Abstract
Objective
To undertake a systematic review and meta-analysis to establish the effectiveness of handwashing in reducing absence and/or the spread of respiratory tract (RT) and/or gastrointestinal (GI) infection among school-aged children and/or staff in educational settings.
Design
Randomised-controlled trials (RCTs).
Setting
Schools and other settings with a formal educational component in any country.
Patients
Children aged 3–11 years, and/or staff working with them.
Intervention
Interventions with a hand hygiene component.
Main outcome measures
Incidence of RT or GI infections or symptoms related to such infections; absenteeism; laboratory results of RT and/or GI infections.
Results
Eighteen cluster RCTs were identified; 13 school-based, 5 in child day care facilities or preschools. Studies were heterogeneous and had significant quality issues including small numbers of clusters and participants and inadequate randomisation. Individual study results suggest interventions may reduce children's absence, RT infection incidence and symptoms, and laboratory confirmed influenza-like illness. Evidence of impact on GI infection or symptoms was equivocal.
Conclusions
Studies are generally not well executed or reported. Despite updating existing systematic reviews and identifying new studies, evidence of the effect of hand hygiene interventions on infection incidence in educational settings is mostly equivocal but they may decrease RT infection among children. These results update and add to knowledge about this crucial public health issue in key settings with a vulnerable population. More robust, well reported cluster RCTs which learn from existing studies, are required.
Keywords: Infectious Diseases, School Health, Respiratory
What is already known on this topic.
As semiclosed settings where large numbers of children with immature immunity regularly congregate, educational establishments are potentially effective places to prevent spread of infection.
Evidence is equivocal but potentially promising for the effectiveness of hand hygiene interventions in preventing the spread of respiratory tract and gastrointestinal infection.
Three systematic reviews of studies of hand hygiene interventions to prevent respiratory and/or gastrointestinal infections focus on educational settings; each has significant limitations.
What this study adds.
Eighteen cluster randomised controlled trials of the effectiveness of hand hygiene interventions in educational settings were identified; more than in previous dated reviews.
Study design and reporting standards are generally low quality, impeding meta-analyses, but recently published studies show signs of improvements.
Evidence of the impact of hand hygiene interventions among this population remains equivocal: this review makes recommendations for improving future trials to evaluate interventions.
Introduction
Young children are particularly susceptible to respiratory tract (RT) and gastrointestinal (GI) infections. While usually self-limiting, these highly infectious illnesses spread quickly in semiclosed settings such as schools. Infections affect child health, causing missed educational opportunities which may have a detrimental effect on educational outcomes,1 2 lost productivity and days off work for school staff.3 Educational settings where large numbers of children with immature immunity congregate are promising sites for preventing infection, particularly as outbreaks can affect whole schools and spread to vulnerable populations (eg, younger siblings) in the community.4 5
Several systematic reviews (SRs) have evaluated evidence of interventions to prevent RT and GI infections;6–16 current evidence is equivocal but promising for the effectiveness of hand hygiene interventions in preventing RT and GI infection. Four SRs have included studies evaluating interventions in educational settings alongside other settings;8 9 11 14 two focus on RT infection,11 14 two focus on diarrhoea prevention.8 9 Two of these are Cochrane reviews;8 11 one recommended that: “effort should be concentrated on reducing transmission from young children through regular education at school on hygiene” (ref.11, p.9).
Three SRs12 13 16 focus exclusively on studies among children in educational settings. However, one only included hand sanitiser interventions;13 another included children 2–11 years old and is over a decade old.16 The most recent SR focused on the effects of multicomponent interventions (access to safe water, handwashing facilities, hygiene education) but did not assess study quality, included numerous study designs and had limited search parameters (eg, only searched in two databases).12 None of these SRs included meta-analyses (MAs). This review aimed to update these reviews using thorough methods (eg, searching a range of databases) to identify all relevant studies which apply the most robust study design (randomised controlled trial, RCT) for evaluating interventions.
The objective of this SR was to summarise evidence of the effectiveness of hand hygiene interventions in reducing infectious illness and/or absence in educational settings for children aged 3–11 years and/or staff working with them, and to obtain a quantified estimate of the effect using MAs if possible.
Methods
This SR is reported in line with current guidance.17 Review coauthors agreed the review protocol.18
Eligibility criteria
This SR included RCTs of interventions with a hand hygiene component (any comparator) in educational settings for children aged 3–11 years in any country. No length of follow-up was defined.
Educational settings were defined as institutions incorporating formal educational activities including day care facilities and nurseries. Other community settings (eg, playschools) and domestic child care settings were excluded. Study populations could include staff and/or children in these settings. The review age range aimed to ensure the inclusion of all studies in formal educational settings for younger (primary or elementary school-aged) children—hereafter referred to as primary school-aged children—where children can be expected to understand hand hygiene, toilet themselves and clean their own hands. Study populations could include children whose age overlapped with the review age range (eg, 2–6-year-old, 5–12 year-old) because school policy and practice varies between countries: children start formal education at different ages; children may repeat a year so may be older than 11 years in primary school; structured nursery facilities for younger children may be integrated in schools.
Hand hygiene interventions were defined as any initiative for children and/or staff working with them undertaken to prevent the spread of infectious illness. Comparators could include placebos or active comparators such as handwashing with soap compared with hand sanitiser use.
Inclusion criteria were piloted on reports known to authors.
Primary review outcomes were: incidence of RT or GI infections or symptoms related to such infections; absenteeism rate; or laboratory results of RT and/or GI infections. Secondary outcomes were: hospital admissions due to such infections; changes in knowledge, attitudes, beliefs or behaviours about hand hygiene among children and/or staff working with them. We intended that outcomes related to children and staff be considered separately: we did not anticipate many studies would report staff outcomes. Studies which presented outcome data for staff and children together would be considered separately from studies which presented data for staff and students.
