Abstract
Aim
The aim of the present study was to investigate the occurrence of postoperative delirium (POD) in elderly patients undergoing transurethral resection of prostate (TURP) and to identify those factors associated with delirium.
Methods
From July 2010 to February 2015, 358 patients, aged ≥65 years and undergoing TURP were prospectively enrolled. Personal, medical and cognitive data, laboratory assessments, pain intensity, preoperative medications, and details of hemodynamic control were collected as predictors of delirium. POD was assessed using the Confusion Assessment Method.
Results
In the present study, POD occurred in 28 out of 358 cases (7.8%) after TURP, with duration of 1–4 days. The multivariate analysis showed that old age and visual analog scale pain scores were associated with POD. Marital status, body mass index, education, alcohol consumption, smoking history, preoperative psychotropic medication usage, activities of daily living scores, preoperative Mini-Mental Status Examination score, anesthesia type, American Society of Anesthesiologists classification, or hypotensive episodes during surgery did not significantly correlate with the occurrence of POD.
Conclusion
Old age and pain intensity after surgery were found as the risk factors for the development of delirium in elderly patients undergoing TURP. These findings might help develop preventive strategies to decrease POD through targeted evaluation.
Keywords: elderly, postoperative delirium, risk factors, transurethral resection of prostate
Introduction
Delirium is an acute confusional state characterized by disturbance of consciousness, reduced ability to maintain attention and memory impairment, and known to occur usually in the elderly people.1 Its prevalence is known to increase during the perioperative period and the resultant delirium can cause major medical management problems. Postoperative delirium (POD) is associated with severe obstacles to increased lengths of hospital stay, costs, morbidity, and mortality.2,3 Investigations have spanned various surgical fields, and several previous reviews indicate that the incidence of POD varies from 10% to 46% in general surgical population.4,5 To date, previous studies of POD included too few patients undergoing urological surgery, and no trials have specifically examined POD in elderly patients undergoing transurethral resection of prostate (TURP).
Old age and cognitive impairment act as most common predisposing factors for POD have been identified within various cohort studies.4 However, wide variations reported the incidence and significance of other risk factors depend on the heterogeneity of clinical cohorts include methodological differences between the studies and study of population characteristics.6 Multicomponent interventions to prevent delirium are the most effective and nursing care have shown to decrease the incidence of delirium, and prophylactic use of haloperidol diminished the severity and duration of delirium.7,8 Benign prostatic hyperplasia has been known as a cause of lower urinary tract dysfunction and the most prevalent disease affecting the aging men. Fifty percent of men over the age of 50 years and 90% of men at the age of 80 years will have an enlarged prostate.9 TURP has, for decades, been the standard surgical therapy for lower urinary tract symptoms secondary to benign prostatic hyperplasia. Therefore, a more complete understanding of the incidence of, and potential risk factors responsible for, delirium in older patients undergoing TURP is needed.
Methods
Study population
In this prospective cohort study, we enrolled all patients aged 65 years and older, who were scheduled to undergo TURP during the period January 2010 to February 2015 at a single medical center in the People’s Republic of China. Surgical procedures and postoperative treatment protocols used in the study were based on clinical guidelines for urological surgery. Exclusion criteria included cognitive impairment such as Alzheimer’s disease, dementia, or preoperative depression. Seven patients were excluded from the study, and the remaining 358 patients were invited to participate in the study after having received detailed information in both oral and written form. There was no patient who developed delirium before surgery in this study.
Clinical assessment
Recorded possible confounding factors included age, education level, body mass index, marital status, smoking history, alcohol consumption, preexisting disease, preoperative psychotropic medication usage, surgical procedure time, pain intensity, type of anesthesia, American Society of Anesthesiologists classification, hypotensive episodes during surgery, activities of daily living scores, preoperative Mini-Mental Status Examination score, and laboratory information. Pharmacological treatment on admission was recorded, in particular the use of benzodiazepines, neuroleptics (antipsychotics), or drugs with anticholinergic effects. Routine preoperative blood test was performed, including complete blood count, electrolyte panel, liver function test, and thyroid hormones. Chest radiogram and electrocardiogram were also collected.
Delirium evaluation
Clinical features of delirium were evaluated by nursing staff and documented in daily nursing records. Preoperative cognitive status was evaluated using mini-mental state examination. Different cutoff scores were used to measure baseline cognitive status. All the patients were evaluated postoperatively for delirium using the Confusion Assessment Method, for a week and at the onset of confusion-related symptoms, according to the DSM-IV TR. Confusion Assessment Method scores are determined using a diagnostic algorithm consists of four clinical criteria: 1) acute onset or fluctuating course, 2) inattention, 3) disorganized or incoherent thinking, and 4) alteration in alertness. Diagnosis of delirium was made if the first and second criteria are present and either criterion three or four is present.
