Abstract
In 2020, for the first time, the Dietary Guidelines for Americans will include recommendations for children from birth to age 24 mo. We examined average nutrient intakes as well as total vegetable and white potato (WP) consumption among children aged 1–3 y using day 1 dietary data from the NHANES 2009–2012 and the Food Patterns Equivalents Database 2009–2012. Appropriate survey weights were used to calculate average daily consumption of total vegetables and WPs, which included French-fried potatoes and chips, for boys and girls aged 1–3 y. We calculated mean intakes of selected nutrients of concern, including vitamin D, potassium, dietary fiber (DF), and calcium. We also examined intakes of selected nutrients by major food group. Average intakes of most nutrients, including calcium, by children aged 1–3 y exceeded Dietary Reference Intakes (DRIs). However, average intakes of potassium, DF, and vitamin D were 67%, 55%, and 49% of DRIs, respectively. Mean total vegetable intake was less than the recommendation of 1 cup/d. Boys and girls aged 1–3 y consumed an average of 0.58 cup equivalents of total vegetables on the day of the survey, which included 0.16 cups of WPs. Average vegetable consumption and mean intakes of potassium, DF, and vitamin D were far below recommendations. The consumption of all vegetables, particularly those that are excellent sources of potassium and DF, such as potatoes, should be encouraged.
Keywords: vegetables, potatoes, toddlers, potassium, dietary fiber, nutrient intake
Introduction
The Dietary Guidelines for Americans (DGA)3 were first published in 1980 by the USDA and the US Department of Health and Human Services. By law, the guidelines are updated every 5 y and are intended for healthy individuals over the age of 2. In 2020, and for the first time since 1980, the DGA will include recommendations for infants and toddlers from birth to 24 mo of age. Little is known, however, about the nutrient requirements for this age group, with most recommendations being extrapolated from studies conducted in older children or adults.
Key recommendations in the 2010 DGA included increasing vegetable and fruit intake and choosing foods that provide more potassium, dietary fiber (DF), calcium, and vitamin D, which are nutrients of concern in the American diet (1). Moreover, the 2010 DGA recommend that children 2–3 y of age consume at least 1 cup of vegetables each day—and more for physically active children. There are no guidelines for vegetable consumption by infants and toddlers aged 1–3 y.
The DGA affect 15 federal food assistance programs, which are used by 1 in 4 Americans every day (2). The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) serves at-risk, low-income pregnant, breastfeeding, and postpartum women, infants, and young children under age 5. More than half of newborn infants in the United States are served by WIC. In 2012, more than half of WIC participants were 1- to 4-y-old children (3). Certain foods that are rich sources of selected nutrients are specified to supplement the diets of WIC participants.
The National Academies’ Institute of Medicine (IOM) affects dietary guidance as it convenes expert committees that examine various health issues. In 2007, the IOM published a report that recommended that the USDA encourage greater fruit and vegetable consumption by issuing a cash value voucher (CVV). USDA regulation allowed WIC participants to use the CVV for purchasing any fruit or vegetable, except for white potatoes (WPs) (4).
In 2014, the USDA sponsored another IOM review of the WIC food package with an expedited review of the exclusion of WPs in the WIC program. After its review, the IOM committee published a letter report to the USDA on 3 February 2015, recommending that WPs be included in the WIC program like any other vegetable (5). The report concluded that, “The nutrient profile of white potatoes does not support their exclusion from the CVV because their nutrient content is similar to that of other starchy vegetables included in the CVV. Increased consumption of white potatoes could improve potassium intake for both women and children.”
The IOM report also reiterated that WIC participants’ intake of all fruit and vegetables could be improved, including that of starchy vegetables. Research has found that most children and adolescents do not consume the recommended daily servings of fruit and vegetables (6).
The purpose of this study was to assess nutrient intakes and vegetable and WP consumption across races/ethnicities among toddlers aged 1–3 y. We also identified food groups that contribute to the intake of selected nutrients: potassium, DF, calcium, iron, and vitamins A and D.
Methods
We examined mean intakes of macro- and micronutrients of concern as well as consumption of total vegetables, WPs, oven-baked and deep-fried French-fried potatoes (FFPs), and other starchy vegetables by children aged 1–3 y using dietary data from NHANES 2009–2010 and 2011–2012 and the Food Patterns Equivalents Database (FPED) 2009–2010 and 2011–2012 (7–9). NHANES is conducted by the National Center for Health Statistics of the CDC, and survey data are released in 2-y cycles. All NHANES data collections receive approval from the National Center for Health Statistics Research Ethics Review Board. These data are publicly available and represent all noninstitutionalized persons living in the United States.
