Abstract
Total knee arthroplasty (TKA) is the most worldwide practiced surgery for knee osteoarthritis and its efficacy is mightily described by literature. Concerns about the invasiveness of TKA let the introduction of segmental resurfacing of the joint for younger patients with localized osteoarthritis. Bone stock sparing and ligaments preservation are the essence of both unicompartmental knee arthroplasty (UKA) and bicompartmental knee arthroplasty (BKA). Advantages related to BKA are the respect of knee biomechanics, lower complications rates, shorter hospital stay, faster rehabilitation. Moreover, in case of failure of the first implant the conversion to TKA is undemanding and can be compared to a standard prosthesis. Our experience suggest that BKA is a reliable technique in selected cases and especially younger people with higher functional requests can favourably profit from it. Although those results are encouraging, we still need further prospective, randomized, long-term studies to finally assess BKA indications and outcomes.
Keywords: Bicompartmental knee arthroplasty (BKA), patello femoral arthroplasty, medial unicompartmental knee arthroplasty (UKA), lateral unicompartmental knee arthroplasty
Luigi Sabatini, MD.

Francesco Atzori, MD.
Total knee arthroplasty (TKA) is the treatment of choice in case of advanced osteoarthritis (OA) affecting the three compartments of the knee. Although the effectiveness and high reproducibility of this surgery are responsible of its worldwide success, there are some worries about certain sub-groups of patients. In particular younger people with localized arthritis can be negatively affected by both bone stock waste and ligaments demolition related to TKA procedure.
If OA involves two of the three compartments, the treatment of choice becomes more controversial.
In these cases surgical treatments proposed include high tibial osteotomy—with or without tibial tubercle transposition, UKA without patella resurfacing, TKA or bicompartmental knee arthroplasty (BKA).
Young patients with higher functional demand and higher risk of potential revision can benefit by the implant of unicompartmental knee arthroplasty (UKA), patellofemoral arthroplasty (PFA) or the combination of the two, which are considered an effective solution for localized arthritis (1-4).
BKA has become in the last years a convincing alternative treatment to TKA due to improved techniques, prosthesis design enhancement and better clinical results achievements (5,6).
The rationale of performing a segmental resurfacing of the joint originates from the observation of normal age-related cartilage wear in cadaveric and radiographic studies. Structural changes typically progress from condyles to patellofemoral compartment (7,8). The Oxford group also observed a significant incidence of patellofemoral cartilage erosion in patients undergoing UKA; an overall rate of full thickness cartilage loss was recorded in 13% of the knees, with 9% involving the medial facet and 4% the lateral facet of the patella (9-12). Ledingham et al. reported a 58% incidence of bicompartmental OA in their population of patients referred to hospital and a relatively small number of tricompartmental OA. Medial and patellofemoral compartment involvement was the dominant pattern and was observed in 50% of the knees, while lateral and patellofemoral was found in 8% of patients (13). Beside this, Heekin et al. demonstrated that a significant subset of candidates for TKA had intact cruciate ligaments. They subsequently established that a relevant group of patients (28%) could benefit from cruciate ligaments preservation and bone sparing BKA (14). The same authors found that women are more likely to be candidate for bicompartmental knee replacement if compared with men of the same age group.
The preservation of ligaments and the minimal impact on bone stock are the main advantages related to UKA or BKA and the keys to comprehend the functional advantages related to these procedures (15,16). The principal aim of bicompartmental arthroplasty is to restore a better functionality of the knee with a less invasive surgery if compared to TKA. This target is essentially achieved by preserving the ligaments and the bone stock (16-21). The deriving enhanced stability and maintenance of joint proprioception increase functional results as far as the better kinematic of the operated knee reduces shear stress at the implant-bone interface (22-24). Bone and ligaments sparing is considered a minimally invasive surgery, more than dimensions of skin incision (16-21).
