Abstract
Hypertension is a major risk factor for developing cardiovascular disease, stroke, and kidney disease. To lower blood pressure (BP), several lifestyle changes are recommended such as weight loss, exercise, and following a healthy diet. Investigating the effect of single nutrients may have positive results, but food is consumed as part of a whole diet, resulting in nutrient interactions. The aim of this systematic review and meta-analysis was to assess the effect of dietary patterns on BP in adults. Studies that were published between January 1999 and June 2014 were retrieved using Scopus, Web of Science, and the MEDLINE database. Seventeen randomized controlled trials were included in the meta-analysis. The results suggest that healthy dietary patterns such as the Dietary Approaches to Stop Hypertension diet, Nordic diet, and Mediterranean diet significantly lowered systolic BP and diastolic BP by 4.26 mm Hg and 2.38 mm Hg, respectively. These diets are rich in fruit, vegetables, whole grains, legumes, seeds, nuts, fish, and dairy and low in meat, sweets, and alcohol. Lifestyle factors such as exercise and weight loss in combination with dietary changes may also reduce BP. Further research is needed to establish the effect of dietary patterns on BP in different cultures other than those identified in this review. The review was registered on PROSPERO (International prospective register of systematic reviews) as CRD42015016272.
Keywords: dietary patterns, blood pressure, healthy diet, hypertension, DASH diet, Nordic diet, Mediterranean diet
Introduction
Hypertension or high blood pressure (BP)5 is a major risk factor for developing cardiovascular disease (CVD), stroke, and kidney disease, and it affects ∼1 billion people globally (1). In 2001, high BP was said to cause ∼54% of strokes, 47% of ischemic heart disease, 75% of hypertensive disease, and 25% of other CVDs, leading to ∼7.6 million deaths worldwide (2). It has been estimated that lowering systolic BP (SBP) and diastolic BP (DBP) in the US population by 5.0 and 3.0 mm Hg, respectively, would result in a 15% reduction in the incidence of coronary artery disease and a 27% reduction in stroke incidence (3). Conversely, an increase of 20 mm Hg in SBP and 10 mm Hg in DBP in adults aged 40–70 y has been estimated to double the risk of developing CVD (1).
There are various approaches to dealing with high BP in the community. The report from the Eighth Joint National Committee on recommendations for the management of high BP (4) endorses the lifestyle changes recommended by the Lifestyle Work Group (5). These include weight loss for those who are overweight or obese, engaging in regular physical activity, following a healthy eating plan such as the Dietary Approaches to Stop Hypertension (DASH) diet, and reducing dietary sodium intake.
The question of the relative effects of whole lifestyles, dietary patterns, and single nutrients drives a number of areas of research. Numerous studies, including randomized controlled trials, have investigated the effect of single nutrients on BP. For example, a recent meta-analysis demonstrated that a reduction of salt (sodium chloride) intake to a mean of 4.4 g/d (1716 mg sodium/d) led to a reduction in BP by 5/3 mm Hg in hypertensive subjects and 2/1 mm Hg in normotensive subjects (6). Similarly, a large meta-analysis involving 29 randomized clinical trials showed that increased potassium intake of ≥20 mmol/d (≥780 mg/d) led to a reduction by 4.9 mm Hg and 2.7 mm Hg in SBP and DBP, respectively, without the use of antihypertensive medication (7). Although investigating the effect of single nutrients on BP may be informative, these nutrients are delivered in food, and food is usually consumed as whole diets. In addition, multiple interactions may occur between components of whole diets, so there is value in assessing the effects of the entire dietary pattern (8). Furthermore, dietary patterns may vary between different cultural environments because of the differences in types of foods consumed (9).
In addition to studying single nutrients, various randomized controlled trials and observational studies have investigated the effect of individual foods on BP with conflicting results. These include fruit and vegetables (10–12), dairy and eggs (10, 13–15), nuts (16), pulses (17), meat (11, 13, 18), chocolate (19), tea (20), coffee (21), red wine (22), and fats and oils (23). Alcohol intake is associated with an increased incidence of hypertension (24), although the magnitude of the effect depends on the timing of BP measurement after intake, with peak levels registered after ∼10 h (25). Inconsistencies in single food-based analyses provide support to the argument that it is the context in which the food is eaten that may be important in better understanding diet-BP associations.
The effects of entire dietary patterns on BP have best been demonstrated by following the DASH diet (3) and the Nordic diet (26). Both of these dietary patterns emphasize consumption of different combinations of healthy foods to lower BP. Otherwise, there are little data on which types of dietary patterns are effective in lowering BP in hypertensive and normotensive adults. The aim of this review was to assess the effect of dietary patterns on BP in adults.
Methods
Protocol and registration
The review was carried out in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines (27). The review was registered on PROSPERO (International prospective register of systematic reviews) as CRD42015016272 (28). The research question was the following: is a particular dietary pattern more effective in lowering BP in hypertensive and normotensive adults compared with an alternative diet?
Data sources
A systematic review of randomized controlled trials that investigated the effect of dietary patterns on BP in adults aged >19 y was conducted. Original research studies that were published between 1 January 1999 and 22 June 2014 were identified using the following computer-assisted published databases: Scopus, Web of Science, and MEDLINE. The initial search was conducted by using a combination of the following keywords: dietary pattern* OR dietary habit* OR food pattern* OR food habit* AND blood pressure. Inclusion criteria included randomized controlled trials, adults aged >19 y, measurement of BP as a primary or secondary outcome, and studies published in English. Initial screening was based on title and abstracts and subsequently through full-text if required. Information on study design and outcomes was entered into summary tables.
Assessment of risk of bias in included studies
Each study that was included in the meta-analysis was assessed for quality using the “risk of bias” assessment tool (29) and rated as low, unclear, or high according to defined criteria.
Statistical analysis
A meta-analysis was conducted on data from 17 randomized controlled trials identified in the review. Weighted mean differences between intervention and control groups were calculated for SBP and DBP and presented with 95% CIs using the random-effects models to account for heterogeneity in participant populations and the nature of dietary patterns (30). If the SD of the mean change was not stated in the original publication, it was computed from CIs and the SEM. Where trials reported incomplete data, the authors were contacted to provide missing information. A subgroup analysis was conducted with types of dietary patterns as subgroups and also according to the nature of intervention, such as weight loss, increased exercise, or sodium restriction. Heterogeneity was assessed using the χ2 test and the I2 statistic, with 75% considered substantial heterogeneity (29). Statistical analyses were conducted using Cochrane Review Manager Software, RevMan Version 5.3 (The Cochrane Collaboration, Copenhagen).
