Abstract
Obesity is associated with metabolic disturbances that cause tissue stress and dysfunction. Obese individuals are at a greater risk for chronic disease and often present with clinical parameters of metabolic syndrome (MetS), insulin resistance, and systemic markers of chronic low-grade inflammation. It has been well established that cells of the immune system play an important role in the pathogenesis of obesity- and MetS-related chronic diseases, as evidenced by leukocyte activation and dysfunction in metabolic tissues such as adipose tissue, liver, pancreas, and the vasculature. However, recent findings have highlighted the substantial impact that obesity and MetS parameters have on immunity and pathogen defense, including the disruption of lymphoid tissue integrity; alterations in leukocyte development, phenotypes, and activity; and the coordination of innate and adaptive immune responses. These changes are associated with an overall negative impact on chronic disease progression, immunity from infection, and vaccine efficacy. This review presents an overview of the impact that obesity and MetS parameters have on immune system function.
Introduction
Obesity and metabolic syndrome are significant public health concerns because of their high global prevalence and association with an increased risk for developing chronic diseases (1–3). The prevalence of obesity has increased over the past few decades. More than one-third of adults and 17% of children and adolescents in the United States are now obese (4). Obesity has been deemed the leading cause of preventable death (5) and has become a global economic and health burden (6, 7).
Obesity is the result of a disruption of energy balance that leads to weight gain and metabolic disturbances that cause tissue stress and dysfunction (8). Clinical manifestation of these underlying disturbances often present as the parameters of metabolic syndrome (MetS),5 a condition characterized by a clustering of 3 or more of the following components: central adiposity, elevated blood glucose, plasma TGs, blood pressure, and low plasma HDL-cholesterol (2). In addition to these qualifying parameters, obesity and MetS are associated with endothelial dysfunction, atherogenic dyslipidemia, insulin resistance, and chronic low-grade inflammation (9). In line with national obesity trends in the United States, it has been estimated that ~34% of adults have MetS (10, 11). The high prevalence of MetS is significant, as classification with MetS increases an individual’s risk of cardiovascular disease and type 2 diabetes mellitus by 2- and 5-fold, respectively (2).
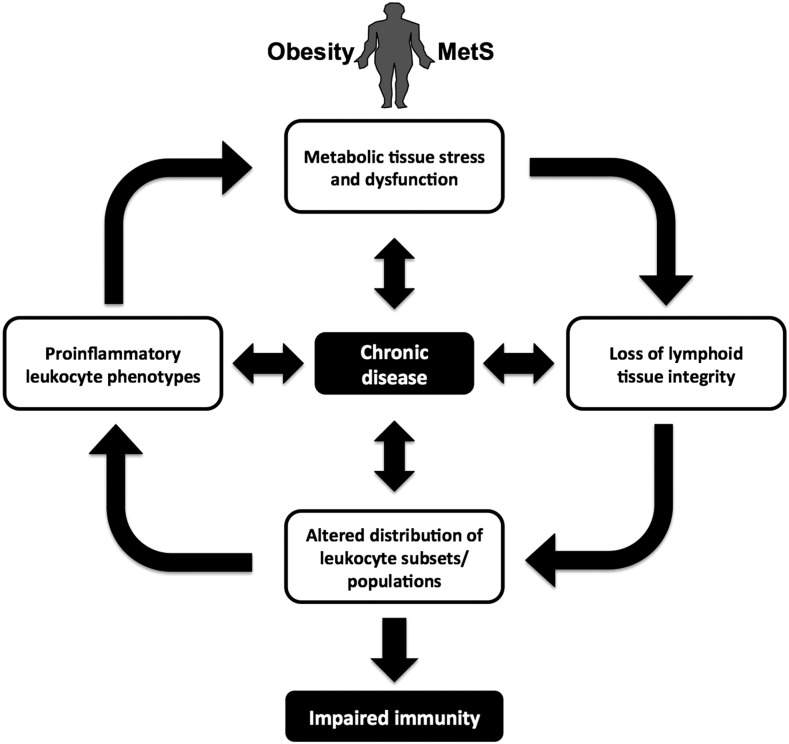
Researchers have elucidated an important role for immune cells in the physiological dysfunction associated with obesity and MetS, in addition to the pathogenesis and development of subsequent chronic diseases (8, 12). Metabolic disturbances lead to immune activation in tissues such as adipose tissue, liver, pancreas, and the vasculature, and individuals often present with elevated plasma markers of chronic low-grade inflammation (8, 13–15). In addition to immune cells playing a role in the perpetuation of chronic disease, it has further been established that obesity negatively affects immunity, as evidenced by higher rates of vaccine failure and complications from infection (16, 17). The detrimental effects of obesity on immunity are associated with alterations in lymphoid tissue architecture and integrity and shifts in leukocyte populations and inflammatory phenotypes (12, 18, 19). These effects may not only complicate and further perpetuate immune-mediated metabolic dysfunction and disease risk, but may also increase the risk for other infectious and chronic diseases (13, 17, 20, 21). An overview of the relation between obesity, metabolic syndrome, and immunity is depicted in Figure 1. Because the role of immune cells in the pathogenesis of metabolic disease has been extensively studied, this review focuses on the effects of obesity and MetS parameters on lymphoid tissues, the distribution of leukocyte subsets and phenotypes, and immunity against foreign pathogens.
FIGURE 1.
The impact of obesity and MetS on immune system function. Obesity and MetS are associated with stress and dysfunction of metabolic tissues, including adipose tissue, liver, skeletal muscle, and pancreas. Systemic physiological dysfunction that arises from obesity-related complications leads to fat accumulation in primary lymphoid organs (bone marrow and thymus), resulting in a breakdown of tissue architecture and integrity. Obesity-induced changes in lymphoid tissues are further associated with an altered distribution of leukocyte subsets and populations and greater numbers of leukocytes with proinflammatory phenotypes. Obesity-induced disruptions in the immune system impair immunity and contribute to the progression of metabolic dysfunction and chronic disease. Chronic disease can further perpetuate dysfunction throughout the immune system. MetS, metabolic syndrome.
Coordination of Innate and Adaptive Immune Responses
The immune system is made up of 2 distinct arms—the innate and adaptive immune systems. Proper function and defense conferred by these systems depends on sophisticated developmental and maturation processes in lymphoid tissues, including the bone marrow, thymus, spleen, and lymph nodes (22, 23), and the intricate coordination of innate and adaptive immune responses—from appropriately initiating immune activation to resolving inflammatory responses (24, 25).
The innate immune system is made up of cells from myeloid lineages, including monocytes, macrophages, dendritic cells, mast cells, natural killer cells, and the granulocytes: basophils, eosinophils, and neutrophils (26). The innate immune system serves as the body’s first line of defense in response to injury or pathogens. The presence of pattern recognition receptors allows for proinflammatory activation to general, nonspecific stimuli but does not allow for long-term immunological memory (24). Conversely, the adaptive immune system comprises B and T lymphocytes, which enable immunological memory after the exposure and activation by a specific antigen (27–29). The activation of adaptive immune responses depends upon critical interactions with innate immune cells that involve antigen presentation and receptor-mediated activation, resulting in the adaptive immune system having greater lag times between the time of exposure to response (24, 27, 30). The coordinated efforts of innate and adaptive immune systems allow for the targeted elimination of pathogens via proinflammatory mechanisms (24, 31).
Given the inflammatory nature of innate and adaptive immune responses, it is essential that all stages of immune activity are carefully regulated. Immune cells must be ready to respond to any potential damaging pathogenic stimuli that may be encountered throughout the lifetime while also being able to carefully distinguish between “pathogen” and “self,” thereby preventing the incidence of autoimmune disorders (27, 32). It is similarly important to ensure that inflammatory immune responses—which are typically acute in nature—undergo resolution in an effective and timely manner after the pathogenic factor is eliminated. Resolution involves suppressing inflammatory mediators, promoting tissue repair, and returning to normal, healthy tissue homeostasis (25, 33). Failure to properly restore tissue health may lead to further tissue stress and chronic inflammation, resulting in a shift in homeostatic set points to perpetuate a maladaptive state with no defined marker of resolution (34).