Historically two types of femoral design have been used in bicompartmental arthroplasty; the older monolithic architecture with a fixed position of tibiofemoral and patellofemoral components, or the more recent modular unlinked design where the two parts are split and placed independently (16,22,25,26). The implant of monolithic femoral component forces the surgeon to compromise the final placement on the coronal plane to best resurface medial and patellofemoral compartments. Poor results were recorded with this design (27,28). The high incidence of persistent knee pain and reduced function made the rate of failure and subsequent conversion to TKA unacceptable, so that monolithic BKA is not suggested anymore. On the other hand, a modular unlinked trochlear and condylar prosthesis allows the individual compartmental resurfacing to be performed almost independently. The orientation and alignment of each component can be precisely adjusted relatively to the axial and rotational axes of the distal femur to best suit any individual morphology (29).
Best results for bicompartmental arthroplasty are achieved if accurate indication is given; inclusion criteria aside from OA grade and extension were established by Kozinn and Scott: minimum of 90° flexion arc and less than 5° of flexion contracture, angular deformity of no more than 10° of varus and 15° of valgus and intact anterior cruciate ligament (ACL) (30). No limitations of weight and age are recommended, although BKA is especially suitable for young and active patients with body mass index (BMI) <32 and high functional expectations (1,2,4,16,25).
Early results for the less invasive procedure of BKA showed excellent pain relief and knee function, lower complications rate (fat embolism, blood loss, infection and venous thromboembolism), shorter hospital stay, allows faster rehabilitation and return to daily activities, if compared to TKA (4,5,15,16,31). The possible future surgery for conversion to TKA is undemanding, although revision is uncommon due to the high survival rate of the implant (21,25,29,32-34).
The great amount of existing literature states that TKA produces predictable and durable results (32). Nevertheless TKA unavoidably alters knee biomechanics and loads distribution of the joint. The preservation of a more physiological biomechanics as it happens in BKA should theoretically protect the implant and limit the stresses acting on it. The bicompartmental prosthesis should have at least the same potential survivorship capability of its more invasive alternative, however, few long-term studies are available.
In a 17-year follow up analysis Parratte et al. found a 54% of BKA revisions, radiographic loosening or disease progression (31). Among the 27 aseptic loosening cases, 20 knees had an isolated loosening of the patellofemoral component, 7 knees had loosening of the medial component related to PE wear and failure of the tibial plateau. An interesting aspect was that 15 of the 20 patellofemoral loosenings were uncemented implant, performed before 1989; cemented components produced a significant superior long-term outcome and thus are recommended. The same authors continue to advocate for modular BKA, recognizing that cementless trochlear component fixation, crude instrumentation and techniques, and poor polyethylene quality were responsible for aseptic loosening. Other papers reported no surgical revisions after a mean follow up of approximately 12 years (35).
Revision, if required, is often carried out without difficulty and performed with the utilization of primary implant TKA. Occasionally the employment of augments and stems is required, and the use of revision TKA is generally not necessary.
Since BKA is a relatively new procedure, strong mid-term and long-term outcomes have still to be established. Further studies should determine whether long-term durability of the implant compares to that of TKA or single compartment arthroplasty for bicompartmental disease. A characterization of the un-resurfaced compartment response to BKA and its disease-free survivorship has yet to be done.
Radiological findings in follow up for BKA show generally good implant stability. Minor cases of small radiolucencies are reported but mostly stable over the years, except for the cases needing revision as mentioned before.
Although generally considered a more complicated procedure than TKA, BKA provides the same advantages as UKA over TKA. Preservation of the intercondylar eminence with both of the cruciate ligaments, restoration of normal kinematic and gait, preservation of bone stock, maintenance of the rotational axis, maintenance of normal leg morphology, normal patella level and tracking and conservation of proprioception are the fundamental characteristics supporting partial resurfacing procedures (36-41).
UKA patients showed better functional outcomes and increased likelihood of returning to normal functional activity and to low impact sports (37). Studies regarding BKA are less powerful to assess clear benefits of this surgery over the worldwide spread TKA, although bicompartmental resurfacing concept is actually much more comparable to UKA than to TKA.
