Abstract
Background
With the development of conservative mastectomies, there are an increasing number of women seeking immediate implant based and autologous breast reconstruction. Despite the oncologic safety of the procedures, the focus will be on the timing of reconstruction.
Methods
Our plastic surgery unit is focused primarily on autologous breast reconstruction and is part of an interdisciplinary breast center. We offer immediate breast reconstruction (IBR) with autologous tissue for patients with positive BRCA 1 and 2, ductal carcinoma in situ (DCIS), invasive cancer without margin problems to the skin, as well as to correct poor oncologic and aesthetic breast conserving therapy (BCT) outcomes. In the majority of cases we prefer an Immediate-DElayed AutoLogous (IDEAL) breast reconstruction concept with a two-stage procedure.
Results
Over the last 10 years we performed more than 1,600 breast reconstructions with free flaps, performing the deep inferior epigastric perforator (DIEP) flap as our first choice for autologous tissue. We recommend IDEAL breast reconstruction, however approximately 15% of our cases are immediate one stage conservative mastectomies and breast reconstruction with the DIEP flap.
Conclusions
For immediate reconstruction, the aesthetic outcome should not take precedence over oncologic considerations. Immediate one-stage, breast reconstruction with autologous tissue can be offered to the suitable patients which is most likely a healthy women with a small-to-medium sized non ptotic breast receiving a conservative mastectomy. In all other cases, we recommend an IDEAL breast reconstruction approach in order to achieve a final result that is both satisfyingly pleasing and oncologically safe.
Keywords: Mastectomy, deep inferior epigastric perforator flap (DIEP flap), immediate-delayed reconstruction, oncoplastic surgery
Introduction
Breast cancer is the most common cancer affecting woman, appearing with a lifetime risk of up to 10%. As a method of treatment, one third of the patients diagnosed with breast cancer receive a mastectomy of various oncological extents resulting in a reconstructive challenge for the oncoplastic surgeon (1). Between 2005 and 2011 the mastectomy rate in the US increased up to 51% with an increasing number of patients receiving bilateral prophylactic mastectomy with immediate reconstruction (2). The term “conservative mastectomies” was first used by Nava et al. in 2009. It outlined the need for preservation of mammary appearance, biomechanical balance, adequate volume restoration and symmetrical scarring in oncoplastic surgery (3,4). Moreover, the most common form of conservative techniques became the implant based breast reconstructions. Nava sees an increasing need of autologous breast reconstruction through increased indications for radiotherapy and therefore an unaccepted rate of capsular contractures and radiodermatitis in implant based reconstruction (3,5).
Breast reconstruction should always be attempted in a multidisciplinary approach. An optimal oncologic and surgical treatment takes the following into consideration:
Breast conserving therapy (BCT);
Mastectomy;
Skin sparing mastectomy (SSM);
Nipple sparing mastectomy (NSM).
Breast reconstruction following surgical treatment of breast cancer takes the choice of alloplastic or autologous reconstruction and the timing of reconstruction into consideration:
Implant vs. autologous reconstruction;
Immediate vs. delayed reconstruction.
Implant based breast reconstruction
Implant based breast reconstruction has many advantages, but to achieve the best results, the ideal indications must be met. When there is a lack of sufficient soft tissue coverage, the need of acellular dermal matrix (ADM) lead to substandard results. In addition, the possibility of pre- and post-reconstruction radiotherapy leads to a high rate of capsular contractures and with this, there is a high rate of secondary procedures involving capsular removement and implant changes (6,7).
Autologous breast reconstruction
Considering the high rate of complications in implant based breast reconstruction including capsular contracture and the need for implant removal, reconstruction with autologous tissue is preferable to implant based reconstructions, especially after radiation therapy (6,8-10). The downside of radiation therapy following autologous reconstruction is that it leads to inferior aesthetic results, such as fat necrosis and skin fibrosis.
