Abstract
Background and Objectives
Illicit drug use, particularly of cannabis, is common among opiate-dependent individuals, and has the potential to impact treatment in a negative manner.
Methods
To examine this, patterns of cannabis use prior to and during methadone maintenance treatment (MMT) were examined to assess possible cannabis-related effects on MMT, particularly during methadone stabilization. Retrospective chart analysis was used to examine outpatient records of patients undergoing MMT (n=91), focusing specifically on past and present cannabis use and its association with opiate abstinence, methadone dose stabilization, and treatment compliance.
Results
Objective rates of cannabis use were high during methadone induction, dropping significantly following dose stabilization. History of cannabis use correlated with cannabis use during MMT, but did not negatively impact the methadone induction process. Pilot data also suggested that objective ratings of opiate withdrawal decrease in MMT patients using cannabis during stabilization.
Conclusions and Scientific Significance
The present findings may point to novel interventions to be employed during treatment for opiate dependence that specifically target cannabinoid-opioid system interactions.
1. Introduction
Methadone maintenance treatment (MMT) is an opiate agonist pharmacotherapy prescribed for opiate-dependent individuals as a means of extinguishing illicit opiate use and reducing associated risk behaviors 1, 2. Initiation on methadone maintenance treatment is a federally regulated process that requires slow and careful titration of methadone dosing to avoid risk of overmedication. Dose titration proceeds through initiation, induction, and stabilization phases prior to reaching a maintenance phase 3–5. The initial period of methadone dose stabilization is one of particular vulnerability to relapse due to the persistence of low-moderate grade opiate withdrawal and associated stress during dose titration 6–10. Non-opiate illicit drug use often persists during the early phases of treatment for opiate dependence 11–18, promoted at least in part by the experience of withdrawal and craving. There is a limited amount of research focused on the impact of continued non-opiate substance use on methadone dose titration and overall treatment compliance.
Cannabis (marijuana) is commonly used in combination with heroin or oral opiates, in addition to other substances such as cocaine and benzodiazepines 19–21. In several studies of non-opiate illicit drug use in opiate-dependent individuals, rates of cannabis use were shown to remain high during treatment for opiate dependence 15, 22–25. Several groups have investigated the impact of cannabis use on various measures of treatment outcome and success, such as retention in treatment or compliance 16, 23–28. However, very limited research has focused specifically on the impact of cannabis exposure during the process of methadone dose titration (referred to herein as methadone induction) and the early stabilization phase. The present study sought to examine the trends in cannabis use of individuals during the early phases of MMT initiation in order to test the hypothesis that cannabis use may impact illicit drug use, and subsequently methadone stabilization. Based on findings from experimental models of opiate dependence, it is hypothesized that the use of cannabinoids, via its interaction with the opioid system, may impact opioid signaling in the brain 29–36. Multiple groups have reported synergy between cannabinoids and opiates when administered concurrently 10, 37–40. The present study attempted to investigate whether similar evidence of cannabinoid-opioid interactions can be found in the clinical setting among treatment-seeking opiate-dependent individuals. The authors hypothesized that cannabis use may increase during dose titration, and that this elevated use may impact methadone induction and stabilization on MMT. Additionally, associations between pre-treatment history of opiate and cannabis use were examined as they relate to methadone dosing and titration, and illicit drug use during treatment.
2. Materials and Methods
The data presented in this retrospective study were collected from outpatient charts belonging to individuals enrolled in the Narcotic Addiction Rehabilitation Program (NARP) at Thomas Jefferson University in Philadelphia, PA. This urban, publicly funded and university-sponsored clinic offers medication-assisted treatment and intensive outpatient programs for opiate dependence. Criteria for admission to treatment included a minimum of one-year documented history of opiate use, being at least 18 years of age, and a positive opiate urine drug screen (UDS) at admission. Approximately 365 individuals were enrolled in NARP at any given point in time over the past decade. This study was approved by the Institutional Review Board of Thomas Jefferson University.
2.1. Sample Criteria
Criteria for study inclusion were a minimum of nine months in treatment and the presence of the following data in the outpatient chart: monthly urinary drug screen results, treatment compliance (daily attendance), and medical intake evaluation information. In order to capture data from the weeks both prior to and immediately following methadone dose stabilization, the time in treatment criteria was established at a minimum of nine months. Charts were sampled from individuals that were enrolled in NARP between December 1, 2005 and July 1, 2009 (approximately 500 in total). The authors collected and analyzed data from all criteria-meeting patients that had at least one cannabis-positive urinary drug screen (UDS) during treatment (n=56). An additional random sample of 35 non-cannabis using individuals from the same enrollment period was used as a comparison group. These charts were pulled using a random number generator and were selected for the study if all inclusion criteria were met.
2.2. Treatment enrollment and structure
As part of the intake process, individuals seeking admission participated in a structured clinical interview and medical evaluation where detailed drug use histories were collected. Individuals were then initiated on methadone maintenance therapy according to federal guidelines, with assigned daily medication times. Dosing was slowly titrated until a blocking dose of methadone was achieved and opiate craving and use were controlled. For the purposes of this project, dose stabilization was defined as a period of eight weeks at a constant dose of methadone. Acquisition of this dose marked the transition from methadone induction to early stabilization phase in patients. Progress was monitored through regular meetings with counselors and medical staff, as well as UDS performed at least once-monthly on a random basis. During the titration period, in which low to moderate-grade opiate withdrawal symptoms were typically experienced, the Clinical Opiate Withdrawal Scale (COWS) (21) was administered by the medical staff as needed to help assess the need for dose increases, and periodically thereafter when dose changes were requested or needed.
