 19 . However, little is known about the pathways to regulate the mechano-induced expression of osteoprotegerin (OPG), the decoy receptor of RANKL, which inhibits bone resorption while promoting bone formation 6 .
The Ca2+/calmodulin-dependent kinase (CAMK) family has been recognized as a key mediator in living organisms and various biological processes 9 . Recent studies have revealed its critical role in bone development and homeostasis. The CAMK II pathway has been found to regulate the RANKL-induced osteoclast formation via the cAMP-response element binding protein (CREB) pathway 3 . The involvement of CAMK II in regulating the RANK-MEK-ERK pathway has been detected 21 . Moreover, the CAMK II-CREB pathway was proposed to play an important role in bone homeostasis.
We previously established a periodontal ligament tissue model (PDLtm) to simulate the bioprocess at the pressure side of PDL 18 . Interestingly, through microarray screening, we found up-regulation of the CAMK II pathway in the loaded PDLCs 17 , which is known to respond to compression and result in OPG enhancement in osteoblast 11 . Therefore, in the present study, we aimed to investigate the potential role of CAMK II pathway in the expression of OPG and RANKL in the PDLtm under static compression.
MATERIAL AND METHODS
Preparation of PLGA scaffold
The poly lactic-co-glycolic (PLGA) polymers (105 g/mol) were used for the synthesis of the scaffolds as previously described 17 . Briefly, 200 mg mixture of PLGA polymers and sucrose particulates with a volume ratio of 15:85 was applied with compression to form a thin sheet in a square mould (2 cm × 2 cm). Subsequently, the sheets were placed in a CO2 reaction kettle for 48 h, and the sucrose was then removed by immersing the PLGA sheets in ddH2O for 48 h. After that, the PLGA sheets (2 cm×2 cm×300 μm) were packaged and sterilized for experimental use.
Establishment of the PDLtm
Five lines on human PDLCs were established following a well-documented method 17 . The periodontal tissue was collected from the teeth extracted for orthodontic reasons with the donors signing an informed consent form and the approval of the Institutional Review Board in our hospital. The PDLCs of the 3-6th passage were used for this experiment. The 3-D PDLtm was established by dripping suspension of PDLCs into the PLGA sheet that was put in a 6-well plate, approximate 1×105 cells in 2 ml medium per sheet. After 24 h, the PDLtm was displaced to another 6-well plate. Each cell line (n=5) was used for the experiment in three replicates, two of which were pooled together for western blot and one for real-time PCR.
Histological observation
Four days after the establishment of PDLtm, the growth of PDLCs in scaffolds was investigated by microscopic observations. First, the PDLtm was stained by acridine orange (0.01%) and observed under a fluorescence inverted microscope (Leica DMI6000B, Germany). Second, the PLGA/PDLC construct was prepared for scanning of electron microscopy (SEM, Inspect F, FEI, USA) 17 .
Application of compressive force
The PDLtms were randomly assigned into three groups, i.e., the control group, the compression group (Cg) and the compression+KN-93 (an inhibitor of the CAMK II pathway) group (CKg). To simulate the pressured periodontium in OTM, a modified “weight” method was used. Briefly, a cover glass and a bottle of granules were placed on the PDLtm to produce a compression of 25 g/cm2, which has been proved to be the optimal force level for this model 18 . In the compression+KN-93 group, 0.01 mM KN-93 (Sigma) was added to the media to suppress the CAMK II pathway.
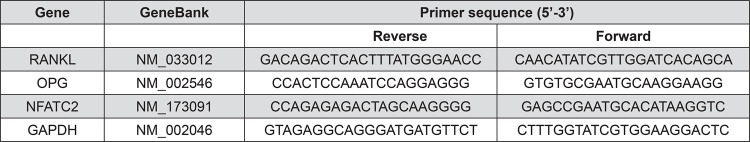
Real-time PCR
Three, six and twelve hours after applying interventions, total RNA (n=5) was extracted by dissolving the PDLtm using TRIzol reagent (Invitrogen, Carlsbad, USA). The quality and integrity of extracted RNA samples were validated before their use. Real-time PCR was performed with a SYBR Green reaction Kit (Roche Diagnostics, China) in a LightCycler according to the manufacturer’s instruction to investigate the mRNA expression of RANKL, OPG, and Nuclear factor of activated T-cells (NFAT) C2. GAPDH served as the internal control. The sequences of relevant primers were shown in Figure 1.