Immediate vs. delayed reconstruction
The decision between immediate and delayed reconstruction is complex and needs to be approached in a multidisciplinary fashion. It is important to take the patient’s choice into consideration, the need for postoperative radiotherapy, the extent of the disease, as well as other medical conditions, such as bleeding complications that may favor one method over the other.
Immediate breast reconstruction (IBR)—advantages
Decreased risk of social or emotional difficulties;
Better cosmetic results;
Possibly fewer surgeries and lower surgery cost;
No difference in rate of development of local cancer recurrence;
No difference in the ability to detect local cancer recurrence.
Immediate breast reconstruction (IBR)—disadvantages
Possible skin and nipple perfusion problems;
Indications for radiation therapy unclear;
Longer hospitalization and recovery times than mastectomy alone;
More scarring than mastectomy alone;
Surgery prolonged;
Reimbursement is difficult.
Immediate-DElayed AutoLogous (IDEAL) breast reconstruction—advantages
Best option to maintain the balance between optimal aesthetic outcomes and effective radiation delivery (11);
Minimizing unpleasant aesthetic outcomes (contracture, distortions);
Revision of the inframammary fold;
Debridement of any nonviable mastectomy skin (if present) before the insetting of an autologous tissue flap (12).
IDEAL breast reconstruction—disadvantages
More surgeries and hospitalizations;
Possibly increased risk of social or emotional difficulties;
Prolonged and elongated time of therapy;
Higher costs.
Radiotherapy and immediate breast reconstruction (IBR)
The challenge in breast reconstruction remains to preoperatively predict the probability of the necessity of post mastectomy radiotherapy (PMRT). However, when immediate reconstructions are irradiated, the outcome might be compromised. The patient with an implant may develop capsular fibrosis. On the other hand, with a tissue flap there may be distortion and shrinkage of the tissue (5,7,13). In a meta-analysis overlooking 28 studies with autologous reconstruction published by Schaverien et al., their conclusion found an increased risk of fat necrosis and a higher portion of revisional surgery after IBR and post mastectomy radiation therapy compared to delayed immediate reconstruction. They did however report satisfactory outcomes with adjuvant radiation therapy (14).
The ideal breast for primary autologous reconstruction
In a youthful, full and non ptotic breast, as often presented in patients with BRCA 1/2 mutations seeking prophylactic mastectomies, an immediate reconstruction after SSM can be performed using a uni- or bilateral deep inferior epigastric perforator (DIEP) flap. However, the one stage approach leads to a longer duration of the surgery and therefore increases the general intraoperative risks.
The average breast for primary autologous reconstruction
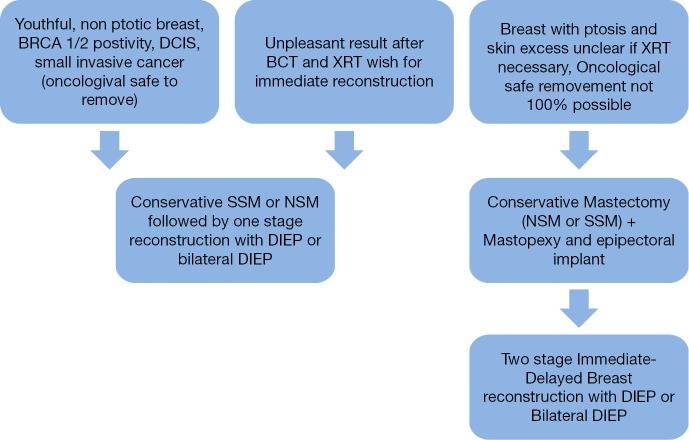
The patient presenting with a ptotic and large breast, which makes up the majority of our patients on the other hand, is more feasible for an IDEAL two-stage reconstruction approach. In a primary procedure, the tumor removal can be combined with a mastopexy of the skin; therefore the secondary autologous reconstruction has the ideal setting to achieve an aesthetic pleasing result (Figure 1).
