Abstract
Background.
Qualifying the relationship between multi-morbidity, health-related quality of life (HRQOL) and depressive symptoms in primary care can help to inform the development of appropriate interventions and services which can help to enhance HRQOL in patients with chronic disease.
Objective.
The objective of this study was to determine whether the physical aspect of HRQOL mediates the relationship between chronic disease multi-morbidity and depressive symptoms in Chinese primary care patients.
Methods.
A cross-sectional survey was conducted on patients recruited from the waiting rooms of 59 primary care clinics distributed across Hong Kong. About 9259 subjects were included for the mediation model analysis. The primary outcome was level of depressive symptoms as measured by the Patient Health Questionniare 9. The mediation model was tested using a bootstrapping method.
Results.
The prevalence of chronic disease was 50.4%, with 25.4% having two or more co-morbidities. The relationship between multi-morbidity and depressive symptoms was found to be mediated by the Physical Component Summary score of the SF-12 v2. Further analysis found the general health (GH) and role physical domains of the SF-12 were the strongest mediators, followed by bodily pain and physical functioning (PF).
Conclusion.
To enhance the functional capacity of primary care patients with co-existing chronic disease and depressive symptoms, health care interventions should be directed at improving the physical aspects of HRQOL, in particular enhancing patients’ GH perception, role functioning and PF, and to better manage chronic pain.
Key words: Chinese, depression, family practice, morbidity, primary health care, quality of life.
Introduction
Co-morbidity of chronic disease and depression is very common (1). The association between physical health and emotional symptoms is thought to be related to the loss in the functional capacity to conduct routine daily activities (2–4). It has been postulated that physical illness affects mental health via biological mechanisms (e.g. hormonal change and side effects of treatments), behavioural pathways (e.g. disruption of daily routines and sick role behaviours), cognitive effects (e.g. perceived stress and locus of control) and social interference (e.g. impediment of usual role functioning or deterioration of social networks) (5).
The medical management of multi-morbidity is challenging because patients with chronic disease often require complicated treatments (4) and have poor health outcomes. Multi-morbidity can also impact health-related quality of life (HRQOL) (6). Previous studies have found that people with more chronic physical disease are at a higher risk of having major depression (3). With population ageing, it is expected that as the prevalence of chronic disease increases, there will be a concomitant increase in the prevalence of depression (7).
A study conducted in Australia by Gunn et al. (8) found a dose–response relationship between the number of chronic physical problems and severity of depressive symptoms, and that the relationship was potentially mediated by two aspects of HRQOL (functional limitation and self-rated health). In that study, a regression analysis was used to explore the relationship which is not robust enough to confirm if a mediation model exists. Also, only two questions were used to measure physical HRQOL which may oversimplify the construct. The study was conducted in a western setting and the findings may not be transferable to Asian settings where health beliefs and health systems are different.
In recent decades, there has been a shift in chronic disease management away from specialist settings to primary care. Primary care clinicians are trained to use a patient-centred, holistic management approach are well placed to coordinate the multi-disciplinary care often required by patients with chronic disease (9). A better understanding of the relationship between multi-morbidity, HRQOL and depressive symptoms can help primary care doctors to better manage patients with chronic disease by informing the development of interventions that can address their multi-dimensional needs. The aim of this study was to determine whether the physical aspects of HRQOL mediated the relationship between multi-morbidity and depressive in a Chinese primary care patient population.
Methods
To further and strengthen the findings by Gunn et al. (10), we chose a bootstrapping method approach to explore the relationship between multi-morbidity, HRQOL and depressive symptoms, using a well-validated HRQOL measure to assess the physical aspects of HRQOL.
Design
This study was conducted as part of an observational study examining the epidemiology of depressive disorders in Hong Kong’s primary care (11,12). Data obtained from a cross-sectional survey was analysed to explore the association between multi-morbidity, HRQOL and depressive symptoms.
Subjects and sampling
Doctors working in primary care clinics located across Hong Kong were identified from the 1500-member mailing list of the Hong Kong College of Family Physicians and invited to join our practice-based research network. A total of 59 doctors voluntarily joined the study: 11 from public-sector clinics and 48 from private practice settings, aligning proportionately with the delivery of primary care services in Hong Kong. All eligible patients presenting to the study doctor on one randomly selected day each month over 1 year were consecutively recruited to join the study. Patients were approached in the doctor’s waiting room by field workers and excluded if they were (1) aged < 18 years (2), could not understand English, Cantonese or Mandarin (3), had cognitive or communication difficulties (4), had already been recruited to the study and (5) did not consult the study doctor. A 12-month collection period was used to account for seasonal variability and to improve the representation of the primary care case load. Data collection occurred between October 2010 and January 2012.