Postoperative pain measurement and management
General anesthesia or spinal anesthesia was administered for endoscopic surgery and may reduce postoperative pain. However, bladder irrigation and/or irritation from catheters can provoke detrusor reflex contractions and the urge to void. People who have had such bladder spasms describe them as a cramping pain. A trained research assistant asked all health service patients to assess whether they had been aware of any discomfort after TURP using a verbal version of the visual analog scale (VAS) ranging from “no pain” to “very severe pain”. Patients were asked to record their pain intensity both at rest preoperatively and on postoperative days 1 and 2. Pain intensity was measured at the same time that patients were evaluated for delirium. Tolterodine and/or intravesical bupivacaine were used as analgesia in patients with bladder spasm after prostate operation.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation and categorical variables are presented as percentages. The Mann–Whitney U-test was used to compare the mean of the continuous variables between patients with delirium and those without the syndrome. The chi-square test was performed to assess the differences in categorical variables between the two comparison groups. A multivariate logistic regression model was used to identify the most important risk factors for developing POD included variables with a significant trend on univariate analysis. Significance was established at P<0.05. All statistical analyses were performed using the statistical package SPSS for Windows (Version 18, SPSS, Chicago, IL, USA).
Ethical approval
All human studies were approved by the Institutional Ethics Committee of First People’s Hospital of Lianyungang and performed after obtaining written informed consent. All procedures performed in studies involving human participants were in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Results
Of the 358 patients studied, delirium was diagnosed in 28 (7.8%) patients after TURP. Twenty-one patients developed symptoms of delirium on postoperative day 1, and seven patients on postoperative day 2, with symptoms lasting for 1–4 days. Patients who developed POD on either of the postoperative days tended to be older, had more comorbidity, and experienced significantly higher VAS scores (Table 1).
Table 1.
Demographics and clinical characteristics (n=358)
| Demographic and clinical data | Delirious (n=28) | Non-delirious (n=330) | P-value |
|---|---|---|---|
| Age (years)a | 78.14±5.33 | 74.84±6.39 | 0.004 |
| Marital statusb | 0.110 | ||
| Married | 22 | 293 | |
| Single | 6 | 37 | |
| Education (years)a | 9.60±1.96 | 10.00±1.63 | 0.233 |
| BMI (kg/m2)a | 20.93±1.36 | 20.62±1.74 | 0.270 |
| Active alcohol consumptionb | 0.612 | ||
| None | 17 | 184 | |
| Yes | 11 | 146 | |
| Pack-years smokinga | 10.79±8.55 | 11.56±8.53 | 0.650 |
| Preoperative psychotropic medication usageb | 0.306 | ||
| No | 21 | 273 | |
| Yes | 7 | 57 | |
| Preoperative MMSE scorea | 27.86±1.76 | 28.40±1.31 | 0.119 |
| ADL scorea | 5.2±0.9 | 5.5±0.6 | 0.812 |
| Number of co-existent medical conditionsb | 0.048 | ||
| 0 and 1 | 13 | 215 | |
| ≥2 | 15 | 115 | |
| Anesthesia typeb | 0.570 | ||
| General | 17 | 182 | |
| Spinal | 11 | 148 | |
| ASA classificationb | 0.214 | ||
| 1 and 2 | 22 | 287 | |
| ≥3 | 6 | 43 | |
| Hypotension during surgeryb | 0.668 | ||
| No | 21 | 259 | |
| Yes | 7 | 71 |
Notes:
Data are shown as mean ± standard deviation and were compared using the Mann–Whitney U-test.
Data are shown as n and were compared using the chi-square test. Bold values indicate P<0.05.
Abbreviations: ADL, activities of daily living; ASA, American Society of Anesthesiologists; BMI, body mass index; MMSE, Mini-Mental Status Examination.
The preoperative VAS scores were not significantly different between patients who subsequently developed POD and those who did not (Figure 1). In contrast, patients who were delirious postoperatively experienced significantly more pain than non-delirious patients (for postoperative day 1: mean postoperative VAS at rest 3.79±0.93 vs 2.42±0.83, P=0.021; and for postoperative day 2: mean postoperative VAS at rest 2.71±0.82 vs 2.05±0.76, P=0.025).
Figure 1.