The shared leukocyte-mediated processes and molecular signaling that underlie acute and chronic inflammation allows for inflammatory crosstalk, which has been implicated in the pathogenesis of chronic disease and immune dysfunction (12, 35). Improper resolution of acute immune responses has been implicated in perpetuating obesity-associated inflammation and tissue dysfunction (36), whereas the dysfunctional physiological milieu of obesity and MetS has been associated with altered lymphoid tissue architecture and integrity, shifts in leukocyte populations and inflammatory phenotypes, and impaired resolution and pathogen defense (12, 18, 19, 37, 38) (Table 1). The following section presents an overview of metabolic dysfunction observed in obesity and MetS and highlights the mechanisms by which these conditions can affect the immune system.
TABLE 1.
Effects of obesity and MetS on the immune system1
| Immune system parameter | Model/condition | Effect on immune system | Reference |
| Bone marrow characteristics | Obese men and women | Bone marrow adiposity | (39) |
| Wistar rats fed HFD | ↑ Proinflammatory gene expression of bone marrow MSCs | (40) | |
| Thymus characteristics | C56BL/6 mice fed HFD | ↑ Thymic involution and adiposity | (18) |
| Diabetic rats, streptozotocin-induced | ↑ Thymic involution | (41) | |
| Diabetic mice, alloxan-induced | ↑ Thymic involution | (42) | |
| Leptin deficiency (ob/ob mice) | ↓ Thymus size and cellularity, ↑ thymocyte apoptosis | (43) | |
| Spleen characteristics | C56BL/6 mice fed HFD | ↑ Effector/memory T cell, ↓ TCR diversity | (18) |
| Lymph node characteristics | Diet-induced obese mice | ↓ Inguinal lymph node size, ↓ T cell numbers | (44) |
| Impaired lymphatic fluid transport, DC migration | (44) | ||
| Leukocyte development | Adipocyte-rich BM in C57BL/6J mice | ↓ Hematopoeisis | (45) |
| Leptin receptor deficiency (db/db mice) | ↓ Hematopoeisis | (46) | |
| Low HDL, Abca1−/− Abcg1−/− BM mice | ↓ BM HSC and myeloid progenitor proliferation | (47) | |
| C56BL/6 mice fed HFD | ↑ Myeloid progenitor cells, ↓ lymphoid progenitors | (18) | |
| ↓ Thymic output of naïve T cells | (18) | ||
| Obese and insulin resistant patients | ↓ Thymic output of naïve T cells | (18) | |
| Clinical leukocyte profiles | MetS populations | ↑ WBC counts | (48–50) |
| Healthy men, MELANY cohort | ↑ 7.6% T2DM risk for every 1000 cells/mm3 increase in WBCs | (51) | |
| Weight loss, overweight, and obese subjects | ↓ WBC counts | (52) | |
| Leukocyte inflammation | Obese mouse models | ↑ M1 macrophages, ↓ M2 macrophages in adipose | (53–55) |
| ↑ T cell infiltration in adipose | (13) | ||
| ↑ TH1 cells, ↓ Treg cells in adipose | (13, 20) | ||
| Obese human subjects | ↑CD4+ T cells, ↓ CD8+ peripheral T cells | (56) | |
| ↑ NF-κB activation in PBMCs | (19) | ||
| ↑ MIF, IL-6, TNF-α, MMP-9 mRNA expression in PBMCs | (19) | ||
| Morbidly obese human subjects | ↑ Peripheral TH2 and Treg cells | (57) | |
| ↑ CD4+ and CD8+ T cell proliferation | (57) | ||
| Weight loss, obese women | ↓ PBMC proinflammatory gene expression | (58) | |
| Weight loss, obese women | ↔ CD4+ and CD8+ ratios | (59) | |
| −/− mice | ↑ T cell lipid rafts and proliferation | (60) | |
| Pathogen defense | HDL infusion in C57BL6/CBA mice | ↑ Survival from lethal dose of LPS | (61) |
| Lipoprotein-bound LPS, septic patients | ↓ LPS bioactivity | (62) | |
| HFD-fed and ob/ob mice | ↑ Mortality from S. aureus-induced sepsis | (63) | |
| Diabetic tuberculosis patients | ↑ CD4+ TH1 and TH17 cytokines in plasma | (64) | |
| Adiponectin-deficient mice | ↑ Risk of sepsis-related mortality | (65) | |
| Immunity | Leptin deficiency (ob/ob mice) | ↓ Cell-mediated immunity | (66) |
| Diet-induced obese mice | ↓ DC antigen presentation | (67) | |
| Type 2 diabetic patients | ↓ Phagocytic activity of PBMCs | (68) | |
| Obese and diabetic mice | ↑ Lung cancer metastasis, ↓ NK cell function at early cancer stages | (69) | |
| Diet-induced obese mice | ↓ Maintenance of influenza-specific CD8+ memory T cells | (37) | |
| Obese, glucose intolerant rats | ↓ Immunological memory after hepatitis B vaccine | (70) | |
| Type 2 diabetic hemodialysis patients | ↑ Risk of hepatitis B vaccine failure | (71) | |
| Overweight children | ↑ Risk of tetanus vaccine failure | (72) | |
| Obese human subjects | ↑ Risk of influenza vaccine failure | (17) | |
| Diabetic patients | ↑ Risk of influenza-related complications and hospitalizations | (73, 74) | |
| Communities with high obesity prevalence | ↑ Risk of influenza-related hospitalizations | (74) | |
| Child obesity, NHANES 2005–2006 | ↑ Allergic disease | (75) |
Abca1−/− , ATP-binding cassette transporter A1; Abcg1−/− , ATP-binding cassette transporter G1; BM, bone marrow; DC, dendritic cell; HFD, high-fat diet; HSC, hematopoietic stem cell; MELANY, Metabolic, Life-Style and Nutrition Assessment in Young Adults; MetS, metabolic syndrome; MIF, migration inhibition factor; MMP-9, matrix metalloproteinase 9; MSC, mesenchymal stem cell; NK, natural killer; PBMC, peripheral blood mononuclear cell; T2DM, type 2 diabetes mellitus; TCR, T cell receptor; TH1, TH2, and TH17, T helper cells 1, 2, and 17, respectively; Treg, regulatory T; WBC, white blood cell; ↑, increase; ↓ decrease; ↔, no change.
Adipose Dysfunction Underlies Systemic Chronic Inflammation and Metabolic Disturbances in Obesity and MetS
Chronic inflammation is a common feature of obesity and MetS and predominantly results from metabolic tissue stress caused by weight gain and adipose tissue dysfunction (8, 14). Excess nutrient intake requires adipose tissue expansion to accommodate the increased influx of nutrients—a process that depends upon insulin-mediated energy storage (8). In adults, adipose tissue expansion occurs primarily through adipocyte hypertrophy rather than adipocyte hyperplasia, which predominates in early age (76). However, lipid-engorged, hypertrophic adipocytes are more prone to activating endoplasmic reticulum and mitochondrial stress responses, in addition to inducing shear mechanical stress on the extracellular environment. Together, these factors promote the activation of a chronic, proinflammatory state within adipose tissue (8, 77).
Persistent stress and inflammation within adipose tissue can lead to adipocyte apoptosis and the release of chemotactic mediators, resulting in inflammatory leukocyte infiltration (78). Whereas macrophages represent ~5–10% of cells in healthy adipose tissue, they can represent up to 50% of all cell types within the hypertrophic obese adipose tissue of mice and humans (79, 80), often taking on a proinflammatory phenotype (53, 81). Inflammatory leukocytes within adipose tissue further perpetuate the dysfunctional state brought on by adipocyte hypertrophy by producing resistin and IL-1β, whereas both hypertrophic adipocytes and macrophages increase the secretion of TNF-α, IL-6, and monocyte chemoattractant protein-1 (82). The degree of adipose tissue stress and inflammation can often be measured systemically in human populations. Compared with healthy controls, subjects with MetS have greater levels of inflammatory cytokines in plasma and subcutaneous adipose tissue and greater macrophage infiltration and crown-like structures (14)—a marker for apoptotic adipocytes (83).
