Abstract
AIM: To explore the difference of somatostatin receptor subtype 2 (SST2R) gene expression in pancreatic cancerous tissue and its adjacent tissue, and the relationship between the change of SST2R gene expression and pancreatic tumor angiogenesis related genes.
METHODS: The expressions of SST2R, DPC4, p53 and ras genes in cancer tissues of 40 patients with primary pancreatic cancer, and the expression of SST2R gene in its adjacent tissue were determined by immunohistochemiscal LSAB method and EnVisionTM method. Chi-square test was used to analyze the difference in expression of SST2R in pancreatic cancer tissue and its adjacent tissue, and the correlation of SST2R gene expression with the expression of p53, ras and DPC4 genes.
RESULTS: Of the tissue specimens from 40 patients with primary pancreatic cancer, 35 (87.5%) cancer tissues showed a negative expression of SST2R gene, whereas 34 (85%) a positive expression of SST2R gene in its adjacent tissues. Five (12.5%) cancer tissues and its adjacent tissues simultaneously expressed SST2R. The expression of SST2R gene was markedly higher in pancreatic tissues adjacent to cancer than in pancreatic cancer tissues (P < 0.05). The expression rates of p53, ras and DPC4 genes were 50%, 60% and 72.5%, respectively. There was a significant negative correlation of SST2R with p53 and ras genes (χ12 = 9.33, χ22 = 15.43, P < 0.01), but no significant correlation with DPC4 gene (χ2 = 2.08, P > 0.05).
CONCLUSION: There was a significant difference of SST2R gene expression in pancreatic cancer tissues and its adjacent tissues, which might be one cause for the different therapeutic effects of somatostatin and its analogs on pancreatic cancer patients. There were abnormal expressions of SST2R, DPC4, p53 and ras genes in pancreatic carcinogenesis, and moreover, the loss or decrease of SST2R gene expression was significantly negatively correlated with the overexpression of tumor angiogenesis correlated p53 and ras genes, suggesting that SST2R gene together with p53 and ras genes may participate in pancreatic cancerous angiogenesis.
INTRODUCTION
Recent studies have indicated that somatostatin and its analogs have obviously antiproliferative effects on various solid tumors, such as colon cancer, liver cancer, which are mediated through somatostatin receptors[1-7], but a large number of clinical researches indicate that the therapeutic effects of somatostatin and its analogs on pancreatic cancer are different, the reason is not known[8,9]. Moreover, studies have already reported that the change of SST2R gene expression in human pancreatic cancerous cells is related with tumor angiogenesis factors such as transforming growth factor beta (TGF-β), but the relationship between SST2R and tumor angiogenesis related genes such as DPC4, ras and p53 is still not clear[10]. Our study aimed at exploring the cause for the different therapeutic effects of somatostatin and its analogs on human pancreatic cancer, and the relationship between the changes of SST2R gene expression and pancreatic tumor angiogenesis correlated genes.
Tissue specimens
Tissue samples from 40 primary pancreatic cancer patients were obtained from the Department of Pathology in Tongji Hospital. The patients consisted of 26 males and 14 females aged from 33 to 71 years (means: 55.65 years). All lesions were diagnosed pathologically as pancreatic ductal adenocarcinoma, consisting of 23 pancreatic cancers in the head, and 17 pancreatic cancers in the body and tail of pancreas. All patients were staged according to UICC TNM classification, I-II in 14 patients, and III-IV in 26 patients. All the specimens of pancreatic cancer tissues and its adjacent tissues were fixed and dehydrated in 10% formalin, embedded in paraffin and cut into 4 μm serial sections.
Reagents
Goat SST2R and DPC4 polyclonal antibodies were from Santa Cruz (USA). p53, ras monoclonal antibody and mouse anti-human ras monoclonal antibody were from Maixin Biotech Kaifa Company (Fuzhou, China). Secondary biotinylated rabbit anti-sheep IgG (ZB-2050) was from ZYMED (USA). EnVisionTM mouse-anti reagent kit, EnVisionTM rabbit-anti reagent kit and peroxidase conjugated streptavidin were from DAKO (Denmark).