Study instruments
Subjects completed a waiting-room questionnaire containing items on socio-demographics, a checklist of chronic health conditions, the Patient Health Questionnaire 9 (PHQ-9), and the Short Form-12 Health Survey version 2 (SF-12 v2).
Multi-morbidity
To assess the prevalence of chronic disease, subjects were asked if they had ever been diagnosed by a doctor to have hypertension, diabetes mellitus, heart disease, stroke, chronic respiratory disease (such as asthma, chronic bronchitis and emphysema), arthritis or other chronic rheumatism, chronic pain and other major diseases. This list was adapted from previously performed primary care patient studies (13) and included the most common chronic conditions encountered in Hong Kong’s primary care (14). The number of chronic diseases was calculated by counting the number of conditions selected.
PHQ-9
The PHQ-9 is a 10-item self-report depression scale which scores each of the nine Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria for a diagnosis of major depression episode plus an extra item on functional difficulties as a result of the depressive symptoms. The total score ranged from 0 to 27, with higher score indicating more severe symptoms. It has been validated on primary care patients in Hong Kong. Using a cut-off score of >9, the PHQ-9 has been found to have a sensitivity of 80% and specificity of 92% for diagnosing depressive disorders against the Chinese Hamilton Depression Scale (15).
The Chinese (HK) SF-12 health survey version 2 (SF-12 v2)
The SF-12 v2 is a generic HRQOL measure, which covers eight domains namely physical functioning (PF), role limitation due to physical problems (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role limitation due to emotional problems (RE) and mental health (MH). The domain scores are calculated by summation of the relevant item scores and transformation into a range from 0 to 100. The SF-12 v2 can be summarized into physical and mental component summary (PCS and MCS) scores with higher scores indicating better HRQOL. Its psychometric properties have been evaluated on a sampled of 2410 Chinese adults randomly selected from the general population of Hong Kong and found to be a valid and equivalent substitute for the SF-36 version 2 Health Survey for the Chinese (16).
Statistical analysis
We used mediation analysis, applying the bootstrapping method to explore the relationship between multi-morbidity, depressive symptoms and HRQOL (10). This approach is considered to be more powerful than the Baron and Kenney’s multistage regression approach and the Sobel test for estimating mediation and indirect effects (17). Point estimates were based on 5000 bootstrapping samples and 95% confidence intervals (CI) were generated. An indirect effect (multi-morbidity affects the physical aspects of HRQOL, which in turn affects depressive symptoms) was considered significant if the CI did not contain zero.
The SF-12 v2 PCS was first used as the mediator. To further explore the impact of HRQOL on the relationship between multi-morbidity and depressive symptoms, the PF, RP, BP and GH domains were simultaneously used in the mediation analysis to allow comparison of the strength of the mediation effects (contrast) of each domain. As there were four mediators, there were six possible pairwise contrasts.