The importance of ACL and posterior cruciate ligament (PCL) retaining in knee arthroplasty has both biological and biomechanical explanation. The deriving enhanced stability of the joint is given by the less altered tibiofemoral kinematics and the preservation of proprioception. As the native biomechanics are maintained the stresses acting on prosthetic components are reduced, and shear forces between implant and bone minimized. ACL action on the resurfaced knee may be different from the native knee. Some clinical findings support it, although no in vitro data are available to biomechanically evaluate the ability of the ACL to maintain knee joint kinematics after bicruciate retaining BKA (15,31,35). Some authors simulated weight bearing knee flexion to investigate the role of cruciate ligaments in BKA and TKA with posterior cruciate retaining. They tested BKA with both ligaments preserved, ACL-resected BKA and the previously mentioned TKA for translational and rotational joint kinematics. They found that the translational and rotational knee joint kinematics resemble that of the native knee in bi-cruciate retaining BKA; the PCL-retaining TKA reached similar translational characteristics but resulted in loss of rotation (22). If both ligaments are conserved femoral rollback and tibial internal rotation with flexion are maintained (19,42,43). Ultimately, though, the sparing of cruciate ligaments in BKA may be advantageous in terms of implant survivorship, stair-climb ability, joint kinematics and patient satisfaction (16,21,42-47).
The small amount of studies concerning articulation after BKA implantation generally reported a satisfactory range of motion (ROM) recovery. Most of the patients reached a complete flexion greater than 120° with no pain and complete extension (5,23).
Current studies show a trend towards common complications in line with other popular lower limb surgeries. Deep venous thromboembolism and deep infections are rare, in accordance with literature. Some cases of post-operative stiffness have been reported, however it is unclear if this is a coincidental finding or if the procedure has a tendency to provoke stiffness (48). Furthermore, there isn’t any report of knee instability with walking. Some patient suffered light anterior pain, especially standing up from seated position. An exceptional case of patellar instability has been reported, treated successfully with lateral release.
Some group experienced a higher rate of complications, but it is not clear if this can be ascribed to technique, choice of implant, or patient selection.
Both BKA and TKA effectively reduce pain and improve physical function compared to pre-operative scores. Whether other advantages can be ascribed to the less invasive BKA, is not completely clear.
Firstly BKA resulted in less intra-operative blood loss, due to the minimization of tissue damage and bone sparing (49).
Parratte et al. found that after at least 2 years, contemporary unlinked BKA was associated with greater comfort during everyday activities (forgotten knee) and better functional outcomes, compared to TKA. These short-term results require validation in randomised trials with longer follow-ups (50).
Other authors found that BKA lead to a greater knee extension in the early post-operative period. It seem, however, that these advantages over TKA do not persist past 1 year after surgery; when adjusting for age, sex, BMI and baseline status, the early advantages offered by BKA appear to vanish. The only significant difference they observed was that in the early post-operative period patients experience a more rapid and drastic reduction in stiffness in favour of BKA (28).
Engh recorded that 2 years postoperatively the BKA and TKA groups achieved equivalent results in clinical scores and functional testing (51).
Yeo et al. said that unlinked, modular BCA results in similar clinical and functional scores as TKA for medial and patellofemoral arthritis in the mid-term. Intra-operative blood loss was significantly lower in the BCA group compared to the TKA group. BCA is a viable option for a select group of young and active patients with the advantage of reduced intra-operative blood loss and equivalent functional outcomes as TKA (52).
Other groups found general clinical and functional better outcomes for BKA compared with TKA but no statistical significance was produced. In terms of KSS-function, KOOS stiffness and ADL scores, the BKA group was consistently better than TKA. The better function in the BKA group may be the result of bone and ligaments preserving nature. Postoperative knee ROM and its improvement were again greater in the bicompartmental group (53).