Results
Study characteristics
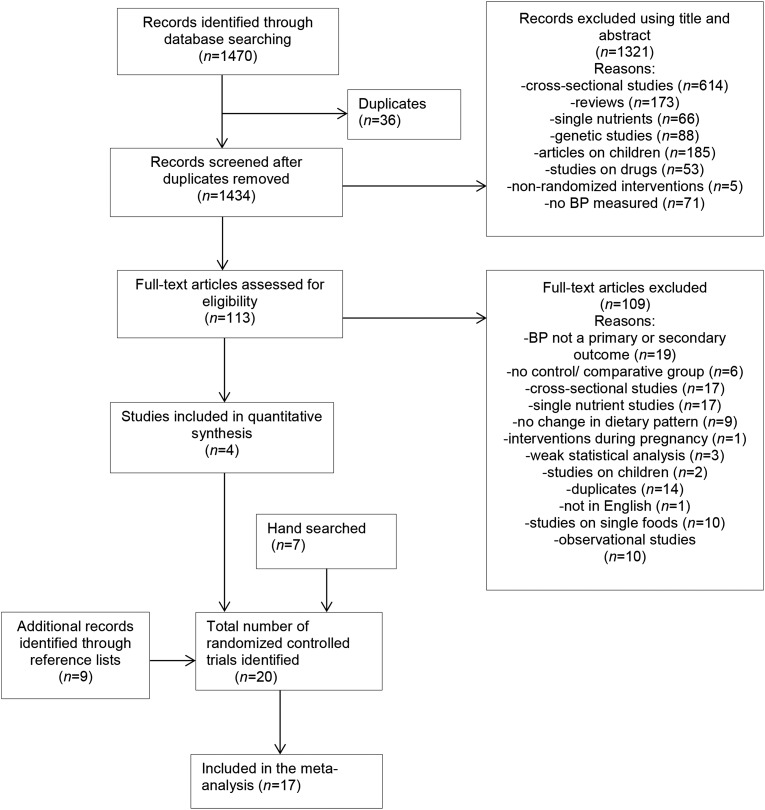
The Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram (Figure 1) illustrates the process of identifying and screening the articles included in this review. The characteristics of 20 studies that were included in the systematic review are summarized in Table 1. These studies were conducted in the following countries: United States (31–37), Italy (38, 39), Brazil (40), Iceland, Sweden (41), Denmark (42), Finland (26), Australia (43–45), France (46), Spain (47), Iran (48), and Germany (49). Overall, the trials involved 5014 participants. Sixteen studies recruited both male and female participants, one study recruited only male participants, and 3 studies recruited only female participants. Individual study duration ranged from 6 wk to 2 y. Thirteen studies included participants who were taking BP-lowering medications.
FIGURE 1.
Preferred reporting items for systematic reviews and meta-analyses flow diagram. BP, blood pressure.
TABLE 1.
Characteristics of the randomized controlled trials on dietary patterns and blood pressure1
| Reference | Country, duration | Subjects | Intervention2 | Control/comparator2 | Office or 24-h ABP | Change in SBP, mm Hg | Change in DBP, mm Hg |
| Moore et al., 1999 (31) | United States, 8 wk | 354 adults >22 y; BP <160/80–95 mm Hg; not taking BP medication | Fruit and vegetable diet: fruit ∼5 servings/d, vegetables ∼3 servings/d, whole grains ∼7 servings/d, low-fat dairy ∼0, nuts/seeds/legumes ∼1 serving/d, snacks/sweets ∼1 serving/d, fats/oils ∼5 servings/dDASH diet: fruit ∼5 servings/d, vegetables ∼4 servings/d, whole grains ∼8 servings/d, low-fat dairy ∼2 servings/d, nuts/seeds/legumes ∼1 serving/d, snacks/sweets ∼1 serving/d, fat/oils ∼3 servings/d, sodium ∼3000 mg/d | Typical American diet: fruit ∼2 servings/d, vegetables ∼2 servings/d, refined grains ∼8 servings/d, low-fat dairy ∼0, meat ∼1.5 servings/d, nuts/seeds/legumes ∼0, snacks and sweets ∼4 servings/d, fats/oils ∼6 servings/d, sodium ∼3000 mg/d | ABP | DASH diet: −4.5 (−6.2,−2.8)*3Fruit and vegetable diet: −3.1 (−4.8, −1.4)* | DASH diet: −2.7 (−4.0, −1.4)*Fruit and vegetable diet: −2.0 (−3.3, −0.8)* |
| Sacks et al., 2001 (32) | United States, 90 d | 412 adults >22 y; BP 120–159/80–95 mm Hg; not taking BP medication | DASH diet with 3 sodium amounts for both intervention and control: High: 150 mmol/d (3500 mg Na), intermediate: 100 mmol/d (2300 mg Na), low: 50 mmol/d (1150 mg Na) | Typical American diet | Office BP | High sodium: −5.9 (−8.0, −3.7)*Intermediate sodium: −5.0 (−7.6, −2.5)*Low sodium: −2.2 (−4.4, −0.1)* | High sodium: −2.9 (4.3, −1.5)*Intermediate sodium: −2.5 (−4.1, −0.8)*Low sodium: −1.0 (−2.5, 0.4)* |
| Appel et al., 2003 (33) | United States, 6 mo | 810 adults >25 y; BP 120–159/80–95 mm Hg; not taking BP medication | Established behavioral intervention: weight loss; sodium intake ~2300 mg/d; increased exercise; limited alcohol intake; no goal for fruit, vegetable, or dairyEstablished plus DASH diet: above goals plus fruit and vegetables ∼9–12 servings/d, low-fat dairy ∼2–3 servings/d | Advised on factors affecting BP such as weight, sodium reduction, physical activity and DASH diet; no behavior change counseling | Office BP | Established: −3.7 (−5.3, −2.1)*Established plus DASH: −4.3 (−5.9, −2.8)* | Established: 1.7 (−2.8, −0.6)*Established plus DASH: −2.6 (−3.7, −1.5)* |
| Blumenthal et al., 2010 (34) | United States, 4 mo | 144 adults >35 y; BP 130–159/85–99 mm Hg; not taking BP medication | Two interventions: DASH diet alone and DASH diet plus weight management, reduced caloric intake, increased exercise | Usual care (typical American diet) | Office BP and ABP | DASH plus weight management: −12.7 ± 4.5*4DASH diet alone: −7.8 ± 4.5* | DASH plus weight management: −6.1 ± 2.2*DASH diet alone: −3.7 ± 2.4* |
| Svetkey et al., 2009 (35) | United States, 6 mo | 574 adults ≥25 y; hypertensive and taking BP medications | MDI: training on management of BPPI: DASH diet, weight loss, exercise, reduced sodium intake, moderate alcohol intake | MDC: usual carePC: usual care (written), materials on lifestyle modification according to guidelines | Office BP | MDI/PI: −9.7 ± 12.7* | MDI/PI: −5.4 ± 4.6* |
| Lima et al., 2013 (40) | Brazil, 6 mo | 206 adults >20 y; BP >140/90 mm Hg; taking BP medication | Intervention: Low glycemic indexBrazilian diet incorporating DASH-Na principles: reduced salt, low-fat dairy ∼3 servings/d, fruit ∼3–5 servings/d, vegetables ∼4–5 servings/d, legumes ∼1 serving/d, grains/roots/tubers ∼5–9 servings/d, meat (mainly fish) ∼1–2 servings/d | Usual care: salt reduction, BP control | Office BP | −9.2 (SD not provided)* | −6.2 (SD not provided)* |
| Brader et al., 2014 (26) | Iceland, Sweden, Denmark, Finland; 12 wk | 37 adults 30–65 y; BP <160/100 mm Hg with or without BP medications, metabolic syndrome | Nordic diet: whole grains (rye, barley, oats), nuts, rapeseed oil, fruit/berries ≥150g/d, vegetables ≥500 g/d, fish ≥300 g/wk, low-fat dairy ∼2 servings/d, salt intake <7 g/d men, <6 g/d women | Control (mean nutrient intake in Nordic countries): wheat products, dairy-based spreads, fruit, vegetables ≤250 g/d, fish ≤100 g/wk, salt intake <10 g/d | ABP | No significant change | −4.4 (−6.9, −2.0)* |
| Nowson et al., 2005 (43) | Australia, 12 wk | 63 men >25 y; BP ≥120/80 mm Hg | DASH diet: fruit ≥4 servings/d, vegetables ≥4 servings/d, low-fat dairy ≥3 servings/d, fish ≥3 servings/wk, legumes ∼1 cup/wk, unsalted nuts ∼30 g 4 times/wk, red meat ≤2 servings/wk, fat ∼4 servings/d | Low-fat diet: advised to reduce high-energy food and drinks, choose plant-based foods, choose low-fat dairy, limit cheese and ice cream, use lean meat, avoid frying foods | Home BP | −5.2 ± 1.8* | −4.8 ± 1.3* |
| Burke et al., 2005 (44) | Australia, 4 and 12 mo | 241 adults 40–70 y; BP <160/90 mm Hg; taking BP medication | Lifestyle program (4 mo): DASH diet high in fruit and vegetables, 4 fish meals/wk, alcohol <2 standard drinks/d, low salt and sugar 12 mo follow-up: telephone contact, group workshops | Usual care: provided with information from the National Heart Foundation and Health Department; no behavior change information | ABP | −3.0 (−6.3, 0.1)* | −1.8 (−3.4, −0.2)* |