In order to overcome the potential effect of confounders, socio-demographic factors including age, gender, educational attainment, marital status and employment status were adjusted for in the analyses. Listwise deletion was used to handle the missing data.
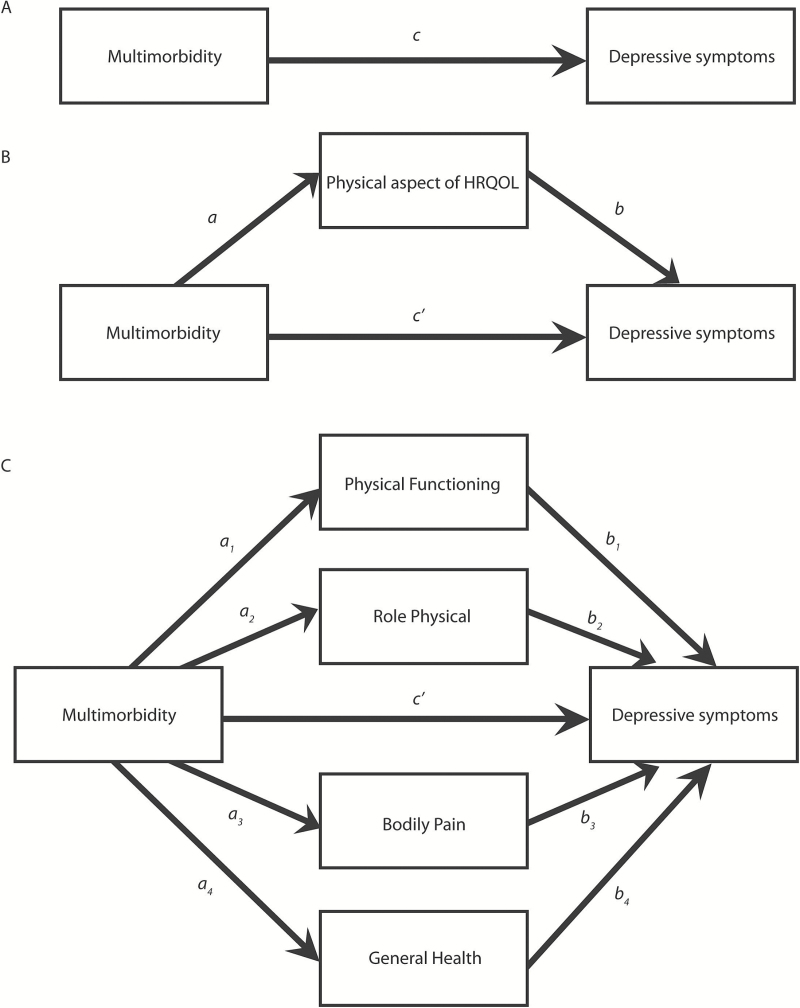
The proposed mediation models are shown in Figure 1. Figure 1A shows the effect of multi-morbidity on depressive symptoms, without considering any mediators. In Figure 1B, a is the coefficient for multi-morbidity in a model predicting the physical component of HRQOL from multi-morbidity, and b and c′ are the coefficients in a model predicting depressive symptoms from the physical component of HRQOL and multi-morbidity. c′ quantifies the direct effect of multi-morbidity on depressive symptoms, whereas the product of a and b (point estimate) quantifies the indirect effect of multi-morbidity on depressive symptoms through the physical component of HRQOL. In other words, c = c′ + ab. The indirect effect, ab, is the difference between the total and direct effect of multi-morbidity: ab = c – c′. The product ab can be clinically interpreted as the amount by which depressive symptoms are expected to change indirectly through HRQOL per a unit change in multi-morbidity. Figure 1C shows the proposed mediation model with multiple mediators. The specific indirect effect of multi-morbidity on depressive symptoms through one of the mediators is quantified as a n b n (point estimate). The total indirect effect of multi-morbidity on depressive symptoms is the sum of the specific indirect effects (a 1 b 1 + a 2 b 2 + a 3 b 3 + a 4 b 4). The total effect can be expressed as c = c′ + a 1 b 1 + a 2 b 2 + a 3 b 3 + a 4 b 4.
Figure 1.
The proposed mediation models
The ratio of the indirect effect to the total effect was used to quantify the effect size of the mediation model (P M). The proportion mediated is a frequently used effect-size measure. This measure indicated what proportion of the total effect is mediated by the intervening variable. The proportion mediated also assessed the relative contribution of single mediators in multiple mediator models by indicating what proportion of the total effect is attributable to individual mediational pathways.
All significance tests were two-tailed with P < 0.05 considered statistically significant. All statistical analysis were performed using STATA Version 13.0.
Results
Sample characteristics
A total of 10 179 subjects completed the survey at baseline (response rate of 81.0%). About 920 subjects had missing data in multi-morbidity, SF-12 v2 or PHQ-9. As a result, the data of 9259 subjects were included for unadjusted analysis. Of these, 9028 subjects who had the entire socio-demographic record were included for the adjusted analysis. Table 1 shows the socio-demographics, PHQ-9 and SF-12 v2 scores, and the prevalence of chronic disease by condition and number of co-morbidities. The prevalence of chronic disease was 50.4% of subjects with 25.4% having two or more chronic physical conditions. The most commonly reported chronic physical conditions were hypertension (28.0%), arthritis or other chronic rheumatism (16.2%), chronic pain (12.6%) and diabetes mellitus (10.4%).
Table 1.