2.3. Plan of Analysis
Study data was analyzed as follows using SPSS 16.0 Graduate Pack software. The authors first examined whether a history of pre-treatment cannabis use was associated with proxy measures of opiate addiction and severity (i.e., daily opiate expenditure, number of previous opiate dependence treatment episodes, and cumulative years of opiate use). Next, the patterns and effects of both pre-treatment and in-treatment cannabis use on methadone induction and opiate use were studied. Recent cannabis history (dichotomized as Yes/No) referred to any self-reported history of cannabis use in the month prior to enrollment in treatment. Data on in-treatment cannabis use was recorded from urinalyses conducted during the initial 9 months of MMT enrollment. To test the hypothesis that cannabis use impacts the process of methadone induction, a series of ANOVAs were conducted using either recent cannabis history or cannabis use during methadone induction as independent variables. Because illicit drug use during stabilization could have potentially complicated the dose titration process, the dependent measures included: 1. rates of cannabis and opiate drug use during the methadone induction phase and early stabilization phase, 2. the number of weeks required to complete methadone dose titration (induction), 3. the methadone blocking dose upon stabilization, and 4. medication compliance (attendance for daily methadone administration). Parallel ANCOVAs were conducted for each operationalization of the independent variable, using daily opiate expenditure as a covariate to control for pre-treatment opiate use/severity of dependence. In this manner, it was possible to study how the patterns of cannabis use interact with opiate dependence prior to treatment, and also the possible impact of cannabis use on MMT and opiate use during two critical phases of treatment: methadone induction and early stabilization.
3. Results
3.1. Sample Statistics
Data from a total of 91 individuals were recorded. Due to the limited availability of certain data in the clinical record, some analyses were performed on a smaller subset of cases. Average age at admission was 39 ± 11 years, and ranged from 20-62 years of age. Sixty percent (n=55) of subjects were male. Almost eighty percent (n=70) of subjects were Caucasian, the remainder were African American (n=12, 13.5%), and Hispanic (n=6, 6.7%). The majority of the sample were intravenous drug users (n=61, 67.0%), but oral narcotic (n=44, 50%) and intranasal administration (n=43, 49.4%) was also commonly reported. In the month prior to entering treatment, almost half of the individuals (46.6%) were using multiple substances (benzodiazepines, cannabis, or stimulants) in addition to opiates. (See Table 1)
Table 1.
Descriptive Characteristics
| Variable | N | Values |
|---|---|---|
| Age | ||
| Mean | 91 | 39.37 |
| Standard Deviation | ± 11.29 | |
| Range | 20–62 | |
|
| ||
| Stable Methadone Blocking Dose | ||
| Mean | 85* | 111.98mg/day |
| Standard Deviation | ± 60.80 | |
| Range | 20–330 | |
|
| ||
| Weeks to Stabilization | ||
| Mean | 91 | 11.01 |
| Standard Deviation | ± 9.38 | |
| Range | 1–56** | |
|
| ||
| Variable | N | Percentage |
|
| ||
| Gender | ||
| Female | 55 | 60.4% |
| Male | 36 | 39.6% |
|
| ||
| Race/Ethnicity | ||
| African America | 12 | 13.5% |
| Caucasian | 70 | 78.7% |
| Hispanic | 6 | 6.7% |
| Other | 1 | 1.1% |
|
| ||
| Opiate Route of Administration⋄ | ||
| Intravenous | 67.8 % | |
| Oral | 91 | 50% |
| Intranasal | 49.4% | |
| Combination of ≥ 2 of the Above | 38.9% | |
|
| ||
| History of Illicit Drug Use: Lifetime+⋄ | ||
| Marijuana | 91 | 71.5% |
| Stimulants | 64.8% | |
| Benzodiazepines | 70.3% | |
| Combination of ≥ 2 of the Above | 80.2% | |
|
| ||
| History of Illicit Drug Use: Recent+⋄ | ||
| Marijuana | 42%++ | |
| Stimulants | 91 | 39.3% |
| Benzodiazepines | 51.7% | |
| Combination of ≥ 2 of the Above | 46.6% | |
6 individuals did not stabilize within the initial 9 month period
only data from those that stabilized within the initial 9 month period were considered.
values do not sum to 100% due to poly-drug use.
in addition to opiates
values may be biased by purposeful sampling for cannabis use while in treatment.
Analysis of stabilization involved examination of two distinct treatment phases during the time period from enrollment through month nine of treatment. “Methadone induction phase” was used to refer to the period of time during which an individual’s methadone dose was titrated to a stable blocking dose, while “early stabilization phase” denoted the remainder of the nine month study period following acquisition of a blocking dose. Almost all subjects (n=85) were able to achieve a stable blocking dose of methadone (x=112.42±61.03mg) within an average of 11±9.4 weeks. For a variety of reasons, 6 of the 91 subjects were unable to achieve a stable blocking dose during the study timeframe. In the nine months following enrollment, subjects on average missed daily dosing 18.5±24.6 times. Stabilization on MMT, operationalized in this study as 8 weeks on a stable methadone dose, was associated with a significant decrease in the percentage of opiate-positive UDS. A within-subjects comparison of opiate use between methadone induction and early stabilization treatment phases revealed an approximately 50% decrease in the mean percentage of opiate-positive UDS [57.4 to 28.2%, t(82)=6.58, p<0.001]. Cannabis use during stabilization on MMT was examined next. (See Table 1)
3.2. Cannabis use: pre-treatment history and use during methadone induction
Data on self-reported pre-treatment cannabis use was gathered from information recorded during the intake medical evaluation. Within the sample, 28.6% (n=26) individuals reported no history of cannabis use, past or recent (i.e., 30 days prior to enrollment). While 31.9% (n=29) of subjects reported past but no recent cannabis use, almost 40% (n=36) reported past and recent cannabis use. During the nine-month study period, 38.5% were cannabis-abstinent (n=35), while 61.5% (n=56) used cannabis at least once. Not surprisingly, when examining the relationship between pre-admission reports of marijuana use and urine results in the first nine-months of treatment, a strong positive effect was observed (r=0.736, p< 0.001). Evidence of ongoing cannabis use was also examined. Based on monthly UDS results during the first nine months of enrollment, cannabis using individuals were classified as occasional users (1-3 months cannabis-positive, n=27) or frequent users (> 3 months cannabis, n = 29). There was a positive correlation between rates of cannabis use and illicit benzodiazepine use during the initial nine months in treatment: r(91)=0.374, p<0.01. (See Table 2)
Table 2.