Figure 1.
Timing and concept of breast reconstruction with the DIEP flap. DIEP, deep inferior epigastric perforator; DCIS, ductal carcinoma in situ; BCT, breast conserving therapy; XRT, radiation therapy; NSM, nipple sparing mastectomy; SSM, skin sparing mastectomy.
Material and methods
Autologous breast reconstruction with the DIEP flap
The DIEP flap was first described by Koshima et al. in 1989 and since has evolved to the work horse of autologous breast reconstruction (15-21). Over the last two decades, multiple free flap procedures have been performed, but after all, the DIEP flap procedure is the most feasible free flap for breast reconstruction. The benefits of the DIEP flap include all the benefits of the free transverse rectus abdominal myo-cutaneous (TRAM) flap without the donor site complications including abdominal hernias and weakness of the abdomen (16). Besides BCT and radiotherapy, the traditional concept of mastectomies, adjuvant therapy and delaying reconstruction is being supplemented by the increasing use of immediate reconstruction.
We have an interdisciplinary breast center that includes a department of senology for the oncologic treatment and a plastic surgery unit for the autologous breast reconstruction. Our plastic surgery unit specializes in breast reconstruction—over the last 10 years, we have performed over 1,600 free autologous breast reconstructions (8).
The crucial part of IBR with the DIEP flap is the right patient selection:
Indications:
Young healthy women;
Prophylactic mastectomy;
No PMRT needed.
Contraindications:
Classification of American Society of Anesthesiologists (ASA) >3;
Previous abdominoplasty or abdominal surgery (when perforators are destroyed);
Severe haematological disorders.
Preoperatively, all patients receive a CT angiography to detect the perforator vessel nourishing the abdominal skin flap. The markings preoperatively are performed with the patient in the standing up position. Standard abdominoplasty markings are applied to the donor side area. The midline and inframammary fold are marked as well as the perforators as detected in the CT angiography. The DIEP flap is performed on a daily basis with a two-team approach. Two surgeons perform the flap harvesting while another surgeon is dissecting the recipient vessels for which we use the internal mammary artery and vein. The dissection of the flap and the recipient vessels is performed bloodless with bipolar micro-forceps. After dissection of the relevant perforators, temporary clamping of all the perforators, except the main perforators, will be done. The flap is now evaluated and depending on the number of perforators needed, the decision is made to choose a DIEP or a MS-2-TRAM flap. By using this protocol with standard CT angiography and intraoperative clamping of the perforators and flap evaluation, we were able to reduce the number of MS-2-TRAM flaps to around 10% of all autologous breast reconstructions with a constant flap loss rate below 1%.
The dissection is always performed with bipolar hemostasis. Perioperatively, the patients receive a shot of 2 g cefazolin over 24 hours. After detaching the flap, it is cooled during ischemia and the anastomosis to the internal mammary vessels is done with 9.0 Prolene. First the vein and then the artery is anastomosed. The patients receive single shot of 2.500 IE heparin. We use fibrin glue for stabilization of the anastomosis to prevent kinking and torsion of the pedicle. The flap is warmed again after the anastomosis is done and the flap is reperfused. If the blood supply of the skin of the mastectomy flap is questionable, we insert the flap without de-epithelization and wait 4-6 days until we finish the reconstruction. Postoperatively the patients are monitored hourly and the flap is controlled via Doppler detection on the intensive care unit. The patients receive aspirin 100 mg p.o. daily for 6 weeks and low molecular weight heparin (LMWH) subcutaneously until complete ambulation. The patients get out of bed the first postoperative day and will usually be discharged between day 7 and 10. The postoperative schedule involves appointments in the outpatients clinic 1, 3, 6, and 12 months after surgery as described in previous reports (8).