Baseline subject characteristics and prevalence of multi-morbidity (n = 9259)
| Demographic characteristics | Prevalence of chronic physical illness by type and number of conditions (n, %) | ||||
|---|---|---|---|---|---|
| Age (median, IQR) | 48 | 29 | |||
| Gender (n, %) | Hypertension | 2589 | 28.0 | ||
| Male | 3898 | 42.1 | Diabetes mellitus | 963 | 10.4 |
| Female | 5352 | 57.8 | Heart disease | 487 | 5.3 |
| Missing | 9 | 0.1 | Stroke | 143 | 1.5 |
| Educational attainment (n, %) | Chronic respiratory disease | 706 | 7.6 | ||
| No formal school | 715 | 7.7 | Arthritis or other chronic rheumatism | 1502 | 16.2 |
| Primary | 1507 | 16.3 | Chronic pain | 1168 | 12.6 |
| Secondary (including matriculation) | 3816 | 41.2 | Other major diseases | 943 | 10.2 |
| Tertiary | 3151 | 34.0 | |||
| Missing | 70 | 0.8 | |||
| Marital status (n, %) | Median number of multi-morbidities (IQR) | 1 | 2 | ||
| Single | 2531 | 27.3 | Prevalence of multi-morbidity (n, %) | ||
| Married | 5633 | 60.8 | No condition | 4592 | 49.6 |
| Widow(er) | 726 | 7.8 | One condition | 2317 | 25.0 |
| Separated or divorced | 295 | 3.2 | Two conditions | 1363 | 14.7 |
| Missing | 74 | 0.8 | Three conditions | 622 | 6.7 |
| Employment status (n, %) | Four conditions | 260 | 2.8 | ||
| Working | 5698 | 61.5 | Five conditions | 82 | 0.9 |
| Not working | 3498 | 37.8 | Six conditions | 20 | 0.2 |
| Missing | 63 | 0.7 | Seven conditions | 2 | 0.022 |
| Eight conditions | 1 | 0.011 | |||
| Depressive symptoms and HRQOL | Median | IQR | |||
| PHQ-9 total score | 3 | 5 | |||
| SF-12 v2 | |||||
| Physical functioning | 100 | 25 | |||
| Role physical | 87.5 | 25 | |||
| Bodily pain | 75 | 50 | |||
| General health | 25 | 35 | |||
| Vitality | 75 | 25 | |||
| Social functioning | 100 | 25 | |||
| Role emotional | 87.5 | 25 | |||
| Mental health | 75 | 25 | |||
| Physical component summary | 49.9 | 10.6 | |||
| Mental component summary | 54.9 | 10.8 | |||
HRQOL, health-related quality of life; IQR, interquartile range; SD, standard deviation.
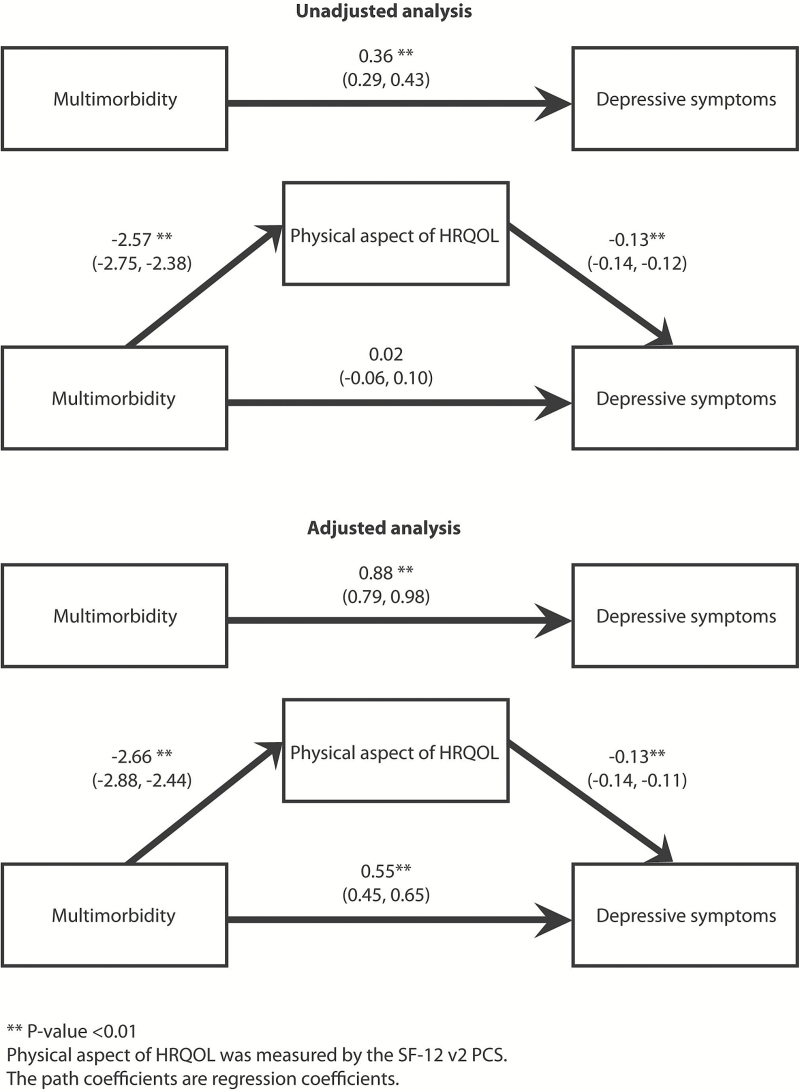
The effect of HRQOL as measured by the SF-12 v2 PCS, controlling for sociodemographics
After controlling for the SF-12 v2 PCS score, the direct effect of multi-morbidity on depressive symptoms remained statistically significant (P < 0.01) (Figure 2). The bootstrapping method showed that the 95% CI (corrected for bias) did not contain zero (point estimate: 0.3365; 95% CI: 0.2962–0.3806) (Table 2), supporting a partial mediation model. Multi-morbidity was associated with depressive symptoms both directly as well as through the physical components of HRQOL. Clinically, subjects with one unit change in multi-morbidity would have 0.34-point change in depressive symptoms through the physical component of HRQOL (indirect effect), and 0.55-point change in depressive symptoms directly (direct effect). In other words, PHQ-9 score is expected to increase by 0.89-point (0.34-point through physical component of HRQOL and 0.55-point by direct effect) for every one-unit increase in multi-morbidity. The effect size was 0.38 suggesting that the indirect effect accounted for 38% of the total effect.