Our analysis used data from the first day of the 24-h dietary recall (24HR) and the total nutrient intake files. Dietary intake was measured by using a multipass 24HR instrument that has been thoroughly tested for accuracy. Methods of collecting these data are explained on the USDA’s website (10). The 24HR data were provided by the children’s primary caregivers. Only day 1 dietary recall data were used because, according to the NHANES documentation, “the mean of the population’s distribution of usual intake can be estimated from a sample of individuals’ 24-h recalls, without sophisticated statistical adjustment” (11). In addition, day 1 dietary recall data were collected in-person, whereas day 2 data were collected on a smaller subsample by phone interview.
The FPED converts foods and beverages in the Food and Nutrient Database for Dietary Studies to cup equivalents of fruit, vegetables, and dairy; ounce equivalents of grains and protein foods; teaspoon equivalents of added sugars; gram equivalents of solid fats and oils; and number of alcoholic drinks (7, 8). For coding purposes, the FPED groups foods and beverages into the following categories: milk and milk products (dairy); meat, poultry, fish, and mixtures (meats); eggs; legumes, nuts, and seeds (beans and seeds); grain products including whole grains and refined grains (carbohydrates); fruit; vegetables; fats, oils, and salad dressings (fats); and sugars, sweets, and sugar-sweetened beverages (sweets). The sweets category includes added sugars, which were defined as sugars that were added to foods as an ingredient during preparation, processing, or at the table. In the fruit and vegetable groups, a cup equivalent is the amount of a food considered to be equivalent to 1 cup of a cut-up fruit or vegetable (7, 8).
Appropriate survey weights were used to calculate average daily nutrient intakes and consumption of total vegetables, WPs, FFPs, and other starchy vegetables (sweet corn, green peas, and lima beans) for boys and girls aged 1–3 y. For purposes of this study, WPs included the following: baked, boiled, fried, hash-browned, home-fried, mashed, roasted, salad, scalloped, stuffed, with sauce, and potato chips. FFPs were included in the total WP means.
We also calculated mean day 1 intakes of all nutrients of concern for this population, including vitamin D, calcium, potassium, DF, and iron and estimated the average contribution of these nutrients from WPs. The FPED was used to convert grams of vegetables and vegetable combinations, including WPs, to cup equivalents.
We compared mean vegetable consumption and nutrient intake across genders and races/ethnicities, which included non-Hispanic blacks (NHBs), non-Hispanic whites (NHWs), Mexican Americans (MAs), and other races/ethnicities (OREs). The ORE group was diverse and included non-MA Hispanics, Asian Americans, Pacific Islanders, and others; therefore, results should be interpreted with caution. Group means for each data cycle of NHANES were estimated in STATA 9.2 by using the “svyreg” procedure to adjust for the complex design of the survey and the “subpop” option to calculate the group means for the age group (12). This procedure used a Taylor linearization approach to correct the estimated SEs for survey design effects. The significance of differences of intakes between gender and race/ethnicity means (P < 0.05) was calculated by using the STATA “test” procedure, which performed an adjusted Wald test when used after the “svyreg” procedure. This test calculated the probability that any 2 estimated means were equal to one another. WP consumers were defined as individuals who reportedly consumed any type of WP on the given survey day. Children who reportedly consumed any breast milk were excluded from the analysis.
Results
Demographic characteristics.
There were 370 NHW, 304 NHB, 320 MA, and 319 ORE children in the combined NHANES 2009–2012 unweighted sample (Table 1). Approximately 30% of households with children ages 1–3 y reported a total household income <$25,000, with ∼39% of children living at <130% of the federal poverty level. Approximately half of MA children and more than half of NHB children lived in households with an annual family income <$25,000, whereas approximately one-third of ORE children and 15% of NHW children lived in households with an annual income <$25,000.
TABLE 1.