Immediate-DElayed AutoLogous (IDEAL) breast reconstruction concept
Regarding the timing of breast reconstruction, many different concepts have been published (12,22). Our protocol of patient selection according to cancer status and breast form as well as for the timing of breast reconstruction is shown in Figure 1. It has been developed in close cooperation with our Department of Senology as part of our breast center.
In patients with youthful, non ptotic breast, presenting positive BRCA 1/2, ductal carcinoma in situ (DCIS), or small invasive cancer, an IBR could be feasible, either with autologous or alloplastic reconstruction. However, the conservative mastectomy should be oncologically safe and no radiotherapy after immediate reconstruction is needed (Figures 2,3,4).
Figure 2.

A 45-year-old woman with invasive breast cancer on the right side. Preoperative view.
Figure 3.

Result 3 months postoperatively after SSM + immediate bilateral breast reconstruction with a DIEP flap. SSM, skin sparing mastectomy; DIEP, deep inferior epigastric perforator.
Figure 4.

Result 3 years postoperatively after nipple reconstruction with star flaps and tattooing of the areolar complex.
To exclude an advanced tumor stage, a complete diagnostic workup consisting of mammography, breast ultra sound and MRI is recommended in these cases. Sentinel biopsy should always be done before immediate reconstruction to rule out the need for PMRT. Before we consider a one stage reconstruction, the patients have a sentinel lymph node biopsy performed to detect lymph node status. If positive, we recommend axilla dissection and radiation therapy, therefore a one-stage procedure is not advisable.
This approach can also be used with any dissatisfying and unpleasing results after BCT, or previous reconstruction (implant or autologous) and postoperative radiation therapy that has altered the aesthetic outcome resulting in skin damage and capsular contracture. Still, in patients with breast ptosis, skin excess or with the uncertainty whether oncological safety can be guaranteed with the cancer removal where they must be followed with postoperative radiation therapy, we prefer our immediate-delayed-breast reconstruction concept. However, in patients with breast ptosis and skin excess, or with unclear oncologic breast tissue removal or postoperative radiation therapy that is indicated, we prefer our immediate-delayed-breast reconstruction concept. This concept consists of conservative mastectomy (NSM or SSM) combined with a mastopexy if needed and epipectoral implant or expander (in case of SSM) positioning. The radiation therapy is done before the implant reconstruction in a neo-adjuvant setting.
Patients that receive radiotherapy after DIEP flap reconstruction show poorer outcomes than patients who do not undergo radiation after surgery (23). Rogers et al. states that immediate reconstructed DIEP flaps, exposed to radiotherapy, experience significantly increased rates of fat necrosis, fibrosis and contracture (23). The odds of the development of flap fat necrosis are almost three times higher when the flap was subjected to radiotherapy (24). Further, in the study of Motwani et al. it was concluded that IBR poses challenges for the treatment planning of post mastectomy radiation therapy because of suboptimal field coverage and organ protection (25). Thus, IBR is discouraged due to a potential risk of impaired tumor treatment and oncological surveillance (25). Patients who have their breast reconstructed before their radiotherapy are exposed to increased late complication rates (26) and unpredictable outcomes (23) due to which the timing of breast reconstruction has to be planned carefully.
After 3-6 months, the patients return for a secondary breast reconstruction with a DIEP flap. Also after BCT with poor outcomes an immediate delayed approach can be feasible (Figures 5,6).
Figure 5.

A 54-year-old woman with previous BCT and poor cosmetic outcome after radiation therapy and chemo therapy, immediate delayed concept. BCT, breast conserving therapy.
Figure 6.

Same patient 6 months postoperatively.
The skin or NSM is routinely performed by the breast surgeon (Figure 7). In case of NSM the skin incision is placed in an inferolateral submammary area. Viable skin flaps are important for later reconstruction. When autologous reconstruction using the DIEP flap is planned, the implant is placed epipectorally. In a second stage the flap is also placed in an epipectoral plane to avoid animation problems (Figure 8).
Figure 7.