Figure 2.
Models showing the effect of multimorbidity on depressive symptoms as mediated by the SF-12 v2
Table 2.
The mediation effect (indirect effects) of HRQOL on the relationship between multi-morbidity and depressive symptoms by the bootstrapping method
| The unadjusted mediation effect | |||
|---|---|---|---|
| Bias corrected 95% CIa | |||
| Point estimate | Lower | Upper | |
| The SF-12 v2 | |||
| PCS | 0.3404 | 0.3030 | 0.3819 |
| PF | 0.0241 | −0.0009 | 0.0499 |
| RP | 0.0601 | 0.0327 | 0.0871 |
| BP | 0.0955 | 0.0775 | 0.1168 |
| GH | 0.2322 | 0.2084 | 0.2564 |
| Comparing the strength of the mediators (indirect effects) | |||
| Bias corrected 95% CIb | |||
| Point estimate | Lower | Upper | |
| PF versus RP | −0.0360 | −0.0753 | 0.0018 |
| PF versus BP | −0.0714 | −0.1059 | −0.0388 |
| PF versus GH | −0.2081 | −0.2426 | −0.1708 |
| RP versus BP | −0.0354 | −0.0621 | −0.0075 |
| RP versus GH | −0.1721 | −0.2042 | −0.1385 |
| BP versus GH | −0.1366 | −0.1671 | −0.1061 |
| The adjusted mediation effectc | |||
| Bias corrected 95% CIa | |||
| Point estimate | Lower | Upper | |
| The SF-12 v2 | |||
| PCS | 0.3365 | 0.2962 | 0.3806 |
| PF | 0.0425 | 0.0203 | 0.0667 |
| RP | 0.2109 | 0.1781 | 0.2474 |
| BP | 0.1663 | 0.1372 | 0.1967 |
| GH | 0.2458 | 0.2201 | 0.2732 |
| Comparing the strength of the mediators (indirect effects) | |||
| Bias corrected 95% CIb | |||
| Point estimate | Lower | Upper | |
| PF versus RP | −0.1684 | −0.2133 | −0.1269 |
| PF versus BP | −0.1238 | −0.1634 | −0.0845 |
| PF versus GH | −0.2033 | −0.2380 | −0.1676 |
| RP versus BP | 0.0446 | 0.0009 | 0.0909 |
| RP versus GH | −0.0349 | −0.0738 | 0.0076 |
| BP versus GH | −0.1684 | −0.2133 | −0.1269 |
BP, bodily pain; GH, general health; PCS, physical component summary; PF, physical functioning; RP, role physical; SE, standard error.
aIf the 95% confidence interval (CI) does not contain zero, the mediation (indirect effect) is significant.
bIf the 95% confidence interval (CI) does not contain zero, the contrast is significant.
cControlling for age, gender, educational attainment, marital status and employment status.