The knee muscles strength recovery seems to be equivalent between BKA and TKA. The less-invasive procedure however gives better results in isokinetic quadriceps strength, which is related to better performance during strenuous activities such as jogging or stair climbing (54).
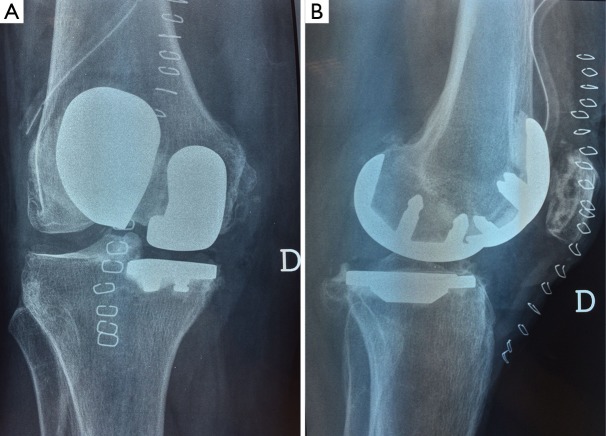
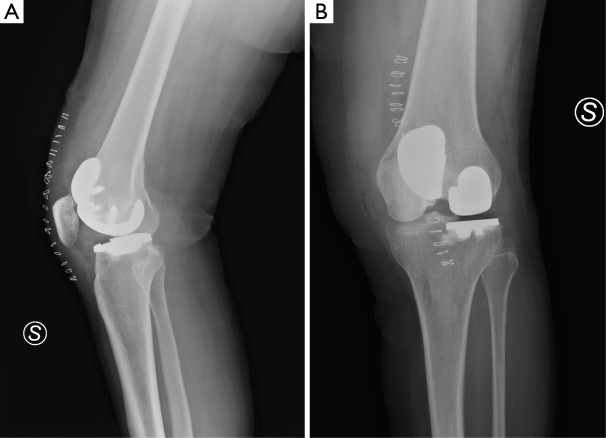
In our experience we performed BKA in selected cases with bicompartmental OA, both medial unicompartmental and patellofemoral arthroplasty (Figure 1) and lateral unicompartmental and patellofemoral replacement (Figure 2); we prefer this surgical technique in young active people and our surgical results confirm very good patients satisfaction in short and medium term follow up without complications.
Figure 1.
A case of medial unicompartmental and patellofemoral bicompartmental knee arthroplasty.
Figure 2.
A case of lateral unicompartmental and patellofemoral bicompartmental knee arthroplasty.
In conclusion, BKA shows undoubtedly important advantages such as bone-stock and ligaments sparing. Overall results of this surgery are at least comparable to that of TKA, the gold standard treatment for diffused knee OA. For its features of less-invasive surgery, BKA find its ideal indication in young patients affected by medial or lateral tibiofemoral OA, plus patellofemoral compartment involvement. Active and high-demanding patients can also benefit from BKA.
Although encouraging results are emerging from recent studies, further prospective, randomized, long-term analysis comparing BKA and TKA have to be performed before definitive treatment recommendation can be done.
Acknowledgements
None.
Biographies
Authors’ introduction: Luigi Sabatini was born in Torino (Italy) in 1978; he finished his residency in Orthopaedics and Traumatology in 2008 with honour. He is surgeon in the University Division of Orthopaedics and Traumatology of San Luigi Hospital of Orbassano (Torino). His main clinical and surgical interests are in joints reconstruction (hip and knee over all) and knee surgery (conservative and sport medicine). He has authored several articles in peer-reviewed journals and he is also reviewer in several international journals.