Demographic characteristics by race/ethnicity among children aged 1–3 y: NHANES 2009–20121
| All (n = 1313) | NHWs (n = 370) | NHBs (n = 304) | MAs (n = 320) | OREs (n = 319) | |
| Boys, % | 52.8 ± 2.0 | 55.4 ± 3.3 | 51.9 ± 3.7 | 52.1 ± 3.4 | 46.4 ± 4.1 |
| Age, y | 2.0 ± 0.03 | 2.1 ± 0.05 | 2.0 ± 0.05 | 1.9 ± 0.05 | 2.1 ± 0.06 |
| Families with annual income <$25,000, % | 29.6 ± 1.6 | 15.4 ± 2.0 | 56.2 ± 4.0 | 47.4 ± 3.9 | 33.2 ± 4.2 |
| Families living in poverty (<130% of PIR), % | 39.0 ± 1.8 | 23.1 ± 2.5 | 64.0 ± 4.1 | 63.9 ± 4.1 | 42.6 ± 4.3 |
Values are sample-weighted means or proportions ± SEs calculated by using STATA, 2006. Children who consumed breast milk on the day of the survey were excluded from the analysis. MA, Mexican American; NHB, non-Hispanic black; NHW, non-Hispanic white; ORE, other race/ethnicity; PIR, poverty-to-income ratio.
Intake of nutrients.
The mean energy intake for this sample of 1- to 3-y-old children was ∼1400 kcal/d—on the higher end of the range established for 2- to 3-y-old children by the 2010 DGA (Table 2). Mean protein and total fat intakes were greater than the RDA and Acceptable Macronutrient Distribution Range, whereas average DF intake, 10.5 g DF/d, was lower than the recommended Adequate Intake (AI) (14).
TABLE 2.
Mean daily intakes of energy and selected nutrients by gender and race/ethnicity among children aged 1–3 y: NHANES 2009–20121
| All (n = 1313) | Boys (n = 693) | Girls (n = 620) | NHWs (n = 370) | NHBs (n = 304) | MAs (n = 320) | OREs (n = 319) | DRI2 | |
| Energy, kcal/d | 1400 ± 14.3 | 1440 ± 17.5 | 1370* ± 25.7 | 1410b ± 29.1 | 1520a ± 38.9 | 1340b ± 35.8 | 1350b ± 33.0 | — |
| Protein, g/d | 51.9 ± 0.7 | 52.3 ± 0.9 | 51.6 ± 1.1 | 52.0 ± 1.3 | 52.7 ± 1.2 | 51.8 ± 1.4 | 51.2 ± 1.7 | 13 |
| Total fat, g/d | 50.5 ± 0.7 | 51.4 ± 1.0 | 49.6 ± 1.1 | 50.5a,b ± 1.5 | 56.1a ± 2.2 | 49.9b ± 1.7 | 46.4b ± 1.5 | 30–40 |
| SFAs, g/d | 18.9 ± 0.3 | 18.9 ± 0.5 | 18.9 ± 0.4 | 19.4a ± 0.7 | 19.0a,b ± 0.7 | 19.1a ± 0.7 | 17.2b ± 0.6 | — |
| Cholesterol, mg/d | 167 ± 5.2 | 167 ± 9.1 | 168 ± 4.9 | 153c ± 7.8 | 184a,b ± 9.3 | 198a ± 8.1 | 163b,c ± 12.0 | — |
| Dietary fiber, g/d | 10.5 ± 0.2 | 10.8 ± 0.3 | 10.2 ± 0.3 | 10.7 ± 0.4 | 10.5 ± 0.4 | 9.91 ± 0.5 | 10.6 ± 0.5 | 19 |
| Vitamin C, mg/d | 83.1 ± 3.9 | 86.3 ± 5.6 | 79.8 ± 3.9 | 78.2b,c ± 6.0 | 102a ± 6.8 | 73.7c ± 4.7 | 89.6a,b ± 5.4 | 15 |
| Vitamin A, μg/d | 576 ± 13.9 | 589 ± 21.9 | 563 ± 19.4 | 597 ± 21.8 | 540 ± 24.5 | 589 ± 38.2 | 537 ± 21.2 | 300 |