Figure 1. Primer used in real-time PCR analysis.
Western blotting
Twelve hours after force application, the total proteins (n=5) were collected using total protein extraction kit (Keygen Biotech, China). The 15 μL prepared samples (40 μg of protein) per lane were separated by SDS-PAGE and then transferred to the polyvinylidene difluoride (PVDF) membrane. After that, the PVDF membranes were probed with antibodies to RANKL (1:1000, Santa-Cruz, USA), OPG (1:1000, Santa-Cruz, USA) GAPDH (1:1000, Beyotime, China) overnight at 4°C. Subsequently, the membranes were immersed in secondary antibody (1:5000, Beyotime, China) for 1 h. The immunoreactive proteins were visualized by a chemiluminescence kit (Millipore). The band intensities were evaluated using Quantity One software (Bio-Rad, Hercules, USA).
Statistical analysis
All data was expressed as mean±SD. The comparison among 3 groups was conducted by one-way analysis of variance (ANOVA) followed by LSD post hoc test using SPSS software of version 13.0. Differences with p<0.05 were set as significant.
RESULTS
The 3-D cultured PDLCs
By acridine orange staining, the growth of PDLCs was observed under microscope (Figure 2A). In addition, the secreted extracellular matrix, the PDLCs and the scaffolds were observed to be interconnected under SEM (Figure 2B). More characterization of this PDLtm has been previously shown 18 .
Figure 2. The microscopic observations of PDLtm. (A) Spindle PDLCs grew densely with nuclear in green-yellow and cytoplasma in orange-red, 200×; (B) The PDLCs, secreted extracellular matrix (SEM) and PLGA scaffolds were integrated, 300×.

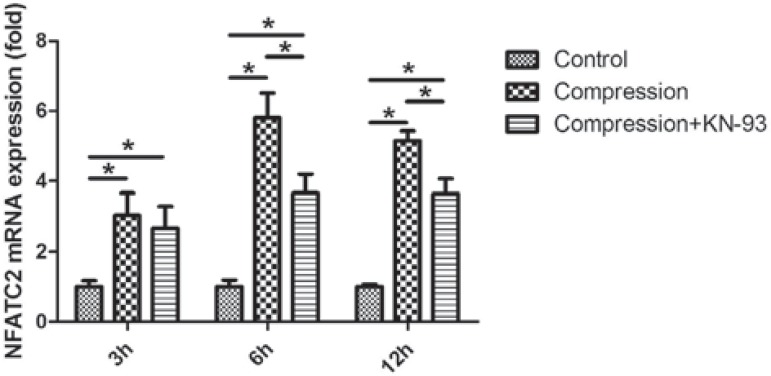
The NFATC2 expression
Under static compression, the NFATC2 expression was significantly up-regulated, which peaked in 6 h (Figure 3). KN-93 partially suppressed the compression-induced up-regulation of NFATC2 in 6 and 12 h.
Figure 3. The time-course expression of NFATC2 in loaded PDLCs at mRNA level. Compression enhanced the NFATC2 expression throughout the experiment, while its expression was inhibited by KN-93 after 6 and 12 h. *p<0.05.
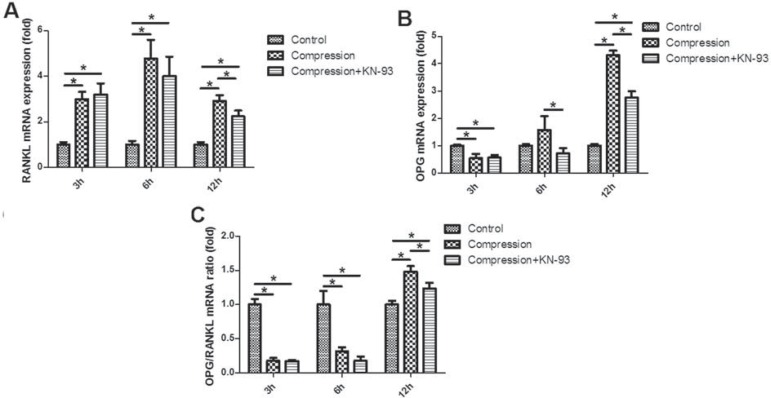
The OPG/RANKL expression
The real-time PCR analysis revealed the significant up-regulation of RANKL expression under static compression, which peaked in 6 h (Figure 4A). In contrast, the OPG expression was significantly down-regulated after 3 h, while up-regulated in 12 h (Figure 4B). The OPG/RANKL ratio was reduced in 3 and 6 h while enhanced in 12 h (Figure 4C).