The abundance of proinflammatory mediators in adipose tissue promotes further dysfunction related to obesity and MetS, including hyperlipidemia, hyperglycemia, and insulin resistance (9). High levels of TNF-α counteract insulin-mediated nutrient uptake by inhibiting glucose transporter type 4 translocation to the surface of skeletal muscle cells, in addition to impairing perilipin-mediated lipid droplet formation and PPAR-γ-mediated TG synthesis for free fatty acid adipocyte storage (8, 84–86). Together, these effects are associated with increased free fatty acid mobilization from adipose into the circulation, as discussed in the following paragraphs (87). Retinol-binding protein 4, an adipokine derived from hypertrophic adipocytes, is also known to impair insulin signaling by reducing phosphatidylinositol-3 kinase signaling in muscle, while concomitantly increasing hepatic gluconeogenic enzyme expression (88, 89).
Proinflammatory mediators also block the production of anti-inflammatory and insulin-sensitizing adipokines such as adiponectin (8). Adiponectin is known to inhibit sterol regulatory element-binding protein-1c-induced lipogenesis and NF-κB-mediated proinflammatory gene transcription, and promotes PPAR-α and -γ transcriptional activity to increase β-oxidation and glucose transporter type 4 translocation (90). Adipocyte-derived leptin also stimulates fatty acid oxidation; however, high circulating levels found in obesity typically indicate leptin resistance (91). Therefore, hypertrophic stress prevents adequate contribution of anti-inflammatory, antihyperlipidemic, and insulin-sensitizing adipocyte mediators.
As a consequence of hypertrophy-induced inflammation and leukocyte infiltration, the dysfunctional adipose tissue observed in obesity and MetS loses insulin sensitivity, resulting in increased lipolysis and impaired lipid storage (8). Free fatty acids and TGs are mobilized to the circulation, leading to the accumulation of lipid derivatives in the skeletal muscle, liver, and pancreatic β-cells and resulting in impaired tissue functioning and systemic insulin resistance. These underlying disturbances often present as the clinical parameters of MetS and elevated plasma levels of proinflammatory cytokines and acute-phase proteins such as C-reactive protein (14). Prolonged maintenance or worsening of this metabolically dysfunctional state further perpetuates the dysregulation of lipid metabolism and immune responses, thereby increasing an individual’s risk for developing a wide range of chronic diseases (8).
Obesity Impairs Lymphoid Tissue Architecture and Function
As described previously, the physiological dysfunction that underlies obesity leads to ectopic lipid accumulation in nonadipose tissue (8). Interestingly, this phenomenon is not restricted to metabolic tissues, as obesity has been shown to increase fat deposition in tissues of the immune system, including the bone marrow and thymus (12). These changes lead to alterations in the distribution of leukocyte populations, lymphocyte activity, and overall immune defenses (12, 18, 37, 92–95).
Throughout the human lifespan, bone marrow-derived pluripotent hematopoietic stem cells continuously replenish multipotent and committed progenitor populations, which ultimately give rise to blood cells of both lymphoid (T and B lymphocytes and natural killer cells) and myeloid (monocytes, macrophages, dendritic cells, granulocytes, erythrocytes, megakaryocytes, and mast cells) lineages (22). The generation of mature T lymphocytes requires further developmental stages in the thymus, which is considered to be a primary lymphoid organ along with bone marrow (12, 96). Mature lymphocytes then take up residence in secondary lymphoid tissues, including spleen, lymph nodes, and mucosa-associated lymphoid tissue, to perform immune surveillance and await activation in response to pathogens (97).
The integrity of immune tissue architecture is essential to proper leukocyte generation and maturation because the cells within these tissues provide critical interactions with developing leukocytes to ensure functionality (23). Interestingly, obesity has been shown to increase the adipose content of primary lymphoid tissues, thereby altering the cellular milieu by disrupting tissue integrity (12, 18). High-fat feeding has also been shown to increase the inflammatory gene expression of bone marrow mesenchymal stem cells in Wistar rats (40), which may affect hematopoietic niches and developmental environments (98). As such, adipocytes in bone marrow have been shown to suppress hematopoiesis (45). Obesity also disproportionately affects the ratios of progenitor lineages generated in bone marrow. In C57BL/6 mice, diet-induced obesity from high-fat feeding (60% of energy) has been shown to skew the ratios of leukocyte progenitor populations to increase the number of myeloid progenitor cells while reducing lymphoid progenitors (18). Interestingly, bone marrow fat content has been associated with several parameters related to obesity and MetS. For example, Bredella et al. (39) reported that bone marrow fat was positively correlated with serum TGs and inversely correlated with plasma HDL-cholesterol levels in obese men and women (39).
The accumulation of fat tissue in lymphoid organs is not a novel phenomenon, as it is known to naturally occur with age (96, 99). However, this change adversely affects immunity in older individuals (96, 100). Interestingly, caloric restriction is known to impede this process and is associated with greater immunity and a longer lifespan in various animal models, including rodents and nonhuman primates (94, 101). Therefore, obesity is thought to promote premature “aging” of the immune system (96, 99).
Obesity-induced changes in lymphoid tissue have similarly been observed in the thymus. In C57BL/6 mice, diet-induced obesity from high-fat feeding (60% of energy) resulted in alterations in thymic architecture (18), resembling the process of thymic involution that occurs with age (96). These changes included increased perithymic adiposity, loss of corticomedullary junctions, and reductions in lymphocyte precursor populations (18). Thymic tissue structure is critical for proper T cell development and maturation, as it provides key cell-cell interactions that ensure appropriate T cell receptor signaling, thereby preventing the output of dysfunctional and autoreactive T cells (23). High-fat diet-induced changes in thymic architecture were further associated with reduced thymic output of naive T cells, which may negatively affect immune surveillance (18). Interestingly, obesity and insulin resistance are associated with reduced thymic output in humans (18). Accelerated thymic involution has also been demonstrated in streptozotocin-induced diabetic rats (41) and alloxan-induced diabetic mice (42).
Obesity has also been shown to adversely affect the dynamics of secondary lymphoid tissues. In murine spleens, high-fat feeding is associated with more effector/memory T cells compared with chow-fed controls and an overall restriction in T cell receptor diversity (18). These findings suggest that obesity reduces the repertoire of circulating T cells, thus limiting the range of pathogenic antigens to which they can respond (12, 93). Obesity has also been shown to decrease inguinal lymph node size, impair lymphatic fluid transport and dendritic cell migration to peripheral lymph nodes, and reduce lymph node T lymphocyte numbers (44). Overall, obesity disrupts immune system integrity and leads to alterations in leukocyte development, migration, and diversity.
The Impact of Obesity and MetS Parameters on Leukocyte Activation and the Coordination of Immune Responses
As described previously, it is clear that physiological complications of obesity perpetuate dysfunction in the immune system, partly because of adipose deposition in primary lymphoid tissues (12, 18). However, another important element that disrupts immune function is the interaction of leukocytes with systemic markers of insulin resistance, chronic inflammation, and MetS.
Research has highlighted a growing role for HDL in modulating immune function (102). Low plasma HDL-cholesterol is among the qualifying parameters of MetS (2), indicating that the pool of HDL particles is reduced in number and/or size (103). Low HDL may have significant effects on immunity because HDL possesses various anti-inflammatory and immunoregulatory properties (104). This is because HDL serves as a carrier for a variety of oxidized lipid-neutralizing enzymes and bioactive lipid species, including paraoxonase 1, platelet-activating factor acetylhydrolase, lecithin-cholesterol acyltransferase, and sphingosine-1-phosphate (105). HDL also acts as an acceptor of leukocyte cholesterol via ATP-binding cassette transporter A1 and ATP-binding cassette transporter G1 (106, 107), which can have profound effects on leukocyte activity and proliferative capacity. Low plasma HDL can also contribute to excess accumulation of cellular cholesterol, resulting in greater lipid raft formation and responsiveness to proliferative cues, whereas elevated HDL levels have been shown to suppress proliferation of bone marrow-derived hematopoietic stem cells and myeloid progenitors (47, 60, 108, 109).