| Nowson et al., 2009 (45) | Australia, 14 wk | 111 women 45–75 y; office BP: 120–160/80–95 mm Hg; home BP: ≥116/78 mm Hg | Vitality diet (low acid load, low sodium DASH diet): red meat 6 servings/wk, low-fat dairy ≥3 servings/d, fruit ≥4 servings/d, vegetables ≥4 servings/d, fats/oils ≥4 tsp/d, whole grains ≤4 servings/d, caffeine drinks ≤4 servings/d, alcoholic drinks ≤2 servings/d; sodium 1590 mg/d | Reference healthy diet (high acid load, high carbohydrate, low fat): red meat ≤2 servings/wk, low-fat dairy ≥3 servings/d, fruit ∼2 servings/d, vegetable ∼2–3 servings/d, fats/oils ≥8 tsp/d, whole grains ≥4 servings/d, caffeine drinks ≤4 servings/d, alcoholic drinks ≤2 servings/d | Home BP | Significant change only in those taking antihypertensives: −5.5 (−11.0, 0.1)* | Significant change only in those taking antihypertensives: −3.6 (−6.9, −0.3)*, −5.3 (−8.5, −2.1)* |
| Miller et al., 2002 (36) | United States, 9 wk | 45 adults 22–70 y; BP 130–170/80–100 mm Hg; taking BP medication | Comprehensive lifestyle intervention: DASH diet alcohol ∼2 drinks/d, caffeinated beverages 3/d, sodium 2300 mg/d, increased exercise | Control: no intervention | ABP | −9.5 (−14.5, −4.5)* | −5.3 (−8.5, −2.1)* |
| Toobert et al., 2003 (37) | United States, 6 mo | 279 women <75 y; postmenopausal with type 2 diabetes | Mediterranean lifestyle Program: increased amounts of bread, vegetables, fruit, legumes, fish, less red meat, avoid cream and butter, use of olive/canola oil or margarines | Usual care | Office BP | No significant change | No significant change |
| Esposito et al., 2004 (38) | Italy, 24 mo | 180 adults with metabolic syndrome | Mediterranean diet: whole grains ∼400 g/d, fruit ∼250–300 g/d, vegetables ∼120–150 g/d, walnuts ∼25–30 g/d, olive oil ∼8 g/d | Prudent diet: general information on healthy food choices | Office BP | −3.0 (−5.0, −1.0)* | −2.0 (−3.5, −0.5)* |
| Esposito et al., 2003 (39) | Italy, 24 mo | 120 women 20–46 y | Mediterranean diet: information on calorie restriction for weight loss, behavioral and psychological counseling | Control: information about healthy food choices and exercise | Office BP | −2.0 (−3.5, −0.5)* | −1.7 (−3.0, −0.4)* |
| Vincent-Baudry et al., 2005 (46) | France, 3 mo | 212 adults 18–70 y; BP 140–190/90–105 mm Hg | Mediterranean diet recommended foods: nuts, whole-meal bread and cereals, fresh or dried fruit, vegetables, legumes, olive oil, fish ∼4 times/wk, red meat ∼1/wk, red wine ∼2 glasses/d (men), 1 glass/d (women) | Low-fat diet recommended foods: more poultry, avoid offal and saturated fat–rich animal products, fish ∼2–3 times/wk, fruit and vegetables, low-fat dairy products, use of vegetable oils | Office BP | No significant change | No significant change |
| Domenech et al., 2014 (47) | Spain, 1 y | 284 adults; men 55–80 years, women 60–80 years; type 2 diabetes or with ≥3 CVD risk factors | Interventions: Mediterranean diet and extra virgin olive oil; Mediterranean diet and mixed nuts (30 g/d) Mediterranean diet (amounts used to assess adherence): olive oil ≥4 tbs/d, vegetables ≥2 servings/d, fruit ≥3 servings/d, red meat or meat products <1 serving/d, butter/margarine/cream <12 g/d, sweet and carbonated drinks <1/d, wine ≥7 glasses/wk, legumes ≥3 servings/wk, fish ≥3 servings/wk, sweets/pastries < 3 times/wk, nuts ≥30 g/wk | Control: low-fat diet | ABP | Mediterranean diet and extra virgin olive oil: −4.0 (−6.4, −1.6)*Mediterranean diet and nuts: −4.3 (−6.7, −1.9)* | Mediterranean diet and extra virgin olive oil: −1.9 (−3.4, −0.4)*Mediterranean diet and nuts: −1.9 (−3.4, −0.4)* |
| Adamsson et al., 2011 (41) | Sweden, 6 wk | 88 adults 25–65 y; BP <145/85 mm Hg | Nordic diet: foods supplied to participants except beverages: fruits, berries, legumes, vegetables, low-fat dairy, fatty fish, oats, barley, soy protein, almonds, psyllium seeds | Control (usual Western diet); no foods provided | Office BP | −7.2 (−12.3, −1.9)* | No significant change |
| Poulsen et al., 2014 (42) | Denmark, 26 wk | 181 adults 18–65 y; BP >130/85 mm Hg | New Nordic diet: vegetables ∼400 g/d, fruit ∼300 g/d (berries ∼75 g/d), wild plants and mushrooms ∼5 g/d, nuts ∼30 g/d, milk ∼500 g/d, cheese ∼25 g/d, eggs ∼25 g/d, fresh herbs—no limit, foods organically grown | Average Danish diet: vegetables ∼180 g/d, fruit 200 g/d (berries ∼4 g/d), potatoes ∼100 g/d, no wild plants and mushrooms, fresh herbs ≤1 serving/d, nuts ≤1 serving/d, refined grains, imported fruit | Office BP | −5.2 (−8.0, −2.4)* | No significant change |
| Von Haehling et al., 2013 (49) | Germany, 12 mo | 524 adults >18 y; metabolic syndrome; coronary artery disease | Traditional Tibetan diet: cereals: barley, wheat, rye, corn, rice, oat, buckwheat; meat: beef, mutton, hare, chicken, venison; vegetables: onion, garlic, radish, fennel, leek, carrot, soy beans, dark beans; fruit: pomegranate, banana, pineapple, mango, bramble, apricot, nectarine | Usual care (Western diet): Guidelines by American Heart Association and German Academy and Society of Nutritional MedicineCereals: whole-grain rice, noodles, grains; meat: chicken, turkey, veal, rabbit; all vegetables; all fruits | Office BP | No significant change | No significant change |
| Azadbakht et al., 2011 (48) | Iran, 8 wk | 44 adults, 44–70 y; type 2 diabetes | DASH diet: fruit ∼5 servings/d, vegetables ∼7 servings/d, dairy ∼3 servings/d, whole grains ∼5 servings/d, sodium ∼2300 mg/d | Usual diabetic diet: fruit ∼3 servings/d, vegetables ∼4 servings/d, dairy ∼2 servings/d, whole grains ∼3 servings/d, sodium ∼3000 mg/d | Office BP | −10.5 (−19.2, 1.8)* | −8.8 (−17.1, −0.6)* |
Significant change, *P < 0.05. ABP, ambulatory blood pressure; BP, blood pressure; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; DBP, diastolic blood pressure; MDC, physician intervention; MDI, physician control; Na, sodium; PC, patient control; PI, patient intervention.