Patterns of Cannabis Use in the Sample
| Cannabis use history | n | Percentage | Frequency of cannabis use in-treatment | n | Percentage |
|---|---|---|---|---|---|
|
| |||||
| No Lifetime/No Recent | 26 | 28.6% | Abstinent | 35 | 38.5% |
| Yes Lifetime/No Recent | 29 | 31.9% | Occasional | 27 | 29.7% |
| Yes Lifetime/Yes Recent | 36 | 39.6% | Heavy | 29 | 31.9% |
|
| |||||
| Rate of Cannabis Use+ | Change & SD | Statistics | |||
|
| |||||
| Individuals with lifetime cannabis history | |||||
| Methadone induction phase | 48.8% | −11.2±42.9% | t(56) = 1.96 | ||
| Early stabilization phase | 37.6% | p = 0.055 | |||
|
| |||||
| Individuals with recent cannabis history | |||||
| Methadone induction phase | 74.6% | −25.3±45.2% | t(33) = 3.27 | ||
| Early stabilization phase | 49.3% | p = 0.003 | |||
|
| |||||
| Correlations | r value | p value | |||
|
| |||||
| Cannabis use: prior to & during treatment | r(80)=0.736 | p<0.001 | |||
|
| |||||
| Pre-stabilization cannabis use & unfavorable discharge status | r(80)=0.069 | p=0.567 | |||
|
| |||||
| Pre-stabilization cannabis use & MMT attendance | r(65)=0.151 | p=0.230 | |||
|
| |||||
| Rate of cannabis use & opiate use (during treatment) | r(82)=0.018 | p=0.873 | |||
|
| |||||
| Cannabis use during treatment & age | r(91)= −0.210 | p=0.047 | |||
|
| |||||
| Rate of cannabis use & daily opiate expenditure | r(49)= −0.313 | p=0.028 | |||
Percentage of positive UDS*
cutoff for cannabis-positive result is 50ng/ml
3.3. Role of drug use history and proxy measures of addiction severity in cannabis use
Opiate addiction history and severity of dependence at treatment intake was assessed via several proxy measures reported in the intake medical evaluation: years of opiate abuse, number of previous treatment episodes for opiate dependence (excluding Narcotics Anonymous), and daily opiate expenditure. The following analyses included data from all individuals in the sample providing complete information. In addition to having 2.42 ±1.70 (n=51) previous episodes in treatment, individuals had an average of a 15.68 ±10.71 (n=71) year history of opiate abuse upon presentation to the clinic for treatment, and spent an average of $108.00 ±65.00 (n=49) per day on opiates.
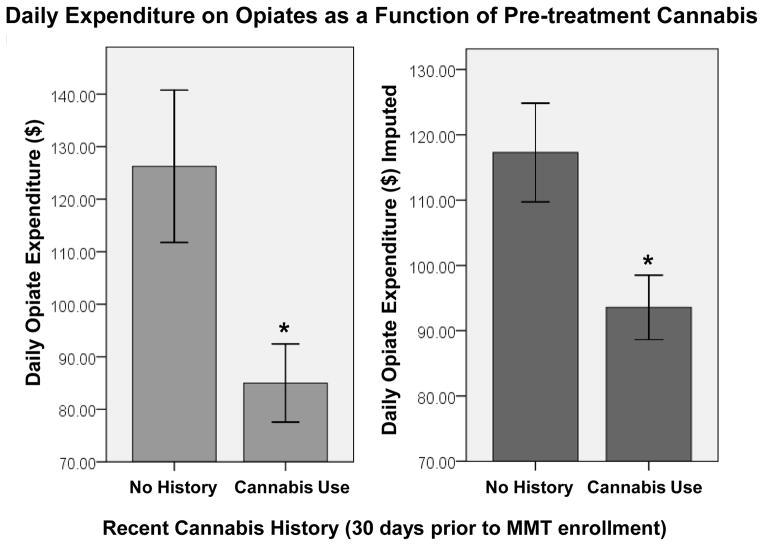
To test the hypothesis that cannabis users may actually use less opiates and possibly constitute a unique subset of opiate-dependent individuals, analyses were performed to examine whether pre-treatment cannabis use was associated with any of the proxy measures of opiate addiction severity. Neither years of opiate abuse nor number of previous treatment episodes differed based on history of recent cannabis use [t(71)=0.026, p=0.796 and t(51)=01.360, p=0.178, respectively]. Interestingly, decreased daily opiate expenditure spent on opiates (i.e. pre-treatment opiate use) was associated with a history of recent cannabis use (Mn=$85.00) when compared to those with no recent cannabis use (Mn=$126.25) [t(49)= 2.373, p=0.022]. (Figure 1) These data indicate that cannabis users appear to spend less per day on the purchase of opiates, and may in turn use a lesser amount of opiates daily.
Figure 1.