In addition to these functions, HDL may alter inflammatory responses by neutralizing LPS—an immunostimulatory glycolipid located on the outer membrane of Gram-negative bacteria that activates innate immune responses via pattern recognition receptors (110, 111). All lipoproteins are capable of binding the bioactive lipid A portion of LPS within their phospholipid-rich surfaces, thereby preventing it from interacting with receptor molecules on LPS-responsive cells (62, 112); however, LPS seems to preferentially bind to HDL in plasma (62, 113). Some studies suggest that the binding of LPS to HDL has profound effects in protecting against endotoxin-induced inflammation and shock. In C57BL6/CBA mice, Levine et al. (61) found that doubling the plasma HDL level by human apoA-I transgenic expression or infusion of reconstituted HDL resulted in a 3- to 4-fold increase in survival from a lethal dose of LPS (61). Lipoprotein-bound LPS has also been shown to lose its bioactivity in septic patients (62). The LPS-neutralizing properties of HDL may be particularly important in obesity and MetS, where blood LPS levels are often found to be elevated (114, 115). This phenomenon is likely attributable to the altered composition of microbiota in obesity, where relatively higher amounts of Gram-negative bacteria are observed, in addition to increased uptake into the circulation via chylomicron-mediated transport and abnormal gut permeability (116–119). Thus, the low levels and dysfunctional nature of HDL in obese and MetS populations may fail to effectively sequester LPS, thereby further exacerbating metabolic disease progression and immune cell activation (31, 115, 120).
Additional parameters associated with MetS have been shown to exert immunomodulatory functions, including elevated blood glucose and insulin resistance. Whereas resting T cells have low energy needs, T cell activation triggers large increases in insulin receptor expression and glucose transporter type 1-mediated glucose uptake. However, the presence of insulin resistance in obesity and MetS may suppress insulin signaling, leading to insufficient T cell activation in response to pathogens (121). Insulin resistance may inhibit T cell-mediated resolution of inflammation, as insulin has been shown to promote anti-inflammatory T helper cell 2 (TH2) differentiation (122). Conversely, excessive glucose uptake can lead to hyperactive immune responses, which have been linked to cancer and autoimmunity (121).
Adipose-derived adipokines associated with obesity and MetS have also been shown to exert effects on immune activity. Leptin is among the most well characterized of these adipokines and plays important roles in metabolism and immunity (123). Under healthy conditions, leptin acts as a satiety hormone to reduce energy intake and increase energy expenditure; however, the metabolic dysfunction that underlies obesity and MetS often leads to systemic leptin resistance (124). Leptin deficiency is associated with reduced hematopoiesis, T cell production, and impaired immunity (46, 66, 121, 125), as leptin plays a regulatory role in bone marrow hematopoiesis (46) while also exerting T cell generation and development in the thymus and determining T cell subsets in lymph nodes (43, 123).
Similar to leptin, the adipokine adiponectin has in addition been shown to affect immunity. Adiponectin has both anti-inflammatory and insulin-sensitizing properties and is often decreased in obesity and MetS (126). Whereas leptin plays a more significant role in preparing and initiating immune responses, adiponectin is essential for inflammatory resolution. Teoh et al. (65) demonstrated that adiponectin-deficient mice had an 8-fold greater risk of sepsis-related mortality than wild-type controls and that the loss of adiponectin increased endothelial activation and inflammation (65). Interestingly, elevated blood levels of adiponectin are commonly observed in patients with immune-mediated inflammatory diseases such as autoimmune disorders, pulmonary conditions, and heart failure—the mechanisms and consequences of which are unknown (127). Although this trend may be a physiological attempt to combat inflammation, these findings indicate that the role of adiponectin in immunity and inflammatory diseases requires further elucidation.
Obesity and MetS Alter Leukocyte Profiles in Peripheral Blood and Adipose Tissue
In addition to affecting immune system tissue architecture and leukocyte development, obesity and MetS alter the distribution of leukocyte subsets, their inflammatory phenotypes, and total leukocyte numbers (12). Elevation in the standard clinical white blood cell (WBC) measure has been used as a marker of leukocyte inflammation and activation, particularly within the context of MetS. According to Japanese MetS criteria, WBC counts serve as a positive predictor of MetS (48). In addition to MetS being associated with higher WBC counts in Japanese populations (49), MetS components are typically worsened in higher WBC quartiles. Similarly, in a Swedish population aged 75 y, WBC counts were found to be positively associated with parameters of MetS; however, this was more prevalent in women (50). Conversely, long-term, moderate weight loss (5.4% of body weight over 3 y) has been shown to reduce WBC counts and serum inflammatory markers (IL-1β, IL-6, and urinary isoprostanes) (52). Interestingly, in the Metabolic, Life-Style, and Nutrition Assessment in Young Adults cohort of 24,897 healthy men, WBC counts were found to be an independent risk factor for developing type 2 diabetes, with a 7.6% increase in incident type 2 diabetes for every 1000 cells/mm3 (51).
Alterations in leukocyte subsets are also observed in obesity and MetS, with implications for both chronic disease progression and immunity. Pulse-labeling studies conducted in vivo have demonstrated that the macrophages recruited into adipose tissue at the onset of obesity are highly proinflammatory, classically activated M1 macrophages. In contrast, resident macrophages in lean adipose are typically alternatively activated, anti-inflammatory M2 macrophages (53–55). Increased T cell infiltration is also observed in obese adipose tissue, and some evidence suggests that these lymphocytes may become activated in response to unique antigens generated in obese adipose tissue during high-fat feeding (13). In addition, greater levels of proinflammatory TH1 cells have been observed in obese adipose, whereas levels of anti-inflammatory regulatory T cells are reduced, corresponding to greater impairments in insulin sensitivity (13, 20). Obese patients have also been shown to have a greater frequency of CD4+ T cells and reduced CD8+ T cells (56); however, ratios of CD4+ and CD8+ T cells were not shown to change in women who underwent weight loss from gastric banding or gastric bypass (59).
Similar to what has been observed in metabolic tissues, blood leukocytes from obese subjects often reside in an elevated basal proinflammatory state. Peripheral blood mononuclear cells from obese subjects display greater NF-κB activation, as evidenced by increased p50 and p65 DNA binding compared with healthy, normal-weight control subjects. Obese subjects similarly exhibited increased mRNA expression of NF-κB target genes, including migration inhibition factor, IL-6, TNF-α, and matrix metalloproteinase 9 (19). Proinflammatory peripheral blood mononuclear cell markers can also be reduced with a 5% weight loss (58). Interestingly, a recent study (57) conducted in morbidly obese subjects found that peripheral CD4+ T cell numbers were 2-folds higher than lean controls, with greater levels of anti-inflammatory TH2 and Treg cells observed. CD4+ T cell numbers positively correlated with plasma levels of fasting insulin, IL-7, and chemokine (C-C motif) ligand 5, whereas the elevation in T cell subsets were attributed to increased T cell proliferation (57). Although the elevated leukocyte counts observed corresponds with previous studies (49, 50), these findings contradict previous reports of elevated proinflammatory T cell populations in the peripheral blood and adipose in obesity (19, 58). These findings may be indicative of an adaptive shift in the anti-inflammatory T cell set point as a means of combating dysfunction in obesity; however, it is important to note that the subjects (n = 13) were relatively healthy, in that they were nondiabetic and did not exhibit elevated levels of plasma TNF-α or IL-6 (57), as was commonly observed in obese and MetS populations (14). However, these results may also suggest that immune parameters can be differentially affected by the degree of obesity (i.e., obese compared with morbidly obese), which warrants further investigation.