Immunohistochemical staining
Three-step methods (LSAB) were used for DPC4 and SST2R staining, and two-step methods (EnVisionTM system) were used for p53 and ras genes. Formalin-fixed, paraffin-embedded sections were dewaxed, rehydrated, and boiled in 0.01M-citrate buffer, pH 6.0 in a microwave oven for 10 minutes. Then primary antibody was added and incubated at 4 °Covernight. Biotinylated rabbit anti-sheep IgG (1:300 dilution) was added and incubated at 37 °C for 1 hour, followed by incubation with peroxidase conjugated streptavidin (1:400 dilution) at 37 °C for 30 minutes. For p53 and ras staining, peroxidase conjugated streptavidin was replaced by EnVision. DAB chromogen was applied for 10 to 20 minutes and rinsed for visualization under microscope, followed by slight counterstaining with haematoxylin, dehydration, and finally cover slips were sealed with permount. Negative control was obtained by replacing the primary antibody with PBS.
Evaluation of immunohistochemical staining
Positive staining was located in cell membrane/cytoplasm for SST2R, and the cytoplasm for DPC4 and ras, and the nucleus for p53. At least 1000 cells were counted per 40 X 10 field. The expressions were graded, as follows. Negative (-) if < 10% of the cancerous cells in a given specimen were positively stained. Weak positive (+) if 10% to 20% of the cancerous cells in a given specimen were positively stained. Positive (++) if 20% to 50% of the cancer cells in a given specimen were positively stained, and strongly positive (+++) if 75% of the cancer cells in a given specimen were positively stained.
Statistical analysis
Chi-square test was used to analyze the results. P < 0.05 was considered statistically significant.
RESULTS
Expression of SST2R gene in pancreatic cancer tissue and its adjacent tissue
The expression rate of SST2R gene was markedly higher in the adjacent non-cancerous tissue (85%) than in cancer tissue (12.5%) (P < 0.05). Twenty-nine patients (72.5%) expressed SST2R gene only in the adjacent non-cancerous tissue. For SST2R gene expression in pancreatic cancer tissue, strong positive was only 10%, weak positive 2.5%, and negative 87.5%, 12.5% pancreatic cancer tissue and its adjacent non-cancerous tissue expressed SST2R simultaneously (Table 1 and Figures 1, Figures 2).
Table 1.
Expressions of SST2R and ras, DPC4 and p53 genes in 40 primary pancreatic cancerous tissues
| Strong positive (++-+++) n (%) | Weak positive (+) n (%) | Negative (-) n (%) | |
| SST2R | 4.0(10) | 1.0(2.5) | 35.0(87.5) |
| ras | 14.0(35) | 10.0(25) | 16.0(4) |
| DPC4 | 7.0(17.5) | 4.0(10) | 19.0(47.5) |
| P53 | 19.0(47.5) | 1.0(2.5) | 20.0(50) |
| Cancer | 34.0(85) | 0.0 | 6.0(15) |
| adjacent SST2R |
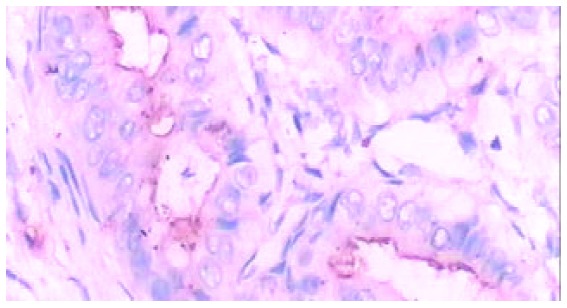
Figure 1.
Ductal adenocarcinoma in pancreatic head (Immunohisto-chemistry LSAB method, × 400). Brown yellow staining of SST2R gene expression in cell membrane/cytoplasm.
Figure 2.
Pancreatic ductal adenocarcinoma in pancreatic body and tail (Immunohistochemistry LSAB method, × 400). Brown yellow staining of SST2R gene expression in cell membrane/ cytoplasm.