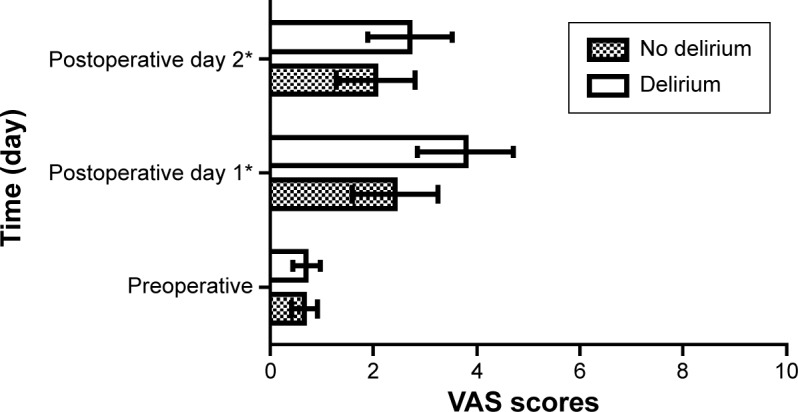
The VAS pain scores for patients with and without postoperative delirium in the preoperative period and postoperative period are shown.
Note: *P<0.05.
Abbreviation: VAS, visual analog scale.
Hypotension during surgical procedures was more frequent (25%) in the delirious patients than in the non-delirious patients (21.5%), but the difference was not statistically significant. No differences were seen in delirious compared with non-delirious patients in anesthesia type in both groups. There was no difference between patients with or without delirium and preoperative psychotropic medication usage (Table 1). Multivariate analysis suggested that higher VAS scores (odds ratio =4.45, 95% confidence interval: 1.69–6.58) and older age (odds ratio =3.85, 95% confidence interval: 1.60–9.27) were associated with the occurrence of POD (Table 2).
Table 2.
Factors associated with the development of delirium after TURP
| Parameters | Odds ratio | 95% CI | P-value |
|---|---|---|---|
| Age | 3.85 | 1.60–9.27 | 0.003 |
| VAS pain scores | 4.45 | 1.69–6.58 | 0.012 |
Abbreviations: CI, confidence interval; TURP, transurethral resection of prostate; VAS, visual analog scale.
Discussion
Varying incidences of POD have been reported in different studies. Previous reviews noted that the incidence of delirium ranges from 10% to 46% in general surgical population.4,5 The risk factors included older age, cognitive impairment, illness severity, psychopathological symptoms, preoperative depression, preoperative psychotropic drug use, greater comorbidity, and perioperative complications.6
The incidence of POD was 7.8% in this study, which is similar to a previous study (incidence: 8.8%) that investigated 90 patients (81 males and nine females; average age of 74.3±0.40 years) undergoing urological surgery.10 However, Our findings were lower than another studies reported 29% incidence in elderly patients after radical cystectomy.11 In accord with previous studies, delirium most often occurred in the early postoperative period and the likelihood of delirium decreased over time.12,13 The present study showed that endoscopic urological surgery is associated with low rate of delirium. Conventional TURP continues to be the most common treatment in the operative management of benign prostatic hypertrophy, and it is a less traumatic procedure than major surgery. Usually, TURP is a selective operation; thus, the patients are well prepared by the procedure. It means that avoiding anemia, infection, electrolyte disorders, hormonal disorder, neurological dysfunction, dehydration, renal failure, and other identified potential confounding factors probably lowers the onset of POD.
In our study, older age and postoperative pain were significantly associated with the development of POD on multivariate analysis. Previous studies have also demonstrated that advanced age is a consistent, well-established risk factor for the development of delirium.3,14 In our study, the delirious group was, on average, 3 years older than the non-delirious group. Here only older patients were analyzed, 65 years of age and older. Pain intensity after surgery was found to be the risk factor for delirium in the present study, which was similar to previous published studies.15,16 Bladder irrigation after TURP and/or irritation from catheters is often distressing because of pain arising from detrusor muscle spasm. People who have had such spasms describe them as a cramping pain and sometimes as a burning sensation. Common causes include surgery, irritation from catheters, and urinary tract infections. Our date showed that patients with POD had significantly higher VAS scores for pain following surgery than those who were not delirious. The overall severity of postoperative bladder spasm can be reduced with opioids, anticholinergic medication, and sedatives. Although many patients need pain medication for postoperative pain control, there is some controversy over whether opioid use may itself be a risk factor for delirium.17,18 Medication use, particularly anticholinergic medications, has long been recognized as a common precipitating risk factor for the development of delirium. Anticholinergics work by blocking the effects of acetylcholine in the substantia nigra. It is hypothesized that acetylcholine is one of the brain’s natural neurotransmitters that may be involved in the pathogenesis and development of delirium.19 In a randomized controlled trial, the use of tolterodine was shown to have a low incidence of central nervous system side effects and was effective in the treatment of older patients with urinary symptoms attributable to overactive bladder.20 In this study, tolterodine is largely used as analgesia in patients with bladder spasm after prostate operation. Nonetheless, pain status may be a confounding factor rather than a sufficient reason for the increased rate of delirium in these trials. In addition, replacing opioids with other medications such as intravesical bupivacaine has also been used as a new method to suppress postoperative bladder spasm.21
A recent study has shown that anesthesia based on sevoflurane carries a predictive value for the development of delirium in elderly patients after major abdominal surgery.22 In the present analysis, however, anesthesia type was not a significant risk factor for POD. It has also been reported that hypotensive episodes intrasurgery, activities of daily living scores are associated with the development of POD in geriatric patients after urologic surgery.10 In the current study, we found that hypotension during surgery, activities of daily living scores, alcohol consumption, smoking history, and intraoperative and postoperative narcotic usage were not predictive of POD. However, the mechanism underlying the development of POD is controversial, and predisposing and precipitating risk factors for developing delirium after urological surgery have not been well investigated. Identification of potentially modifiable risk factors provides an opportunity for effective intervention.
