Abstract
Background:
To evaluate whether serotonin (5-HT), 5-HT2A receptor (5-HT2AR), and 5-HT transporter (serotonin transporter [SERT]) are associated with different disease states of depression, myocardial infarction (MI) and MI co-exist with depression in Sprague-Dawley rats.
Methods:
After established the animal model of four groups include control, depression, MI and MI with depression, we measured 5-HT, 5-HT2AR and SERT from serum and platelet lysate.
Results:
The serum concentration of 5-HT in depression rats decreased significantly compared with the control group (303.25 ± 9.99 vs. 352.98 ± 13.73; P = 0.000), while that in MI group increased (381.78 ± 14.17 vs. 352.98 ± 13.73; P = 0.000). However, the depression + MI group had no change compared with control group (360.62 ± 11.40 vs. 352.98 ± 13.73; P = 0.036). The changes of the platelet concentration of 5-HT in the depression, MI, and depression + MI group were different from that of serum. The levels of 5-HT in above three groups were lower than that in the control group (380.40 ± 17.90, 387.75 ± 22.28, 246.40 ± 18.99 vs. 500.29 ± 20.91; P = 0.000). The platelet lysate concentration of 5-HT2AR increased in depression group, MI group, and depression + MI group compared with the control group (370.75 ± 14.75, 393.47 ± 15.73, 446.66 ± 18.86 vs. 273.66 ± 16.90; P = 0.000). The serum and platelet concentration of SERT in the depression group, MI group and depression + MI group were all increased compared with the control group (527.51 ± 28.32, 602.02 ± 23.32, 734.76 ± 29.59 vs. 490.56 ± 16.90; P = 0.047, P = 0.000, P = 0.000 in each and 906.38 ± 51.84, 897.33 ± 60.34, 1030.17 ± 58.73 vs. 708.62 ± 51.15; P = 0.000 in each).
Conclusions:
The concentration of 5-HT2AR in platelet lysate and SERT in serum and platelet may be involved in the pathway of MI with depression. Further studies should examine whether elevated 5-HT2AR and SERT may contribute to the biomarker in MI patients with depression.
Keywords: 5-HT, 5-HT2A Receptor, Depression, Myocardial Infarction, Serotonin Transporter
INTRODUCTION
Major depression and coronary heart disease (CHD) are two most global burden diseases worldwide. The co-occurrence of these two disorders is common and associated with substantially increased morbidity and mortality. Recent epidemiological research has shown that major depression and CHD each independently increase risk for the other disorder. Although many plausible explanations have been proposed, the biological mechanisms linking depression and CHD remain unclear. Dysregulation of peripheral serotonin, common to both depression and CHD, may contribute to this association. Because of serotonin's dual effects promoting platelet aggregation and arterial vasoconstriction, serotoninergic signaling pathways are important in the etiology and pathogenesis of both major depression and vascular thrombosis.[1]
Serotonin is a vasoactive substance found in the brain, gut, and blood platelets. Alteration of the serotonin system associated with depressive disorders includes increased platelet aggregation, alteration in platelet serotonin uptake, decreased platelet serotonin transporter [SERT] sites, and increases in platelet serotonin binding density. In cardiac system, it exerts diverse cardio-physiologic effects, with 5-HT1 receptor mediating vasodilation and the 5-HT2 receptor mediating vasoconstriction.
All the 5-HT played an important role in the state of depression[2] and acute coronary syndrome occurring during the process of development; one of the common disease mechanisms is platelet 5-HT and 5-HT receptor. However, there is no evidence to show which biological marker can be used to screen the co-occurrence of acute coronary syndrome and depression. So our study aimed to observe the changes of platelet 5-HT, 5-HT2A receptor (5-HT2AR) and SERT level in different disease states, which include normal, acute myocardial infarction (MI), depression, acute MI with depression.
METHODS
Animal model
Control group
Sprague-Dawley (SD) adult male rats (250 g n = 6).
Depression group: The forced swim test
Sprague-Dawley adult male rats (250 g n = 6) were submitted to a modified forced swim test (FST) similar to described by Porsolt et al.,[3] except that the water was deeper. Briefly, each animal was placed in a cylinder (40 cm height, 20 cm diameter) containing 30 cm water maintained at 25°C. The modified FST with 30 cm water depth was used in order to avoid false immobility due to the capability of adult rats to rest on their tail touching the bottom of the cylinder when the lower volume, that is, 15 cm in the FST described by Porsolt et al., is used.