Nipple sparing mastectomy with total breast tissue removement and preservation of blood supply to the skin.
Figure 8.

Skin necrosis after immediate reconstruction due to poor skin perfusion after mastectomy.
Timing of secondary procedures
If symmetricalisation procedures are needed 6-12 months after the breast reconstruction, patients receive a mastopexy of the contralateral side and a nipple reconstruction. For the nipple reconstruction we prefer the Star flap (3,27,28). The Areolar complex is usually tattooed.
Discussion
The role of oncoplastic surgery constantly rises and eventually leads to new concepts for a multidisciplinary treatment plan and team approach that consists not only of breast surgeons, but also oncologist and a plastic surgeon that discuss further treatment plans among each other (29). The possibility of conservative mastectomies provides the oncoplastic surgeon with an ideal basis for optimal skin saving, volume restoring and breast reshaping tissue transfer for results especially tailored to the patient’s oncological and anatomical situation (3,21).
The most important aspects to keep in mind with any form of breast reconstruction is the oncological safety.
Motwani et al. concluded that IBR poses challenges for the treatment planning of post mastectomy radiation therapy because of suboptimal field coverage and organ protection (25). Thus, a multidisciplinary team has to discuss the option of immediate vs. immediate-delayed-breast reconstruction in regards to a potential risk of impaired tumor treatment and oncological surveillance (25). Secondly, after the oncological and patient safety, the patient quality of life and cosmetics plays another role in the well-being of the patient and influences their choice for additional reoperations. The decision of an IBR should be undertaken carefully and in close dialogue with an oncologist to be able to plan the time of breast reconstruction with the possibility to “immediately-delay” the surgery for a better oncological and complication-free result (29) and to avoid, at its best, radiotherapy to the reconstructed breast. It is without a doubt that IBR following conservative mastectomies for poor outcomes after BCT can lead to excellent results that are oncological safe (30) with a low complication rate (8). Nevertheless it has to be taken into account that these results can be achieved mainly when the immediately reconstructed breast is not radiated afterwards. Since the exposure to radiotherapy causes increased late complication rates (26) and unpredictable outcomes (23). The risk of developing a fat necrosis of the immediately reconstructed flap is almost three times higher when the flap was subjected to radiotherapy (24).
IBR may impose limitations on the treatment planning of PMRT but the challenge remains to preoperatively predict the probability of the necessity of PMRT. Since PMRT influences implant based and autologous reconstruction alike in a negative manner (31,32), the patient should always be offered a delayed primary reconstruction if the need of PMRT is unclear, in order to avoid the exposure of the patients to consecutive operations and unsatisfying aesthetic results. It is important to have a good doctor-patient communication to inform and prepare the patient for the following treatment possibilities and tailor the reconstruction to the patient's needs, oncological state and anatomy.
In IBR after conservative mastectomies the perfusion of the breast envelope can sometimes be poor (Figure 8). Therefore, the concept of delayed de-epithelialization has been described and is a helpful tool in IBR, preventing poor outcomes with skin necrosis and extensive scaring and saves the patient of unnecessary re-operations and complications (33).
Last but not least, besides the oncological state of the patient, the shape of the breast is also an important factor in the timing of immediate versus delayed IBR (22). A youthful, non ptotic breast can be reconstructed in a single stage procedure while the average breast with ptosis and lax skin is preferred to be treated with the immediate delayed approach with mastopexy, epipectoral implant and finally autologous reconstruction using the DIEP flap in a second stage, thus called IDEAL breast reconstruction.