A systematic review of published studies showed great inconsistencies in definition, incidence, severity, and duration of POD.23 Therefore, the effective identification, prevention, and treatment of pre-, intra-, and postoperative risk factors are the cornerstones for the prevention of POD. However, heterogeneity of the trials and the small sample sizes precluded conclusions regarding the interventions that are likely to prevent POD. The limited data suggested that the appropriate anesthesia strategy, qualified nursing surveillance, a tailored selection of drugs used perioperatively, systematic use of diagnostic tools, and accurate staff communication reduce the incidence and clinical impact of POD.24
In addition to cognitive failures, urination disorders are a common symptom in patients with dementia and Alzheimer’s disease. In principle, all medical treatment options are available for those patients with cognitive impairment. However, the extent and invasivity of therapeutic methods should be adapted to the individual patient. In most of the cases, outpatients with cognitive impairment receive conservative treatment rather than urological surgery in our hospital. The limitations of this study included the exclusion of patients with cognitive impairment and preoperative depression, which would lessen the incidence of delirium, as cognitive impairment and preoperative depression are also a risk factor for delirium.6 In this study, pain measurement was used at the same time of delirium assessment to represent the pain level for each specific postoperative day. Using subjective instrument such as the VAS for measuring pain may pose a substantial problem in subjects with perceptual impairments such as POD, as the validity and reliability for the evaluation is uncertain. However, further investigations in this direction would be required to confirm this. Additionally, pharmacological interventions were not further explored and this may be an important confounder in some studies. Despite these limitations, the strengths of the study are its prospective design and the relatively large population of elderly patients participating in this study.
Conclusion
In conclusion, delirium occurred in approximately 7.8% of elderly patients with benign prostatic hyperplasia undergoing TURP. A higher postoperative VAS score and older age were significantly associated with the development of POD. The two identified predictors can be used to identify patients at increased risk for POD after TURP, and it provides an opportunity for effective intervention.
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Inouye SK. Delirium in older persons. N Engl J Med. 2006;354(11):1157–1165. doi: 10.1056/NEJMra052321. [DOI] [PubMed] [Google Scholar]
- 2.Marcantonio ER, Kiely DK, Simon SE, et al. Outcomes of older people admitted to postacute facilities with delirium. J Am Geriatr Soc. 2005;53(6):963–969. doi: 10.1111/j.1532-5415.2005.53305.x. [DOI] [PubMed] [Google Scholar]
- 3.Bucht G, Gustafson Y, Sandberg O. Epidemiology of delirium. Dement Geriatr Cogn Disord. 1999;10(5):315–318. doi: 10.1159/000017161. [DOI] [PubMed] [Google Scholar]
- 4.Mittal V, Muralee S, Williamson D, et al. Review: delirium in the elderly: a comprehensive review. Am J Alzheimers Dis Other Demen. 2011;26(2):97–109. doi: 10.1177/1533317510397331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deiner S, Silverstein JH. Postoperative delirium and cognitive dysfunction. Br J Anaesth. 2009;103(Suppl 1):i41–i46. doi: 10.1093/bja/aep291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dasgupta M, Dumbrell AC. Preoperative risk assessment for delirium after noncardiac surgery: a systemic review. J Am Geriatr Soc. 2006;54(10):1578–1589. doi: 10.1111/j.1532-5415.2006.00893.x. [DOI] [PubMed] [Google Scholar]