| Vitamin D, μg/d | 7.4 ± 0.2 | 7.3 ± 0.2 | 7.5 ± 0.2 | 7.5a ± 0.3 | 6.3b ± 0.3 | 8.1a ± 0.4 | 7.5a ± 0.3 | 15 |
| Vitamin E,3 mg/d | 5.1 ± 0.1 | 5.4 ± 0.2 | 4.7* ± 0.1 | 5.1a,b ± 0.2 | 5.6a ± 0.3 | 4.7b ± 0.2 | 4.9b ± 0.2 | 6 |
| Folate, μg/d | 266 ± 5.1 | 268 ± 8.0 | 263 ± 8.3 | 260a,b ± 7.3 | 278a,b ± 9.2 | 252b ± 8.1 | 283a ± 12.4 | 150 |
| Calcium, mg/d | 1020 ± 22.6 | 1030 ± 32.7 | 1010 ± 26.9 | 1070a ± 43.2 | 885b ± 30.1 | 1030a ± 36.7 | 992a ± 30.6 | 700 |
| Iron, mg/d | 10.2 ± 0.2 | 10.4 ± 0.3 | 10.1 ± 0.3 | 10.0b ± 0.3 | 11.5a ± 0.3 | 9.67b ± 0.3 | 10.4b ± 0.4 | 7 |
| Potassium, mg/d | 2000 ± 27.5 | 2040 ± 33.4 | 1970 ± 46.0 | 2000 ± 51.3 | 2010 ± 43.8 | 2010 ± 59.6 | 2000 ± 56.1 | 3000 |
| Sodium, mg/d | 1990 ± 28.1 | 2010 ± 37.4 | 1980 ± 44.5 | 1990b ± 55.9 | 2220a ± 59.3 | 1860b ± 58.1 | 1930b ± 62.7 | 1000 |
Values are sample-weighted means ± SEs based on day 1 24-h dietary recall data calculated by using STATA, 2006. Children who consumed breast milk on the day of the survey were excluded from the analysis. *Different from boys, P < 0.05. Labeled race/ethnicity means in a row without a common superscript letter differ, P < 0.05. MA, Mexican American; NHB, non-Hispanic black; NHW, non-Hispanic white; ORE, other race/ethnicity.
The DRIs for protein, vitamin C, vitamin A, vitamin D, vitamin E, folate, calcium, iron, and sodium are RDAs. The DRI for total fat is an Acceptable Macronutrient Distribution Range. The DRIs for dietary fiber and potassium are Adequate Intakes (13–19).
Includes added α-tocopherol.
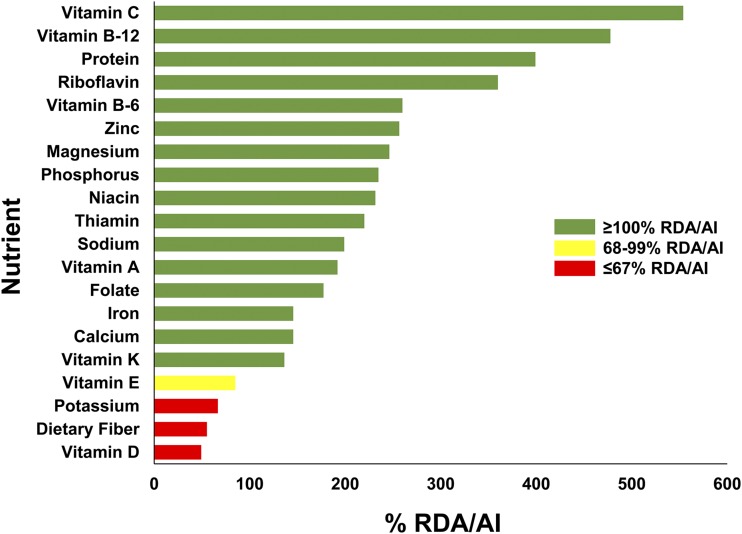
Mean intakes of most micronutrients by children aged 1–3 y exceeded the DRIs (13, 15–19) (Figure 1). For example, mean vitamin C intake was >500% of the RDA. Mean vitamin A, calcium, and iron intakes were ∼150–200% of RDAs. The mean intake of vitamin E was 5.1 mg/d, lower than the RDA of 6 mg/d. Mean intakes of potassium and vitamin D were lower than the IOM’s DRIs. Mean potassium intake among children aged 1–3 y was ∼2000 mg/d—two-thirds of the AI. Mean intake of vitamin D was 7.4 μg/d, whereas the RDA for vitamin D is 15 μg/d.
FIGURE 1.
Mean daily intakes of selected nutrients as a percentage of DRIs (RDA or AI) among children aged 1–3 y: NHANES 2009–2012 (13–19). AI, Adequate Intake.
Boys and girls in this age group had few significant differences in intakes of most nutrients, including protein, total fat, saturated fat, cholesterol, folate, iron, DF, vitamin A, vitamin C, vitamin D, calcium, potassium, and sodium. On average, boys consumed more total energy and vitamin E than did girls (Table 2).