Figure 4. The time-course expression of osteoprotegerin (OPG) and RANKL in loaded PDLCs at mRNA level. (A) RANKL; (B) OPG; (C) OPG/RANKL ratio.*p<0.05.
Notably, after 12 h, the up-regulation of RANKL, OPG and OPG/RANKL ratio was partially suppressed by KN-93, suggesting that the CAMK II pathway took part in the up-regulation of RANKL and OPG in PDLCs induced by long-term stimulation of static compression (Figure 4).
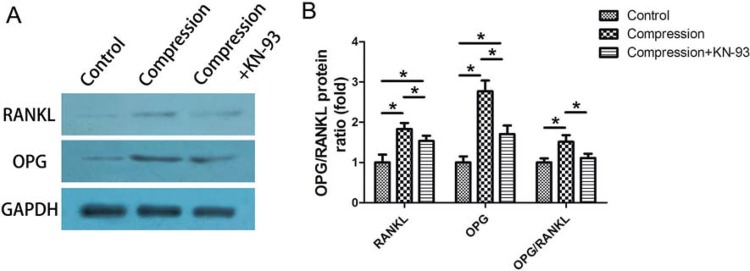
Moreover, the western blotting method showed results similar to the PCR assay, indicating that after 12 h of static compression there was an increased protein expression of RANKL and OPG, which was partially suppressed by KN-93 (Figure 5).
Figure 5. (A) The protein expression of osteoprotegerin (OPG) and RANKL in the loaded PDLCs after 12 h. The static compression significantly elevated the OPG and RANKL expression in PDLCs, while the enhancement was suppressed by KN-93; (B) The fold change of the expression of OPG, RANKL and OPG/RANKL ratio. *p<0.05.
DISCUSSION
Orthodontic tooth movement (OTM) has been generally featured with bone remodeling, a fundamental biological process consisting of bone resorption and bone formation 23 . Particularly, the initiated bone resorption at compression sites results in tooth movement, and the following bone formation surrounding roots strengthen the new position of the teeth 29 . Numerous studies focused on the osteoclastogenesis at the pressure side and sketched the contour of underlying mechanisms 12 , 13 , while the subsequent bone formation was less studied.
The CAMK family contains a series of proteins playing critical roles in bone modeling and remodeling. Afamin enhances osteoclastogenesis by decreasing intracellular cAMP levels via the CAMK pathways 14 . The role of the CAMK II pathway in the parathyroid hormone-related protein (PTHrP)-regulating osteoclast inhibitory lection has been recently identified 32 . Though KN-93 was observed to exert effects on other pathways 8 , it has been applied as a classic CAMK II pathway inhibitor in many studies 25 , 27 . Recently, by using KN-93, the enhancement of OPG in osteoblast under mechanical stimuli was suppressed 11 . However, limited information concerning its effect on OTM is available till now.
The microarray screening for gene expression profiles in our previous study has revealed the potential role of the CAMK II pathway in the mechanoresponse of PDLCs 17 . In the present study, PDLCs were embedded in 3-D PLGA scaffolds and cultured under static compressive force. The ratio of OPG/RANKL expression was significantly down-regulated 3 and 6 h after loading, indicating a potential role of osteoclastogenesis induction 24 , 31 . On the other hand, the OPG expression declined in 3 h, while started to elevate in 6 h and was significantly up-regulated after 12 h. As an important anti-osteoclastic and pro-osteogenic factor, the marked up-regulation of OPG after 12h indicates suppression for bone resorption 15 . However, this elevation was greatly impeded by KN-93, a specific CAMK II pathway inhibitor, suggesting that CAMK II pathway takes part in the OPG up-regulation induced by long-term static compression stimulation. Notably, the CAMK II pathway has also been reported to regulate the mechano-induced OPG enhancement in osteoblast 11 , which is to a great extent similar to PDL fibroblast 2 .