Information sources and search strategy
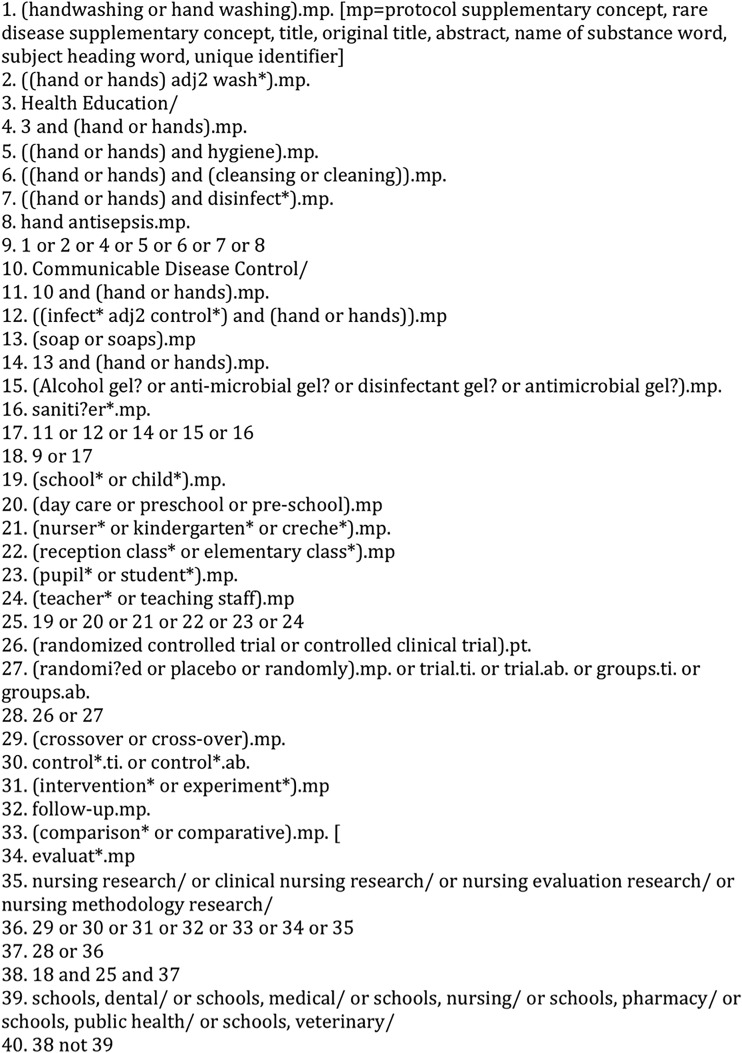
The search strategy had three components: handwashing, population and setting and study type. Handwashing, population and setting terms were extensive; handwashing terms used free-text terms as well as available controlled vocabulary terms. Population and setting terms were not used in education databases (Education Resource Information Center, Australian Education Index, British Education Index). The search focused on sources reporting RCTs and excluded unpublished literature as the coauthors agreed this was unlikely to report RCTs. A broad study type filter was used in databases where RCTs were less well indexed (see figure 1 for MEDLINE search strategy). No date or language restrictions were applied.
Figure 1.
Search strategy used for Medline.
Eight electronic databases were initially searched from inception to April 2011: MEDLINE (1950 to date), EMBASE (1980–2011, week 15), Social Science & Science Citation Indexes (ISI Web of Knowledge), CINAHL, Cochrane Library, Education Resource Information Center (1966 to date), Australian Education Index (1979 to date) and British Education Index (1975 to date). The search was updated twice using the same strategy, first to cover up to 26 September 2012, then up to 5 September 2014; dates overlapped with previous searches to ensure items were not missed. Results of each search were uploaded to an EndNote database, combined and deduplicated.
Study selection and data collection process
All titles were screened for eligibility by one reviewer; 10% were independently screened by a second reviewer (Cohen's κ statistic=≥0.75). Abstracts were independently screened by two reviewers. Where reviewers did not agree, abstracts were included in full paper screening. Full papers were dual reviewed and reasons for exclusion recorded: coauthors moderated where there was disagreement. Additional studies were identified through references in full papers and citation search facilities in ISI Web of Science, journal websites and Google Scholar.
Two potentially eligible abstracts not in English were reviewed by native speakers. A full translation was obtained for the one study that met review criteria.19 Protocols for included studies were obtained from trial registers where available.
Data collection and data items
Two reviewers independently extracted study data using a form developed from a template from another SR16 and piloted on a sample of included studies. Data included were: study details; intervention description; study recruitment; random allocation; study baseline data; follow-up; process evaluation; outcomes and analysis. Reviewers discussed differences and recorded moderated results.
Risk of bias assessment
Study quality was assessed independently by two reviewers using the Cochrane Risk of Bias tool (V.5.1), compliance with reporting guidance20 21 and good research practice (research governance, process evaluation, outcome measurement methods) pertinent to interventions with this population in these settings.
Summary measures
All effect measures pertaining to review outcomes are reported. Where studies included children under 3 years old and stratified the results they presented by age, we only report results for children over 3 years old. Where possible we present unadjusted results, where adjusted results are stated the variables used for adjustment are described. As a large number of studies reported absence by reason, three additional sets of outcome data are presented; absence due to any illness, absence due to RT infection, absence due to GI infection.