Across race/ethnicity we found no significant differences in mean intakes of the following nutrients: protein, DF, vitamin A, and potassium (Table 2). MAs and OREs had significantly lower intakes of total fat than did NHB children; ORE children had significantly lower mean intakes of saturated fat than did NHW and MA children and significantly lower mean cholesterol intakes than did MA children.
Mean calcium intakes for all races/ethnicities were greater than the Estimated Average Requirement (500 mg Ca/d) and the RDA (700 mg Ca/d) (17, 18). Although average calcium intake by NHB children was greater than the RDA, NHB children consumed significantly less calcium and vitamin D than did all other children, which possibly reflects lower consumption of milk and other dairy products by NHBs (20). NHB children also had significantly higher mean intakes of vitamin E and iron than their MA and ORE counterparts. Mean potassium intake was below the AI and was not significantly different across races/ethnicities. Although mean sodium intakes of all children were higher than the AI, NHB children had a significantly higher intake of this nutrient than did children of all other races/ethnicities. The mean sodium-to-potassium ratio for this sample, therefore, was higher for NHB children than it was for other children.
Vegetable consumption.
The 2010 DGA recommend 1–1.5 cups of vegetables/d and 2–3.5 cups of starchy vegetables/wk for individuals consuming 1000–1400 kcal/d (1). Boys and girls aged 1–3 y across all races/ethnicities consumed an average of 0.58 cup equivalents of total vegetables/d, which included 0.21 cup equivalents of total starchy vegetables/d, or ∼1.5 cup equivalents of starchy vegetables/wk (Table 3). On average, young children consumed 0.16 cup equivalents of WPs/d (including FFPs and potato chips). The mean consumption of FFPs was ∼0.05 cup equivalents/d or <2.5 teaspoons/d—and there were few significant differences in consumption across races/ethnicities. On average, NHB children consumed more WPs than did NHW, MA, and ORE children and more FFPs than did ORE children.
TABLE 3.
Mean daily intakes of total vegetables and selected starchy vegetables by race/ethnicity among children aged 1–3 y: NHANES 2009–2012 and FPED 2009–20121
| All (n = 1313) | NHWs (n = 370) | NHBs (n = 304) | MAs (n = 320) | OREs (n = 319) | |
| Total vegetables2 | 0.58 ± 0.02 | 0.57 ± 0.03 | 0.63 ± 0.04 | 0.58 ± 0.04 | 0.57 ± 0.04 |
| White potatoes3 | 0.16 ± 0.01 | 0.14b ± 0.02 | 0.23a ± 0.02 | 0.16b ± 0.02 | 0.15b ± 0.02 |
| French-fried potatoes4 | 0.05 ± 0.01 | 0.06a,b ± 0.01 | 0.07a ± 0.01 | 0.05a,b ± 0.01 | 0.03b ± 0.01 |
| Other starchy vegetables5 | 0.06 ± 0.01 | 0.06a ± 0.01 | 0.06a ± 0.01 | 0.03b ± 0.01 | 0.06a,b ± 0.02 |
Values are sample-weighted cup equivalent means ± SEs based on day 1 24-h dietary recall data calculated by using STATA, 2006. Children who consumed breast milk on the day of the survey were excluded from the analysis. Labeled means in a row without a common superscript letter differ, P < 0.05. FPED, Food Patterns Equivalents Database; MA, Mexican American; NHB, non-Hispanic black; NHW, non-Hispanic white; ORE, other race/ethnicity.
Includes white potatoes and other starchy vegetables.
Includes baked, boiled, fried, hash-browned, home-fried, mashed, roasted, scalloped, stuffed, with sauce, potato salad, and potato chips.
Includes oven-baked and deep-fried French fried potatoes.
Includes sweet corn, green peas, and lima beans.
Food groups and associated nutrients of concern.
For children aged 1–3 y, dairy and fruit were top sources of potassium (Table 4). All vegetables—including WPs—provided 195 mg K/d, on average; WPs contributed ∼38% of the potassium from vegetables. In addition to potassium, dairy products were the top source of vitamin A and calcium. Top sources of DF included the category of carbohydrates (i.e., breads, cereals, and other grain products), fruit, and vegetables. WPs provided 29% of vegetable fiber to the diets of young children. Top food sources of vitamin D included carbohydrates, dairy, and meats (Table 4).