Subsequent analyses included daily opiate expenditure as a covariate in an attempt to control for variation based upon the amount of pre-treatment opiate use. For all subsequent analyses involving daily opiate expenditure (Mn=$107.65±64.56, n=51), imputation with the mean was performed in cases where this information was missing in patient records. To verify that this procedure did not alter the findings of associations with cannabis use, analyses were repeated using the imputed form of daily opiate expenditure (Mn=$107.65±48.12, n=91). A recent history of cannabis use was again associated with decreased daily opiate expenditure [t(89)=2.368, p=0.020]. (Figure 1)
3.4. Effect of cannabis use history on methadone induction
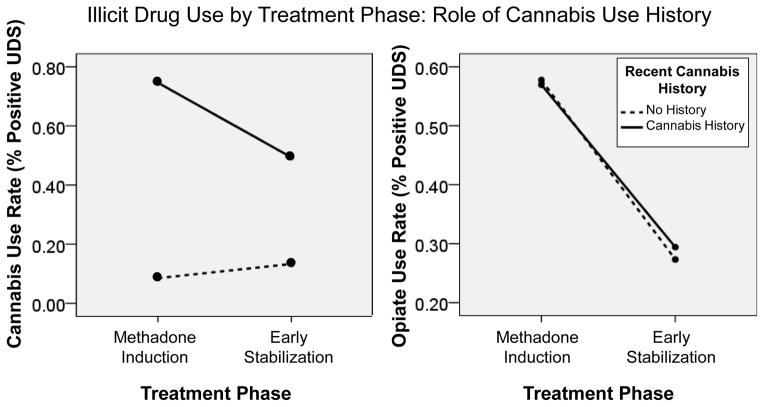
ANOVAs were next used to determine whether a history of cannabis use was associated with changes in rates of drug use during the methadone induction phase and early stabilization phase. Analyses first examined whether past cannabis use was associated with increased cannabis use during methadone induction or early stabilization. There was a significant interaction between treatment phase (methadone induction/early stabilization) and cannabis history on rates of cannabis use during treatment [F(1,80)=14.669, p<0.001]. Those with a history of recent cannabis use decreased from an average of 75±38% cannabis-positive UDS during methadone induction to 49±38% during early stabilization. However, individuals with no recent cannabis use history increase from an average of 9±23% cannabis-positive UDS during induction to 13±28% during early stabilization. A parallel ANCOVA controlling for daily opiate expenditure yielded similar results [F(1,79)=12.973, p=0.001]. (Figure 2)
Figure 2.
Analogous mixed-effects analyses crossing recent cannabis history and early MMT treatment phase (methadone induction/early stabilization) were then conducted employing opiate use as the outcome measure. Supportive of treatment efficacy, a main effect of treatment phase demonstrated that the rates of opiate use declined significantly between the induction and early stabilization phase [F(1,81)=141.338, p<0.001]. To control for severity of pre-treatment opiate abuse, a repeated-measures ANCOVA was performed using daily opiate expenditure as the covariate, and a similar pattern of findings was observed [F(1,80)=9.616, p=0.003]. Additionally, there was no significant interaction observed between treatment phase and cannabis history on in-treatment rates of opiate use [F(1,80)= 0.044, p = 0.835].
In addition to rates of illicit drug use, the analyses also sought to uncover any potential associations between recent cannabis history and several other measures of stabilization difficulty such as time required to complete methadone dose titration (methadone induction), methadone blocking dose upon stabilization, and medication compliance. Cannabis use prior to treatment was not associated with any changes in the time required to complete methadone induction [t(83)=0.875, p=0.384], or the eventual stabilization dose [t(82)=0.219, p=0.827]. Increases in the total daily medication absences over the initial nine months of the MMT program were also not associated with recent cannabis use [t(68)=0.982, p=0.330].
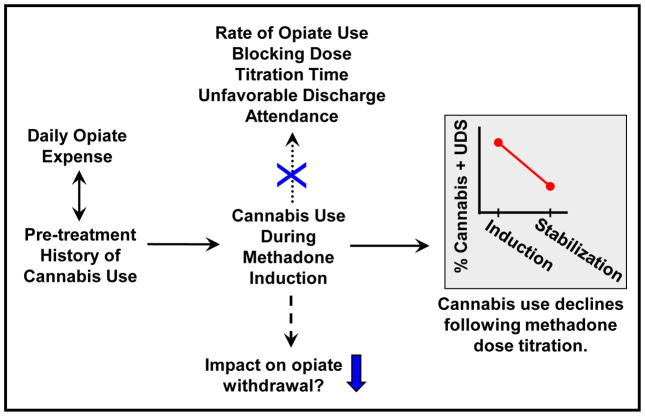
3.5. Effects of cannabis use during methadone induction
To address potential detrimental effects of cannabis on MMT stabilization, in-treatment cannabis use was examined in several ways to reveal any potential associations with illicit opiate use or measures of stabilization difficulty. Rates of cannabis-positive UDS and opiate-positive UDS did not correlate during either phase of treatment [methadone induction: r(82)=0.104, p=0.332; early stabilization: r(82)=0.038, p=0.734]. Dichotomized (yes/no) in-treatment cannabis use was not associated with change in opiate use during any treatment phase [F(1, 81)=0.999, p=0.321], and ANCOVA controlling for daily opiate expenditure yielded similar results [F(1,80)=0.087, p=0.769]. Cannabis use during methadone induction was not associated with any significant differences in time required for dose titration [t(80)=0.150, p=0.881], blocking dose [t(79)=0.847, p=0.399], or medication compliance [t(63)=1.212, p=0.230]. Furthermore, cannabis use did not significantly affect premature discharge status [X2(1)=3.009, p=0.222]. (Figure 3)
Figure 3.