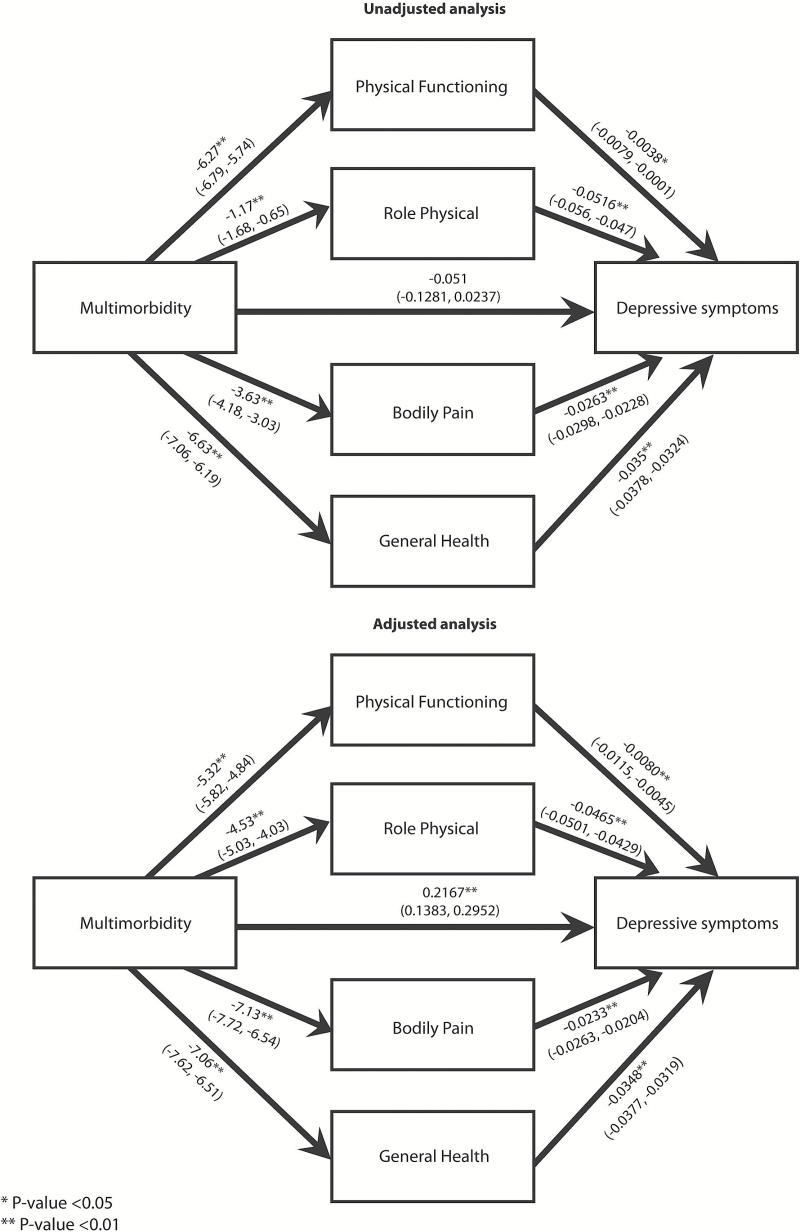
The effects of HRQOL as measured by the SF-12 v2 PF, RP, BP and GH controlling for socio-demographics
After simultaneously controlling for the SF-12 v2 PF, RP, BP and GH, the direct effect of multi-morbidity on depressive symptoms remained statistically significant (P < 0.01) (Figure 3). The bootstrapping method showed that the 95% CI (corrected for bias) did not contain zero, indicating that the indirect effect of multi-morbidity on depressive symptoms through the SF-12 v2 PF(point estimate: 0.0425; 95% CI: 0.0203–0.0667; effect size: 0.16), RP(point estimate: 0.2109; 95% CI: 0.1781–0.2474; effect size: 0.49), BP (point estimate: 0.1663; 95% CI: 0.1372–0.1967; effect size: 0.43) and GH (point estimate: 0.2458; 95% CI: 0.2201–0.2732; effect size: 0.53) were all valid whilst adjusting for the other domains (Table 2), supporting a partial mediation model. After simultaneously controlling for the socio-demographic and other mediators, subjects with one unit change in multi-morbidity would have 0.0425-point change in depressive symptoms through the PF (16% of the total effect), 0.2109-point change through role physical (49% of the total effect), 0.1663 through BP (43% of the total effect) or 0.2458 though GH (43% of the total effect),.
Figure 3.
Models showing the effect of multimorbidity on depressive symptoms as mediated simultaneously by the PF, RP, BP and GH domains
When the strengths of different mediators were compared, no difference was found between the SF-12 v2 GH and RP (as the 95% CI contained zero). The mediation effects of SF-12 v2 GH and RP were stronger than SF-12v2 BP whilst the effect of the SF-12v2 PF was the weakest (Table 2).