Obesity Alters Immunity and Pathogen Defense
Despite having increased basal levels of inflammatory leukocytes, obesity is associated with impaired immune responses. Both high-fat diet-fed and ob/ob obese mice experience increased mortality in response to Staphylococcus aureus-induced sepsis, which corresponds with several impaired innate immune functions (63). As mentioned previously, obesity has also been associated with impaired T cell-mediated immune surveillance by promoting reductions in thymopoiesis and constricting T cell receptor diversity (18). The reduction in certain lymphocyte subsets may coincide with concomitant increases in T cells that respond to antigens unique to dysfunctional adipose and lymphocytes that favor metabolic tissue infiltration and proinflammatory responses (13, 20). These patterns are known to induce insulin resistance (13, 20), which is also associated with altered immune responses to pathogen exposure. In diabetics diagnosed with tuberculosis, ex vivo stimulation of whole blood with a Mycobacterium tuberculosis antigen increased CD4+ TH1 and TH17 cell numbers and was associated with greater levels of proinflammatory TH1 and TH17 cytokines in plasma (64).
Several studies have further demonstrated the complications of obesity after influenza exposure. Diet-induced obesity has been shown to impair memory CD8+ T cell responses to an influenza virus infection, resulting in increased mortality, viral titers in lung, and worsened lung pathology (37). These adverse effects were associated with an obesity-induced failure to maintain influenza-specific CD8+ memory T cells, which are essential in ensuring vaccine efficacy (37). Accordingly, obesity has been shown to increase the risk of vaccine failure, including the vaccines for hepatitis B (70), tetanus (72), and influenza (17). Obesity is also associated with a greater risk of influenza-related complications and hospitalizations (73, 74).
The impact of obesity on immunity further extends to other chronic conditions. In the NHANES 2005–2006 cohort, obesity was associated with an increased prevalence of allergic disease in children that was primarily driven by allergic sensitization to food (75). Individuals who are obese are also at an increased risk of developing different types of cancers, including colon, breast, liver, pancreatic, and leukemia. Obesity is also associated with poorer cancer treatment efficacy and greater cancer-related mortality (128). Given the important role of the immune system in cancer surveillance (129), it is likely that obesity-related impairments in immunity may contribute to the increased risk of developing cancer. Accordingly, it has been demonstrated that obesity and diabetes promote lung cancer metastasis in mice, corresponding to decreased natural killer cell function in early stages (69). Together, these findings suggest that obesity impairs normal immune functioning and may further perpetuate chronic disease development and metabolic disease complications.
Conclusions
The findings presented in this review highlight the significant impact that obesity and MetS have on the immune system. Obesity-induced disruptions affect the integrity of lymphoid tissues and the distribution of leukocyte subsets and phenotypes, and thus, in turn, the development of chronic diseases and immunity (12). This is a significant public health concern, as rising levels of obesity throughout the world predispose individuals to an increased risk of both metabolic and infectious diseases. As research continues to elucidate the mechanisms that underlie obesity- and MetS-related immune dysfunction, the potential for developing therapeutic lifestyle, dietary, and pharmaceutical therapies will likely expand in an effort to combat the detrimental effects of obesity on immunity.
Acknowledgments
All authors read and approved the final manuscript.
Footnotes
Abbreviations used: MetS, metabolic syndrome; TH1, 2, and 17, T helper cells 1, 2, and 17, respectively; WBC, white blood cell.
References
- 1.Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, Rimm E, Colditz GA. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med 2001;161:1581–6. [DOI] [PubMed] [Google Scholar]
- 2.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001;285:2486–97. [DOI] [PubMed] [Google Scholar]
- 3.Zimmet P, Magliano D, Matsuzawa Y, Alberti G, Shaw J. The metabolic syndrome: a global public health problem and a new definition. J Atheroscler Thromb 2005;12:295–300. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief 2012;82:1–8. [PubMed] [Google Scholar]
- 5.Jia H, Lubetkin EI. Trends in quality-adjusted life-years lost contributed by smoking and obesity. Am J Prev Med 2010;38:138–44. [DOI] [PubMed] [Google Scholar]
- 6.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab 2008;93:S9–30. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–31. [DOI] [PubMed] [Google Scholar]
- 8.Guilherme A, Virbasius JV, Puri V, Czech MP. Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol 2008;9:367–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech 2009;2:231–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Report 2009;13:1–7. [PubMed] [Google Scholar]
- 11.Aguilar M, Bhuket T, Torres S, Liu B, Wong RJ. Prevalence of the metabolic syndrome in the United States, 2003–2012. JAMA 2015;313:1973–4. [DOI] [PubMed] [Google Scholar]
- 12.Kanneganti TD, Dixit VD. Immunological complications of obesity. Nat Immunol 2012;13:707–12. [DOI] [PubMed] [Google Scholar]
- 13.Winer S, Chan Y, Paltser G, Truong D, Tsui H, Bahrami J, Dorfman R, Wang Y, Zielenski J, Mastronardi F, et al. Normalization of obesity-associated insulin resistance through immunotherapy. Nat Med 2009;15:921–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bremer AA, Jialal I. Adipose tissue dysfunction in nascent metabolic syndrome. J Obes 2013;2013:393192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bremer AA, Devaraj S, Afify A, Jialal I. Adipose tissue dysregulation in patients with metabolic syndrome. J Clin Endocrinol Metab 2011;96:E1782–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bandaru P, Rajkumar H, Nappanveettil G. The impact of obesity on immune response to infection and vaccine: an insight into plausible mechanisms. Endocrinol Metab Syndr 2013;2:2. [Google Scholar]
- 17.Sheridan PA, Paich HA, Handy J, Karlsson EA, Hudgens MG, Sammon AB, Holland LA, Weir S, Noah TL, Beck MA. Obesity is associated with impaired immune response to influenza vaccination in humans. Int J Obes (Lond) 2012;36:1072–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang H, Youm YH, Vandanmagsar B, Rood J, Kumar KG, Butler AA, Dixit VD. Obesity accelerates thymic aging. Blood 2009;114:3803–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ghanim H, Aljada A, Hofmeyer D, Syed T, Mohanty P, Dandona P. Circulating mononuclear cells in the obese are in a proinflammatory state. Circulation 2004;110:1564–71. [DOI] [PubMed] [Google Scholar]
- 20.Feuerer M, Herrero L, Cipolletta D, Naaz A, Wong J, Nayer A, Lee J, Goldfine AB, Benoist C, Shoelson S, et al. Lean, but not obese, fat is enriched for a unique population of regulatory T cells that affect metabolic parameters. Nat Med 2009;15:930–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell 2010;140:883–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iwasaki H, Akashi K. Myeloid lineage commitment from the hematopoietic stem cell. Immunity 2007;26:726–40. [DOI] [PubMed] [Google Scholar]
- 23.Takahama Y. Journey through the thymus: stromal guides for T-cell development and selection. Nat Rev Immunol 2006;6:127–35. [DOI] [PubMed] [Google Scholar]