After a pretest session of 15 cm, the rats were dried (under a warm air current), and 24 h later exposed again to the FST for 5 min, as described above.
Myocardial infarction group: Myocardial infarction animal model
According to surgical model of MI, the SD rats were anesthetized with ketamine (40 mg/kg) and xylazine (1 mg/kg) by intramuscular application, and then conduct surgical model of MI according to Akbay et al. previous described.[4]
Depression + myocardial infarction group: Depression with myocardial infarction animal model
After recovered from MI surgery, the SD rat conducted FST.
Experiment material and regent preparation
Instruments and materials: Microplate reader capable of measuring absorbance at 450 nm, micropipette, pipette tips, distilled water or deionized water, filter paper
×30 wash solution: Dilute with distilled or deionized water 1:30.
Sample collection and storage
The blood samples were collected from the tail vein and placed into chilled tubes containing ethylenediaminetetraacetic acid. Whole blood was aliquoted and stored at −70°C until time of assay. The blood was centrifuged within 30 min for 15 min at 200 ×g at room temperature to obtain platelet-rich plasma (PRP) as described previously.[5] Successively, PRP was aspirated and sonicated with three cycles of 10s on ice. In order to prepare isolated platelets, PRP was centrifuged for 10 min at 2100 ×g at 4°C, and then prepared according to Rao et al.[5]
ELISA method to detect 5-HT, 5-HT2A receptor, and serotonin transporter content
According to the instruction of ELISA kits of 5-HT, 5-HT2AR and SERT.
Statistical analysis
Differences in characteristics between different groups were compared using tests for a continuous variable.
RESULTS
Table 1 indicates the concentration of 5-HT, 5-HT2AR, and SERT in serum and platelet lysate in different groups (control group, depression group, MI group, depression + MI group). The serum concentration of 5-HT in depression rats decreased significantly compared with the control group (303.25 ± 9.99 vs. 352.98 ± 13.73), there were significant differences (P = 0.000), while in MI group increased (381.78 ± 14.17 vs. 352.98 ± 13.73; P = 0.000). However, the depression + MI group had no change compared with control group (360.62 ± 11.40 vs. 352.98 ± 13.73; P = 0.036), had significant changes compared with depression group and MI group (P = 0.000, P = 0.009).
Table 1.
Concentration of 5-HT, 5-HT2AR, and SERT in serum and platelet lysate in different group (control group, depression group, MI group, depression + MI group)
| Groups | n | Mean ± SD | P |
|---|---|---|---|
| Serum 5-HT | |||
| Control | 6 | 352.98 ± 13.73 | 0.000* |
| Depression | 6 | 303.25 ± 9.99 | |
| MI | 6 | 381.78 ± 14.17 | 0.001* |
| 0.000† | |||
| Depression + MI | 6 | 360.62 ± 11.40 | 0.326* |
| 0.000† | |||
| 0.009‡ | |||
| Platelet 5-HT | |||
| Control | 6 | 500.29 ± 20.91 | 0.000* |
| Depression | 6 | 380.40 ± 17.90 | |
| MI | 6 | 387.75 ± 22.28 | 0.000* |
| 0.571† | |||
| Depression+MI | 6 | 246.40 ± 18.99 | 0.000* |
| 0.000† | |||
| 0.000‡ | |||
| Platelet 5-HT2AR | |||
| Control | 6 | 273.66 ± 16.90 | 0.000* |
| Depression | 6 | 370.75 ± 14.75 | |
| MI | 6 | 393.47 ± 15.73 | 0.000* |
| 0.037† | |||
| Depression+MI | 6 | 446.66 ± 18.86 | 0.000* |
| 0.000† | |||
| 0.000‡ | |||
| Serum SERT | |||
| Control | 6 | 490.56 ± 28.50 | 0.047* |
| Depression | 6 | 527.51 ± 28.32 | |
| MI | 6 | 602.02 ± 23.32 | 0.000* |
| 0.000† | |||
| Depression + MI | 6 | 734.76 ± 29.59 | 0.000* |
| 0.000† | |||
| 0.000‡ | |||
| Platelet SERT | |||
| Control | 6 | 708.62 ± 51.15 | 0.000* |
| Depression | 6 | 906.38 ± 51.84 | |
| MI | 6 | 897.33 ± 60.34 | 0.000* |
| 0.773† | |||
| Depression + MI | 6 | 1030.17 ± 58.73 | 0.000* |
| 0.001† | |||
| 0.001‡ |
*Contrast to control group; †Contrast to depression group; ‡Contrast to MI group. MI: Myocardial infarction; SD: Standard deviation; SERT: Serotonin transporter; 5-HT2AR: 5-HT2A receptor.