Synthesis of results
We aimed to conduct MAs if studies were sufficiently homogenous and data were adequate. Missing and unclear data were identified in the data extraction form. Studies where additional data could not be accessed were excluded from MA and reasons recorded. Authors were only contacted in exceptional circumstances due to the length of time since completion for many studies. No authors provided additional data. This led to the exclusion of several studies. Six studies were excluded due to design flaws (risk of contamination between study arms); cross-over design,22 23 clusters at class level,24–26 and clusters at class and school levels.27 28 Therefore, MAs were not conducted.
Additional analyses
Prespecified subgroup analyses (age, gender, location, setting, intervention and duration) and sensitivity analyses were not possible due to poor reporting and data quality.
Results
Study selection
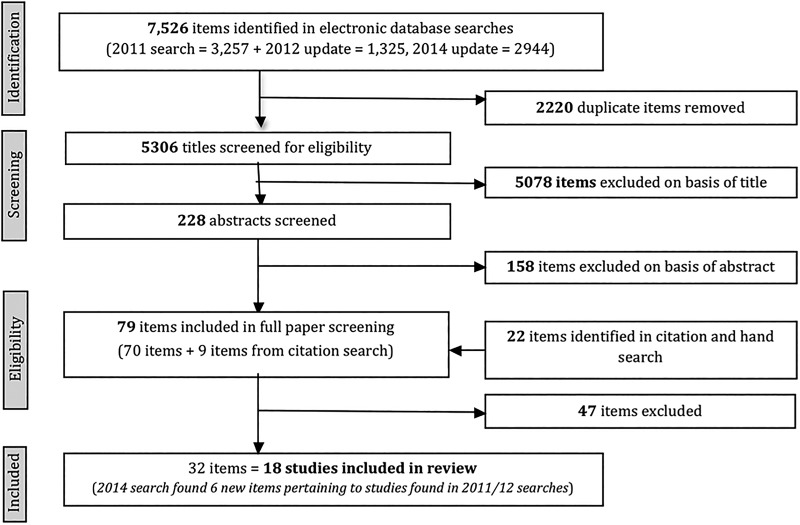
Of the 5306 titles assessed for eligibility, 18 studies fitted review criteria (figure 2). Protocols for four RCTs with as yet unpublished results were identified.29–32
Figure 2.
Flow of papers through the review.
Study characteristics
All included studies were cluster RCTs, including two with a cross-over design22 23 (table 1).
Table 1.
Characteristics of included studies
| Study author (study name) | Year of study | Population | Intervention (product details provided where reported) | Control (not all authors defined standard practice) | Study design (cluster RCTs) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Participants | Age in years (school grade) | Setting | Location | Cluster | Number of clusters | ||||
| School-based studies | |||||||||
| Azor Martínez et al27 28 | 2009–2010 | School children (n=1640) | 4–12 years | Primary school (n=5) | Spain (Almeria) | Handwashing with soap followed by hand sanitiser (ALCO ALOE GEL) | Standard practice | School and classroom | 4 schools, 29 classes from another school |
| Bowen et al33 (Safeguard Promotion Program) | 2003–2004 | School children (n=3962) | Median 7.53 years (1st grade) |
Primary school (n=90) | China (3 counties in Fujian Province) | (1) Standard programme (teacher training to encourage handwashing with soap, student take home pack) (2) Enhanced programme (standard programme plus supply of safeguard soap, student peer mentors) | Standard practice (Annual statement about Handwashing before eating and after toilet) | School | 90 30 intervention (1), 30 intervention (2), 30 controls |
| Freeman et al (WASH programme)34 35 | 2007 | School children (n=5989 supplied absence data) | 6–16 years; median 13 years (4th–8th grade) | Public primary school (n=135) | Kenya (4 districts in Nyanza Province) | (1) Hygiene promotion (HP) and water treatment (WT) (3 days teacher training, follow-up sessions) (2) HP and WT plus up to 7 new latrines per school | Standard practice | School | 135 45 intervention (1) 45 intervention (2) 45 controls |
| Graves et al36 (substudy of NICHE: Nyando Integrated Child Health and Education) | 2008–2009 | School children (precise number not reported) | Age not reported (Students in NICHE study were in 4th–8th grade) | Primary school (n=21) | Kenya (rural western area) | NICHE intervention (multiple components including health promotion by teachers, installation of drinking water, handwashing stations) plus a visual aid poster designed by students in intervention schools | NICHE intervention only | School | 21 schools 10 intervention 11 control (14 included in analysis) |
| Morton and Schultz (Healthy hands)22 | 2000–2001 | School children (n=253) | Age not reported (Kindergarten–3rd grade) | Elementary school (n=1) | USA (New England) | Handwashing with soap and AlcoSCRUB alcohol gel use (45 min session for students) | Standard practice (handwashing with soap) | Classroom | 17 (cross-over design) |
| Pandejpong et al24 | 2009–2010 | School children (n=1437) | 2–3, 3–4, 4–5, 5–6 years | Private school (n=1) | Thailand (suburban Bangkok) | Application of alcohol hand gel: Two intervention groups (1) every 60 min; (2) every 120 min | Standard practice (alcohol gel application once, before lunch) | Classroom | 68 (not clear how many classes in each arm) |
| Pickering et al37 | Unclear | School children (n=1364) | 5–10 years (preunit to P5). 1 included a nursery (2–4 years), 4 included 10–13-year-olds (P6-8 grades) | Primary school (n=6) | Kenya (Kibera urban community in Nairobi) | (1) Handwashing with soap. Two soap dispensers installed by toilets, eating area (plus water tank with a spigot). (2) Alcohol-based hand sanitiser use (Purell). Two dispensers installed by toilets, eating area | No intervention (standard practice) | School | 6 2 intervention (1) 2 intervention (2) 2 controls |
| Priest et al38–40 | 2009 | School children (n=16 245) | 5–11 years (school years 1–6) | Primary school (n=68) | New Zealand (Dunedin, Christchurch, Invercargill) | 30 min inclass hand hygiene education session, instruction on hand sanitiser use, ‘no touch’ dispensers installed in classrooms | 30 min inclass hand hygiene education session only (no instruction on hand sanitiser use) | School | 68 schools 34 intervention 34 controls |
| Sandora et al25 | 2006 | School children (n=285) | Age not reported (3rd–5th grade) | Elementary school (n=1) | USA (Avon, Ohio) | Handwashing with soap, Aerofirst hand sanitiser use, plus Clorox disinfectant wipes (Student instruction, teachers wiped students’ desks once a day, after lunch) | Standard practice (handwashing with soap) | Team | 6 teams in 15 classrooms |
| Stebbins et al (Pittsburgh Influenza Prevention Project)41–44 | 2007–2008 | School children (n=3360) | Age not reported (Kindergarten—5th grade) | Elementary school (n=10) | USA (Pittsburgh, Pennsylvania) | Handwashing and Purell hand sanitiser use (45 min presentation for students, educational materials for parents) | Standard practice | School | 10 5 intervention 5 controls |