TABLE 4.
Mean daily intakes of selected nutrients by food source among children aged 1–3 y: NHANES 2009–20121
| Potassium, mg/d | Dietary fiber, g/d | Vitamin A, μg/d | Vitamin C, mg/d | Iron, mg/d | Calcium, mg/d | Vitamin D, μg/d | |
| Dairy | 725 ± 16.9 | 0.4 ± 0.03 | 272 ± 8.0 | 2.3 ± 0.3 | 0.6 ± 0.04 | 683 ± 21.2 | 0.6 ± 0.05 |
| Fruit | 391 ± 17.5 | 2.6 ± 0.1 | 12.9 ± 0.9 | 50.7 ± 2.9 | 0.5 ± 0.02 | 52.9 ± 4.5 | 0.4 ± 0.02 |
| Carbohydrates | 308 ± 7.2 | 4.7 ± 0.1 | 155 ± 6.9 | 4.9 ± 0.3 | 7.0 ± 0.2 | 189 ± 6.1 | 1.9 ± 0.1 |
| Meats | 226 ± 8.9 | 0.6 ± 0.03 | 23.8 ± 3.7 | 1.7 ± 0.2 | 1.0 ± 0.04 | 26.7 ± 1.3 | 0.6 ± 0.03 |
| Total vegetables2 | 195 ± 10.0 | 1.4 ± 0.1 | 67.6 ± 8.0 | 6.9 ± 0.5 | 0.4 ± 0.02 | 16.5 ± 1.2 | 0.5 ± 0.03 |
| White potatoes3 | 73.5 ± 7.6 | 0.4 ± 0.05 | 2.2 ± 0.3 | 1.1 ± 0.1 | 0.1 ± 0.01 | 3.9 ± 0.6 | 0.1 ± 0.02 |
| Sweets | 71.7 ± 6.2 | 0.1 ± 0.01 | 10.8 ± 3.9 | 16.0 ± 2.0 | 0.2 ± 0.02 | 31.0 ± 1.3 | 0.4 ± 0.06 |
| Beans | 56.7 ± 5.8 | 0.8 ± 0.1 | 1.1 ± 0.4 | 0.4 ± 0.1 | 0.3 ± 0.04 | 8.0 ± 0.9 | 0.4 ± 0.05 |
| Eggs | 28.4 ± 3.7 | 0.02 ± 0.01 | 25.5 ± 2.7 | 0.2 ± 0.1 | 0.2 ± 0.03 | 15.7 ± 1.8 | 0.2 ± 0.03 |
| Fats | 0.6 ± 0.1 | 0.003 ± 0.001 | 0.2 ± 0.03 | 0.01 ± 0.004 | 0.005 ± 0.001 | 0.3 ± 0.04 | 0.04 ± 0.006 |
Values are sample-weighted means ± SEs based on day 1 24-h dietary recall data calculated by using STATA, 2006. Children who consumed breast milk on the day of the survey were excluded from the analysis.
Includes white potatoes.
Includes baked, boiled, fried, hash-browned, home-fried, mashed, roasted, scalloped, stuffed, with sauce, potato salad, and potato chips.
Discussion
In general, average nutrient intakes of children aged 1–3 y were greater than or equal to the recommended levels. Our findings are similar to the FITS (Food Intake by Infants and Toddlers) 2008, which showed that the majority of infants and toddlers met or exceeded requirements for most nutrients (21). Our study also showed that average intakes of potassium, DF, and vitamin D across all races were far below recommendations. NHB toddlers had a significantly lower intake of vitamin D than did all other toddlers.
Although the intake of calcium was above the Estimated Average Requirement and RDA for all races, lower intakes of calcium by NHB children begins in toddlerhood and persists into adolescence and adulthood. NHB adolescent and adult females, in particular, have significantly lower intakes of calcium and lower consumption of milk and milk products than do other races/ethnicities (22–24). The mean intake of potassium and DF in toddlers was approximately half of the AI for these nutrients, suggesting the need for greater consumption of foods that are good sources of these nutrients, such as milk, fruit/fruit juices, and WPs. As shown previously, WPs, including FFPs, are rich in potassium and are important sources of DF (25).