Francesco Atzori was born in Turin in 1968; he finished his residency in Orthopaedics and Traumatology in 1998 with honour. He is senior surgeon responsible for the knee surgery (conservative surgery, knee replacement and sport medicine) in the University Division of Orthopaedics and Traumatology of San Luigi Hospital of Orbassano (Torino). He has authored several articles in peer-reviewed journals and some book chapters.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Kamath AF, Levack A, John T, et al. Minimum two-year outcomes of modular bicompartmental knee arthroplasty. J Arthroplasty 2014;29:75-9. [DOI] [PubMed] [Google Scholar]
- 2.Thienpont E, Price A. Bicompartmental knee arthroplasty of the patellofemoral and medial compartments. Knee Surg Sports Traumatol Arthrosc 2013;21:2523-31. [DOI] [PubMed] [Google Scholar]
- 3.Lonner JH. Patellofemoral arthroplasty. J Am Acad Orthop Surg 2007;15:495-506. [DOI] [PubMed] [Google Scholar]
- 4.John T, Sheth N, Lonner JH. Modular bicompartmental arthroplasty of the knee. New Orleans, LA: Knee Society; 2010. [Google Scholar]
- 5.Argenson JN, Parratte S, Bertani A, et al. The new arthritic patient and arthroplasty treatment options. J Bone Joint Surg Am 2009;91 Suppl 5:43-8. [DOI] [PubMed] [Google Scholar]
- 6.Argenson JN, Flecher X, Parratte S, et al. Patellofemoral arthroplasty: an update. Clin Orthop Relat Res 2005;440:50-3. [DOI] [PubMed] [Google Scholar]
- 7.Miller R, Kettelkamp DB, Laubenthal KN, et al. Quantitative correlations in degenerative arthritis of the knee. J Bone Joint Surg Am 1973;55:956-62. [PubMed] [Google Scholar]
- 8.Tibesku CO, Innocenti B, Wong P, et al. Can CT-based patient-matched instrumentation achieve consistent rotational alignment in knee arthroplasty? Arch Orthop Trauma Surg 2012;132:171-7. [DOI] [PubMed] [Google Scholar]
- 9.Beard DJ, Pandit H, Ostlere S, et al. Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg Br 2007;89:1602-7. [DOI] [PubMed] [Google Scholar]
- 10.Ritter MA, Faris PM, Thong AE, et al. Intra-operative findings in varus osteoarthritis of the knee. An analysis of pre-operative alignment in potential candidates for unicompartmental arthroplasty. J Bone Joint Surg Br 2004;86:43-7. [PubMed] [Google Scholar]
- 11.McAlindon TE, Snow S, Cooper C, et al. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Ann Rheum Dis 1992;51:844-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan R, Peat G, Thomas E, et al. Incidence, progression and sequence of development of radiographic knee osteoarthritis in a symptomatic population. Ann Rheum Dis 2011;70:1944-8. [DOI] [PubMed] [Google Scholar]
- 13.Ledingham J, Regan M, Jones A, et al. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Ann Rheum Dis 1993;52:520-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heekin RD, Fokin AA. Incidence of bicompartmental osteoarthritis in patients undergoing total and unicompartmental knee arthroplasty: is the time ripe for a less radical treatment? J Knee Surg 2014;27:77-81. [DOI] [PubMed] [Google Scholar]
- 15.Rolston L, Siewert K. Assessment of knee alignment after bicompartmental knee arthroplasty. J Arthroplasty 2009;24:1111-4. [DOI] [PubMed] [Google Scholar]
- 16.Rolston L, Bresch J, Engh G, et al. Bicompartmental knee arthroplasty: a bone-sparing, ligament-sparing, and minimally invasive alternative for active patients. Orthopedics 2007;30:70-3. [PubMed] [Google Scholar]
- 17.Fuchs S, Tibesku CO, Frisse D, et al. Clinical and functional comparison of uni- and bicondylar sledge prostheses. Knee Surg Sports Traumatol Arthrosc 2005;13:197-202. [DOI] [PubMed] [Google Scholar]