3.5.1. Preliminary data on cannabis and opiate withdrawal severity
To examine whether cannabis intake during MMT treatment could be related to opiate withdrawal symptoms, associations between cannabis use and severity of opiate withdrawal were investigated using data from the Clinical Opiate Withdrawal Scale (COWS), an index designed to serve as an objective measure of opiate withdrawal 41. Effective in January of 2007, the COWS was added as an additional clinical assessment tool, administered in response to patients’ complaints of opiate withdrawal symptoms and craving. While induction COWS data were only available for a subset of the sample (n=40), when subjects were categorized as either low (n=29) or moderate withdrawal severity (n=11), a significant relationship with cannabis use was observed. Specifically, a 2x2 contingency table revealed that cannabis users preferentially fell into the low-severity withdrawal category while those that abstained from cannabis were more often in the moderate-level withdrawal category [X2(1)=7.54, p=0.006]. When further characterizing in-treatment cannabis users as abstinent, occasional or frequent use, 3x2 chi-square analysis demonstrated an inverse association between frequency of cannabis use and opiate withdrawal severity [X2(2)=6.71, p=0.035]. Further prospective studies are needed to assess this effect in a more controlled manner. (Figure 3)
4. Discussion
4.1. Association between cannabis and opiate use in treatment-seeking individuals
Cannabis-using opiate-dependent individuals presenting for MMT reported significantly less daily expenditure on acquisition of opiates. When considering this observation, note that the proxy measures of opiate addiction severity used in this study were selected based on available information in the patient record, and therefore lack the control of prospective assessment of addiction severity. Nonetheless, these findings highlighted a potentially interesting trend associated with concurrent cannabis and opiate use. A possible explanation for this finding may be that cannabis users in this study were less “severe” opiate addicts, or required lesser opiate intake. However, cannabis-using individuals did not differ from cannabis-abstinent individuals based on other proxy measures of severity of opiate dependence that included one’s cumulative years of opiate use and number of previous treatment episodes. Interaction between the molecular targets of opiates and cannabis in the brain may underlie the observation that those concurrently using both cannabis and opiates actually purchase and use less opiates37, 39, 40, 42, 43.
While cannabis users appeared to purchase (and presumably used) less opiates than cannabis-abstinent individuals at the time of program enrollment, rates of persistent illicit opiate use during MMT were not found to differ based on cannabis use. Data from this sample demonstrated no cannabis effects on dose titration, induction time, attendance, or unfavorable early discharge. These findings were in agreement with several previous studies concerning cannabis effects on MMT. In a large retrospective analysis of MMT, cannabis use was not associated with treatment retention, opiate/cocaine use, or any measure of treatment outcome 27. Similarly, no risk or harm to treatment outcome was associated with cannabis use in additional studies of patients on MMT 15, 44, 45 or buprenorphine 25. Intermittent cannabis users were found to have improved retention and outcomes in antagonist treatment for opiate dependence 16, 28. In a study examining post-discharge cannabis use following inpatient treatment, using cannabis was associated with relapse to alcohol and cocaine use, but not with relapse to heroin use 46.However, negative aspects of cannabis use on treatment for opiate dependence have also been reported. Several groups have demonstrated the association of cannabis use with likelihood of poly-drug use 24, 45 and increased risk for heroin relapse 47. Overall, studies of cannabis use on heroin intake in clinical populations did not support this trend16, 26–28, 48.
4.2. Decreased cannabis use upon completion of methadone induction
Interestingly, upon acquisition of a blocking dose of methadone, there was a concurrent decline in cannabis use in the sample as a whole. Although this could possibly have been a direct effect of methadone, methadone dose was not found to be related to cannabis use rates in our sample. In a study comparing detection of substance use over the first year of heroin-maintenance and MMT, similar but less dramatic decreases in cannabis use were observed among methadone-maintained patients. Both heroin and methadone-maintenance resulted in dramatic reduction of illicit opiate use despite common cannabis use 49. Although our group has demonstrated the decline in multiple types of illicit drug use with long-term MMT in the past 11–13, the present findings were to our knowledge the first to specifically examine patterns of cannabis use over time during the critical early stages of MMT.
4.2.1. Potential role for cannabis in reduction of opiate withdrawal
The transition from methadone induction to the early stabilization phase of treatment was expected to be accompanied by a decline in opiate craving and withdrawal 1, 9, 10. Decreases in the rate of cannabis-positive UDS were also observed during this transition, but it is unknown if this decline in cannabis use was related to diminished withdrawal symptoms, as clinical data regarding this phenomenon is limited. One group found that cannabis use was positively associated with lower plasma methadone concentrations, and while cannabis use could have caused metabolic changes that resulted in this finding, it is also possible that “cannabis use may be a compensatory response to opioid withdrawal symptoms in some individuals with more rapid methadone clearance” 50. In a study on the efficacy of non-opioid drugs for opiate withdrawal, cannabis was reported by patients to be less effective in reduction of symptoms than benzodiazepines, but more effective than cocaine, alcohol and nicotine 18. There was a positive correlation between rates of cannabis and benzodiazepine use (based on monthly UDS results) in our sample. Further studies will be required to determine how the effects of benzodiazepine may interact with those of cannabis during methadone induction. However, numerous studies of cannabinoid-opioid interactions in animal models of opiate addiction have provided strong evidence for an ameliorative effect of cannabinoids on opiate withdrawal symptoms 30, 34, 51–54.
The current study used objective measures (COWS and UDS) to examine this relationship in a pilot data set, where increased cannabis use was found to be associated with lower severity of withdrawal in a subset of the sample with available chart data. These results suggested a potential role for cannabis in the reduction of withdrawal severity during methadone induction, however prospective studies will be required to verify these initial findings.
4.3. Limitations and Prospective Studies
Due to the study design, the information gleaned from this retrospective chart analysis was descriptive in nature and interpretation of its findings must be cautiously considered. The challenges presented by the nature of the data included lessened control over inherent confounds in studies of drug use, and missing or limited chart information reduced the sample size for certain analyses. While UDS data provided an objective view of drug use during treatment, tests were required to be administered only once a month. Weekly quantitative drug screens detailing the specific amount of drug use would have been optimal and should be employed in prospective studies. Additionally, the study data on substance use history prior to treatment was limited to self-reported information present in the medical record. Optimally, more detailed objective analysis of pre-treatment substance use would be undertaken.
More extensive studies will be necessary to elucidate whether cannabis does indeed alleviate withdrawal signs during stabilization and whether it may be associated with treatment prognosis. Additionally, many individuals within this sample concurrently used cannabis and illicit benzodiazepines during MMT. Unfortunately, the nature of the data made it impossible to control for benzodiazepine use. Therefore, carefully-controlled studies will be essential to determine whether concurrent use of cannabis and benzodiazepines during methadone induction results in additive, subtractive, or synergistic decreases in opiate withdrawal signs. Additionally, further studies will be necessary to examine the specific patterns and effects of cannabis use in individuals on other types of therapeutic interventions for opiate dependence, such as antagonist or buprenorphine treatment.