Expression of p53 gene in pancreatic cancer tissue
For p53 gene in pancreatic cancerous tissue, 19 patients (47.5%) had strong positive expression, 20 patients (50%) negative expression, and 1 patient (2.5%) weak positive expression. The SST2R gene expression in 17 patients with strong positive expression of p53 was negative. Three patients with strong positive expression of SST2R were negative for p53 gene expression. The SST2R and p53 gene expressions in 1 patient were strong positive. One patient with weak positive expression of p53 gene was negative for SST2R gene expression. The SST2R gene expression of 1 patient with strong positive expression of p53 gene was weak positive (Table 1 and Figure 3).
Figure 3.
Ductal adenocarcinoma in pancreatic head (EnVisionTM method, × 400). Brown yellow staining of p53 gene expression in cell nucleus.
Expression of ras gene in pancreatic cancer tissue
For expression of ras gene, 14 patients (35%) were strong positive, 10 patients (25%) weak positive, and 16 patients (40%) negative. Eleven patients with strong positive expression of ras gene showed negative expression of SST2R gene, 1 patient with negative expression of ras gene showed strong positive expression of SST2R gene. The SST2R and ras genes in 4 patients showed positive expression of different grades correspondingly. The SST2R and ras gene expressions in 15 patients were negative. Nine patients with weak positive expression of ras gene were negative for SST2R gene expression (Table 1 and Figure 4).
Figure 4.
Ductal adenocarcinoma in pancreatic body and tail (EnVisionTM method, × 400). Brown yellow staining of ras gene expression located in cytoplasm.
Expression of DPC4 gene in pancreatic cancer tissue
Seven patients (17.5%) were positive, 4 patients (10%) weak positive, and 29 patients (72.5%) negative for DPC4 gene expression. Twenty-six patients (65%) had negative expression of both DPC4 and SST2R gene. Of the 9 patients with negative expression of SST2R gene, 5 patients were strong positive, and 4 patients weak positive for DPC4 gene expression. Both SST2R and DPC4 genes expression of 2 patients were strong positive. One patient with negative expression of DPC4 gene was weak positive for SST2R gene expression (Table 1 and Figure 5).
Figure 5.
Ductal adenocarcinoma in pancreatic body and tail (EnVisionTM method, × 400). Brown yellow staining of DPC4 gene expression located in cytoplasm.
Statistical analysis indicated that SST2R was significantly negatively correlated with the expression of p53 or ras genes (P < 0.01), whereas not distinctly correlated with DPC4 gene (P > 0.05).
DISCUSSION
Somatostatin and its analogs can inhibit the growth of benign and malignant tumors, and it has been found that the inhibitory effects are directly correlated with the expression of SST2R on tumor tissues[11-15]. The mechanisms of the inhibition are the combined interaction of somatostatin and its analogs with SST2R in tumor tissues, either directly inhibiting division and proliferation of tumor cells or inhibiting the activities of growth factors such as vascular endothelial growth factor (VEGF), insulin-like growth factor (IGF)[16-21], and moreover, counteracting tumorigenesis and tissue proliferation[22,23]. In addition, somatostatin and its analogs could arrest pancreatic cancer cell cycle at G0-S1 phase by up-regulating p27, and thus induced apoptosis[24,25].
The expression of SST2R was decreased or lost in primary pancreatic cancerous tissue[26-29], but there is no report on the expression of SST2R in pancreatic cancerous adjacent tissue. Our study showed that 5 of 40 primary pancreatic cancer tissues showed positive expression of SST2R gene, suggesting that most of pancreatic cancerous tissues lack the expression of SST2R, which may be the major reason why somatostatin and its analogs had no marked therapeutic effects on pancreatic cancer. Interestingly, expression of SST2R was higher in most of the pancreatic cancerous adjacent tissues, which may be beneficial for somatostatin and its analogs to inhibit fast outward infiltration and growth of tumor cells. Our study indicated that if SST2R decreased in pancreatic cancerous tissue and its adjacent tissue, somatostatin and its analogs might not have therapeutic effect on pancreatic cancer. But when pancreatic cancerous tissue and its adjacent tissue obviously expressed SST2R, they had a definite therapeutic effect on patients with pancreatic cancer. Hence the differences in the expression of SST2R in pancreatic cancerous tissue and its adjacent tissue would certainly lead to different therapeutic effects. At present, this is the main possible cause for the different therapeutic effects of somatostatin and its analogs on pancreatic cancer. We consider that it is important to define the expression of SST2R in pancreatic cancerous tissue and its adjacent tissue before using somatostatin and its analogs. This will be beneficial to the ultimate definition of the exact therapeutic effects of somatostatin and its analogs on pancreatic cancer.