- 24.Iwasaki A, Medzhitov R. Regulation of adaptive immunity by the innate immune system. Science 2010;327:291–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Serhan CN, Chiang N, Van Dyke TE. Resolving inflammation: dual anti-inflammatory and pro-resolution lipid mediators. Nat Rev Immunol 2008;8:349–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dranoff G. Cytokines in cancer pathogenesis and cancer therapy. Nat Rev Cancer 2004;4:11–22. [DOI] [PubMed] [Google Scholar]
- 27.Eisen HN, Chakraborty AK. Evolving concepts of specificity in immune reactions. Proc Natl Acad Sci USA 2010;107:22373–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harrington LE, Janowski KM, Oliver JR, Zajac AJ, Weaver CT. Memory CD4 T cells emerge from effector T-cell progenitors. Nature 2008;452:356–60. [DOI] [PubMed] [Google Scholar]
- 29.McHeyzer-Williams LJ, McHeyzer-Williams MG. Antigen-specific memory B cell development. Annu Rev Immunol 2005;23:487–513. [DOI] [PubMed] [Google Scholar]
- 30.Fazilleau N, McHeyzer-Williams LJ, McHeyzer-Williams MG. Local development of effector and memory T helper cells. Curr Opin Immunol 2007;19:259–67. [DOI] [PubMed] [Google Scholar]
- 31.Mogensen TH. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin Microbiol Rev 2009;22:240–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Todd DJ, Lee AH, Glimcher LH. The endoplasmic reticulum stress response in immunity and autoimmunity. Nat Rev Immunol 2008;8:663–74. [DOI] [PubMed] [Google Scholar]
- 33.Serhan CN, Savill J. Resolution of inflammation: the beginning programs the end. Nat Immunol 2005;6:1191–7. [DOI] [PubMed] [Google Scholar]
- 34.Medzhitov R. Origin and physiological roles of inflammation. Nature 2008;454:428–35. [DOI] [PubMed] [Google Scholar]
- 35.Patel PS, Buras ED, Balasubramanyam A. The role of the immune system in obesity and insulin resistance. J Obes 2013;2013:616193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rius B, Lopez-Vicario C, Gonzalez-Periz A, Moran-Salvador E, Garcia-Alonso V, Claria J, Titos E. Resolution of inflammation in obesity-induced liver disease. Front Immunol 2012;3:257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karlsson EA, Sheridan PA, Beck MA. Diet-induced obesity in mice reduces the maintenance of influenza-specific CD8+ memory T cells. J Nutr 2010;140:1691–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.White PJ, Arita M, Taguchi R, Kang JX, Marette A. Transgenic restoration of long-chain n-3 fatty acids in insulin target tissues improves resolution capacity and alleviates obesity-linked inflammation and insulin resistance in high-fat-fed mice. Diabetes 2010;59:3066–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bredella MA, Gill CM, Gerweck AV, Landa MG, Kumar V, Daley SM, Torriani M, Miller KK. Ectopic and serum lipid levels are positively associated with bone marrow fat in obesity. Radiology 2013;269:534–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cortez M, Carmo LS, Rogero MM, Borelli P, Fock RA. A high-fat diet increases IL-1, IL-6, and TNF-alpha production by increasing NF-kappaB and attenuating PPAR-gamma expression in bone marrow mesenchymal stem cells. Inflammation 2013;36:379–86. [DOI] [PubMed] [Google Scholar]
- 41.Barbu-Tudoran L, Gavriliuc OI, Paunescu V, Mic FA. Accumulation of tissue macrophages and depletion of resident macrophages in the diabetic thymus in response to hyperglycemia-induced thymocyte apoptosis. J Diabetes Complications 2013;27:114–22. [DOI] [PubMed] [Google Scholar]
- 42.Nagib PR, Gameiro J, Stivanin-Silva LG, de Arruda MS, Villa-Verde DM, Savino W, Verinaud L. Thymic microenvironmental alterations in experimentally induced diabetes. Immunobiology 2010;215:971–9. [DOI] [PubMed] [Google Scholar]
- 43.Howard JK, Lord GM, Matarese G, Vendetti S, Ghatei MA, Ritter MA, Lechler RI, Bloom SR. Leptin protects mice from starvation-induced lymphoid atrophy and increases thymic cellularity in ob/ob mice. J Clin Invest 1999;104:1051–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weitman ES, Aschen SZ, Farias-Eisner G, Albano N, Cuzzone DA, Ghanta S, Zampell JC, Thorek D, Mehrara BJ. Obesity impairs lymphatic fluid transport and dendritic cell migration to lymph nodes. PLoS One 2013;8:e70703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Naveiras O, Nardi V, Wenzel PL, Hauschka PV, Fahey F, Daley GQ. Bone-marrow adipocytes as negative regulators of the haematopoietic microenvironment. Nature 2009;460:259–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bennett BD, Solar GP, Yuan JQ, Mathias J, Thomas GR, Matthews W. A role for leptin and its cognate receptor in hematopoiesis. Curr Biol 1996;6:1170–80. [DOI] [PubMed] [Google Scholar]
- 47.Yvan-Charvet L, Pagler T, Gautier EL, Avagyan S, Siry RL, Han S, Welch CL, Wang N, Randolph GJ, Snoeck HW, et al. ATP-binding cassette transporters and HDL suppress hematopoietic stem cell proliferation. Science 2010;328:1689–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ishizaka N, Ishizaka Y, Toda E, Nagai R, Yamakado M. Association between cigarette smoking, white blood cell count, and metabolic syndrome as defined by the Japanese criteria. Intern Med 2007;46:1167–70. [DOI] [PubMed] [Google Scholar]
- 49.Oda E, Kawai R. The prevalence of metabolic syndrome and diabetes increases through the quartiles of white blood cell count in Japanese men and women. Intern Med 2009;48:1127–34. [DOI] [PubMed] [Google Scholar]
- 50.Nilsson G, Hedberg P, Jonason T, Lonnberg I, Tenerz A, Ohrvik J. White blood cell counts associate more strongly to the metabolic syndrome in 75-year-old women than in men: a population based study. Metab Syndr Relat Disord 2007;5:359–64. [DOI] [PubMed] [Google Scholar]
- 51.Twig G, Afek A, Shamiss A, Derazne E, Tzur D, Gordon B, Tirosh A. White blood cells count and incidence of type 2 diabetes in young men. Diabetes Care 2013;36:276–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chae JS, Paik JK, Kang R, Kim M, Choi Y, Lee SH, Lee JH. Mild weight loss reduces inflammatory cytokines, leukocyte count, and oxidative stress in overweight and moderately obese participants treated for 3 years with dietary modification. Nutr Res 2013;33:195–203. [DOI] [PubMed] [Google Scholar]
- 53.Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest 2007;117:175–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lumeng CN, Deyoung SM, Bodzin JL, Saltiel AR. Increased inflammatory properties of adipose tissue macrophages recruited during diet-induced obesity. Diabetes 2007;56:16–23. [DOI] [PubMed] [Google Scholar]
- 55.Nguyen MT, Favelyukis S, Nguyen AK, Reichart D, Scott PA, Jenn A, Liu-Bryan R, Glass CK, Neels JG, Olefsky JM. A subpopulation of macrophages infiltrates hypertrophic adipose tissue and is activated by free fatty acids via Toll-like receptors 2 and 4 and JNK-dependent pathways. J Biol Chem 2007;282:35279–92. [DOI] [PubMed] [Google Scholar]
- 56.O’Rourke RW, Kay T, Scholz MH, Diggs B, Jobe BA, Lewinsohn DM, Bakke AC. Alterations in T-cell subset frequency in peripheral blood in obesity. Obes Surg 2005;15:1463–8. [DOI] [PubMed] [Google Scholar]
- 57.van der Weerd K, Dik WA, Schrijver B, Schweitzer DH, Langerak AW, Drexhage HA, Kiewiet RM, van Aken MO, van Huisstede A, van Dongen JJ, et al. Morbidly obese human subjects have increased peripheral blood CD4+ T cells with skewing toward a Treg- and Th2-dominated phenotype. Diabetes 2012;61:401–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sheu WH, Chang TM, Lee WJ, Ou HC, Wu CM, Tseng LN, Lang HF, Wu CS, Wan CJ, Lee IT. Effect of weight loss on proinflammatory state of mononuclear cells in obese women. Obesity (Silver Spring) 2008;16:1033–8. [DOI] [PubMed] [Google Scholar]
- 59.Merhi ZO, Durkin HG, Feldman J, Macura J, Rodriguez C, Minkoff H. Effect of bariatric surgery on peripheral blood lymphocyte subsets in women. Surg Obes Relat Dis 2009;5:165–71. [DOI] [PubMed] [Google Scholar]