Conclusions
The ideal reconstruction is an individualized treatment plan. Immediate one stage breast reconstruction with a DIEP flap can be offered to the suitable patients which most likely is a healthy women with a small to medium size and non ptotic breast receiving prophylactic mastectomy. According to our selection criteria we offer patients immediate reconstruction with the DIEP flap. If risk of skin or nipple necrosis or tumor free margins cannot safely be achieved, and the patient would like autologous reconstruction, we prefer an IDEAL breast reconstruction approach. This approach consists of a conservative mastectomy followed by an immediate epipectoral implant placement, eventually combined with a skin reducing procedure. In a second stage 3-6 months later, the implant is removed and replaced by an autologous reconstruction favoring the DIEP flap. In no case should cosmetics take precedence over oncologic considerations.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Cordeiro PG. Breast reconstruction after surgery for breast cancer. N Engl J Med 2008;359:1590-601. [DOI] [PubMed] [Google Scholar]
- 2.Lucas DJ, Sabino J, Shriver CD, et al. Doing more: trends in breast cancer surgery, 2005 to 2011. Am Surg 2015;81:74-80. [PubMed] [Google Scholar]
- 3.Nava MB, Catanuto G, Pennati A, et al. Conservative mastectomies. Aesthetic Plast Surg 2009;33:681-6. [DOI] [PubMed] [Google Scholar]
- 4.Zhong NQ. Highlights of Gland Surgery 2015: breast surgery. Gland Surg 2014;3:E10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cordeiro PG, Pusic AL, Disa JJ, et al. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg 2004;113:877-81. [DOI] [PubMed] [Google Scholar]
- 6.Kim SW, Lee HK, Kang SM, et al. Short-term outcomes of immediate breast reconstruction using an implant or tissue expander after mastectomy in breast cancer patients. Breast Cancer 2014. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 7.Ascherman JA, Hanasono MM, Newman MI, et al. Implant reconstruction in breast cancer patients treated with radiation therapy. Plast Reconstr Surg 2006;117:359-65. [DOI] [PubMed] [Google Scholar]
- 8.Andree C, Munder BI, Seidenstuecker K, et al. Skin-sparing mastectomy and immediate reconstruction with DIEP flap after breast-conserving therapy. Med Sci Monit 2012;18:CR716-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lindegren A, Halle M, Docherty Skogh AC, et al. Postmastectomy breast reconstruction in the irradiated breast: a comparative study of DIEP and latissimus dorsi flap outcome. Plast Reconstr Surg 2012;130:10-8. [DOI] [PubMed] [Google Scholar]
- 10.Spear SL, Parikh PM, Reisin E, et al. Acellular dermis-assisted breast reconstruction. Aesthetic Plast Surg 2008;32:418-25. [DOI] [PubMed] [Google Scholar]
- 11.Kronowitz SJ, Robb GL. Breast reconstruction with postmastectomy radiation therapy: current issues. Plast Reconstr Surg 2004;114:950-60. [DOI] [PubMed] [Google Scholar]
- 12.Kronowitz SJ. Delayed-immediate breast reconstruction: technical and timing considerations. Plast Reconstr Surg 2010;125:463-74. [DOI] [PubMed] [Google Scholar]
- 13.Evans GR, Schusterman MA, Kroll SS, et al. Reconstruction and the radiated breast: is there a role for implants? Plast Reconstr Surg 1995;96:1111-5; discussion, 1116-8. [PubMed] [Google Scholar]
- 14.Schaverien MV, Macmillan RD, McCulley SJ. Is immediate autologous breast reconstruction with postoperative radiotherapy good practice?: a systematic review of the literature. J Plast Reconstr Aesthetic Surg 2013;66:1637-51. [DOI] [PubMed] [Google Scholar]
- 15.Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg 1989;42:645-8. [DOI] [PubMed] [Google Scholar]