Our study showed that the mean consumption of vegetables and starchy vegetables, including WPs, was lower than the DGA recommendations among children aged 1–3 y. There are many challenges associated with increasing vegetable consumption, particularly among young children (26–28). Resistance to eating new vegetables is particularly challenging when trying to increase fruit and vegetable consumption among toddlers (29, 30). Serving a variety of vegetables or pairing familiar tastes of well-accepted vegetables, such as WPs, with less familiar ones may also help guide children into eating more vegetables.
The results suggest that patterns of potassium, DF, and vitamin D intake for young children should be studied further in order to develop strategies for increasing intakes of these crucial nutrients. The consumption of a variety of all vegetables, including WPs, is important to increase potassium and DF intakes and should be encouraged. Understanding racial and ethnic differences in vegetable consumption and nutrient intake will allow policy makers to tailor policies to promote healthy lifestyles.
Acknowledgments
Both authors read and approved the final version of the manuscript.
Footnotes
Abbreviations used: AI, Adequate Intake; CVV, cash value voucher; DF, dietary fiber; DGA, Dietary Guidelines for Americans; FFP, French-fried potato; FPED, Food Patterns Equivalents Database; IOM, Institute of Medicine; MA, Mexican American; NHB, non-Hispanic black; NHW, non-Hispanic white; ORE, other race/ethnicity; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; WP, white potato; 24HR, 24-h dietary recall.
References
- 1.USDA; US Department of Health and Human Services. Dietary guidelines for Americans, 2010. 7th ed Washington (DC): US Government Printing Office; 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.USDA. US Department of Agriculture Budget Summary and Annual Performance Plan FY16 [cited 2015 Feb 25]. Available from: http://www.obpa.usda.gov/budsum/fy16budsum.pdf.
- 3.USDA, Food and Nutrition Service, Office of Policy Support. Women, infants, and children (WIC) participant and program characteristics 2012: summary. December 2013 [cited 2015 Feb 25]. Available from: http://www.fns.usda.gov/sites/default/files/WICPC2012_Summary.pdf.
- 4.Institute of Medicine. WIC food packages: time for a change. Washington (DC): National Academies Press; 2006. [Google Scholar]
- 5.Institute of Medicine. Review of WIC food packages: an evaluation of white potatoes in the cash value voucher [letter report]. Washington (DC): National Academies Press; 2015. [PubMed] [Google Scholar]
- 6.Nielsen SJ, Rossen LM, Harris DM, Ogden CL. Fruit and vegetable consumption of U.S. youth, 2009–2010. Hyattsville (MD): National Center for Health Statistics; 2014. NCHS Data Brief No. 156. [PubMed] [Google Scholar]
- 7.Bowman SA, Clemens JC, Thoerig RC, Friday JE, Shimizu M, Moshfegh AJ. Food patterns equivalents database 2009–10: methodology and user guide [online]. Beltsville (MD): Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, USDA; 2013. [cited 2014 Mar 11]. Available from: http://www.ars.usda.gov/ba/bhnrc/fsrg.
- 8.Bowman SA, Clemens JC, Friday JE, Thoerig RC, Moshfegh AJ. Food Patterns Equivalents Database 2011–12: methodology and user guide [online]. Beltsville (MD): Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, USDA; 2014. [cited 2014 Mar 12]. Available from: http://www.ars.usda.gov/nea/bhnrc/fsrg.
- 9.USDA, Agricultural Research Service. USDA Automated Multiple-Pass Method [cited 2014 Mar 12]. Available from: http://www.ars.usda.gov/Services/docs.htm?docid=7710.
- 10.US Department of Health and Human Services; National Center for Health Statistics. National Health and Nutrition Examination Survey: dietary interviewers procedures manual. [cited 2014 Oct 22]. Available from: http://www.cdc.gov/nchs/data/nhanes/dr-1-5.pdf.
- 11.US Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Health Statistics. NHANES dietary data tutorial: module 14, task 1: key concepts about estimating mean food intakes [cited 2015 Feb 26]. Available from: http://www.cdc.gov/nchs/tutorials/Dietary/Basic/PopulationMeanIntakes/Info1.htm.
- 12.Stata Statistical Software. Release 9.2. College Station (TX): StataCorp; 2006.