- 60.Armstrong AJ, Gebre AK, Parks JS, Hedrick CC. ATP-binding cassette transporter G1 negatively regulates thymocyte and peripheral lymphocyte proliferation. J Immunol 2010;184:173–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Levine DM, Parker TS, Donnelly TM, Walsh A, Rubin AL. In vivo protection against endotoxin by plasma high density lipoprotein. Proc Natl Acad Sci USA 1993;90:12040–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kitchens RL, Thompson PA, Munford RS, O’Keefe GE. Acute inflammation and infection maintain circulating phospholipid levels and enhance lipopolysaccharide binding to plasma lipoproteins. J Lipid Res 2003;44:2339–48. [DOI] [PubMed] [Google Scholar]
- 63.Strandberg L, Verdrengh M, Enge M, Andersson N, Amu S, Onnheim K, Benrick A, Brisslert M, Bylund J, Bokarewa M, et al. Mice chronically fed high-fat diet have increased mortality and disturbed immune response in sepsis. PLoS One 2009;4:e7605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kumar NP, Sridhar R, Banurekha VV, Jawahar MS, Nutman TB, Babu S. Expansion of pathogen-specific T-helper 1 and T-helper 17 cells in pulmonary tuberculosis with coincident type 2 diabetes mellitus. J Infect Dis 2013;208:739–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Teoh H, Quan A, Bang KW, Wang G, Lovren F, Vu V, Haitsma JJ, Szmitko PE, Al-Omran M, Wang CH, et al. Adiponectin deficiency promotes endothelial activation and profoundly exacerbates sepsis-related mortality. Am J Physiol Endocrinol Metab 2008;295:E658–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chandra RK. Cell-mediated immunity in genetically obese C57BL/6J ob/ob) mice. Am J Clin Nutr 1980;33:13–6. [DOI] [PubMed] [Google Scholar]
- 67.Smith AG, Sheridan PA, Tseng RJ, Sheridan JF, Beck MA. Selective impairment in dendritic cell function and altered antigen-specific CD8+ T-cell responses in diet-induced obese mice infected with influenza virus. Immunology 2009;126:268–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lecube A, Pachon G, Petriz J, Hernandez C, Simo R. Phagocytic activity is impaired in type 2 diabetes mellitus and increases after metabolic improvement. PLoS One 2011;6:e23366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mori A, Sakurai H, Choo MK, Obi R, Koizumi K, Yoshida C, Shimada Y, Saiki I. Severe pulmonary metastasis in obese and diabetic mice. Int J Cancer 2006;119:2760–7. [DOI] [PubMed] [Google Scholar]
- 70.Bandaru P, Rajkumar H, Nappanveettil G. Altered or impaired immune response to hepatitis B vaccine in WNIN/GR-Ob rat: an obese rat model with impaired glucose tolerance. ISRN Endocrinol 2011;2011:980105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ocak S, Eskiocak AF. The evaluation of immune responses to hepatitis B vaccination in diabetic and non-diabetic haemodialysis patients and the use of tetanus toxoid. Nephrology (Carlton) 2008;13:487–91. [DOI] [PubMed] [Google Scholar]
- 72.Eliakim A, Schwindt C, Zaldivar F, Casali P, Cooper DM. Reduced tetanus antibody titers in overweight children. Autoimmunity 2006;39:137–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Allard R, Leclerc P, Tremblay C, Tannenbaum TN. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care 2010;33:1491–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Charland KM, Buckeridge DL, Hoen AG, Berry JG, Elixhauser A, Melton F, Brownstein JS. Relationship between community prevalence of obesity and associated behavioral factors and community rates of influenza-related hospitalizations in the United States. Influenza Other Respir Viruses 2013;7:718–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Visness CM, London SJ, Daniels JL, Kaufman JS, Yeatts KB, Siega-Riz AM, Liu AH, Calatroni A, Zeldin DC. Association of obesity with IgE levels and allergy symptoms in children and adolescents: results from the National Health and Nutrition Examination Survey 2005–2006. J Allergy Clin Immunol 2009;123:1163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Naaz A, Holsberger DR, Iwamoto GA, Nelson A, Kiyokawa H, Cooke PS. Loss of cyclin-dependent kinase inhibitors produces adipocyte hyperplasia and obesity. FASEB J 2004;18:1925–7. [DOI] [PubMed] [Google Scholar]
- 77.Deng J, Liu S, Zou L, Xu C, Geng B, Xu G. Lipolysis response to endoplasmic reticulum stress in adipose cells. J Biol Chem 2012;287:6240–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sartipy P, Loskutoff DJ. Monocyte chemoattractant protein 1 in obesity and insulin resistance. Proc Natl Acad Sci USA 2003;100:7265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ferrante AW., Jr The immune cells in adipose tissue. Diabetes Obes Metab 2013;15(Suppl 3):34–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003;112:1796–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kraakman MJ, Murphy AJ, Jandeleit-Dahm K, Kammoun HL. Macrophage polarization in obesity and type 2 diabetes: weighing down our understanding of macrophage function? Front Immunol 2014;5:470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lagathu C, Yvan-Charvet L, Bastard JP, Maachi M, Quignard-Boulange A, Capeau J, Caron M. Long-term treatment with interleukin-1beta induces insulin resistance in murine and human adipocytes. Diabetologia 2006;49:2162–73. [DOI] [PubMed] [Google Scholar]
- 83.Altintas MM, Azad A, Nayer B, Contreras G, Zaias J, Faul C, Reiser J, Nayer A. Mast cells, macrophages, and crown-like structures distinguish subcutaneous from visceral fat in mice. J Lipid Res 2011;52:480–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.de Alvaro C, Teruel T, Hernandez R, Lorenzo M. Tumor necrosis factor alpha produces insulin resistance in skeletal muscle by activation of inhibitor kappaB kinase in a p38 MAPK-dependent manner. J Biol Chem 2004;279:17070–8. [DOI] [PubMed] [Google Scholar]
- 85.Grunfeld C, Gulli R, Moser AH, Gavin LA, Feingold KR. Effect of tumor necrosis factor administration in vivo on lipoprotein lipase activity in various tissues of the rat. J Lipid Res 1989;30:579–85. [PubMed] [Google Scholar]
- 86.Zhang HH, Halbleib M, Ahmad F, Manganiello VC, Greenberg AS. Tumor necrosis factor-alpha stimulates lipolysis in differentiated human adipocytes through activation of extracellular signal-related kinase and elevation of intracellular cAMP. Diabetes 2002;51:2929–35. [DOI] [PubMed] [Google Scholar]
- 87.Bézaire V, Mairal A, Anesia R, Lefort C, Langin D. Chronic TNFalpha and cAMP pre-treatment of human adipocytes alter HSL, ATGL and perilipin to regulate basal and stimulated lipolysis. FEBS Lett 2009;583:3045–9. [DOI] [PubMed] [Google Scholar]
- 88.Norseen J, Hosooka T, Hammarstedt A, Yore MM, Kant S, Aryal P, Kiernan UA, Phillips DA, Maruyama H, Kraus BJ, et al. Retinol-binding protein 4 inhibits insulin signaling in adipocytes by inducing proinflammatory cytokines in macrophages through a c-Jun N-terminal kinase- and toll-like receptor 4-dependent and retinol-independent mechanism. Mol Cell Biol 2012;32:2010–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yang Q, Graham TE, Mody N, Preitner F, Peroni OD, Zabolotny JM, Kotani K, Quadro L, Kahn BB. Serum retinol binding protein 4 contributes to insulin resistance in obesity and type 2 diabetes. Nature 2005;436:356–62. [DOI] [PubMed] [Google Scholar]