| Talaat et al45 | 2008 | School children (n=44 451) | Median 8 years (1st–3rd grade) | Elementary school (n=60) | Egypt (Cairo) | Handwashing with soap (school-specific activities, coordinated by teachers, school nurse; pupils provided soap, drying materials) | Standard practice | School | 60 30 intervention 30 controls |
| Vessey et al23 | Not known | School children (n=383) | Age not reported (2nd and 3rd grades) | Elementary school (n=4) | USA (Butte, Montana) | Hand sanitiser use (one educational session for students) | Handwashing with soap | Classroom | 18 (cross-over design) |
| White et al26 | 1999 | School children (n=769) | 5–12 years (Kindergarten—6th grade) | Elementary school (n=3) | USA (California) | Handwashing and alcohol-free hand sanitiser use (all students attended 22-min assembly) | Handwashing and placebo sanitiser use (all students had 22-min assembly) | Classroom | 72 32 retained for analysis: 16 intervention, 16 controls |
| Non-school based studies | |||||||||
| Correa et al46 | 2008 | Children (n=1727) | 1–5-years | Child care centre (n=42) | Colombia (6 urban settings) | Purell alcohol-based hand sanitiser use (training workshop for staff and children, monthly refresher workshops) | Standard practice (handwashing with soap) | Child care centre | 42 (32 community, 10 preschool) |
| Ladegaard and Stage19 | Not known | Children (n=399 aged 3–6 years) | 0–2 years and 3–6 years | Nursery (n=8) | Denmark (Borough of Odense) | Handwashing with soap (staff training, take home book, 1 h education session for children) | Standard practice | Nursery | 8 4 intervention, 4 controls |
| Lennell et al47 | 2004–2005 | Children (n=1477) | 0–5 years. Mean: 3.2 years (intervention), 3.1 years (control). Circa 30% <3 years | Day care centre (n=60) | Sweden (10 counties, south and mid-Sweden) | Handwashing with soap and alcohol-based oily disinfectant gel use (instruction, demonstration to staff and children) | Standard practice (handwashing with soap) | Day care centre | 60 30 intervention, 30 controls (matched pairs) |
| Rosen et al (Jerusalem handwashing study)48–52 | 2001 | Children (n=1029) | 3 years and 4 years | Preschool (n=40) | Israel (Jerusalem) | Handwashing with soap (2 3-h staff training sessions, child education programme, take home pack) | Standard practice and alternative take-home pack (about oral hygiene) | Preschool | 40 20 intervention 20 controls |
| Uhari and Möttönen53 | 1991–1992 | Children (n=1522) | 861 >3 years 661 <3 years Mean: 3.6 years (intervention), 3.5 years (control) |
Child day care centre (n=20) | Finland (Oulu city) | Handwashing with soap and alcohol-based oily disinfectant use, plus cleaning environment (staff lecture on infection prevention; cleaning toys; staff encouraged to take sick leave at first sign of symptoms) | Standard practice | Day care centre | 20 10 intervention 10 controls (matched pairs) |
RCT, randomised controlled trial; WASH, Water, Sanitation and Hygiene.
Study participants
Age of participating children was not always reported. Five of the 13 school-based studies included all children in each school;26 27 37 39 41 others included one or more age grade. Six studies included children under 3 years.19 24 37 46 47 53 These were retained because the interventions included hand hygiene for children as well as staff. Four studies included students over the typical maximum primary school age of 11 years.27 34 36 37 These were retained because students’ education level was likely to be equivalent to students in other contexts.
Country location and setting
Thirteen studies were school-based; five were in day care facilities or preschools. Institutions were not necessarily representative of settings in that country. For example, one study only included schools with continuous water supply.45 Eleven studies were in high-income countries (defined using World Bank categories54); only two did not involve hand sanitiser.19 48 Four studies were from middle-income countries;24 33 45 46 three were from one low-income country (Kenya).34 36 37
Interventions and comparators
Twelve interventions included hand sanitiser;22–27 37 39 41 46 47 53 six focused on handwashing with soap.19 33 34 36 45 48 Several interventions included additional infection control measures, such as eliminating shared cups,48 water treatment and building new latrines,34 36 cleaning toys or equipment.25 53 Five included a home component such as parental information.19 33 41 45 48
Fourteen studies compared interventions with ‘standard practice’ but this was often unclearly defined. One study was placebo-controlled,26 three compared an intervention with an alternative intervention.23 36 39 Four studies compared two interventions and a control.24 33 34 37 Only two studies adopted a multifactorial design to test the effect of different intervention components.24 37
Hand hygiene protocols varied. For example, only 7 of the 12 studies including hand sanitiser described the frequency and/or intensity of use. Nine interventions lasted 10 weeks or less.19 22 23 25 26 33 34 37 48
Outcomes
The online supplementary table S2 presents study results according to review outcomes. Only three studies34 36 46 did not report absence outcomes. Six studies presented results concerning RT infection and/or symptoms;33 37 41 45 46 53 four presented results concerning GI infection and/or symptoms.33 37 46 53 Two studies reported laboratory results, both pertaining to influenza-like illness (ILI).41 45 Six studies presented knowledge, attitude and/or behavioural outcomes.34 36 37 41 48 53 No study reported hospital admissions due to infection. Four studies presented staff outcomes.36 37 48 53
Outcome definitions and summary measures varied. Three reports did not clearly define illnesses or symptoms.23 47 48 Some only reported adjusted outcomes (variables differed between studies).