Discussion
Summary and main findings
We found that the association between multi-morbidity and depressive symptoms was partially mediated by the physical aspects of HRQOL, suggesting that multi-morbidity is associated with depressive symptoms both directly as well as through the physical aspects of HRQOL. GH perception and role limitation due to physical problems were the strongest mediators, suggesting that patient’s perception of their GH and the amount of limitation to their role functioning had a greater impact on the relationship between multi-morbidity and depressive symptoms than other aspects of HRQOL. Our findings were supported by the theoretical framework that physical illness affects depressive symptoms via behavioural and social pathways. Given that HRQOL appears to mediate the relationship between multi-morbidity and depressive symptoms, for patients with co-morbid depressive and chronic physical illness, interventions should be directed at improving the physical aspect of HRQOL, GH perception, role functioning and PF and to alleviate BP to help reduce the impact of the physical co-morbidities on MH.
Discussion of findings and existing literature
The prevalence of chronic disease in our primary care patient sample was 50.4% with 25.4% having multi-morbidity which was higher than in a general population study in southern China where the prevalence of multi-morbidity was only 11.1% (18). This discrepancy was to be expected because the current study was conducted on a patient population. An earlier study on primary care patients found that multi-morbidity measured by a simple count of chronic health problems was associated with the PF, RP, BP and GH domains, and the PCS scale, after controlling for confounders (6). Other studies have also found that activities of daily living (ADL) (19), instrumental ADL (19), self-rated health (19) and pain (20) are associated with depressive symptoms. Our findings fit ‘the activity restriction model of depressed affect’ proposed by Williamson, suggesting that a decline in normal activities are associated with the development of depression (2).
Our study strengthens the findings by Gunn et al. (8), which identified that self-rated HRQOL partially mediated the link between multi-morbidity and depressive symptoms. In this current study, the SF-12 v2 was used to measure the different domains of HRQOL which can make our mediation model more generalizable than the two single items used by Gunn et al. Furthermore, we simultaneously put the PF, RP, BP and GH domains into the model to compare the strength of the mediation effects of these domains.
Strengths and limitations
There were some strengths and limitations to this study. First, we had a large sample size with subjects recruited from a diverse range of settings representative of how primary health care is delivered in Hong Kong which strengthens the external validity of our results. We also had a high response rate. However, as the doctor’s practices used to recruit patients were not randomly selected, study population may not be fully representative of the Hong Kong primary care population. Future studies involving a larger or more random selection of practices or studies which recruit subjects from the general population by probability sampling may help to strengthen the generalizability of the study findings. Second, although the PHQ-9 and the SF-12 v2 have been well validated in this setting, all outcome measures were self-reported and may be subject to recall bias. Third, we used a checklist of eight specific chronic physical conditions to measure multi-morbidity which may be considered an oversimplification. Some might advocate using more sophisticated measures like the Charlson Comorbidity Index, however, such measures are complex to use in clinical practice, and may make the findings less generalizable. Also, as our checklist was designed to cover the most common chronic conditions encountered in Hong Kong’s primary care (13,14) the list may not be applicable to settings with differing morbidity profiles. Finally, although mediation analyses on cross-sectional data have been widely used, the model established should not be equated with causality that would require a longitudinal design.
Implications for research and practice
Since most chronic diseases are incurable, and given that GH and role limitations due to physical problems were the strongest mediators, interventions that target GH perception and enhancing functional capacity should be trialled such as patient empowerment strategies, exercise therapies, relaxation techniques, mindfulness meditation as well as physical or occupational therapies aimed at reducing pain and improving function. Furthermore, as patients with chronic disease may have their depressive symptoms masked by co-existing somatic complaints, a more holistic management approach may allow for better identification of coexisting problems and reduce the amount of depressive disorders that are missed in primary care.
To the best of our knowledge, this was the first study to use a bootstrapping method to explore the interrelationship between multi-morbidity, HRQOL and depressive symptoms. Further research is suggested to assess the strength of other potential mediating pathways between multi-morbidity and depression to help gain a better understanding of how these two sources of global burden may be eased. An exploration of the association between multi-morbidity, HRQOL and MH using HRQOL as an outcome measure and MH symptoms as the mediator could be conducted to better understand the relative importance of these complexes and multi-dimensional constructs in patients with chronic disease.
Conclusion
Over half of our primary care study population have at least one chronic disease with a quarter having multiple co-morbidities. We found that patients with more chronic disease tend to have more severe depressive symptoms and the relationship is fully mediated through physical HRQOL, in particular, GH perception, BP and role functioning. Targeting these aspects of HRQOL may help to alleviate the impact of multi-morbidity on MH. We hope that the study can provide a conceptual framework for intervention delivery.