- 18.Banks SA, Fregly BJ, Boniforti F, et al. Comparing in vivo kinematics of unicondylar and bi-unicondylar knee replacements. Knee Surg Sports Traumatol Arthrosc 2005;13:551-6. [DOI] [PubMed] [Google Scholar]
- 19.Fuchs S, Tibesku CO, Genkinger M, et al. Proprioception with bicondylar sledge prostheses retaining cruciate ligaments. Clin Orthop Relat Res 2003;(406):148-54. [DOI] [PubMed] [Google Scholar]
- 20.Fuchs S, Tibesku CO, Genkinger M, et al. Clinical and functional comparison of bicondylar sledge prostheses retaining all ligaments and constrained total knee replacement. Clin Biomech (Bristol, Avon) 2004;19:263-9. [DOI] [PubMed] [Google Scholar]
- 21.Confalonieri N, Manzotti A, Cerveri P, et al. Bi-unicompartmental versus total knee arthroplasty: a matched paired study with early clinical results. Arch Orthop Trauma Surg 2009;129:1157-63. [DOI] [PubMed] [Google Scholar]
- 22.Wünschel M, Lo J, Dilger T, et al. Influence of bi- and tri-compartmental knee arthroplasty on the kinematics of the knee joint. BMC Musculoskelet Disord 2011;12:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Isaac SM, Barker KL, Danial IN, et al. Does arthroplasty type influence knee joint proprioception? A longitudinal prospective study comparing total and unicompartmental arthroplasty. Knee 2007;14:212-7. [DOI] [PubMed] [Google Scholar]
- 24.Barrack RL, Skinner HB, Cook SD, et al. Effect of articular disease and total knee arthroplasty on knee joint-position sense. J Neurophysiol 1983;50:684-7. [DOI] [PubMed] [Google Scholar]
- 25.Zanasi S. Innovations in total knee replacement: new trends in operative treatment and changes in peri-operative management. Eur Orthop Traumatol 2011;2:21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am 2002;84-A:2235-9. [PubMed] [Google Scholar]
- 27.Palumbo BT, Henderson ER, Edwards PK, et al. Initial experience of the Journey-Deuce bicompartmental knee prosthesis: a review of 36 cases. J Arthroplasty 2011;26:40-5. [DOI] [PubMed] [Google Scholar]
- 28.Morrison TA, Nyce JD, Macaulay WB, et al. Early adverse results with bicompartmental knee arthroplasty: a prospective cohort comparison to total knee arthroplasty. J Arthroplasty 2011;26:35-9. [DOI] [PubMed] [Google Scholar]
- 29.Lonner JH. Modular bicompartmental knee arthroplasty with robotic arm assistance. Am J Orthop (Belle Mead NJ) 2009;38:28-31. [PubMed] [Google Scholar]
- 30.Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am 1989;71:145-50. [PubMed] [Google Scholar]
- 31.Parratte S, Pauly V, Aubaniac JM, et al. Survival of bicompartmental knee arthroplasty at 5 to 23 years. Clin Orthop Relat Res 2010;468:64-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pradhan NR, Gambhir A, Porter ML. Survivorship analysis of 3234 primary knee arthroplasties implanted over a 26-year period: a study of eight different implant designs. Knee 2006;13:7-11. [DOI] [PubMed] [Google Scholar]
- 33.Châtain F, Richard A, Deschamps G, et al. Revision total knee arthroplasty after unicompartmental femorotibial prosthesis: 54 cases. Rev Chir Orthop Reparatrice Appar Mot 2004;90:49-57. [DOI] [PubMed] [Google Scholar]
- 34.Järvenpää J, Kettunen J, Miettinen H, et al. The clinical outcome of revision knee replacement after unicompartmental knee arthroplasty versus primary total knee arthroplasty: 8-17 years follow-up study of 49 patients. Int Orthop 2010;34:649-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Heyse TJ, Khefacha A, Cartier P. UKA in combination with PFR at average 12-year follow-up. Arch Orthop Trauma Surg 2010;130:1227-30. [DOI] [PubMed] [Google Scholar]
- 36.Laurencin CT, Zelicof SB, Scott RD, et al. Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res 1991;(273):151-6. [PubMed] [Google Scholar]