Risk of bias within studies
Methodological issues increased risk of bias in most studies (see online supplementary table S1, reviewers’ assessment of the quality and risk of bias of included studies). Some issues highlight difficulties in evaluating behaviour change (eg, lack of participant blinding); others indicate study design weaknesses (eg, random sequence generation) and inadequate reporting (eg, only reported statistically significant results).
Five studies described an adequate method of random sequence generation,39 41 45 46 53 only two adequately described allocation concealment.39 41 Perhaps unsurprisingly given the nature of the intervention, only the study where a placebo hand sanitiser was the comparator was judged to be at low risk of performance bias.26 Only one study39 was assessed as having adequately described all measures to blind outcome assessors. The completeness of data reported for each outcome was assessed as adequate in five studies;23 25 39 46 48 high risk of selective reporting was identified in four studies.24 26 37 41
Four reports did not present baseline data.19 22 23 26 Despite being concerned with illness outcomes, only eight reported baseline health data.24 25 27 39 46–48 53
Six studies22–28 had clusters at class level (two of these applied a cross-over design), therefore increasing risk of contamination between study arms. Not all investigators took clustering into account in sample size calculation or analysis.
Three studies were funded by companies producing hygiene products,23 25 33 three used manufacturer-donated products,22 37 46 one required parents to provide soap and hand drying materials.45 It is unclear whether the way in which these interventions were resourced affected their acceptability, sustainability or study outcomes: only two study reports state the role of these companies in the study, analysis and report. 25 33
Most reports described the intervention protocol and monitoring, three noted intervention costs24 28 46 but few presented process evaluation data.
Most outcome measurement methods could have introduced bias due to poor case definition, use of non-validated tools or self-report (including routine school absence reporting data). Some studies which attempted to validate outcomes (eg, illness) experienced attrition due to the complexity of the process (ref. 41, p.3).
Individual study results
Five of the six studies reporting children's absence and 8 of the 13 studies measuring children's illness absence reported an intervention effect (see online supplementary table S2 for study results according to review outcomes). The one study reporting staff illness absence found it was higher among the intervention group53 which may be because the intervention included asking staff not to attend work if they had infection symptoms.
All five studies reporting RT infection incidence showed a reduction, but each applied different outcome definitions. Three reported RT infection symptoms (rhinitis, cough); one53 found a reduction in both, one37 only identified a reduction in observed rhinorrhoea and another33 found no change in cough and a 12% increase in rhinorrhoea episodes (‘standard’ intervention vs control).
Two studies reported GI incidence; one reported a reduction,46 the other did not.53 Only one of three studies recording diarrhoeal symptoms found any effect.37 Two studies reported vomiting outcomes,37 53 only one found an effect.53
Two studies41 45 collecting laboratory results found some evidence of decreased ILI, although in one study this only related to influenza A (ref. 41, Supplemental Digital Content (SDC) 2).
Four of five studies reporting children's behaviour change identified a positive intervention effect.34 37 41 48 All five studies reporting changes in children's and/or staff hand hygiene knowledge, attitudes and/or beliefs found an intervention effect.34 37 41 51 53
Synthesis of results
Due to study heterogeneity and the generally low quality of study design and of study reporting, coauthors agreed that it could be misleading to present pooled estimates of the effect of interventions using MAs.
Discussion
Main findings
We found 18 cluster RCTs investigating the effect of interventions with a hand hygiene component on absence and infection among 3–11-year-old children in educational settings. Individual study results suggest interventions may reduce children's absence, RT infection incidence and symptoms, and laboratory-confirmed ILI. They may also improve children's and staff hand hygiene attitudes, knowledge and behaviour. Evidence of impact on GI infection or symptoms was equivocal. Despite updating existing SRs and identifying new studies, individual study results appear to show that there remains equipoise about the effectiveness of hand hygiene in preventing RT and GI infection.
Strengths and limitations of this review
Much has been made of the potential of hand hygiene interventions for reducing infection in this population.11 This review provides a more detailed assessment of such interventions and how promising they might be based on studies which apply the most rigorous, RCT evidence. This review updates existing SRs focused on this population, and our comprehensive search strategy resulted in finding more studies than previous SRs. Findings of this review corroborate existing SRs; that studies have significant design limitations and poor quality reporting. The quality of reporting in more recently published studies27 28 39 seems to have improved which perhaps indicates the impact of guidance on the reporting of cluster RCTs.20 21 This may result in improved evidence, capable of demonstrating the effectiveness of this important public health issue. Despite identifying new studies, it was not possible to produce meaningful MAs (as earlier SRs have found) due to study heterogeneity, study design limitations and poor quality reporting.