Declaration
Funding: Food and Health Bureau Commissioned Research on Mental Health Policy and Service (SMH-27).
Ethical approval: Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (UW 09-305); the Research Committee of Hong Kong Sanatorium and Hospital; the Research Ethics Committee for Hong Kong Hospital Authority Kowloon East and Kowloon Central Clusters (KC/KE-10–0159); the Joint Chinese University of Hong Kong - New Territories East Cluster Clinical Research Ethics Committee (CRE-2010.439); the Ethics Committee of the Matilda International Hospital (2010_01); Research Committee of the Evangel Hospital.
Conflict of interest: none.
Acknowledgements
The authors wish to acknowledge the contributions of Ms Kit T.Y. Chan who was the project coordinator for the study. We also wish to acknowledge all the doctors of our Primary Care Research Network for their contribution to this study.
References
- 1. Mercer SW, Smith SM, Wyke S, O’Dowd T, Watt GC. Multimorbidity in primary care:developing the research agenda. Fam Pract 2009; 26: 79–80. [DOI] [PubMed] [Google Scholar]
- 2. Williamson GM. Extending the activity restriction model of depressed affect: evidence from a sample of breast cancer patients. Health Psychol 2000; 19: 339–47. [PubMed] [Google Scholar]
- 3. Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry 2003; 54: 216–26. [DOI] [PubMed] [Google Scholar]
- 4. Knol MJ, Heerdink ER, Egberts AC, et al. Depressive symptoms in subjects with diagnosed and undiagnosed type 2 diabetes. Psychosom Med 2007; 69: 300–5. [DOI] [PubMed] [Google Scholar]
- 5. Cohen S, Rodriquez MS. Pathways linking affective disturbances and physical disorders. Health Psychol 1995; 14: 374–80. [DOI] [PubMed] [Google Scholar]
- 6. Fortin M, Bravo G, Hudon C, et al. Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual Life Res 2006; 15: 83–91. [DOI] [PubMed] [Google Scholar]
- 7. Ferrari AJ, Charlson FJ, Norman RE, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med 2013; 10: e1001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gunn JM, Ayton DR, Densley K, et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatry Psychiatric Epidemiol 2012; 47: 175–84. [DOI] [PubMed] [Google Scholar]
- 9. Glynn LG, Valderas JM, Healy P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Pract 2011; 28: 516–23. [DOI] [PubMed] [Google Scholar]
- 10. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods 2008; 40: 879–91. [DOI] [PubMed] [Google Scholar]
- 11. Chin WY, Lam CL, Wong SY, et al. The epidemiology and natural history of depressive disorders in Hong Kong’s primary care. BMC Fam Pract 2011; 12: 129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chin W, Chan K, Lam C, et al. Detection and management of depression in adult primary care patients in Hong Kong: a cross-sectional survey conducted by a primary care practice-based research network. BMC Fam Pract 2014; 15: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lam CL, Leung GM, Mercer SW, et al. Utilisation patterns of primary health care services in Hong Kong: does having a family doctor make any difference? Hong Kong Med J 2011; 17: 28–32. [PubMed] [Google Scholar]
- 14. Lo Y, Lam C, Lam T, et al. Hong Kong primary care morbidity Survey 2007–2008. Hong Kong Practitioner 2010; 32: 17–26. [Google Scholar]
- 15. Cheng CM, Cheng M. To validate the Chinese version of the 2Q and PHQ-9 questionnaires in Hong Kong Chinese patients. The Hong Kong Practitioner 2007; 29: 381–90. [Google Scholar]
- 16. Lam ET, Lam CL, Fong DY, Huang WW. Is the SF-12 version 2 Health Survey a valid and equivalent substitute for the SF-36 version 2 Health Survey for the Chinese? J Eval Clin Pract 2013; 19: 200–8. [DOI] [PubMed] [Google Scholar]
- 17. Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods 2002; 7: 422. [PubMed] [Google Scholar]
- 18. Wang HH, Wang JJ, Wong SY, et al. Epidemiology of multimorbidity and implications for healthcare: Cross-sectional survey among 162,464 community household residents in southern China. BMC Med 2014; 12: 188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Anstey KJ, von Sanden C, Sargent-Cox K, Luszcz MA. Prevalence and risk factors for depression in a longitudinal, population-based study including individuals in the community and residential care. Am J Geriatric Psychiatry 2007; 15: 497–505. [DOI] [PubMed] [Google Scholar]
- 20. Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry 2003; 60: 39–47. [DOI] [PubMed] [Google Scholar]