The platelet lysate concentration of 5-HT in the depression group, MI group, and depression + MI group were lower than that in the control group (380.40 ± 17.90, 387.75 ± 22.28, 246.40 ± 18.99 vs. 500.29 ± 20.91), and all had significant difference (P = 0.000). There was no significant difference between depression group and MI group (387.75 ± 22.28 vs. 380.40± +17.90; P = 0.571), but two groups had significant difference compared to depression + MI group (380.40 ± 17.90, 387.75 ± 22.28 vs. 246.40 ± 18.99; P = 0.000) [Figure 1].
Figure 1.
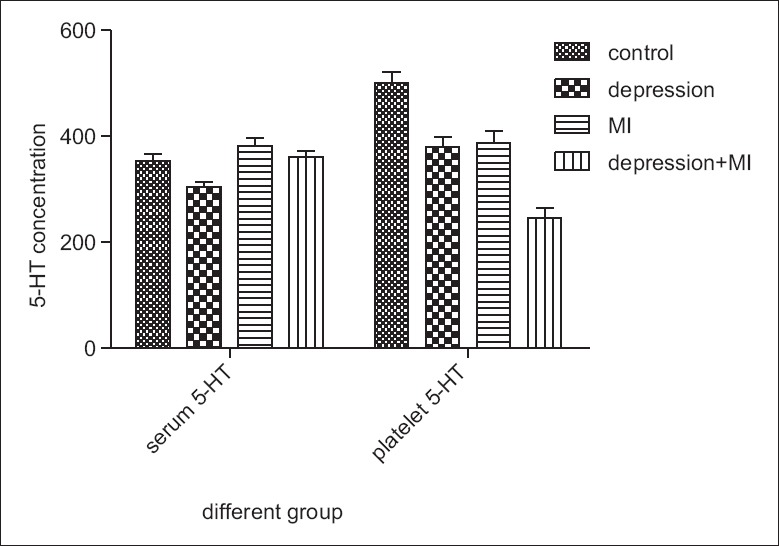
Concentration of 5-HT in serum and platelet lysate.
The platelet lysate concentration of 5-HT2AR increased in depression group, MI group and depression + MI group compared with the control group (370.75 ± 14.75, 393.47 ± 15.73, 446.66 ± 18.86 vs. 273.66 ± 16.90), and all had significant difference (P = 0.000). There is significant difference between the MI group and depression group (393.47 ± 15.73 vs. 370.75 ± 14.75; P = 0.037), Concentration in depression + MI group increased compared with depression group and the MI group, there was statistical difference (446.66 ± 18.86 vs. 370.75 ± 14.75, 393.47 ± 15.73; P = 0.000) [Figure 2].
Figure 2.
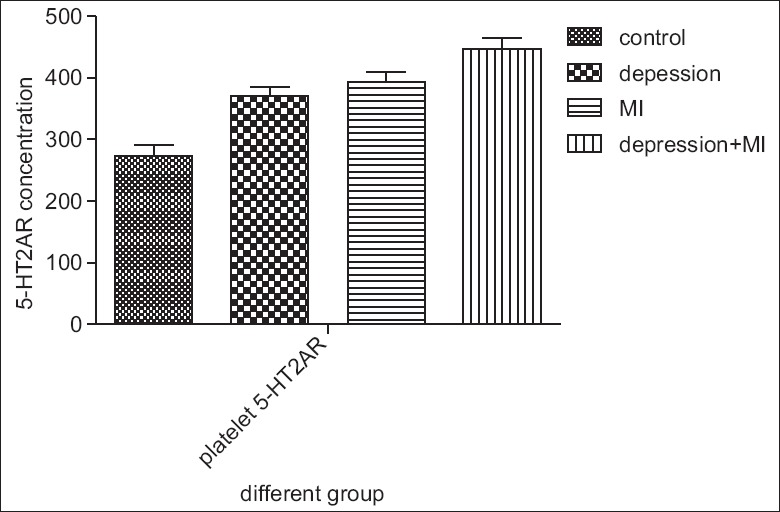
Concentration of 5-HT2A receptor in platelet lysate.