Although the retrospective data presents limitations, this approach offered the opportunity to uncover patterns of cannabinoid-opiate associations in the existing data, so that this information may be used to guide the design of future prospective studies. Poly-drug abuse is extremely common among opiate-dependent individuals, and use of multiple substances often persists during substance abuse treatment. By maintaining a particular focus on the stabilization process during initiation of MMT, it was possible to examine whether cannabis use affected progress during initiation on to MMT, a critical time point in the treatment for opiate dependence.
Acknowledgments
The authors acknowledge the support of grants: DA02019 (Dr. Van Bockstaele) and DA023755 (Dr. Sterling) from the National Institutes of Health, Bethesda, MD.
The authors would like to thank the staff at the Narcotic Addiction Rehabilitation Program for their assistance with the data collection process.
Footnotes
Declaration of Interest:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
References
- 1.Dole VP, Nyswander M. A Medical Treatment for Diacetylmorphine (Heroin) Addiction. a Clinical Trial with Methadone Hydrochloride. Jama. 1965 Aug 23;193:646–650. doi: 10.1001/jama.1965.03090080008002. [DOI] [PubMed] [Google Scholar]
- 2.Nichols AW, Salwen MB, Torrens PR. Outpatient induction to methadone maintenance treatment for heroin addiction. Arch Intern Med. 1971 May;127(5):903–909. [PubMed] [Google Scholar]
- 3.Leavitt SB. Methadone Dosing & Safety in the Treatment of Opiate Addiction. Addiction Treatment Forum. 2003 [Google Scholar]
- 4.Nicholls L, Bragaw L, Ruetsch C. Opioid dependence treatment and guidelines. J Manag Care Pharm. 2010 Feb;16(1 Suppl B):S14–21. doi: 10.18553/jmcp.2010.16.S1-B.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bell J, Zador D. A risk-benefit analysis of methadone maintenance treatment. Drug Saf. 2000 Mar;22(3):179–190. doi: 10.2165/00002018-200022030-00002. [DOI] [PubMed] [Google Scholar]
- 6.Langrod J, Lowinson J, Ruiz P. Methadone treatment and physical complaints: a clinical analysis. Int J Addict. 1981 Jul;16(5):947–952. doi: 10.3109/10826088109038903. [DOI] [PubMed] [Google Scholar]
- 7.Dyer KR, White JM. Patterns of symptom complaints in methadone maintenance patients. Addiction. 1997 Nov;92(11):1445–1455. [PubMed] [Google Scholar]
- 8.Elkader AK, Brands B, Callaghan R, Sproule BA. Exploring the relationship between perceived inter-dose opioid withdrawal and patient characteristics in methadone maintenance treatment. Drug Alcohol Depend. 2009 Dec 1;105(3):209–214. doi: 10.1016/j.drugalcdep.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Belding MA, Iguchi MY, Lamb RJ, Lakin M, Terry R. Coping strategies and continued drug use among methadone maintenance patients. Addict Behav. 1996 May-Jun;21(3):389–401. doi: 10.1016/0306-4603(95)00069-0. [DOI] [PubMed] [Google Scholar]
- 10.Barta WD, Kurth ME, Stein MD, Tennen H, Kiene SM. Craving and self-efficacy in the first five weeks of methadone maintenance therapy: a daily process study. J Stud Alcohol Drugs. 2009 Sep;70(5):735–740. doi: 10.15288/jsad.2009.70.735. [DOI] [PubMed] [Google Scholar]
- 11.Gottheil E, Sterling RC, Weinstein SP. Diminished illicit drug use as a consequence of long-term methadone maintenance. J Addict Dis. 1993;12(4):45–57. doi: 10.1300/J069v12n04_04. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein SP, Gottheil E, Sterling RC, DeMaria PA., Jr Long-term methadone maintenance treatment: some clinical examples. J Subst Abuse Treat. 1993 May-Jun;10(3):277–281. doi: 10.1016/0740-5472(93)90075-d. [DOI] [PubMed] [Google Scholar]
- 13.DeMaria PA, Jr, Sterling R, Weinstein SP. The effect of stimulant and sedative use on treatment outcome of patients admitted to methadone maintenance treatment. Am J Addict. 2000 Spring;9(2):145–153. doi: 10.1080/10550490050173217. [DOI] [PubMed] [Google Scholar]
- 14.Nurco DN, Kinlock TW, Hanlon TE, Ball JC. Nonnarcotic drug use over an addiction career--a study of heroin addicts in Baltimore and New York City. Compr Psychiatry. 1988 Sep-Oct;29(5):450–459. doi: 10.1016/0010-440x(88)90060-0. [DOI] [PubMed] [Google Scholar]
- 15.Nirenberg TD, Liepman MR, Cellucci T, Swift RM, Sirota AD. Cannabis versus other illicit drug use among methadone maintenance patients. Psychology of Addictive Behaviors. 1996;10:222–227. [Google Scholar]
- 16.Church SH, Rothenberg JL, Sullivan MA, Bornstein G, Nunes EV. Concurrent substance use and outcome in combined behavioral and naltrexone therapy for opiate dependence. Am J Drug Alcohol Abuse. 2001 Aug;27(3):441–452. doi: 10.1081/ada-100104511. [DOI] [PubMed] [Google Scholar]