Limitations of this SR include that: we assumed that report titles or abstracts would contain ‘handwashing’ or ‘hand/s’ but they did not; unpublished literature was excluded; some included studies had study populations which included children younger and older than the prespecified review age range; RT and GI infection incidence can vary within the age range included in the review, as can the potential effectiveness of interventions (due to children's developmental stage); risk of bias assessment was impeded by inadequate reporting. Furthermore, all interventions with a hand hygiene component were included so the impact of hand hygiene cannot be isolated. This review does not distinguish between handwashing with soap or hand sanitiser use even though these methods may have different resource implications and be differentially effective in eliminating certain pathogens.55
What this study adds
While studies are heterogeneous, there is evidence that hand hygiene interventions among primary school-aged children in educational settings may be beneficial, particularly in reducing RT infection incidence. However, this SR highlights limitations of evidence on this crucial public health issue in a key setting with a vulnerable population and the need for improved studies to enable more definitive assessment (eg, MA) of the effectiveness of simple public health interventions to inform practice. We have four recommendations for future research and which may enable future estimates of the pooled effects of such interventions using MA.
First, better designed and reported cluster RCTs are required. Investigators should apply guidance20 21 and learn from robust studies39 in order to avoid design flaws (eg, clusters at classroom level) and improve reporting (eg, children's age, control group conditions). Second, studies should incorporate technical advances for outcome measurement, such as the use of environmental swabs to detect the level of viral and/or bacterial contamination in schools56 which may enable robust, standardised outcome measures instead of using self-report and observations. Third, research should include process evaluation to refine interventions and establish intervention acceptability and fidelity. Studies which have done process evaluations40 57 have identified barriers to hand hygiene including access to adequate sanitary facilities (even in high-income countries), suggesting that provision of hygiene products and education may be insufficient to achieve effective infection prevention and control and more robust studies of complex, multicomponent interventions are required. Fourth, studies should evaluate cost, cost-effectiveness and intervention sustainability in educational settings.
Conclusion
Interventions to improve hand hygiene in educational settings may reduce RT infection incidence among younger children. More robust, well reported studies are required, especially of multicomponent interventions.
Supplementary Material
Acknowledgments
The authors thank Val Hamilton for constructing the search strategy and doing the database search in 2011 and 2012; Dagmar Luettel, Lone Gale and Julianna Photopoulos for their translations. Beki Langford advised on the review process; Kate Tilling, Deborah Caldwell and Hayley Jones provided statistical advice.
Footnotes
Contributors: The manuscript has been read and approved by all authors. RC, SB, AN conceived and instigated the study. RC, SB, AN and MW drafted the protocol. MW conducted the 2014 search and all citation searches. MW, GJM and AN screened the results. MW, AN and HB extracted the data and assessed the quality of studies. RC and SB were moderators. MW and RC analysed the data. MW drafted the manuscript for publication. All authors contributed to this report and subsequent revisions. Each author believes that the manuscript represents honest work.
Funding: This work was undertaken with the support of NIHR Research for Patient Benefit Grant (PB-PG-1207-15212) and of The Centre for the Development and Evaluation of Complex Interventions for Public Health Improvement (DECIPHer), a UKCRC Public Health Research Centre of Excellence. Joint funding (MR/KO232331/1) from the British Heart Foundation, Cancer Research UK, Economic and Social Research Council, Medical Research Council, the Welsh Government and the Wellcome Trust, under the auspices of the UK Clinical Research Collaboration, is gratefully acknowledged. Views expressed in this paper do not represent those of the funders. The funders had no role in study design, data collection and analysis, decision to publish or manuscript preparation.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Additional unpublished data from the study (data extraction forms, attempted meta-analyses) are available on request from the corresponding author.
References
- 1.DfE. The link between absence and attainment at KS2 and KS4. 2012/13 Academic Year. Research Report London: Department for Education, 2015. [Google Scholar]
- 2.PHE. The link between pupil health and wellbeing and attainment: A briefing for head teachers, governors and staff in education settings. London: Public Health England, 2014. [Google Scholar]
- 3.Bowers T. Teacher absenteeism and ill health retirement: a review. Cambridge J Educ 2001;31:135–57. 10.1080/0305764012006119 [DOI] [Google Scholar]
- 4.Monto AS. Studies of the community and family: acute respiratory illness and infection. Epidemiol Rev 1994;16:351–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nafstad P, Hagen JA, Botten G, et al. Lower respiratory tract infections among Norwegian infants with siblings in day care. Am J Public Health 1996;86:1456–9. 10.2105/AJPH.86.10.1456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aiello A, Coulborn R, Perez V, et al. Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health 2008;98:1372–81. 10.2105/AJPH.2007.124610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: a systematic review. Lancet Infect Dis 2003;3:275–81. 10.1016/S1473-3099(03)00606-6 [DOI] [PubMed] [Google Scholar]