The RANKL–RANK–OPG axis mediates osteoclast formation through activation of RANK on the osteoclast precursors by RANKL 28 . Although the constitutional expression of OPG in PDLCs is much higher than RANKL 26 , numerous studies demonstrated the comparatively slight up-regulation of RANKL in PDLCs induced by compressive force could promote osteoclast formation and the following tooth movement 13 , 18 . Therefore, the large ratio of total OPG vs. RANKL seems meaningless accounting for osteoclastic induction. A reasonable explanation has been given that it could be due to the tight cell–cell contact between PDLCs and osteoclast precursors, which could create a favorable micro-environment for RANKL–RANK binding, thereby preventing the interaction of OPG with RANKL 5 .
On the other hand, at the sites away from the cell–cell contact area, the expression of OPG could play an important role. In contrast to the study reporting reduced or unchanged OPG expression in PDLCs under compression 20 , in the present study the OPG expression was significantly up-regulated after long-term mechanical stimuli, consistent with our previous data 18 . The delayed but marked increase of OPG could account for the subsequent bone formation at pressure periodontium, which prevents from alveolar bone loss and strengthens tooth again after movement. In this sense, targeting the CAMK II pathway might potentially benefit the OTM periodontium by stimulating OPG expression.
In the present study, we observed that the expression of NFATC2 in PDLCs was enhanced by compressive force while partially inhibited by KN-93 treatment (Figure 3). NFATC2 is a transcription factor which plays an undisputable role in the mechanoresponse of bone tissue 30 . As downstream factors of Wnt-Ca2+ pathways, both NFATC2 and CAMK II are involved in the Wnt-Ca2+ bone formation regulated by pathways 7 . Interestingly, Wnt-Ca2+ pathways were up-regulated when PDLCs were treated with compressive force in our previous study 17 . Therefore, the enhancement of OPG in PDLCs under compressive force might be regulated via Wnt-Ca2+ pathways, which should be further identified in future.
Last but not the least, it is interesting to compare the masticatory force and orthodontic force, both of which are transmitted to alveolar bone through PDL, while it results in opposite effects on alveolar bone metabolism. Obviously, the present theory of “compression-PDL-osteoclastogenesis” process cannot interpret this contradictory phenomenon. Based on our results, it is reasonable to speculate that the CAMK II pathways may be much more sensitive to masticatory force (intermittent force) than orthodontic force (static force), which should be further identified.
CONCLUSION
The OPG expression was significantly up-regulated in PDLCs after long-term static compression stimulation, which is at least partially regulated by the CAMK II pathway. These results have enriched the present understanding to molecular mechanisms in bone remodeling modulation in OTM.
ACKNOWLEDGEMENT
This study was supported by NSFC - National Natural Science Foundation of China (11372202 and 31201087), and by Sichuan University Fund for Outstanding Young Scholars (2082604164243).
REFERENCES
- 1.Alhashimi N, Frithiof L, Brudvik P, Bakhiet M. Orthodontic tooth movement and de novo synthesis of proinflammatory cytokines. Am J Orthod Dentofacial Orthop. 2001;119(3):307–312. doi: 10.1067/mod.2001.110809. [DOI] [PubMed] [Google Scholar]
- 2.Alves LB, Mariguela VC, Grisi MF, Souza SL, Novaes AB, Junior, Taba M, Junior, et al. Expression of osteoblastic phenotype in periodontal ligament fibroblasts cultured in three-dimensional collagen gel. J Appl Oral Sci. 2015;23(2):206–214. doi: 10.1590/1678-775720140462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ang ES, Zhang P, Steer JH, Tan JW, Yip K, Zheng MH, et al. Calcium/calmodulin-dependent kinase activity is required for efficient induction of osteoclast differentiation and bone resorption by receptor activator of nuclear factor kappa B ligand (RANKL) J Cell Physiol. 2007;212(3):787–795. doi: 10.1002/jcp.21076. [DOI] [PubMed] [Google Scholar]