The serum concentration of SERT in the depression group, MI group and depression + MI group were increased compared with the control group (527.51 ± 28.32, 602.02 ± 23.32, 734.76 ± 29.59 vs. 490.56 ± 16.90), and had obvious statistical difference (P = 0.047, P = 0.000, P = 0.000). The SERT concentration in MI group increased compared with depression group, there was statistical difference (602.02 ± 23.32 vs. 527.51 ± 28.32; P = 0.000). The SERT concentration in depression + MI group increased than that of depression group and MI group, there were statistical differences (734.76 ± 29.59 vs. 527.51 ± 28.32, 602.02 ± 23.32; P = 0.000) [Figure 3].
Figure 3.
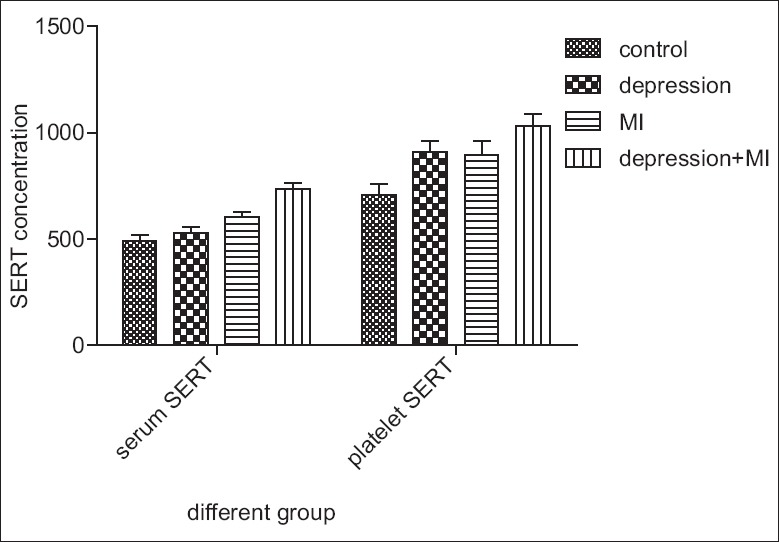
Concentration of serotonin transporter in serum and platelet lysate.
The platelet lysate concentration of SERT in the depression group, MI group, and depression + MI group was increased compared with the control group (906.38 ± 51.84, 897.33 ± 60.34, 1030.17 ± 58.73 vs. 708.62 ± 51.15), and had obvious statistical difference (P = 0.000). There were no changes between MI group and depression group (897.33 ± 60.34, vs. 906.38 ± 51.84; P = 0.773). The concentration in depression + MI group increased compared with depression group and the MI group, there were significant differences (1030.17 ± 58.73 vs. and 906.38 ± 51.84, 897.33 ± 60.34; P = 0.001, P = 0.001) [Figure 3].
DISCUSSION
In order to evaluate whether depression is associated with whole blood serotonin (WBS) in outpatients with stable CHD. The data from the Heart and Soul study showed that in the sample of patients with stable CHD, current major depression was independently associated with high mean WBS levels.[6]
Schins et al. also reported the association of depression with elevated WBS in a small case-control study of 25 depressed and 21 nondepressed MI patients.[7] Vikenes et al. reported that high levels WBS were significantly associated with CHD in an angiography sample, particularly in younger age groups.[8] However, it should be noted that there were some inconsistent results of the studies that have demonstrated an association of depression with lower peripheral serotonin levels,[9] which consistent to our study. Our study showed that concentration of peripheral 5-HT decrease in depression group, increase in MI group and no change in depression + MI group. Part reasons of the inconsistent results dependent on the method of animal model.