Mutations of DPC4, ras and p53 genes have been found to play crucial roles in tumor angiogenesis[30-32]. The mutation rates of these genes are higher in pancreatic cancerous tissue, indicating that the similar mechanism of pancreatic tumorigenesis with other tumorigenesis involving mutation and abnormal expression of multiple genes. Our study indicated that the expression of SST2R gene was significantly negatively correlated with p53 and ras genes, suggesting that the decrease or loss of SST2R gene expression in pancreatic cancerous tissue participates in tumor angiogenesis through certain pathway, further investigation is required to probe into its the mechanism.
Footnotes
Supported by National Natural Science Foundation of China, No. 30271473
Edited by Ren SY and Wang XL
References
- 1.O'Byrne KJ, Schally AV, Thomas A, Carney DN, Steward WP. Somatostatin, its receptors and analogs, in lung cancer. Chemotherapy. 2001;47 Suppl 2:78–108. doi: 10.1159/000049163. [DOI] [PubMed] [Google Scholar]
- 2.Kouroumalis E, Skordilis P, Thermos K, Vasilaki A, Moschandrea J, Manousos ON. Treatment of hepatocellular carcinoma with octreotide: a randomised controlled study. Gut. 1998;42:442–447. doi: 10.1136/gut.42.3.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolff RA. Chemoprevention for pancreatic cancer. Int J Gastrointest Cancer. 2003;33:27–41. doi: 10.1385/IJGC:33:1:27. [DOI] [PubMed] [Google Scholar]
- 4.Samonakis DN, Moschandreas J, Arnaoutis T, Skordilis P, Leontidis C, Vafiades I, Kouroumalis E. Treatment of hepatocellular carcinoma with long acting somatostatin analogues. Oncol Rep. 2002;9:903–907. [PubMed] [Google Scholar]
- 5.Hejna M, Schmidinger M, Raderer M. The clinical role of soma-tostatin analogues as antineoplastic agents: much ado about nothing. Ann Oncol. 2002;13:653–668. doi: 10.1093/annonc/mdf142. [DOI] [PubMed] [Google Scholar]
- 6.Hofsli E. [The somatostatin receptor family--a window against new diagnosis and therapy of cancer] Tidsskr Nor Laegeforen. 2002;122:487–491. [PubMed] [Google Scholar]
- 7.Vainas IG. Octreotide in the management of hormone-refractory prostate cancer. Chemotherapy. 2001;47 Suppl 2:109–126. doi: 10.1159/000049164. [DOI] [PubMed] [Google Scholar]
- 8.Raderer M, Kurtaran A, Scheithauer W, Fiebiger W, Weinlaender G, Oberhuber G. Different response to the long-acting somatostatin analogues lanreotide and octreotide in a patient with a malignant carcinoid. Oncology. 2001;60:141–145. doi: 10.1159/000055311. [DOI] [PubMed] [Google Scholar]
- 9.Raderer M, Hamilton G, Kurtaran A, Valencak J, Haberl I, Hoffmann O, Kornek GV, Vorbeck F, Hejna MH, Virgolini I, et al. Treatment of advanced pancreatic cancer with the long-acting somatostatin analogue lanreotide: in vitro and in vivo results. Br J Cancer. 1999;79:535–537. doi: 10.1038/sj.bjc.6690084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta MK, Qin RY. Mechanism and its regulation of tumor-induced angiogenesis. World J Gastroenterol. 2003;9:1144–1155. doi: 10.3748/wjg.v9.i6.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rochaix P, Delesque N, Estève JP, Saint-Laurent N, Voight JJ, Vaysse N, Susini C, Buscail L. Gene therapy for pancreatic carcinoma: local and distant antitumor effects after somatostatin receptor sst2 gene transfer. Hum Gene Ther. 1999;10:995–1008. doi: 10.1089/10430349950018391. [DOI] [PubMed] [Google Scholar]