Servings per day unless otherwise stated, glass in terms of mL.
Mean; 95% CI in parentheses (all such values).
Mean ± SD (all such values).
Risk of bias within studies
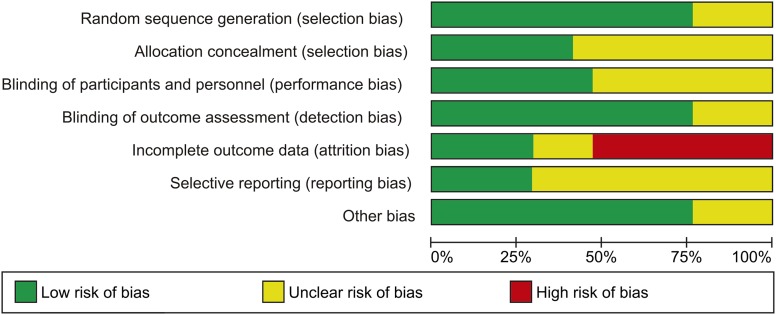
Risk of bias was assessed under various categories such as random sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessment; incomplete outcome data; selective reporting; and other bias. Four studies were unclear about the method of random sequence generation (31, 32, 34, 45), whereas 10 studies had an unclear method of allocation concealment (26, 31–33, 35, 41, 43–45, 48). Because of the challenge of blinding participants in behavioral interventions (50), a low risk was assigned where blinding of participants or staff was attempted. Inclusion of several BP measurements in each visit was considered in the assessment of other bias category. Four studies (41, 43, 44, 49) did not have enough information on whether the outcome assessors were blinded. Ten studies were assigned high risk in the category of incomplete outcome data mainly due to performance of as-treated analysis and no reasons given for missing data (26, 35, 41–45, 47–49). The results of risk of bias assessment are illustrated in Figure 2.
FIGURE 2.
Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies.
Meta-analysis results
Three studies (37, 40, 46) were not included in the meta-analysis because of incomplete data whereby SDs of mean changes could not be computed. Attempts were made to contact study authors for the missing data. Two studies did not find any significant effect of the Mediterranean diet (MD) on BP compared with the usual diet (37) or a low-fat diet (46). The other study (40) found that a low glycemic index Brazilian diet incorporating DASH-sodium principles led to a significant reduction in BP.
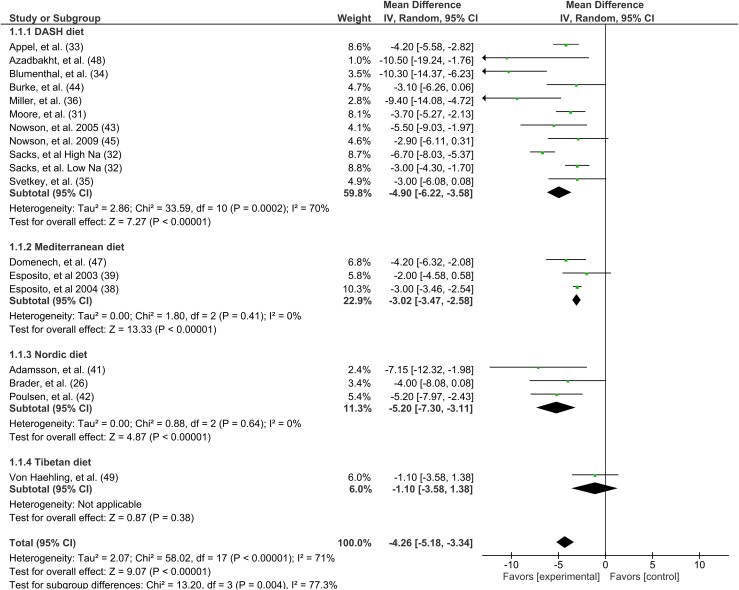
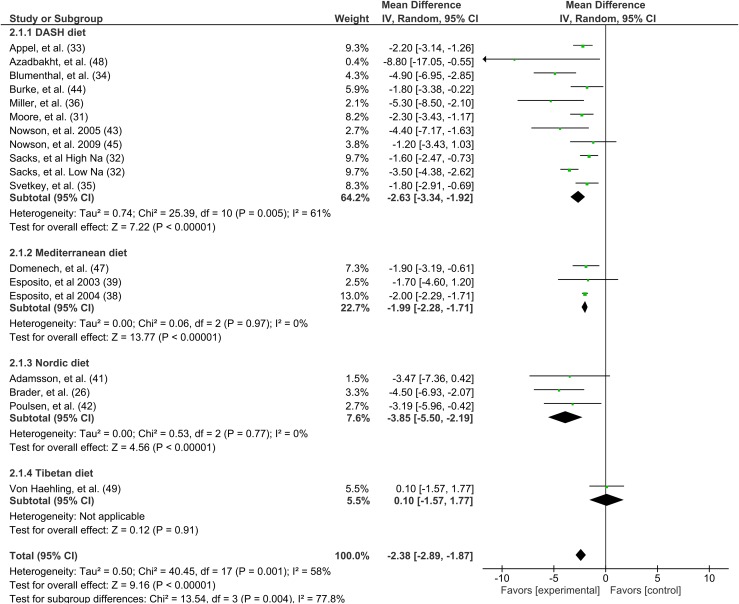
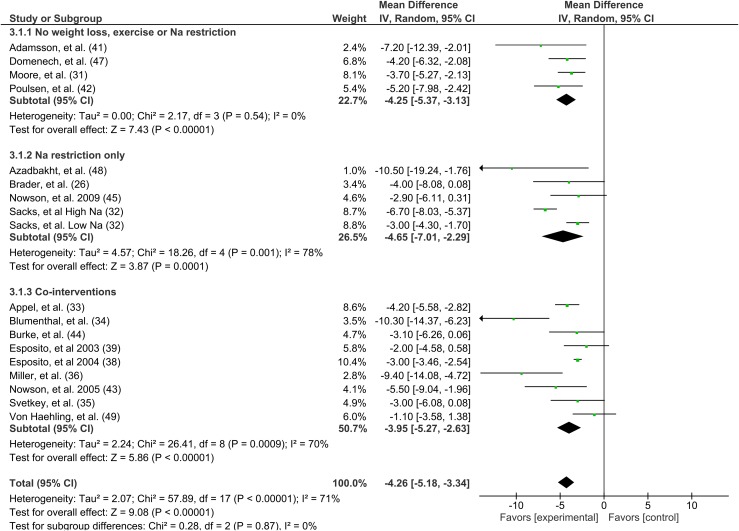
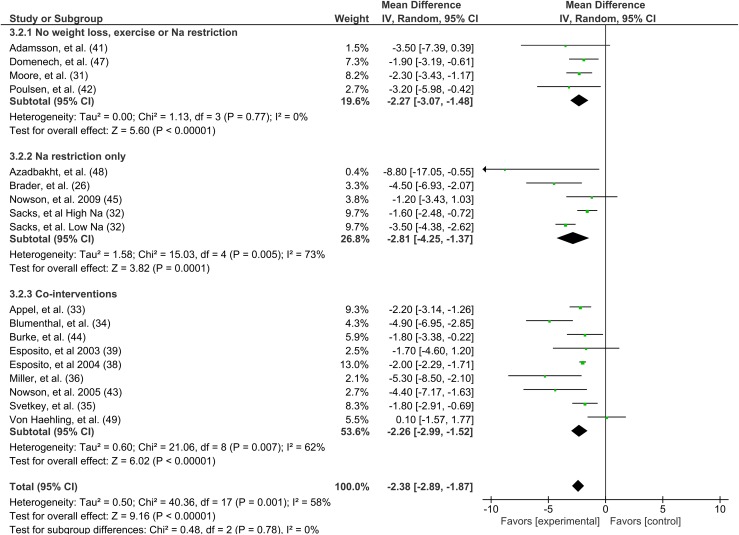
The overall effect was a statistically significant reduction in SBP by 4.26 mm Hg (95% CI: −5.18, −3.34) (Figure 3) and DBP by 2.38 mm Hg (95% CI: −2.89, −1.87) (Figure 4). Significant between-study heterogeneity was observed for both SBP (I2 = 71%, P < 0.00001) and DBP (I2 = 58%, P = 0.001). The results of the subgroup analysis suggested that only the DASH, MD, and Nordic diets significantly reduced both SBP and DBP. When considering the nature of intervention, the studies in which weight loss, exercise, and sodium restriction were kept constant had a significant reduction of 4.25 mm Hg (95% CI: −5.37, −3.13) (Figure 5) and 2.27 mm Hg (95% CI: −3.07, −1.48) (Figure 6) in SBP and DBP, respectively. Greater effects were observed in studies that had sodium restriction only and lesser effects in those that had a combination of weight loss, increased exercise, and sodium restriction.
FIGURE 3.
Forest plot of effect of the different dietary patterns in 17 randomized controlled trials on systolic blood pressure (mm Hg). DASH, Dietary Approaches to Stop Hypertension; IV, inverse variance.
FIGURE 4.
Forest plot of effect of the different dietary patterns in 17 randomized controlled trials on diastolic blood pressure (mm Hg). DASH, Dietary Approaches to Stop Hypertension; IV, inverse variance.
FIGURE 5.
Forest plot of effect of dietary patterns on systolic blood pressure (mm Hg) according to different interventions such as weight loss, exercise, and sodium restriction. IV, inverse variance.
FIGURE 6.
Forest plot of effect of dietary patterns on diastolic blood pressure (mm Hg) according to different interventions such as weight loss, exercise, and sodium restriction. IV, inverse variance.
Discussion