However, many of these studies measured serum or plasma serotonin, and because most serotonin is in platelets, the extent of which WBS correlated with serum or plasma serotonin is unclear. Our animal study also showed the different change of serotonin in plasma and platelet in different groups. And all of the above studies came from patients.
Low levels of central serotonin have been related to the state of depression, and 5-HT is the major target of newer antidepressant drugs, such as selective serotonin re-uptake inhibitors. Neurons and platelets display structural and functional similarities, so that the latter have been proposed as a peripheral model of central functions. In particular, in blood more than 99% of 5-HT is contained in platelet, so that one could consider changes in 5-HT levels in platelets as a mirror of changes in central 5-HT.[10]
The availability of 5-HT is strictly limited by a selective, active re-uptake mechanism performed by a specific protein, the 5-HT transporter (SERT), which plays the significant role of terminating the activity of the neurotransmitter. Besides of the central nervous system, the SERT has been found in intestinal epithelial cells, in blood platelet and blood lymphocytes. The involvement of SERT in clinical depression and anxiety has received enormous attention from discovery of the significance of SERT polymorphisms on human behavior.[11] SERT on platelets is the primary mechanism for 5-HT uptake from blood plasma. Therefore, the regulation of the transporter's activity represents a key mechanism to stabilize the concentration of plasma 5-HT. Specially, in platelets, plasma membrane SERT levels and platelet 5-HT uptake initially rise as plasma 5-HT levels are increased but then fall below normal as the plasma 5-HT level continues to rise. Therefore, we propose that elevated plasma 5-HT limits its own uptake in platelets down-regulating SERT as well as modifying the characteristics of SERT partners in the membrane trafficking pathway.[12]
Increased 5-HT2AR density has been reported in depressed patients.[13] Patients with depressive disorder show signs of hyperactive platelet 5-HT2AR signal transduction system as measured by increased platelet calcium mobilization after stimulation of platelets with serotonin.[14] The 5-HT2AR is linked to the platelet phosphoinositide-signaling system and is responsible for activating 5-HT-mediated platelet aggregation. Because there is direct correlation between the number of platelet 5-HT2ARs and the magnitude of the aggregation response to 5-HT, the increase in 5-HT-mediated platelet reactivity may be a consequence of 5-HT2AR up-regulation. This is supported by several studies indicating that depression is associated with an up-regulation of platelet 5-HTA receptor, and an increased response of the platelet phosphoinositide-signaling system to 5-HT. Our study showed that up-regulation of 5-HT2ARs in depression group, MI group, as well as in co-occurrence group. The MI comorbidity with depression rats had a higher level of 5-HT2AR.
There are many conflicting results from different studies, such as increased serotonin response, increased platelet serotonin receptor density, decreased SERT binding, and decreased platelet serotonin levels in individuals with depression. While the studies to date are not definitive, and the mechanisms responsible unknown, the observation of increased platelet 5-HT2AR and platelet and serum SERT in MI with depression SD rats is a remarkably consistent observation. Thus, measurement of platelet 5-HT2AR and SERT may provide a “window to the brain” and potentially provide a useful, easily available laboratory marker to aid in the diagnosis of depression in MI.
In addition to platelet serotonin specific pathways, other platelet pathways that shown significant changes in depressed individuals include blunting the platelet adenosine response, increased platelet thrombin response, as well as decreased platelet brain-derived neurotrophic factor.[15,16] Hence, the direction of future research in platelet functional changes in depression and CHD[17,18] showed continuous to focus on serotonin specific pathways with emphasis on potential mechanisms of specific pathway changes.