- 12.Buscail L, Saint-Laurent N, Chastre E, Vaillant JC, Gespach C, Capella G, Kalthoff H, Lluis F, Vaysse N, Susini C. Loss of sst2 somatostatin receptor gene expression in human pancreatic and colorectal cancer. Cancer Res. 1996;56:1823–1827. [PubMed] [Google Scholar]
- 13.Guillermet J, Saint-Laurent N, Rochaix P, Cuvillier O, Levade T, Schally AV, Pradayrol L, Buscail L, Susini C, Bousquet C. Somatostatin receptor subtype 2 sensitizes human pancreatic cancer cells to death ligand-induced apoptosis. Proc Natl Acad Sci USA. 2003;100:155–160. doi: 10.1073/pnas.0136771100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vernejoul F, Faure P, Benali N, Calise D, Tiraby G, Pradayrol L, Susini C, Buscail L. Antitumor effect of in vivo somatostatin receptor subtype 2 gene transfer in primary and metastatic pancreatic cancer models. Cancer Res. 2002;62:6124–6131. [PubMed] [Google Scholar]
- 15.Faiss S, Pape UF, Böhmig M, Dörffel Y, Mansmann U, Golder W, Riecken EO, Wiedenmann B. Prospective, randomized, multicenter trial on the antiproliferative effect of lanreotide, interferon alfa, and their combination for therapy of metastatic neuroendocrine gastroenteropancreatic tumors--the International Lanreotide and Interferon Alfa Study Group. J Clin Oncol. 2003;21:2689–2696. doi: 10.1200/JCO.2003.12.142. [DOI] [PubMed] [Google Scholar]
- 16.Hortala M, Ferjoux G, Estival A, Bertrand C, Schulz S, Pradayrol L, Susini C, Clemente F. Inhibitory role of the somatostatin receptor SST2 on the intracrine-regulated cell proliferation induced by the 210-amino acid fibroblast growth factor-2 isoform: implication of JAK2. J Biol Chem. 2003;278:20574–20581. doi: 10.1074/jbc.M210767200. [DOI] [PubMed] [Google Scholar]
- 17.Pollak MN, Schally AV. Mechanisms of antineoplastic action of somatostatin analogs. Proc Soc Exp Biol Med. 1998;217:143–152. doi: 10.3181/00379727-217-44216. [DOI] [PubMed] [Google Scholar]
- 18.Buscail L, Vernejoul F, Faure P, Torrisani J, Susini C. Regulation of cell proliferation by somatostatin. Ann Endocrinol. 2002;63(2 Pt 3):2S13–2S18. [PubMed] [Google Scholar]
- 19.Puente E, Saint-Laurent N, Torrisani J, Furet C, Schally AV, Vaysse N, Buscail L, Susini C. Transcriptional activation of mouse sst2 somatostatin receptor promoter by transforming growth factor-beta. Involvement of Smad4. J Biol Chem. 2001;276:13461–13468. doi: 10.1074/jbc.M010981200. [DOI] [PubMed] [Google Scholar]
- 20.Pagès P, Benali N, Saint-Laurent N, Estève JP, Schally AV, Tkaczuk J, Vaysse N, Susini C, Buscail L. sst2 somatostatin receptor mediates cell cycle arrest and induction of p27(Kip1). Evidence for the role of SHP-1. J Biol Chem. 1999;274:15186–15193. doi: 10.1074/jbc.274.21.15186. [DOI] [PubMed] [Google Scholar]
- 21.Kikutsuji T, Harada M, Tashiro S, Ii S, Moritani M, Yamaoka T, Itakura M. Expression of somatostatin receptor subtypes and growth inhibition in human exocrine pancreatic cancers. J Hepatobiliary Pancreat Surg. 2000;7:496–503. doi: 10.1007/s005340070021. [DOI] [PubMed] [Google Scholar]