- 4.Araújo AS, Fernandes AB, Maciel JV, Netto JN, Bolognese AM. New methodology for evaluating osteoclastic activity induced by orthodontic load. J Appl Oral Sci. 2015;23(1):19–25. doi: 10.1590/1678-775720140351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bloemen V, Schoenmaker T, de Vries TJ, Everts V. Direct cell-cell contact between periodontal ligament fibroblasts and osteoclast precursors synergistically increases the expression of genes related to osteoclastogenesis. J Cell Physiol. 2010;222(3):565–573. doi: 10.1002/jcp.21971. [DOI] [PubMed] [Google Scholar]
- 6.Boyce BF, Xing L. Functions of RANKL/RANK/OPG in bone modeling and remodeling. Arch Biochem Biophys. 2008;473(2):139–146. doi: 10.1016/j.abb.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen Y, Alman BA. Wnt pathway, an essential role in bone regeneration. J Cell Biochem. 2009;106(3):353–362. doi: 10.1002/jcb.22020. [DOI] [PubMed] [Google Scholar]
- 8.Gao L, Blair LA, Marshall J. CaMKII-independent effects of KN93 and its inactive analog KN92: reversible inhibition of L-type calcium channels. Biochem Biophys Res Commun. 2006;345(4):1606–1610. doi: 10.1016/j.bbrc.2006.05.066. [DOI] [PubMed] [Google Scholar]
- 9.Hoeflich KP, Ikura M. Calmodulin in action: diversity in target recognition and activation mechanisms. Cell. 2002;108(6):739–742. doi: 10.1016/s0092-8674(02)00682-7. [DOI] [PubMed] [Google Scholar]
- 10.Huiskes R, Ruimerman R, van Lenthe GH, Janssen JD. Effects of mechanical forces on maintenance and adaptation of form in trabecular bone. Nature. 2000;405(6787):704–706. doi: 10.1038/35015116. [DOI] [PubMed] [Google Scholar]
- 11.Kaneuji T, Ariyoshi W, Okinaga T, Toshinaga A, Takahashi T, Nishihara T. Mechanisms involved in regulation of osteoclastic differentiation by mechanical stress-loaded osteoblasts. Biochem Biophys Res Commun. 2011;408(1):103–109. doi: 10.1016/j.bbrc.2011.03.128. [DOI] [PubMed] [Google Scholar]
- 12.Kanzaki H, Chiba M, Shimizu Y, Mitani H. Dual regulation of osteoclast differentiation by periodontal ligament cells through RANKL stimulation and OPG inhibition. J Dent Res. 2001;80(3):887–891. doi: 10.1177/00220345010800030801. [DOI] [PubMed] [Google Scholar]
- 13.Kanzaki H, Chiba M, Shimizu Y, Mitani H. Periodontal ligament cells under mechanical stress induce osteoclastogenesis by receptor activator of nuclear factor kappaB ligand up-regulation via prostaglandin E2 synthesis. J Bone Miner Res. 2002;17(2):210–220. doi: 10.1359/jbmr.2002.17.2.210. [DOI] [PubMed] [Google Scholar]
- 14.Kim BJ, Lee YS, Lee SY, Park SY, Dieplinger H, Yea K, et al. Afamin stimulates osteoclastogenesis and bone resorption via Gi-coupled receptor and Ca2+/calmodulin-dependent protein kinase (CaMK) pathways. J Endocrinol Invest. 2013;36(10):876–882. doi: 10.3275/8975. [DOI] [PubMed] [Google Scholar]
- 15.Kong YY, Feige U, Sarosi I, Bolon B, Tafuri A, Morony S, et al. Activated T cells regulate bone loss and joint destruction in adjuvant arthritis through osteoprotegerin ligand. Nature. 1999;402(6759):304–309. doi: 10.1038/46303. [DOI] [PubMed] [Google Scholar]
- 16.Lee YH, Nahm DS, Jung YK, Choi JY, Kim SG, Cho M, et al. Differential gene expression of periodontal ligament cells after loading of static compressive force. J Periodontol. 2007;78(3):446–452. doi: 10.1902/jop.2007.060240. [DOI] [PubMed] [Google Scholar]