- 16.Allen RJ, Treece P. Deep inferior epigastric perforator flap for breast reconstruction. Ann Plast Surg 1994;32:32-8. [DOI] [PubMed] [Google Scholar]
- 17.Massey MF, Spiegel AJ, Levine JL, et al. Perforator flaps: recent experience, current trends, and future directions based on 3974 microsurgical breast reconstructions. Plast Reconstr Surg 2009;124:737-51. [DOI] [PubMed] [Google Scholar]
- 18.Healy C, Allen RJ, Sr. The evolution of perforator flap breast reconstruction: twenty years after the first DIEP flap. J Reconstr Microsurg 2014;30:121-5. [DOI] [PubMed] [Google Scholar]
- 19.Blondeel PN, Hijjawi J, Depypere H, et al. Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Part II--Breast reconstruction after total mastectomy. Plast Reconstr Surg 2009;123:794-805. [DOI] [PubMed] [Google Scholar]
- 20.Blondeel PN. One hundred free DIEP flap breast reconstructions: a personal experience. Br J Plast Surg 1999;52:104-11. [DOI] [PubMed] [Google Scholar]
- 21.Nahabedian MY, Tsangaris T, Momen B. Breast reconstruction with the DIEP flap or the muscle-sparing (MS-2) free TRAM flap: is there a difference? Plast Reconstr Surg 2005;115:436-44; discussion 445-6. [DOI] [PubMed] [Google Scholar]
- 22.Munhoz AM, Montag E, Gemperli R. Oncoplastic breast surgery: indications, techniques and perspectives. Gland Surg 2013;2:143-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rogers NE, Allen RJ. Radiation effects on breast reconstruction with the deep inferior epigastric perforator flap. Plast Reconstr Surg 2002;109:1919-24; discussion 1925-6. [DOI] [PubMed]
- 24.Garvey PB, Clemens MW, Hoy AE, et al. Muscle-sparing TRAM flap does not protect breast reconstruction from postmastectomy radiation damage compared with the DIEP flap. Plast Reconstr Surg 2014;133:223-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Motwani SB, Strom EA, Schechter NR, et al. The impact of immediate breast reconstruction on the technical delivery of postmastectomy radiotherapy. Int J Radiat Oncol Biol Phys 2006;66:76-82. [DOI] [PubMed] [Google Scholar]
- 26.Tran NV, Chang DW, Gupta A, et al. Comparison of immediate and delayed free TRAM flap breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg 2001;108:78-82. [DOI] [PubMed] [Google Scholar]
- 27.Anton MA, Eskenazi LB, Hartrampf CR., Jr Nipple Reconstruction With Local Flaps: Star and Wrap Flaps. Seminars in Plastic Surgery 1991;5:67-78. Available online: https://www.thieme-connect.de/DOI/DOI?10.1055/s-2008-1080415 [Google Scholar]
- 28.Farhadi J, Maksvytyte GK, Schaefer DJ, et al. Reconstruction of the nipple-areola complex: an update. J Plast Reconstr Aesthet Surg 2006;59:40-53. [DOI] [PubMed] [Google Scholar]
- 29.Roughton MC, Shenaq D, Jaskowiak N, et al. Optimizing delivery of breast conservation therapy: a multidisciplinary approach to oncoplastic surgery. Ann Plast Surg 2012;69:250-5. [DOI] [PubMed] [Google Scholar]
- 30.Romics L, Stallard S, Weiler-Mithoff E. Oncologic safety of skin-sparing mastectomy followed by immediate breast reconstruction: rate and localization of recurrences, and impact of reconstruction techniques. Orv Hetil 2013;154:163-71. [DOI] [PubMed] [Google Scholar]
- 31.Lam TC, Hsieh F, Boyages J. The effects of postmastectomy adjuvant radiotherapy on immediate two-stage prosthetic breast reconstruction: a systematic review. Plast Reconstr Surg 2013;132:511-8. [DOI] [PubMed] [Google Scholar]
- 32.Rozen WM, Ashton MW. Radiotherapy and breast reconstruction: oncology, cosmesis and complications. Gland Surg 2012;1:119-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guven E, Ozden BC, Basaran K, et al. Delayed deepithelization of the chestwall skin: a cautious approach in perforator flap breast reconstruction. Microsurgery 2010;30:589-90. [DOI] [PubMed] [Google Scholar]