- 8.Ejemot RI, Ehiri JE, Meremikwu MM, et al. Hand washing for preventing diarrhoea. Cochrane Database Syst Rev 2008;(1):CD004265 10.1002/14651858.CD004265.pub2 [DOI] [PubMed] [Google Scholar]
- 9.Freeman MC, Stocks ME, Cumming O, et al. Hygiene and health: systematic review of handwashing practices worldwide and update of health effects. Trop Med Int Health 2014;19:906–16. 10.1111/tmi.12339 [DOI] [PubMed] [Google Scholar]
- 10.Jasper C, Le TT, Bartram J. Water and sanitation in schools: a systematic review of the health and educational outcomes. Int J Environ Res Public Health 2012;9:2772–87. 10.3390/ijerph9082772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jefferson T, Del Mar C, Dooley L, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ 2009;339:b3675 10.1136/bmj.b3675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joshi A, Amadi C. Impact of water, sanitation, and hygiene interventions on improving health outcomes among school children. J Environ Public Health 2013;2013:984626 10.1155/2013/984626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meadows E, Le Saux N. A systematic review of the effectiveness of antimicrobial rinse-free hand sanitizers for prevention of illness-related absenteeism in elementary school children. BMC Public Health 2004;4:50 10.1186/1471-2458-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rabie T, Curtis V. Handwashing and risk of respiratory infections: a quantitative systematic review. Trop Med Int Health 2006;11:258–67. 10.1111/j.1365-3156.2006.01568.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Warren-Gash C, Fragaszy E, Hayward AC. Hand hygiene to reduce community transmission of influenza and acute respiratory tract infection: a systematic review. Influenza Other Respir Viruses 2013;7:738–49. 10.1111/irv.12015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson J, Wang D, Meads C. Simple interventions to prevent respiratory and gastrointestinal infection in children in day care and school settings—a systematic review and economic evaluation. Birmingham: West Midlands Health Technology Assessment Collaboration, 2006. [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nicholson A, Willmott M, Brookes S, et al. A systematic review to evaluate the evidence of the effectiveness of hand washing in reducing the spread of infectious illness in primary schools. Protocol. Bristol: DECIPHer, University of Bristol, 2012. http://decipher.uk.net/research-page/handwashing-absenteeism/ (accessed 27 Apr 2015). [Google Scholar]
- 19.Ladegaard MB, Stage V. Hand-hygiene and sickness among small children attending day care centers. An intervention study. Ugeskr Laeger 1999;161:4396–400. [PubMed] [Google Scholar]
- 20.Schulz K, Altman D, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Campbell MK, Piaggio G, Elbourne DR, et al. Consort 2010 statement: extension to cluster randomised trials. BMJ 2012;345:e5661 10.1136/bmj.e5661 [DOI] [PubMed] [Google Scholar]
- 22.Morton JL, Schultz AA. Healthy Hands: use of alcohol gel as an adjunct to handwashing in elementary school children. J Sch Nurs 2004;20:161–7. 10.1177/10598405040200030601 [DOI] [PubMed] [Google Scholar]
- 23.Vessey JA, Sherwood JJ, Warner D, et al. Comparing hand washing to hand sanitizers in reducing elementary school students’ absenteeism. Pediatr Nurs 2007;33:368–72. [PubMed] [Google Scholar]
- 24.Pandejpong D, Danchaivijitr S, Vanprapa N, et al. Appropriate time-interval application of alcohol hand gel on reducing influenza-like illness among preschool children: A randomized, controlled trial. Am J Infect Control 2012;40:507–11. 10.1016/j.ajic.2011.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sandora TJ, Shih MC, Goldmann DA. Reducing absenteeism from gastrointestinal and respiratory illness in elementary school students: a randomized, controlled trial of an infection-control intervention. Pediatrics 2008;121:e1555–62. 10.1542/peds.2007-2597 [DOI] [PubMed] [Google Scholar]
- 26.White CG, Shinder FS, Shinder AL, et al. Reduction of illness absenteeism in elementary schools using an alcohol-free instant hand sanitizer. J Sch Nurs 2001;17:258–65. 10.1177/10598405010170050501 [DOI] [PubMed] [Google Scholar]
- 27.Azor-Martínez E, Cobos-Carrascosa E, Gimenez-Sanchez F, et al. Effectiveness of a multifactorial handwashing program to reduce school absenteeism due to acute gastroenteritis. Pediatr Infect Dis J 2014;33:e34–9. 10.1097/INF.0000000000000040 [DOI] [PubMed] [Google Scholar]
- 28.Azor-Martínez E, Gonzalez-Jimenez Y, Seijas-Vazquez ML, et al. The impact of common infections on school absenteeism during an academic year. Am J Infect Control 2014;42:632–7. 10.1016/j.ajic.2014.02.017 [DOI] [PubMed] [Google Scholar]
- 29.Johansen A, Denbæk AM, Thørring Bonnesen C, et al. The Hi Five study: design of a school-based randomized trial to reduce infections and improve hygiene and well-being among 6-15 year olds in Denmark. BMC Public Health 2015;15:207 10.1186/s12889-015-1556-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Overgaard HJ, Alexander N, Mátiz MI, et al. Diarrhea and dengue control in rural primary schools in Colombia: Study protocol for a randomized controlled trial. Trials 2012;13:182 10.1186/1745-6215-13-182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zomer TP, Erasmus V, Vlaar N, et al. A hand hygiene intervention to decrease infections among children attending day care centers: design of a cluster randomized controlled trial. BMC Infect Dis 2013;13:259 10.1186/1471-2334-13-259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bowen A. Evaluation of a school-based handwashing promotion program in three countries. Clinical Trials identifier: NCT010438092010. http://clinicaltrials.gov/show/NCT01043809 (accessed 27 Apr 2015).