This meta-analysis of 17 randomized controlled trials evaluated the current evidence on the effect of dietary patterns on BP in adults. A significant reduction of 4.26 mm Hg in SBP and 2.38 mm Hg in DBP was observed in the present analysis. For the studies that had no weight loss, increased exercise, or sodium restrictions, SBP and DBP reduced by 4.25 and 2.27 mm Hg, respectively. A previous meta-analysis found a reduction of 6.74 and 3.59 mm Hg in SBP and DBP, respectively, from the DASH diet only (51). Heterogeneity was substantial for both SBP and DBP. Many differences existed between the populations studied in terms of age, sex, study methods, duration of intervention, number of participants, and difference in combination of foods included within the various dietary patterns. The existing evidence suggests that various dietary patterns are beneficial for BP and include the DASH diet, MD, and Nordic diet.
The DASH diet largely comprises of fruit and vegetables, low-fat dairy, whole grains, nuts, legumes, and seeds, with low intakes of meat and saturated fat (31). The DASH diet has been adopted in various cultural contexts such as in Brazil (40), Australia (43, 45), and Iran (48). Our results are consistent with an earlier analysis of BP and nutrient intakes in the United States, which showed that reduced consumption of dairy products and fruit and vegetable juices was a major predictor of hypertension (52). In observational studies, a high DASH score in the SU.VI.MAX (Supplementation en Vitamines et Mineraux Antioxydants) cohort was associated with lower BP at the first clinical examination and a lower increase in BP after 5 y (10). Although the DASH diet shows positive effects from the randomized controlled trials, the studies are short term in nature, and this may limit their generalization as a long-term intervention.
The Nordic diet is consumed in Nordic countries and consists of foods of Nordic origin such as whole grains, rapeseed oil, berries, fruits, vegetables, fish, nuts, and low-fat dairy products. This diet significantly reduced 24-h ambulatory DBP in comparison to a diet comprising the mean nutrient intake in Nordic countries (26). However, the effects of the diet may not be attributed to reductions in sodium or increases in potassium because neither of these electrolytes differed between intervention and control groups. One of the characteristics of the Nordic diet is that it is rich in berries. Animal studies have shown that Nordic wild blueberries lead to a reduction in BP (53), and likewise, randomized controlled trials have demonstrated that consumption of berries lowers BP (54, 55). The polyphenols, especially flavonoids, found in berries may be contributing to the BP-lowering effect of Nordic diets that typically include these fruits (56). Further research, however, is warranted on the effect of the Nordic diet on BP because only 3 studies were identified from our review.
Another dietary pattern, the MD, is generally high in plant foods such as whole-grain cereals, fresh fruits, vegetables, beans, nuts, and seeds (57, 58). It can have moderate amounts of dairy foods, fish, and poultry and low amounts of red meat, but there may be some variation in food composition between regions. In general, olive oil is the major source of fat, and wine is consumed moderately with meals. In the Prevencion con Dieta Mediterranea (PREDIMED) study, the MD in Spain was supplemented with extra virgin olive oil and with nuts, and significantly lower DBP was observed compared with a low-fat diet (59). Likewise, analysis of ambulatory BP in 235 participants of the PREDIMED study after 1 y showed significant reductions in ambulatory SBP by 4.0 and 4.3 mm Hg in the MD supplemented with extra virgin olive oil and nuts, respectively, and 1.9 mm Hg in DBP for both diets (47). These effects were also seen in studies of the MD in Italy, where significantly lower BP was observed (38, 39). However, no effect was found in one study from France (46) and the United States (37). In addition to possible differences in food and recipe composition, the study duration for these trials was <6 mo. Because diet effects tend to occur over longer periods of time, a long-term follow-up may be necessary to detect BP-lowering effects.