Footnotes
Edited by: Yi Cui
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Olivier B. Serotonin: A never-ending story. Eur J Pharmacol. 2015;753:2–18. doi: 10.1016/j.ejphar.2014.10.031. [DOI] [PubMed] [Google Scholar]
- 2.Jacobsen JP, Medvedev IO, Caron MG. The 5-HT deficiency theory of depression: Perspectives from a naturalistic 5-HT deficiency model, the tryptophan hydroxylase 2Arg439His knockin mouse. Philos Trans R Soc Lond B Biol Sci. 2012;367:2444–59. doi: 10.1098/rstb.2012.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porsolt RD, Le Pichon M, Jalfre M. Depression: A new animal model sensitive to antidepressant treatments. Nature. 1977;266:730–2. doi: 10.1038/266730a0. [DOI] [PubMed] [Google Scholar]
- 4.Akbay E, Onur MA. A new modified myocardial infarction animal model. J Cardiovasc Surg. 2013;1:69–71. [Google Scholar]
- 5.Rao ML, Hawellek B, Papassotiropoulos A, Deister A, Frahnert C. Upregulation of the platelet Serotonin2A receptor and low blood serotonin in suicidal psychiatric patients. Neuropsychobiology. 1998;38:84–9. doi: 10.1159/000026522. [DOI] [PubMed] [Google Scholar]
- 6.Wulsin LR, Musselman D, Otte C, Bruce E, Ali S, Whooley MA. Depression and whole blood serotonin in patients with coronary heart disease from the Heart and Soul Study. Psychosom Med. 2009;71:260–5. doi: 10.1097/PSY.0b013e31819cc761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schins A, Hamulyák K, Scharpé S, Lousberg R, Van Melle J, Crijns H, et al. Whole blood serotonin and platelet activation in depressed post-myocardial infarction patients. Life Sci. 2004;76:637–50. doi: 10.1016/j.lfs.2004.04.060. [DOI] [PubMed] [Google Scholar]
- 8.Vikenes K, Farstad M, Nordrehaug JE. Serotonin is associated with coronary artery disease and cardiac events. Circulation. 1999;100:483–9. doi: 10.1161/01.cir.100.5.483. [DOI] [PubMed] [Google Scholar]
- 9.Cleare AJ. Reduced whole blood serotonin in major depression. Depress Anxiety. 1997;5:108–11. doi: 10.1002/(sici)1520-6394(1997)5:2<108::aid-da8>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 10.Bianchi M, Moser C, Lazzarini C, Vecchiato E, Crespi F. Forced swimming test and fluoxetine treatment: In vivo evidence that peripheral 5-HT in rat platelet-rich plasma mirrors cerebral extracellular 5-HT levels, whilst 5-HT in isolated platelets mirrors neuronal 5-HT changes. Exp Brain Res. 2002;143:191–7. doi: 10.1007/s00221-001-0979-3. [DOI] [PubMed] [Google Scholar]
- 11.Murphy DL, Fox MA, Timpano KR, Moya PR, Ren-Patterson R, Andrews AM, et al. How the serotonin story is being rewritten by new gene-based discoveries principally related to SLC6A4, the serotonin transporter gene, which functions to influence all cellular serotonin systems. Neuropharmacology. 2008;55:932–60. doi: 10.1016/j.neuropharm.2008.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mercado CP, Kilic F. Molecular mechanisms of SERT in platelets: Regulation of plasma serotonin levels. Mol Interv. 2010;10:231–41. doi: 10.1124/mi.10.4.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shelton RC, Sanders-Bush E, Manier DH, Lewis DA. Elevated 5-HT 2A receptors in postmortem prefrontal cortex in major depression is associated with reduced activity of protein kinase A. Neuroscience. 2009;158:1406–15. doi: 10.1016/j.neuroscience.2008.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schins A, Honig A, Crijns H, Baur L, Hamulyák K. Increased coronary events in depressed cardiovascular patients: 5-HT2A receptor as missing link? Psychosom Med. 2003;65:729–37. doi: 10.1097/01.psy.0000088596.42029.10. [DOI] [PubMed] [Google Scholar]
- 15.Williams MS. Platelets and depression in cardiovascular disease: A brief review of the current literature. World J Psychiatry. 2012;2:114–23. doi: 10.5498/wjp.v2.i6.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pleis JR, Ward BW, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2009. Vital Health Stat 10. 2010;249:1–207. [PubMed] [Google Scholar]
- 17.Chen H. Possible role of platelet GluR1 receptors in comorbid depression and cardiovascular disease. Cardiovasc Psychiatry Neurol. 2009;2009:424728. doi: 10.1155/2009/424728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Canan F, Dikici S, Kutlucan A, Celbek G, Coskun H, Gungor A, et al. Association of mean platelet volume with DSM-IV major depression in a large community-based population: The MELEN study. J Psychiatr Res. 2012;46:298–302. doi: 10.1016/j.jpsychires.2011.11.016. [DOI] [PubMed] [Google Scholar]