- 13.Institute of Medicine. Dietary Reference Intakes for water, potassium, sodium, chloride and sulfate (2005). Washington (DC): National Academies Press; [cited 2015 Feb 24]. Available from: http://www.nal.usda.gov/fnic/DRI/DRI_Water/water_full_report.pdf. [Google Scholar]
- 14.Institute of Medicine. Dietary Reference Intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (2002/2005). Washington (DC): National Academies Press; [cited 2015 Feb 20]. Available from: http://www.nap.edu/read/10490/chapter/1. [Google Scholar]
- 15.Institute of Medicine. Dietary Reference Intakes for vitamin C, vitamin E, selenium, and carotenoids (2000). Washington (DC): National Academies Press; [cited 2015 Feb 20]. Available from: http://www.nap.edu/read/9810/chapter/1. [PubMed] [Google Scholar]
- 16.Institute of Medicine. Dietary Reference Intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc (2001). Washington (DC): National Academies Press; [cited 2015 Feb 20]. Available from: http://www.nap.edu/read/10026/chapter/1. [PubMed] [Google Scholar]
- 17.Institute of Medicine. Dietary Reference Intakes for calcium, phosphorous, magnesium, vitamin D, and fluoride (1997). Washington (DC): National Academies Press; [cited 2015 Feb 20]. Available from: http://www.nap.edu/read/5776/chapter/1. [PubMed] [Google Scholar]
- 18.Institute of Medicine. Dietary Reference Intakes for calcium and vitamin D (2011). Washington (DC): National Academies Press; [cited 2015 Feb 20]. Available from: http://www.nap.edu/read/13050/chapter/1. [PubMed] [Google Scholar]
- 19.Institute of Medicine. Dietary Reference Intakes for thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline (1998). Washington (DC): National Academies Press; [cited 2015 Feb 20]. Available from: http://www.nap.edu/read/6015/chapter/1. [PubMed] [Google Scholar]
- 20.Kirkpatrick SI, Dodd KW, Reedy J, Krebs-Smith SM. Income and race/ethnicity are associated with adherence to food-based dietary guidance among U.S. adults and children. J Acad Nutr Diet 2012;112:624–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Butte NF, Fox MK, Briefel RR, Siega-Riz AM, Dwyer JT, Deming DM, Reidy KC. Nutrient intakes of US infants, toddlers, and preschoolers meet or exceed dietary reference intakes. J Am Diet Assoc 2010; 110(12, Suppl)S27–37. [DOI] [PubMed] [Google Scholar]
- 22.Storey ML, Forshee RA, Anderson PA. Associations of adequate intake of calcium with diet, beverage consumption, and demographic characteristics among children and adolescents. J Am Coll Nutr 2004;23:18–33. [DOI] [PubMed] [Google Scholar]
- 23.Kong A, Odoms-Young AM, Schiffer LA, Berbaum ML, Porter SJ, Blumstein L, Fitzgibbon ML. Racial/ethnic differences in dietary intake among WIC families prior to food package revisions. J Nutr Educ Behav 2013;45:39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Storey ML, Forshee RA, Anderson PA. Beverage consumption in the US population. J Am Diet Assoc 2006;106:1992–2000. [DOI] [PubMed] [Google Scholar]
- 25.Storey ML, Anderson PA. Contributions of white vegetables to nutrient intake: NHANES 2009–2010. Adv Nutr 2013;4(Suppl):335S–44S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox MK, Condon E, Briefel RR, Reidy KC, Deming DM. Food consumption patterns of young preschoolers: are they starting off on the right path? J Am Diet Assoc 2010;110:S52–9. [DOI] [PubMed] [Google Scholar]
- 27.Anzman-Frasca S, Savage JS, Marini ME, Fisher JO, Birch LL. Repeated exposure and associative conditioning promote preschool children’s liking of vegetables. Appetite 2012;58:543–53. [DOI] [PubMed] [Google Scholar]
- 28.Cason-Wilkerson R, Goldberg S, Albright K, Allison M, Haemer M. Factors influencing healthy lifestyle changes: a qualitative look at low-income families engaged in treatment for overweight children. Child Obes 2015;11:170–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Savage JS, Peterson J, Marini M, Bordi PL Jr, Birch LL. The addition of a plain or herb-flavored reduced-fat dip is associated with improved preschoolers’ intake of vegetables. J Acad Nutr Diet 2013;113:1090–5. [DOI] [PubMed] [Google Scholar]
- 30.Roe LS, Meengs JS, Birch LL, Rolls BJ. Serving a variety of vegetables and fruit as a snack increased intake in preschool children. Am J Clin Nutr 2013;98:693–9. [DOI] [PMC free article] [PubMed] [Google Scholar]