In comparison to randomized controlled trials, observational studies do not have control over dietary patterns, so not surprisingly, results from observational studies show more conflicting results for the MD. For example, an increased risk of developing hypertension (HR: 1.34; 95% CI: 1.04, 1.73; P = 0.002) was identified in adults with a higher adherence to the MD in Spain as identified through an updated modified MD score (60), but in the United States, an analysis of the Framingham Heart cohort found no association between the MD and BP after 7 y of follow-up in 2370 adults (61). In this case, and in comparison to the DASH diet, the analysis of the MD pattern did not distinguish between full-fat and low-fat dairy. Because low-fat dairy was used in the DASH diet, it has been assumed as contributing to the BP-lowering effect. Likewise, many of the randomized controlled trials chose to use low-fat dairy in their interventions and did not compare with full-fat dairy. Observational studies such as the Coronary Artery Risk Development in Young Adults study (13) did not distinguish between low- and full-fat dairy. Similarly, the analysis of nutrient intakes and BP in the US population did not discern any difference between low- and full-fat dairy (52). Further research is therefore warranted to investigate the effect of low-fat dairy compared with full-fat dairy on BP.
The research on the Tibetan diet was conducted in Germany and emphasized cereals from barley, wheat, rye, corn, rice, oat and buckwheat, and meat such as beef, mutton, roast hare, chicken, and venison (49). Compared with the usual Western diet in a 12-mo clinical trial, there was no significant change in BP between the 2 diets. Only one study on the Tibetan diet was identified, and this means that additional research is required before conclusions on its efficacy can be drawn.
In some studies, the amount of sodium was kept constant in both the intervention and control diets. In the original DASH study, sodium content was maintained at 3000 mg/d in all groups (31), whereas the Brazilian DASH diet was based on an intake of 2400 mg/d (40). In the original DASH diet study, a significant reduction in BP was found even when sodium intake was kept constant (31). When sodium reduction was added to the DASH diet (32), reduced BP was still seen at all sodium amounts, with a greater reduction in the high sodium amount. This suggests that regardless of the sodium content, the food pattern reflective of the DASH diet lowers BP. Sodium intake was also reduced in one of the Nordic diet studies (26) to <2730 mg/d and 2340 mg/d in men and women, respectively, making it difficult to separate out effects. These findings are consistent with recent studies that did not find a significant association between the amount of sodium intake and BP in normotensive populations (62, 63).
Various other nutrients characteristic of the DASH diet such as fiber (64), potassium (7), calcium (65), and magnesium (66) have been associated with reduced BP, but the findings are inconsistent. It is well known that nutrients have multiple interactions, for example, interactions between sodium, potassium, and calcium through either the sodium-to-potassium ratio or the BP-lowering effect of potassium and calcium due to their ability to increase sodium excretion by the kidneys (67). This understanding highlights the importance of considering the synergistic effects of whole foods and diets in examining effects.
Finally, the interface between the adoption of healthy diets and other behavioral lifestyle changes cannot be ignored. Our results indicate that cointerventions such as sodium restriction, exercise, and weight loss also led to significant BP reductions. However, a range of combinations of interventions may be effective for the management of BP, and further research on relative efficacy would be informative.
Various limitations in this review warrant discussion. It should be noted that the nature of intervention differed between studies, whereby some trials provided foods to the participants, whereas others did not. This can influence the amount of adherence to the intervention diet. Also, although the dietary patterns identified may have had some common basic characteristics, they were not homogeneous, and each diet was set in a unique cultural context. The use of BP as an endpoint for sodium intake has limitations. Recent studies using mortality or occurrence of CVD events as the composite outcomes for sodium intake have shown that lower (<7 g salt/d; 2730 mg sodium/d) or higher (>14 g salt/d; 5460 mg sodium/d) intakes are associated with increased risk of death and cardiovascular events (68, 69). In addition, the 2013 Institute of Medicine report (70) pointed out that higher sodium intakes are associated with the risk of CVD, and there is insufficient evidence on the benefit or risk of intake <2300 mg/d. The report did not assess the association of sodium intake with intermediate endpoints such as BP. In this review, we considered both studies that restricted sodium intake and those that did not in our subgroup analysis. The focus of our review, however, was the entire dietary pattern rather than sodium intake alone. Finally, there were limitations associated with individual studies used in the meta-analysis. Biases were identified, especially as-treated data analysis in 8 studies, and 2 studies that did not find a significant effect of the MD were not included. These features may have affected the overall results.
Conclusion
The consumption of dietary patterns characterized by high consumption of fruit, vegetables, whole grains, legumes, seeds, nuts, fish, and dairy and low consumption of meat, sweets, and alcohol resulted in significant reductions in BP. These reductions were found across a range of sodium intakes. Following a healthy lifestyle by incorporating exercise in addition to a healthy diet may also have an additional effect in lowering BP. Much of the population-level efforts to reduce BP are through salt reduction in the food supply. This meta-analysis supports the notion that dietary diversification may also play a role. The association between the consumption of the MD and BP warrants further investigation due to inconsistency in findings between studies. This research should consider an analysis of the effect of dietary patterns on BP in different cultures other than those identified in this review.
Acknowledgments
All authors read and approved the final manuscript.
Footnotes
Abbreviations used: BP, blood pressure; CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; DBP, diastolic blood pressure; MD, Mediterranean diet; SBP, systolic blood pressure.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., Jones DW, Materson BJ, Oparil S, Wright JT Jr., et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA 2003;289:2560–72. [DOI] [PubMed] [Google Scholar]
- 2.Lawes CMM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513–8. [DOI] [PubMed] [Google Scholar]
- 3.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 4.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20. [DOI] [PubMed] [Google Scholar]
- 5.Eckel RH, Jakicic JM, Ard JD, De Jesus JM, Houston Miller N, Hubbard VS, Lee IM, Lichtenstein AH, Loria CM, Millen BE, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation 2014;129(Suppl 2):S76–99. [DOI] [PubMed] [Google Scholar]