- 17.Li Y, Li M, Tan L, Huang S, Zhao L, Tang T, et al. Analysis of time-course gene expression profiles of a periodontal ligament tissue model under compression. Arch Oral Biol. 2013;58(5):511–522. doi: 10.1016/j.archoralbio.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 18.Li Y, Zheng W, Liu JS, Wang J, Yang P, Li ML, et al. Expression of osteoclastogenesis inducers in a tissue model of periodontal ligament under compression. J Dent Res. 2011;90(1):115–120. doi: 10.1177/0022034510385237. [DOI] [PubMed] [Google Scholar]
- 19.Liu L, Igarashi K, Kanzaki H, Chiba M, Shinoda H, Mitani H. Clodronate inhibits PGE(2) production in compressed periodontal ligament cells. J Dent Res. 2006;85(8):757–760. doi: 10.1177/154405910608500813. [DOI] [PubMed] [Google Scholar]
- 20.Nishijima Y, Yamaguchi M, Kojima T, Aihara N, Nakajima R, Kasai K. Levels of RANKL and OPG in gingival crevicular fluid during orthodontic tooth movement and effect of compression force on releases from periodontal ligament cells in vitro. Orthod Craniofac Res. 2006;9(2):63–70. doi: 10.1111/j.1601-6343.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- 21.Park-Min KH, Ji JD, Antoniv T, Reid AC, Silver RB, Humphrey MB, et al. IL-10 suppresses calcium-mediated costimulation of receptor activator NF-kappa B signaling during human osteoclast differentiation by inhibiting TREM-2 expression. J Immunol. 2009;183(4):2444–2455. doi: 10.4049/jimmunol.0804165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ren Y, Maltha JC, Kuijpers-Jagtman AM. Optimum force magnitude for orthodontic tooth movement: a systematic literature review. Angle Orthod. 2003;73(1):86–92. doi: 10.1043/0003-3219(2003)073<0086:OFMFOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Roberts WE, Goodwin WC, Jr, Heiner SR. Cellular response to orthodontic force. Dent Clin North Am. 1981;25(1):3–17. [PubMed] [Google Scholar]
- 24.Sağlam M, Köseoğlu S, Hatipoğlu M, Esen HH, Köksal E. Effect of sumac extract on serum oxidative status, RANKL/OPG system and alveolar bone loss in experimental periodontitis in rats. J Appl Oral Sci. 2015;23(1):33–41. doi: 10.1590/1678-775720140288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saito A, Miyajima K, Akatsuka J, Kondo H, Mashiko T, Kiuchi T, et al. CaMKIIbeta-mediated LIM-kinase activation plays a crucial role in BDNF-induced neuritogenesis. Genes Cells. 2013;18(7):533–543. doi: 10.1111/gtc.12054. [DOI] [PubMed] [Google Scholar]
- 26.Sokos D, Everts V, de Vries TJ. Role of periodontal ligament fibroblasts in osteoclastogenesis: a review. J Periodontal Res. 2015;50(2):152–159. doi: 10.1111/jre.12197. [DOI] [PubMed] [Google Scholar]
- 27.Souza CF, Carneiro AB, Silveira AB, Laranja GA, Silva MA, Neto, Costa SC, et al. Heme-induced Trypanosoma cruzi proliferation is mediated by CaM kinase II. Biochem Biophys Res Commun. 2009;390(3):541–546. doi: 10.1016/j.bbrc.2009.09.135. [DOI] [PubMed] [Google Scholar]
- 28.Tanaka S. Signaling axis in osteoclast biology and therapeutic targeting in the RANKL/RANK/OPG system. Am J Nephrol. 2007;27(5):466–478. doi: 10.1159/000106484. [DOI] [PubMed] [Google Scholar]
- 29.Wise GE, King GJ. Mechanisms of tooth eruption and orthodontic tooth movement. J Dent Res. 2008;87(5):414–434. doi: 10.1177/154405910808700509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu Y, Yang Y, Yang P, Gu Y, Zhao Z, Tan L, et al. The osteogenic differentiation of PDLSCs is mediated through MEK/ERK and p38 MAPK signalling under hypoxia. Arch Oral Biol. 2013;58(10):1357–1368. doi: 10.1016/j.archoralbio.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 31.Yasuda H, Shima N, Nakagawa N, Yamaguchi K, Kinosaki M, Mochizuki S, et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc Natl Acad Sci U S A. 1998;95(7):3597–3602. doi: 10.1073/pnas.95.7.3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zheng F, Liang H, Liu R, Quan JX, Li XX, Dai CL, et al. Parathyroid hormone-related protein regulates osteoclast inhibitory lectin expression via multiple signaling pathways in osteoblast-like cells. Endocrine. 2009;35(1):47–56. doi: 10.1007/s12020-008-9118-2. [DOI] [PubMed] [Google Scholar]