- 7.Milisen K, Lemiengre J, Braes T, Foreman MD. Multicomponent intervention strategies for managing delirium in hospitalized older people: systematic review. J Adv Nurs. 2005;52(1):79–90. doi: 10.1111/j.1365-2648.2005.03557.x. [DOI] [PubMed] [Google Scholar]
- 8.Kalisvaart K, de Jonghe J, Bogaards M, et al. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr. 2005;53(10):1658–1666. doi: 10.1111/j.1532-5415.2005.53503.x. [DOI] [PubMed] [Google Scholar]
- 9.Sausville J, Naslund M. Benign prostatic hyperplasia and prostate cancer: an overview for primary care physicians. Int J Clin Pract. 2010;64(13):1740–175. doi: 10.1111/j.1742-1241.2010.02534.x. [DOI] [PubMed] [Google Scholar]
- 10.Tognoni P, Simonato A, Robutti N, et al. Preoperative risk factors for postoperative delirium (POD) after urological surgery in the elderly. Arch Gerontol Geriatr. 2011;52(3):e166–e169. doi: 10.1016/j.archger.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 11.Large MC, Reichard C, Williams JT, et al. Incidence, risk factors, and complications of postoperative delirium in elderly patients undergoing radical cystectomy. Urology. 2013;81(1):123–128. doi: 10.1016/j.urology.2012.07.086. [DOI] [PubMed] [Google Scholar]
- 12.Amador LF, Goodwin JS. Postoperative delirium in the older patient. J Am Coll Surg. 2005;200(5):767–773. doi: 10.1016/j.jamcollsurg.2004.08.031. [DOI] [PubMed] [Google Scholar]
- 13.Marcantonio ER, Goldman L, Orav EJ, Cook EF, Lee TH. The association of intraoperative factors with the development of postoperative delirium. Am J Med. 1998;105(5):380–384. doi: 10.1016/s0002-9343(98)00292-7. [DOI] [PubMed] [Google Scholar]
- 14.Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168(1):27–32. doi: 10.1001/archinternmed.2007.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leung JM, Sands LP, Paul S, Joseph T, Kinjo S, Tsai T. Does postoperative delirium limit the use of patient-controlled analgesia in older surgical patients? Anesthesiology. 2009;111(3):625–631. doi: 10.1097/ALN.0b013e3181acf7e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robinson S, Vollmer C, Jirka H. Aging and delirium: too much or too little pain medication? Pain Manag Nurs. 2008;9(2):66–72. doi: 10.1016/j.pmn.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Sieber FE, Mears S, Lee H, Gottschalk A. Postoperative opioid consumptionand its relationship to cognitive function in older adults with hip fracture. J Am Geriatr Soc. 2011;59:2256–2262. doi: 10.1111/j.1532-5415.2011.03729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fong HK, Sands LP, Leung JM. The role of postoperative analgesia in delirium and cognitive decline in elderly patients: a systematic review. Anesth Analg. 2006;102:1255–1266. doi: 10.1213/01.ane.0000198602.29716.53. [DOI] [PubMed] [Google Scholar]
- 19.Tune LE, Egeli S. Acetylcholine and delirium. Dement Geriatr Cogn Disord. 1999;10(5):342–344. doi: 10.1159/000017167. [DOI] [PubMed] [Google Scholar]
- 20.Malone-Lee JG, Walsh JB, Maugourd MF. Tolterodine: a safe and effective treatment for older patients with overactive bladder. J Am Geriatr Soc. 2001;49(6):700–705. doi: 10.1046/j.1532-5415.2001.49144.x. [DOI] [PubMed] [Google Scholar]
- 21.Chiang D, Ben-Meir D, Pout K, Dewan PA. Management of post-operative bladder spasm. J Paediatr Child Health. 2005;41(1–2):56–58. doi: 10.1111/j.1440-1754.2005.00537.x. [DOI] [PubMed] [Google Scholar]
- 22.Zabolotskikh IB, Trembach NV. Effect of anaesthesia on incidence of postoperative delirium after major abdominal surgery in elderly patients. Anesteziol Reanimatol. 2013;(6):4–7. [PubMed] [Google Scholar]
- 23.Zhang H, Lu Y, Liu M, et al. Strategies for prevention of postoperative delirium: a systematic review and meta-analysis of randomized trials. Crit Care. 2013;17(2):R47. doi: 10.1186/cc12566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bilotta F, Lauretta MP, Borozdina A, Mizikov VM, Rosa G. Postoperative delirium: risk factors, diagnosis and perioperative care. Minerva Anestesiol. 2013;79(9):1066–1076. [PubMed] [Google Scholar]