- 37.Saccomanni B. Unicompartmental knee arthroplasty: a review of literature. Clin Rheumatol 2010;29:339-46. [DOI] [PubMed] [Google Scholar]
- 38.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 2008;58:26-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Riddle DL, Jiranek WA, McGlynn FJ. Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty 2008;23:408-12. [DOI] [PubMed] [Google Scholar]
- 40.Sah AP, Springer BD, Scott RD. Unicompartmental knee arthroplasty in octogenarians: survival longer than the patient. Clin Orthop Relat Res 2006;451:107-12. [DOI] [PubMed] [Google Scholar]
- 41.Tabor OB, Jr, Tabor OB, Bernard M, et al. Unicompartmental knee arthroplasty: long-term success in middle-age and obese patients. J Surg Orthop Adv 2005;14:59-63. [PubMed] [Google Scholar]
- 42.Komistek RD, Mahfouz MR, Bertin KC, et al. In vivo determination of total knee arthroplasty kinematics: a multicenter analysis of an asymmetrical posterior cruciate retaining total knee arthroplasty. J Arthroplasty 2008;23:41-50. [DOI] [PubMed] [Google Scholar]
- 43.Argenson JN, Komistek RD, Aubaniac JM, et al. In vivo determination of knee kinematics for subjects implanted with a unicompartmental arthroplasty. J Arthroplasty 2002;17:1049-54. [DOI] [PubMed] [Google Scholar]
- 44.Goodfellow JW, O'Connor J. Clinical results of the Oxford knee. Surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Relat Res 1986;(205):21-42. [PubMed] [Google Scholar]
- 45.Skowroński J, Jatskewych J, Długosz J, et al. The Oxford II medial unicompartmental knee replacement. A minimum 10-year follow-up study. Ortop Traumatol Rehabil 2005;7:620-5. [PubMed] [Google Scholar]
- 46.Berger RA, Meneghini RM, Jacobs JJ, et al. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am 2005;87:999-1006. [DOI] [PubMed] [Google Scholar]
- 47.Andriacchi TP, Galante JO, Fermier RW. The influence of total knee-replacement design on walking and stair-climbing. J Bone Joint Surg Am 1982;64:1328-35. [PubMed] [Google Scholar]
- 48.Scuderi GR. The stiff total knee arthroplasty: causality and solution. J Arthroplasty 2005;20:23-6. [DOI] [PubMed] [Google Scholar]
- 49.Tan SM, Dutton AQ, Bea KC, et al. Bicompartmental versus total knee arthroplasty for medial and patellofemoral osteoarthritis. J Orthop Surg (Hong Kong) 2013;21:281-4. [DOI] [PubMed] [Google Scholar]
- 50.Parratte S, Ollivier M, Opsomer G, et al. Is knee function better with contemporary modular bicompartmental arthroplasty compared to total knee arthroplasty? Short-term outcomes of a prospective matched study including 68 cases. Orthop Traumatol Surg Res 2015;101:547-52. [DOI] [PubMed] [Google Scholar]
- 51.Engh GA, Parks NL, Whitney CE. A prospective randomized study of bicompartmental vs. total knee arthroplasty with functional testing and short term outcome. J Arthroplasty 2014;29:1790-4. [DOI] [PubMed] [Google Scholar]
- 52.Yeo NE, Chen JY, Yew A, et al. Prospective randomised trial comparing unlinked, modular bicompartmental knee arthroplasty and total knee arthroplasty: a five years follow-up. Knee 2015;22:321-7. [DOI] [PubMed] [Google Scholar]
- 53.Shah SM, Dutton AQ, Liang S, et al. Bicompartmental versus total knee arthroplasty for medio-patellofemoral osteoarthritis: a comparison of early clinical and functional outcomes. J Knee Surg 2013;26:411-6. [DOI] [PubMed] [Google Scholar]
- 54.Chung JY, Min BH. Is bicompartmental knee arthroplasty more favourable to knee muscle strength and physical performance compared to total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 2013;21:2532-41. [DOI] [PubMed] [Google Scholar]