- 90.Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K. Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Invest 2006;116:1784–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Scarpace PJ, Zhang Y. Leptin resistance: a prediposing factor for diet-induced obesity. Am J Physiol Regul Integr Comp Physiol 2009;296:R493–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Strissel KJ, DeFuria J, Shaul ME, Bennett G, Greenberg AS, Obin MS. T-cell recruitment and Th1 polarization in adipose tissue during diet-induced obesity in C57BL/6 mice. Obesity (Silver Spring) 2010;18:1918–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Yang H, Youm YH, Vandanmagsar B, Ravussin A, Gimble JM, Greenway F, Stephens JM, Mynatt RL, Dixit VD. Obesity increases the production of proinflammatory mediators from adipose tissue T cells and compromises TCR repertoire diversity: implications for systemic inflammation and insulin resistance. J Immunol 2010;185:1836–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yang H, Youm YH, Dixit VD. Inhibition of thymic adipogenesis by caloric restriction is coupled with reduction in age-related thymic involution. J Immunol 2009;183:3040–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kim CS, Lee SC, Kim YM, Kim BS, Choi HS, Kawada T, Kwon BS, Yu R. Visceral fat accumulation induced by a high-fat diet causes the atrophy of mesenteric lymph nodes in obese mice. Obesity (Silver Spring) 2008;16:1261–9. [DOI] [PubMed] [Google Scholar]
- 96.Dixit VD. Impact of immune-metabolic interactions on age-related thymic demise and T cell senescence. Semin Immunol 2012;24:321–30. [DOI] [PubMed] [Google Scholar]
- 97.Ley K, Kansas GS. Selectins in T-cell recruitment to non-lymphoid tissues and sites of inflammation. Nat Rev Immunol 2004;4:325–35. [DOI] [PubMed] [Google Scholar]
- 98.Morrison SJ, Scadden DT. The bone marrow niche for haematopoietic stem cells. Nature 2014;505:327–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dixit VD. Adipose-immune interactions during obesity and caloric restriction: reciprocal mechanisms regulating immunity and health span. J Leukoc Biol 2008;84:882–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Castelo-Branco C, Soveral I. The immune system and aging: a review. Gynecol Endocrinol 2014;30:16–22. [DOI] [PubMed] [Google Scholar]
- 101.Colman RJ, Beasley TM, Kemnitz JW, Johnson SC, Weindruch R, Anderson RM. Caloric restriction reduces age-related and all-cause mortality in rhesus monkeys. Nat Commun 2014;5:3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Feingold KR, Grunfeld C. The role of HDL in innate immunity. J Lipid Res 2011;52:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mora S, Glynn RJ, Ridker PM. High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy. Circulation 2013;128:1189–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Andersen CJ, Fernandez ML. Dietary approaches to improving atheroprotective HDL functions. Food Funct 2013;4:1304–13. [DOI] [PubMed] [Google Scholar]
- 105.Kontush A, Chapman MJ. Functionally defective high-density lipoprotein: a new therapeutic target at the crossroads of dyslipidemia, inflammation, and atherosclerosis. Pharmacol Rev 2006;58:342–74. [DOI] [PubMed] [Google Scholar]
- 106.Zhao Y, Van Berkel TJ, Van Eck M. Relative roles of various efflux pathways in net cholesterol efflux from macrophage foam cells in atherosclerotic lesions. Curr Opin Lipidol 2010;21:441–53. [DOI] [PubMed] [Google Scholar]
- 107.Kellner-Weibel G, de la Llera-Moya M. Update on HDL receptors and cellular cholesterol transport. Curr Atheroscler Rep 2011;13:233–41. [DOI] [PubMed] [Google Scholar]
- 108.Hansson GK, Bjorkholm M. Medicine. Tackling two diseases with HDL. Science 2010;328:1641–2. [DOI] [PubMed] [Google Scholar]
- 109.Feldman DL, Mogelesky TC, Liptak BF, Gerrity RG. Leukocytosis in rabbits with diet-induced atherosclerosis. Arterioscler Thromb 1991;11:985–94. [DOI] [PubMed] [Google Scholar]
- 110.Park BS, Song DH, Kim HM, Choi BS, Lee H, Lee JO. The structural basis of lipopolysaccharide recognition by the TLR4-MD-2 complex. Nature 2009;458:1191–5. [DOI] [PubMed] [Google Scholar]
- 111.Soehnlein O, Lindbom L. Phagocyte partnership during the onset and resolution of inflammation. Nat Rev Immunol 2010;10:427–39. [DOI] [PubMed] [Google Scholar]
- 112.Read TE, Harris HW, Grunfeld C, Feingold KR, Calhoun MC, Kane JP, Rapp JH. Chylomicrons enhance endotoxin excretion in bile. Infect Immun 1993;61:3496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhu X, Parks JS. New roles of HDL in inflammation and hematopoiesis. Annu Rev Nutr 2012;32:161–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Creely SJ, McTernan PG, Kusminski CM, Fisher FM, Da Silva NF, Khanolkar M, Evans M, Harte AL, Kumar S. Lipopolysaccharide activates an innate immune system response in human adipose tissue in obesity and type 2 diabetes. Am J Physiol Endocrinol Metab 2007;292:E740–7. [DOI] [PubMed] [Google Scholar]
- 115.Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 2007;56:1761–72. [DOI] [PubMed] [Google Scholar]
- 116.Pedersen R, Andersen AD, Hermann-Bank ML, Stagsted J, Boye M. The effect of high-fat diet on the composition of the gut microbiota in cloned and non-cloned pigs of lean and obese phenotype. Gut Microbes 2013;4:371–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bervoets L, Van Hoorenbeeck K, Kortleven I, Van Noten C, Hens N, Vael C, Goossens H, Desager KN, Vankerckhoven V. Differences in gut microbiota composition between obese and lean children: a cross-sectional study. Gut Pathog 2013;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Delzenne NM, Neyrinck AM, Cani PD. Modulation of the gut microbiota by nutrients with prebiotic properties: consequences for host health in the context of obesity and metabolic syndrome. Microb Cell Fact 2011;10(Suppl 1):S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vreugdenhil AC, Rousseau CH, Hartung T, Greve JW, van ’t Veer C, Buurman WA. Lipopolysaccharide (LPS)-binding protein mediates LPS detoxification by chylomicrons. J Immunol 2003;170:1399–405. [DOI] [PubMed] [Google Scholar]
- 120.Hansel B, Giral P, Nobecourt E, Chantepie S, Bruckert E, Chapman MJ, Kontush A. Metabolic syndrome is associated with elevated oxidative stress and dysfunctional dense high-density lipoprotein particles displaying impaired antioxidative activity. J Clin Endocrinol Metab 2004;89:4963–71. [DOI] [PubMed] [Google Scholar]
- 121.Maciver NJ, Jacobs SR, Wieman HL, Wofford JA, Coloff JL, Rathmell JC. Glucose metabolism in lymphocytes is a regulated process with significant effects on immune cell function and survival. J Leukoc Biol 2008;84:949–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Viardot A, Grey ST, Mackay F, Chisholm D. Potential antiinflammatory role of insulin via the preferential polarization of effector T cells toward a T helper 2 phenotype. Endocrinology 2007;148:346–53. [DOI] [PubMed] [Google Scholar]
- 123.La Cava A, Matarese G. The weight of leptin in immunity. Nat Rev Immunol 2004;4:371–9. [DOI] [PubMed] [Google Scholar]
- 124.Yang R, Barouch LA. Leptin signaling and obesity: cardiovascular consequences. Circ Res 2007;101:545–59. [DOI] [PubMed] [Google Scholar]
- 125.Farooqi IS, Matarese G, Lord GM, Keogh JM, Lawrence E, Agwu C, Sanna V, Jebb SA, Perna F, Fontana S, et al. Beneficial effects of leptin on obesity, T cell hyporesponsiveness, and neuroendocrine/metabolic dysfunction of human congenital leptin deficiency. J Clin Invest 2002;110:1093–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ouchi N, Walsh K. Adiponectin as an anti-inflammatory factor. Clin Chim Acta 2007;380:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Fantuzzi G. Adiponectin in inflammatory and immune-mediated diseases. Cytokine 2013;64:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Vucenik I, Stains JP. Obesity and cancer risk: evidence, mechanisms, and recommendations. Ann N Y Acad Sci 2012;1271:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Gajewski TF, Schreiber H, Fu YX. Innate and adaptive immune cells in the tumor microenvironment. Nat Immunol 2013;14:1014–22. [DOI] [PMC free article] [PubMed] [Google Scholar]