- 6.He FJ, Li J, Macgregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev 2013;4:CD004937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whelton PK, He J, Cutler JA, Brancati FL, Appel LJ, Follmann D, Klag MJ. Effects of oral potassium on blood pressure: meta-analysis of randomized controlled clinical trials. JAMA 1997;277:1624–32. [DOI] [PubMed] [Google Scholar]
- 8.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 2002;13:3–9. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs DR, Tapsell LC. Food synergy: the key to a healthy diet. Proc Nutr Soc 2013;72:200–6. [DOI] [PubMed] [Google Scholar]
- 10.Dauchet L, Kesse-Guyot E, Czernichow S, Bertrais S, Estaquio C, Peneau S, Vergnaud AC, Chat-Yung S, Castetbon K, Deschamps V, et al. Dietary patterns and blood pressure change over 5-y follow-up in the SU.VI.MAX cohort. Am J Clin Nutr 2007;85:1650–6. [DOI] [PubMed] [Google Scholar]
- 11.Miura K, Greenland P, Stamler J, Liu K, Daviglus ML, Nakagawa H. Relation of vegetable, fruit, and meat intake to 7-year blood pressure change in middle-aged men: the Chicago Western Electric Study. Am J Epidemiol 2004;159:572–80. [DOI] [PubMed] [Google Scholar]
- 12.Schulze MB, Hoffmann K, Kroke A, Boeing H. Risk of hypertension among women in the EPIC-Potsdam study: comparison of relative risk estimates for exploratory and hypothesis-oriented dietary patterns. Am J Epidemiol 2003;158:365–73. [DOI] [PubMed] [Google Scholar]
- 13.Steffen LM, Kroenke CH, Yu X, Pereira MA, Slattery ML, Van Horn L, Gross MD, Jacobs DR Jr. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr 2005;82:1169–77. [DOI] [PubMed] [Google Scholar]
- 14.McNaughton SA, Mishra GD, Stephen AM, Wadsworth MEJ. Dietary patterns throughout adult life are associated with body mass index, waist circumference, blood pressure, and red cell folate. J Nutr 2007;137:99–105. [DOI] [PubMed] [Google Scholar]
- 15.Engberink MF, Hendriksen MAH, Schouten EG, van Rooij FJA, Hofman A, Witteman JCM, Geleijnse JM. Inverse association between dairy intake and hypertension: the Rotterdam Study. Am J Clin Nutr 2009;89:1877–83. [DOI] [PubMed] [Google Scholar]
- 16.Zhou D, Yu H, He F, Reilly KH, Zhang J, Li S, Zhang T, Wang B, Ding Y, Xi B. Nut consumption in relation to cardiovascular disease risk and type 2 diabetes: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr 2014;100:270–7. [DOI] [PubMed] [Google Scholar]
- 17.Jayalath VH, De Souza RJ, Sievenpiper JL, Ha V, Chiavaroli L, Mirrahimi A, Di Buono M, Bernstein AM, Leiter LA, Kris-Etherton PM, et al. Effect of dietary pulses on blood pressure: a systematic review and meta-analysis of controlled feeding trials. Am J Hypertens 2014;27:56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Umesawa M, Kitamura A, Kiyama M, Okada T, Shimizu Y, Imano H, Ohira T, Nakamura M, Maruyama K, Iso H. Association between dietary behavior and risk of hypertension among Japanese male workers. Hypertens Res 2013;36:374–80. [DOI] [PubMed] [Google Scholar]
- 19.Desch S, Schmidt J, Kobler D, Sonnabend M, Eitel I, Sareban M, Rahimi K, Schuler G, Thiele H. Effect of cocoa products on blood pressure: systematic review and meta-analysis. Am J Hypertens 2010;23:97–103. [DOI] [PubMed] [Google Scholar]
- 20.Mozaffari-Khosravi H, Ahadi Z, Barzegar K. The effect of green tea and sour tea on blood pressure of patients with type 2 diabetes: a randomized clinical trial. J Diet Suppl 2013;10:105–15. [DOI] [PubMed] [Google Scholar]
- 21.Steffen M, Kuhle C, Hensrud D, Erwin PJ, Murad MH. The effect of coffee consumption on blood pressure and the development of hypertension: a systematic review and meta-analysis. J Hypertens 2012;30:2245–54. [DOI] [PubMed] [Google Scholar]
- 22.Foppa M, Fuchs FD, Preissler L, Andrighetto A, Rosito GA, Duncan BB. Red wine with the noon meal lowers post-meal blood pressure: a randomized trial in centrally obese, hypertensive patients. J Stud Alcohol 2002;63:247–51. [DOI] [PubMed] [Google Scholar]
- 23.Alonso A, Martínez-González MA. Olive oil consumption and reduced incidence of hypertension: the SUN study. Lipids 2004;39:1233–8. [DOI] [PubMed] [Google Scholar]
- 24.Núñez-Córdoba JM, Valencia-Serrano F, Toledo E, Alonso A, Martínez-González MA. The Mediterranean diet and incidence of hypertension: the Seguimiento Universidad de Navarra (SUN) study. Am J Epidemiol 2009;169:339–46. [DOI] [PubMed] [Google Scholar]
- 25.McFadden CB, Brensinger CM, Berlin JA, Townsend RR. Systematic review of the effect of daily alcohol intake on blood pressure. Am J Hypertens 2005;18:276–86. [DOI] [PubMed] [Google Scholar]
- 26.Brader L, Uusitupa M, Dragsted LO, Hermansen K. Effects of an isocaloric healthy Nordic diet on ambulatory blood pressure in metabolic syndrome: a randomized SYSDIET sub-study. Eur J Clin Nutr 2014;68:57–63. [DOI] [PubMed] [Google Scholar]
- 27.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centre for Reviews and Dissemination. International prospective register of systematic reviews [Internet]. York (United Kingdom): University of York; 2015. [cited 2015 Aug 15]. Available from: http://www.crd.york.ac.uk/PROSPERO/.
- 29.Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions version 5.1.0 (updated March 2011). London: The Cochrane Collaboration; 2011. [Google Scholar]
- 30.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- 31.Moore TJ, Vollmer WM, Appel LJ, Sacks FM, Svetkey LP, Vogt TM, Conlin PR, Simons-Morton DG, Carter-Edwards L, Harsha DW. Effect of dietary patterns on ambulatory blood pressure: results from the Dietary Approaches to Stop Hypertension (DASH) trial. DASH Collaborative Research Group. Hypertension 1999;34:472–7. [DOI] [PubMed] [Google Scholar]
- 32.Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, Simons-Morton DG, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 33.Appel LJ, Champagne CM, Harsha DW, Cooper LS, Obarzanek E, Elmer PJ, Stevens VJ, Vollmer WM, Lin P-H, Svetkey LP, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 2003;289:2083–93. [DOI] [PubMed] [Google Scholar]
- 34.Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med 2010;170:126–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Svetkey LP, Pollak KI, Yancy WS Jr, Dolor RJ, Batch BC, Samsa G, Matchar DB, Lin P-H. Hypertension improvement project: randomized trial of quality improvement for physicians and lifestyle modification for patients. Hypertension 2009;54:1226–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miller ER, Erlinger TP, Young DR, Jehn M, Charleston J, Rhodes D, Wasan SK, Appel LJ. Results of the Diet, Exercise, and Weight Loss Intervention Trial (DEW-IT). Hypertension 2002;40:612–8. [DOI] [PubMed] [Google Scholar]
- 37.Toobert DJ, Glasgow RE, Strycker LA, Barrera M Jr, Radcliffe JL, Wander RC, Bagdade JD. Biologic and quality-of-life outcomes from the Mediterranean Lifestyle Program: a randomized clinical trial. Diabetes Care 2003;26:2288–93. [DOI] [PubMed] [Google Scholar]
- 38.Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D’Armiento M, D’Andrea F, Giugliano D. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA 2004;292:1440–6. [DOI] [PubMed] [Google Scholar]
- 39.Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, Giugliano D. Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA 2003;289:1799–804. [DOI] [PubMed] [Google Scholar]