- 17.San L, Torrens M, Castillo C, Porta M, de la Torre R. Consumption of buprenorphine and other drugs among heroin addicts under ambulatory treatment: results from cross-sectional studies in 1988 and 1990. Addiction. 1993 Oct;88(10):1341–1349. doi: 10.1111/j.1360-0443.1993.tb02020.x. [DOI] [PubMed] [Google Scholar]
- 18.Hermann D, Klages E, Welzel H, Mann K, Croissant B. Low efficacy of non-opioid drugs in opioid withdrawal symptoms. Addict Biol. 2005 Jun;10(2):165–169. doi: 10.1080/13556210500123514. [DOI] [PubMed] [Google Scholar]
- 19.Degenhardt L, Hall W, Lynskey M. The relationship between cannabis use and other substance use in the general population. Drug Alcohol Depend. 2001 Nov 1;64(3):319–327. doi: 10.1016/s0376-8716(01)00130-2. [DOI] [PubMed] [Google Scholar]
- 20.Frauger E, Vigneau C, Orleans V, et al. Consumption of cannabis among subjects with history of abuse/dependence or under an opiate maintenance therapy: OPPIDUM data in 2006 and main trends since 2004. Therapie. 2008 Mar-Apr;63(2):119–127. doi: 10.2515/therapie:2008037. [DOI] [PubMed] [Google Scholar]
- 21.Maremmani I, Stefania C, Pacini M, et al. Differential substance abuse patterns distribute according to gender in heroin addicts. J Psychoactive Drugs. 2010 Mar;42(1):89–95. doi: 10.1080/02791072.2010.10399789. [DOI] [PubMed] [Google Scholar]
- 22.Saxon AJ, Calsyn DA, Blaes PA, Haver VM, Greenberg DM. Marijuana use by methadone maintenance patients. NIDA Res Monogr. 1990;105:306–307. [PubMed] [Google Scholar]
- 23.Ellner M. Marijuana use by heroin abusers as a factor in program retention. J Consult Clin Psychol. 1977 Aug;45(4):709–710. doi: 10.1037//0022-006x.45.4.709. [DOI] [PubMed] [Google Scholar]
- 24.DuPont RL, Saylor KE. Marijuana and benzodiazepines in patients receiving methadone treatment. Jama. 1989 Jun 16;261(23):3409. [PubMed] [Google Scholar]
- 25.Budney AJ, Bickel WK, Amass L. Marijuana use and treatment outcome among opioid-dependent patients. Addiction. 1998 Apr;93(4):493–503. doi: 10.1046/j.1360-0443.1998.9344935.x. [DOI] [PubMed] [Google Scholar]
- 26.Nixon LN. Cannabis use and treatment outcome in methadone maintenance. Addiction. 2003 Sep;98(9):1321–1322. doi: 10.1046/j.1360-0443.2003.00532.x. author reply 1322–1323. [DOI] [PubMed] [Google Scholar]
- 27.Epstein DH, Preston KL. Does cannabis use predict poor outcome for heroin-dependent patients on maintenance treatment? Past findings and more evidence against. Addiction. 2003 Mar;98(3):269–279. doi: 10.1046/j.1360-0443.2003.00310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raby WN, Carpenter KM, Rothenberg J, et al. Intermittent marijuana use is associated with improved retention in naltrexone treatment for opiate-dependence. Am J Addict. 2009 Jul-Aug;18(4):301–308. doi: 10.1080/10550490902927785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Vries TJ, Homberg JR, Binnekade R, Raaso H, Schoffelmeer AN. Cannabinoid modulation of the reinforcing and motivational properties of heroin and heroin-associated cues in rats. Psychopharmacology (Berl) 2003 Jul;168(1–2):164–169. doi: 10.1007/s00213-003-1422-1. [DOI] [PubMed] [Google Scholar]
- 30.Lichtman AH, Sheikh SM, Loh HH, Martin BR. Opioid and cannabinoid modulation of precipitated withdrawal in delta(9)-tetrahydrocannabinol and morphine-dependent mice. J Pharmacol Exp Ther. 2001 Sep;298(3):1007–1014. [PubMed] [Google Scholar]
- 31.Navarro M, Carrera MR, Fratta W, et al. Functional interaction between opioid and cannabinoid receptors in drug self-administration. J Neurosci. 2001 Jul 15;21(14):5344–5350. doi: 10.1523/JNEUROSCI.21-14-05344.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cichewicz DL. Synergistic interactions between cannabinoid and opioid analgesics. Life Sci. 2004 Jan 30;74(11):1317–1324. doi: 10.1016/j.lfs.2003.09.038. [DOI] [PubMed] [Google Scholar]
- 33.Manzanares J, Corchero J, Romero J, Fernandez-Ruiz JJ, Ramos JA, Fuentes JA. Pharmacological and biochemical interactions between opioids and cannabinoids. Trends Pharmacol Sci. 1999 Jul;20(7):287–294. doi: 10.1016/s0165-6147(99)01339-5. [DOI] [PubMed] [Google Scholar]
- 34.Valverde O, Noble F, Beslot F, Dauge V, Fournie-Zaluski MC, Roques BP. Delta9-tetrahydrocannabinol releases and facilitates the effects of endogenous enkephalins: reduction in morphine withdrawal syndrome without change in rewarding effect. Eur J Neurosci. 2001 May;13(9):1816–1824. doi: 10.1046/j.0953-816x.2001.01558.x. [DOI] [PubMed] [Google Scholar]
- 35.Fattore L, Vigano D, Fadda P, Rubino T, Fratta W, Parolaro D. Bidirectional regulation of mu-opioid and CB1-cannabinoid receptor in rats self-administering heroin or WIN 55,212-2. Eur J Neurosci. 2007 Apr;25(7):2191–2200. doi: 10.1111/j.1460-9568.2007.05470.x. [DOI] [PubMed] [Google Scholar]