- 22.Bousquet C, Puente E, Buscail L, Vaysse N, Susini C. Antiproliferative effect of somatostatin and analogs. Chemotherapy. 2001;47 Suppl 2:30–39. doi: 10.1159/000049159. [DOI] [PubMed] [Google Scholar]
- 23.Ferjoux G, Bousquet C, Cordelier P, Benali N, Lopez F, Rochaix P, Buscail L, Susini C. Signal transduction of somatostatin receptors negatively controlling cell proliferation. J Physiol Paris. 2000;94:205–210. doi: 10.1016/s0928-4257(00)00206-0. [DOI] [PubMed] [Google Scholar]
- 24.Benali N, Cordelier P, Calise D, Pages P, Rochaix P, Nagy A, Esteve JP, Pour PM, Schally AV, Vaysse N, et al. Inhibition of growth and metastatic progression of pancreatic carcinoma in hamster after somatostatin receptor subtype 2 (sst2) gene expression and administration of cytotoxic somatostatin analog AN-238. Proc Natl Acad Sci USA. 2000;97:9180–9185. doi: 10.1073/pnas.130196697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fisher WE, Wu Y, Amaya F, Berger DH. Somatostatin receptor subtype 2 gene therapy inhibits pancreatic cancer in vitro. J Surg Res. 2002;105:58–64. doi: 10.1006/jsre.2002.6450. [DOI] [PubMed] [Google Scholar]
- 26.Buscail L, Saint-Laurent N, Chastre E, Vaillant JC, Gespach C, Capella G, Kalthoff H, Lluis F, Vaysse N, Susini C. Loss of sst2 somatostatin receptor gene expression in human pancreatic and colorectal cancer. Cancer Res. 1996;56:1823–1827. [PubMed] [Google Scholar]
- 27.Benali N, Ferjoux G, Puente E, Buscail L, Susini C. Somatostatin receptors. Digestion. 2000;62 Suppl 1:27–32. doi: 10.1159/000051852. [DOI] [PubMed] [Google Scholar]
- 28.Fueger BJ, Hamilton G, Raderer M, Pangerl T, Traub T, Angelberger P, Baumgartner G, Dudczak R, Virgolini I. Effects of chemotherapeutic agents on expression of somatostatin receptors in pancreatic tumor cells. J Nucl Med. 2001;42:1856–1862. [PubMed] [Google Scholar]
- 29.Qin RY, Qiu FZ. SST2R and SST2R mRNA expression in rats with pancreatic cancer and the effect of octreotide. Yixian Bingxue. 2002;2:41–44. [Google Scholar]
- 30.Schwarte-Waldhoff I, Volpert OV, Bouck NP, Sipos B, Hahn SA, Klein-Scory S, Lüttges J, Klöppel G, Graeven U, Eilert-Micus C, et al. Smad4/DPC4-mediated tumor suppression through suppression of angiogenesis. Proc Natl Acad Sci USA. 2000;97:9624–9629. doi: 10.1073/pnas.97.17.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shu X, Wu W, Mosteller RD, Broek D. Sphingosine kinase mediates vascular endothelial growth factor-induced activation of ras and mitogen-activated protein kinases. Mol Cell Biol. 2002;22:7758–7768. doi: 10.1128/MCB.22.22.7758-7768.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bacher M, Schrader J, Thompson N, Kuschela K, Gemsa D, Waeber G, Schlegel J. Up-regulation of macrophage migration inhibitory factor gene and protein expression in glial tumor cells during hypoxic and hypoglycemic stress indicates a critical role for angiogenesis in glioblastoma multiforme. Am J Pathol. 2003;162:11–17 doi: 10.1016/S0002-9440(10)63793-5. doi: 10.1016/S0002-9440(10)63793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