- 40.Lima STRM, da Silva Nalin de Souza B, França AKT, Salgado Filho N, Sichieri R. Dietary approach to hypertension based on low glycaemic index and principles of DASH (Dietary Approaches to Stop Hypertension): a randomised trial in a primary care service. Br J Nutr 2013;110:1472–9. [DOI] [PubMed] [Google Scholar]
- 41.Adamsson V, Reumark A, Fredriksson IB, Hammarström E, Vessby B, Johansson G, Risérus U. Effects of a healthy Nordic diet on cardiovascular risk factors in hypercholesterolaemic subjects: a randomized controlled trial (NORDIET). J Intern Med 2011;269:150–9. [DOI] [PubMed] [Google Scholar]
- 42.Poulsen SK, Due A, Jordy AB, Kiens B, Stark KD, Stender S, Holst C, Astrup A, Larsen TM. Health effect of the New Nordic Diet in adults with increased waist circumference: a 6-mo randomized controlled trial. Am J Clin Nutr 2014;99:35–45. [DOI] [PubMed] [Google Scholar]
- 43.Nowson CA, Worsley A, Margerison C, Jorna MK, Godfrey SJ, Booth A. Blood pressure change with weight loss is affected by diet type in men. Am J Clin Nutr 2005;81:983–9. [DOI] [PubMed] [Google Scholar]
- 44.Burke V, Beilin LJ, Cutt HE, Mansour J, Wilson A, Mori TA. Effects of a lifestyle programme on ambulatory blood pressure and drug dosage in treated hypertensive patients: a randomized controlled trial. J Hypertens 2005;23:1241–9. [DOI] [PubMed] [Google Scholar]
- 45.Nowson CA, Wattanapenpaiboon N, Pachett A. Low-sodium Dietary Approaches to Stop Hypertension–type diet including lean red meat lowers blood pressure in postmenopausal women. Nutr Res 2009;29:8–18. [DOI] [PubMed] [Google Scholar]
- 46.Vincent-Baudry S, Defoort C, Gerber M, Bernard MC, Verger P, Helal O, Portugal H, Planells R, Grolier P, Amiot-Carlin MJ, et al. The Medi-RIVAGE study: reduction of cardiovascular disease risk factors after a 3-mo intervention with a Mediterranean-type diet or a low-fat diet. Am J Clin Nutr 2005;82:964–71. [DOI] [PubMed] [Google Scholar]
- 47.Doménech M, Roman P, Lapetra J, García De La Corte FJ, Sala-Vila A, De La Torre R, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Lamuela-Raventós RM, et al. Mediterranean diet reduces 24-hour ambulatory blood pressure, blood glucose, and lipids: one-year randomized, clinical trial. Hypertension 2014;64:69–76. [DOI] [PubMed] [Google Scholar]
- 48.Azadbakht L, Fard NRP, Karimi M, Baghaei MH, Surkan PJ, Rahimi M, Esmaillzadeh A, Willett WC. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes Care 2011;34:55–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.von Haehling S, Stellos K, Qusar N, Gawaz M, Bigalke B. Weight reduction in patients with coronary artery disease: comparison of traditional Tibetan medicine and Western diet. Int J Cardiol 2013;168:1509–15. [DOI] [PubMed] [Google Scholar]
- 50.Rees K, Hartley L, Flowers N, Clarke A, Hooper L, Thorogood M, Stranges S. ‘Mediterranean’ dietary pattern for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev 2013;8:CD009825. [DOI] [PubMed] [Google Scholar]
- 51.Saneei P, Salehi-Abargouei A, Esmaillzadeh A, Azadbakht L. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis 2014;24:1253–61. [DOI] [PubMed] [Google Scholar]
- 52.McCarron DA, Morris CD, Henry HJ, Stanton JL. Blood pressure and nutrient intake in the United States. Science 1984;224:1392–8. [DOI] [PubMed] [Google Scholar]
- 53.Mykkänen OT, Huotari A, Herzig KH, Dunlop TW, Mykkänen H, Kirjavainen PV. Wild blueberries (Vaccinium myrtillus) alleviate inflammation and hypertension associated with developing obesity in mice fed with a high-fat diet. PLoS One 2014;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Erlund I, Koli R, Alfthan G, Marniemi J, Puukka P, Mustonen P, Mattila P, Jula A. Favorable effects of berry consumption on platelet function, blood pressure, and HDL cholesterol. Am J Clin Nutr 2008;87:323–31. [DOI] [PubMed] [Google Scholar]
- 55.Basu A, Du M, Leyva MJ, Sanchez K, Betts NM, Wu M, Aston CE, Lyons TJ. Blueberries decrease cardiovascular risk factors in obese men and women with metabolic syndrome. J Nutr 2010;140:1582–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wightman JD, Heuberger RA. Effect of grape and other berries on cardiovascular health. J Sci Food Agric 2015;95:1584–97. [DOI] [PubMed] [Google Scholar]
- 57.Willett WC, Sacks F, Trichopoulou A, Drescher G, Ferro-Luzzi A, Helsing E, Trichopoulos D. Mediterranean diet pyramid: a cultural model for healthy eating. Am J Clin Nutr 1995;61(Suppl):1402S–6S. [DOI] [PubMed] [Google Scholar]
- 58.Serra-Majem L, Roman B, Estruch R. Scientific evidence of interventions using the Mediterranean diet: a systematic review. Nutr Rev 2006;64(Suppl 1):S27–47. [DOI] [PubMed] [Google Scholar]
- 59.Toledo E, Hu FB, Estruch R, Buil-Cosiales P, Corella D, Salas-Salvadó J, Covas MI, Arós F, Gómez-Gracia E, Fiol M, et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: results from a randomized controlled trial. BMC Med 2013;11:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Toledo E, Carmona-Torre FD, Alonso A, Puchau B, Zulet MA, Martinez JA, Martinez-Gonzalez MA. Hypothesis-oriented food patterns and incidence of hypertension: 6-year follow-up of the SUN (Seguimiento Universidad de Navarra) prospective cohort. Public Health Nutr 2010;13:338–49. [DOI] [PubMed] [Google Scholar]
- 61.Rumawas ME, Meigs JB, Dwyer JT, McKeown NM, Jacques PF. Mediterranean-style dietary pattern, reduced risk of metabolic syndrome traits, and incidence in the Framingham Offspring Cohort. Am J Clin Nutr 2009;90:1608–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Graudal N, Hubeck-Graudal T, Jürgens G, McCarron DA. The significance of duration and amount of sodium reduction intervention in normotensive and hypertensive individuals: a meta-analysis. Adv Nutr 2015;6:169–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mente A, O’Donnell MJ, Rangarajan S, McQueen MJ, Poirier P, Wielgosz A, Morrison H, Li W, Wang X, Di C, et al. Association of urinary sodium and potassium excretion with blood pressure. N Engl J Med 2014;371:601–11. [DOI] [PubMed] [Google Scholar]
- 64.Eliasson K, Ryttig KR, Hylander B, Rossner S. A dietary fibre supplement in the treatment of mild hypertension: a randomized, double-blind, placebo-controlled trial. J Hypertens 1992;10:195–9. [DOI] [PubMed] [Google Scholar]
- 65.Birkett NJ. Comments on a meta-analysis of the relation between dietary calcium intake and blood pressure. Am J Epidemiol 1998;148:223–28. [DOI] [PubMed] [Google Scholar]
- 66.Whelton PK, Klag MJ. Magnesium and blood pressure: review of the epidemiologic and clinical trial experience. Am J Cardiol 1989;63:26G–30. [DOI] [PubMed] [Google Scholar]
- 67.Kotchen TA, Kotchen JM. Dietary sodium and blood pressure: interactions with other nutrients. Am J Clin Nutr 1997;65(Suppl):708S–11S. [DOI] [PubMed] [Google Scholar]
- 68.O’Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, Yan H, Lee SF, Mony P, Devanath A, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med 2014;371:612–23. [DOI] [PubMed] [Google Scholar]
- 69.Graudal N, Jürgens G, Baslund B, Alderman MH. Compared with usual sodium intake, low- and excessive-sodium diets are associated with increased mortality: a meta-analysis. Am J Hypertens 2014;27:1129–37. [DOI] [PubMed] [Google Scholar]
- 70.Strom BL, Yaktine AL, Oria M, editors. Sodium intake in populations: assessment of evidence. Washington (DC): National Academies Press; 2013. [PubMed] [Google Scholar]