- 36.Fattore L, Spano S, Cossu G, Deiana S, Fadda P, Fratta W. Cannabinoid CB(1) antagonist SR 141716A attenuates reinstatement of heroin self-administration in heroin-abstinent rats. Neuropharmacology. 2005 Jun;48(8):1097–1104. doi: 10.1016/j.neuropharm.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 37.Tham SM, Angus JA, Tudor EM, Wright CE. Synergistic and additive interactions of the cannabinoid agonist CP55,940 with mu opioid receptor and alpha2-adrenoceptor agonists in acute pain models in mice. Br J Pharmacol. 2005 Mar;144(6):875–884. doi: 10.1038/sj.bjp.0706045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cox ML, Haller VL, Welch SP. Synergy between delta9-tetrahydrocannabinol and morphine in the arthritic rat. Eur J Pharmacol. 2007 Jul 12;567(1–2):125–130. doi: 10.1016/j.ejphar.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 39.Roberts JD, Gennings C, Shih M. Synergistic affective analgesic interaction between delta-9-tetrahydrocannabinol and morphine. Eur J Pharmacol. 2006 Jan 13;530(1–2):54–58. doi: 10.1016/j.ejphar.2005.11.036. [DOI] [PubMed] [Google Scholar]
- 40.Cichewicz DL, McCarthy EA. Antinociceptive synergy between delta(9)-tetrahydrocannabinol and opioids after oral administration. J Pharmacol Exp Ther. 2003 Mar;304(3):1010–1015. doi: 10.1124/jpet.102.045575. [DOI] [PubMed] [Google Scholar]
- 41.Wesson DR, Ling W. The Clinical Opiate Withdrawal Scale (COWS) J Psychoactive Drugs. 2003 Apr-Jun;35(2):253–259. doi: 10.1080/02791072.2003.10400007. [DOI] [PubMed] [Google Scholar]
- 42.Parolaro D, Rubino T, Vigano D, Massi P, Guidali C, Realini N. Cellular mechanisms underlying the interaction between cannabinoid and opioid system. Curr Drug Targets. 2010;11(4):393–405. doi: 10.2174/138945010790980367. [DOI] [PubMed] [Google Scholar]
- 43.Vigano D, Rubino T, Parolaro D. Molecular and cellular basis of cannabinoid and opioid interactions. Pharmacol Biochem Behav. 2005 Jun;81(2):360–368. doi: 10.1016/j.pbb.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 44.Saxon AJ, Calsyn DA, Greenberg D, Blaes P, Haver VM, Stanton V. Urine screening for marijuana among methadone-maintained patients. American Journal on Addictions. 1993;2:207–211. [Google Scholar]
- 45.Weizman T, Gelkopf M, Melamed Y, Adelson M, Bleich A. Cannabis abuse is not a risk factor for treatment outcome in methadone maintenance treatment: a 1-year prospective study in an Israeli clinic. Aust N Z J Psychiatry. 2004 Jan-Feb;38(1–2):42–46. doi: 10.1046/j.1440-1614.2003.01296.x. [DOI] [PubMed] [Google Scholar]
- 46.Aharonovich E, Liu X, Samet S, Nunes E, Waxman R, Hasin D. Postdischarge cannabis use and its relationship to cocaine, alcohol, and heroin use: a prospective study. Am J Psychiatry. 2005 Aug;162(8):1507–1514. doi: 10.1176/appi.ajp.162.8.1507. [DOI] [PubMed] [Google Scholar]
- 47.Wasserman DA, Weinstein MG, Havassy BE, Hall SM. Factors associated with lapses to heroin use during methadone maintenance. Drug Alcohol Depend. 1998 Nov 1;52(3):183–192. doi: 10.1016/s0376-8716(98)00092-1. [DOI] [PubMed] [Google Scholar]
- 48.Nava F, Manzato E, Lucchini A. Chronic cannabis use does not affect the normalization of hypothalamic-pituitary-adrenal (HPA) axis induced by methadone in heroin addicts. Prog Neuropsychopharmacol Biol Psychiatry. 2007 Jun 30;31(5):1089–1094. doi: 10.1016/j.pnpbp.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 49.Musshoff F, Trafkowski J, Lichtermann D, Madea B. Comparison of urine results concerning co-consumption of illicit heroin and other drugs in heroin and methadone maintenance programs. Int J Legal Med. 2009 Aug 12; doi: 10.1007/s00414-009-0361-8. [DOI] [PubMed] [Google Scholar]
- 50.Hallinan R, Crettol S, Agho K, et al. Cannabis and benzodiazepines as determinants of methadone trough plasma concentration variability in maintenance treatment: a transnational study. Eur J Clin Pharmacol. 2009 Nov;65(11):1113–1120. doi: 10.1007/s00228-009-0706-8. [DOI] [PubMed] [Google Scholar]
- 51.Frederickson RC, Hewes CR, Aiken JW. Correlation between the in vivo and an in vitro expression of opiate withdrawal precipitated by naloxone: their antagonism by l-(-)-delta9-tetrahydrocannabinol. J Pharmacol Exp Ther. 1976 Nov;199(2):375–384. [PubMed] [Google Scholar]
- 52.Yamaguchi T, Hagiwara Y, Tanaka H, et al. Endogenous cannabinoid, 2-arachidonoylglycerol, attenuates naloxone-precipitated withdrawal signs in morphine-dependent mice. Brain Res. 2001 Aug 3;909(1–2):121–126. doi: 10.1016/s0006-8993(01)02655-5. [DOI] [PubMed] [Google Scholar]
- 53.Cichewicz DL, Welch SP. Modulation of oral morphine antinociceptive tolerance and naloxone-precipitated withdrawal signs by oral Delta 9-tetrahydrocannabinol. J Pharmacol Exp Ther. 2003 Jun;305(3):812–817. doi: 10.1124/jpet.102.046870. [DOI] [PubMed] [Google Scholar]
- 54.Vela G, Ruiz-Gayo M, Fuentes JA. Anandamide decreases naloxone-precipitated withdrawal signs in mice chronically treated with morphine. Neuropharmacology. 1995 Jun;34(6):665–668. doi: 10.1016/0028-3908(95)00032-2. [DOI] [PubMed] [Google Scholar]