- 33.Bowen A, Ma H, Ou J, et al. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Am J Trop Med Hyg 2007;76:1166–73. [PubMed] [Google Scholar]
- 34.Freeman MC, Clasen T, Dreibelbis R, et al. The impact of a school-based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: a cluster-randomized trial. Epidemiol Infect 2014;142:340–51. 10.1017/S0950268813001118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Greene LE, Freeman MC, Akoko D, et al. Impact of a school-based hygiene promotion and sanitation intervention on pupil hand contamination in Western Kenya: a cluster randomized trial. Am J Trop Med Hyg 2012;87:385–93. 10.4269/ajtmh.2012.11-0633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Graves JM, Daniell WE, Harris JR, et al. Enhancing a safe water intervention with student-created visual aids to promote handwashing behavior in Kenyan primary schools. Int Q Community Health Educ 2011;32:307–23. 10.2190/IQ.32.4.d [DOI] [PubMed] [Google Scholar]
- 37.Pickering AJ, Davis J, Blum AG, et al. Access to waterless hand sanitizer improves student hand hygiene behavior in primary schools in Nairobi, Kenya. Am J Trop Med Hyg 2013;89:411–18. 10.4269/ajtmh.13-0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McKenzie JE, Priest P, Audas R, et al. Hand sanitisers for reducing illness absences in primary school children in New Zealand: a cluster randomised controlled trial study protocol. Trials 2010;11:7 10.1186/1745-6215-11-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Priest P, McKenzie JE, Audas R, et al. Hand sanitiser provision for reducing illness absences in primary school children: a cluster randomised trial. PLoS Med 2014;11:e1001700 10.1371/journal.pmed.1001700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reeves LM, Priest PC, Poore MR. School toilets: facilitating hand hygiene? A review of primary school hygiene facilities in a developed country. J Public Health 2012;34:483–8. 10.1093/pubmed/fds028 [DOI] [PubMed] [Google Scholar]
- 41.Stebbins S, Cummings DA, Stark JH, et al. Reduction in the incidence of influenza A but not influenza B associated with use of hand sanitizer and cough hygiene in schools: a randomized controlled trial. Pediatr Infect Dis J 2011;30:921–6. 10.1097/INF.0b013e3182218656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stebbins S, Downs JS, Vukotich CJ Jr. Using nonpharmaceutical interventions to prevent influenza transmission in elementary school children: parent and teacher perspectives. J Public Health Manag Pract 2009;15:112–17. 10.1097/01.PHH.0000346007.66898.67 [DOI] [PubMed] [Google Scholar]
- 43.Stebbins S, Downs JS, Vukotich CJ. The effect of grade on compliance using nonpharmaceutical interventions to reduce influenza in an urban elementary school setting. J Public Health Manag Pract 2011;17:65–71. 10.1097/PHH.0b013e3181e83f42 [DOI] [PubMed] [Google Scholar]
- 44.Stebbins S, Stark JH, Vukotich CJ. Compliance with a multilayered nonpharmaceutical intervention in an urban elementary school setting. J Public Health Manag Pract 2010;16:316–24. 10.1097/PHH.0b013e3181cb4368 [DOI] [PubMed] [Google Scholar]
- 45.Talaat M, Afifi S, Dueger E, et al. Effects of hand hygiene campaigns on incidence of laboratory-confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerg Infect Dis 2011;17:619–25. 10.3201/eid1704.101353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Correa JC, Pinto D, Salas LA, et al. A cluster-randomized controlled trial of handrubs for prevention of infectious diseases among children in Colombia. Rev Panam Salud Publica 2012;31:476–84. 10.1590/S1020-49892012000600005 [DOI] [PubMed] [Google Scholar]
- 47.Lennell A, Kühlmann-Berenzon S, Geli P, et al. Alcohol-based hand-disinfection reduced children's absence from Swedish day care centers. Acta Paediatr 2008;97:1672–80. 10.1111/j.1651-2227.2008.01057.x [DOI] [PubMed] [Google Scholar]
- 48.Rosen L, Manor O, Engelhard D, et al. Can a handwashing intervention make a difference? Results from a randomized controlled trial in Jerusalem preschools. Prev Med 2006;42:27–32. 10.1016/j.ypmed.2005.09.012 [DOI] [PubMed] [Google Scholar]
- 49.Rosen L, Manor O, Engelhard D, et al. Design of the Jerusalem Handwashing Study: meeting the challenges of a preschool-based public health intervention trial. Clin Trials 2006;3:376–84. 10.1177/1740774506070690 [DOI] [PubMed] [Google Scholar]
- 50.Rosen L, Manor O, Engelhard D, et al. Erratum: Design of the Jerusalem Handwashing Study: Meeting the challenges of a preschool-based public health intervention trial (Clinical Trials (2006) 3, (376–384)). Clin Trials 2007;4:475 10.1177/1740774507083366 [DOI] [PubMed] [Google Scholar]
- 51.Rosen L, Zucker D, Brody D, et al. The effect of a handwashing intervention on preschool educator beliefs, attitudes, knowledge and self-efficacy. Health Educ Res 2009;24:686–98. 10.1093/her/cyp004 [DOI] [PubMed] [Google Scholar]
- 52.Rosen L, Zucker D, Brody D, et al. Enabling hygienic behavior among preschoolers: improving environmental conditions through a multifaceted intervention. Am J Health Promot 2010;25:248–56. 10.4278/ajhp.081104-QUAN-265 [DOI] [PubMed] [Google Scholar]
- 53.Uhari M, Möttönen M. An open randomized controlled trial of infection prevention in child day-care centers. Pediatr Infect Dis J 1999;18:672–7. 10.1097/00006454-199908000-00004 [DOI] [PubMed] [Google Scholar]
- 54.World Bank. Data: Country and Lending Groups. 2015. http://data.worldbank.org/about/country-and-lending-groups (accessed 1 Sep 2015). [Google Scholar]
- 55.Bloomfield SF, Aiello AE, Cookson B, et al. The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including handwashing and alcohol-based hand sanitizers. Am J Infect Control 2007;35:S27–64. 10.1016/j.ajic.2007.07.001 [DOI] [Google Scholar]
- 56.Boxman IL, Dijkman R, te Loeke NAJM, et al. Environmental swabs as a tool in norovirus outbreak investigation, including outbreaks on cruise ships. J Food Prot 2009;72:111–19. [DOI] [PubMed] [Google Scholar]
- 57.Chittleborough CR, Nicholson AL, Young E, et al. Implementation of an educational intervention to improve hand washing in primary schools: process evaluation within a randomised controlled trial. BMC Public Health 2013;13:757 10.1186/1471-2458-13-757 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.