INTRODUCTION
Resistant hypertension has become a challenge in the treatment of hypertension. As the population continues to age and obesity, sleep apnea hypopnea syndrome, and chronic kidney disease increase in incidence, resistant hypertension has become an increasingly common issue in clinical practice. Failure to control blood pressure can impair target organs such as the heart, brain, and kidney, facilitating the occurrence of clinical cardiovascular events. Therefore, positive and effective blood pressure control is an important part of the treatment of hypertension. Many factors may negatively affect blood pressure control, including unhealthy lifestyles, poor patient compliance, inadequate or substandard medication, and secondary hypertension. Effective diagnosis and rational medication are important in the control of resistant hypertension. The recent introduction of interventional treatment has provided a new opportunity to treat resistant hypertension. This article generalizes the clinical characteristics and diagnosis and evaluation methods of resistant hypertension as well as the therapeutic strategy for obtaining optimal control of blood pressure. By summarizing the current knowledge on resistant hypertension, we stress the importance of accurate diagnosis and treatment of resistant hypertension to further prevent, improve, and standardize the treatment of hypertension in China.
DEFINITION OF RESISTANT HYPERTENSION
Resistant hypertension is defined as blood pressure that cannot be effectively controlled by lifestyle changes and the concurrent administration of a rational, tolerable, and full dose of three or more types of antihypertensive drugs (including a diuretic) for more than 1-month or that can only be effectively controlled after the concurrent administration of four or more types of antihypertensive drugs.[1,2,3]
EPIDEMIOLOGY AND MORBIDITY OF RESISTANT HYPERTENSION
Since accurate epidemiological data on resistant hypertension cannot be obtained, the morbidity of resistant hypertension remains unclear. However, the ratios of patients whose blood pressure was uncontrolled in recent clinical trials are available for reference. When the ASCOT(Anglo-Scandinavian Cardiac Outcomes Trial–Blood Pressure Lowering Arm) ended, the blood pressure of 47% of patients was uncontrolled (blood pressure of patients with diabetes: ≥130/80 mmHg; blood pressure of patients without diabetes: ≥140/90 mmHg).[4] When the ACCOMPLISH (Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension) trial ended, the blood pressure of 26% of patients was uncontrolled (blood pressure of patients with or without diabetes: ≥140/90 mmHg).[5] Subjects enrolled in these two trials were patients with hypertension at high risk of cardiovascular disease. In these patients, the ratio of resistant hypertension may be relatively high. According to the scientific statement of the American Heart Association on the diagnosis, evaluation, and treatment of resistant hypertension in 2008, a small sample study showed that the morbidity rate of patients with resistant hypertension in general outpatient clinics was approximately 5%.[1]
CAUSES AND PATHOPHYSIOLOGICAL MECHANISMS OF RESISTANT HYPERTENSION
Causes and pathophysiological mechanisms of resistant hypertension vary and include basic as well as central and local neurohumoral mechanisms. A high salt intake, obesity, and a reduced carotid baroreflex are the basic causes of uncontrolled blood pressure of patients with hypertension. In addition, due to activation of the renin-angiotensin-aldosterone system (RAAS) in the circulation and tissues and the excessively elevated activity of the sympathetic nerves in the central or local tissues (especially the kidney), inflammatory factors and oxidative stress are triggered, which facilitates the development and progress of arteriosclerosis and atherosclerosis as well as aggravates abnormalities in vascular structure and function. Thus, increased blood pressure is difficult to control. The persistently increased activity of the sympathetic nerves and RAAS is one of the factors in the pathogenesis of resistant hypertension.[6] Clinical and experimental data also show that multiple factors affect the activation of RAAS and the sympathetic nerves, including insulin resistance, adipocytokines, endothelial dysfunction, intermittent hypoxemia, volume overload, the effect of aldosterone on the central nervous system, and dysfunction of the arterial chemoreceptors and baroreceptors.
The kidney plays an important role in the pathogenesis of resistant hypertension. Locally excessive activation of the renal sympathetic nerves is the basic cause and one of the important pathophysiological mechanisms of resistant hypertension. Renal sympathetic nerves include afferent and efferent fibers. Excessive activation of afferent fibers of the renal sympathetic nerves can enhance the activity of central sympathetic nervous system, which makes the systemic sympathetic nerves highly active and increases epinephrine release. Thus, structural and functional changes occur in the target organs including the kidneys, heart, and blood vessels. Finally, hypertension is persistent and progressive. Overexcitation of the efferent fibers of the renal sympathetic nerves can induce the excessive generation and secretion of noradrenaline, which causes renal vasoconstriction, reduces renal blood flow, and activates the renal and systemic RAAS. Furthermore, contractions of the afferent glomerular arterioles are stronger than those of the efferent glomerular arterioles, which decreases the estimated glomerular filtration rate (eGFR) and increases water and sodium reabsorption. Meanwhile, stimulated granular cells release renin, which additionally activates RAAS. The pathophysiological procedure described above aggravates the blood pressure elevation and is involved in the persistence and progression of resistant hypertension.[7,8,9]
DIAGNOSTIC METHODS OF RESISTANT HYPERTENSION
Blood pressure measurement as a primary diagnostic method
Based on the office blood pressure measurement (OBPM), the use of a continuous home blood pressure measurement (HBPM) and 24-h ambulatory blood pressure monitoring (ABPM) is recommended to eliminate the white coat effect and understand the special forms of blood pressure (dipper type, nondipper type, extreme dipper type, morning surge, and morning hypertension).[10]
Identify the causes of poor blood pressure control and eliminate pseudo resistant hypertension
Incorrect blood pressure measurement: A common cause of pseudo-resistant hypertension. For example, diastolic pressure may be elevated when the patient has no back support while systolic pressure may be elevated with the legs crossed.
Treatment compliance: Check whether the patient continues to take medicine according to the doctor's advice.
Other medications: Check whether the patient is taking the medicines that may affect blood pressure.
Lifestyle factors: High salt intake, over-anxiety, heavy smoking, severe obesity, chronic pain, etc.
Treatment efficacy: Whether the use of anti-hypertensive drugs is not adequate (inadequate dose, lack of a diuretic, incorrect drug combination).
Secondary hypertension causes: Seek clues for causes of secondary hypertension.
IDENTIFICATION OF SECONDARY HYPERTENSION IN RESISTANT HYPERTENSION
With the recent deeper recognition of hypertensive causes and improvement of clinical diagnosis techniques, the diagnostic rate of secondary hypertension is significantly increased. Secondary hypertension generally features a high or uncontrolled blood pressure despite a combination of multiple anti-hypertensive drugs. However, with an etiotropic treatment, blood pressure can be controlled or even returned to normal. Therefore, identifying secondary hypertension and giving corresponding treatment are steps used to control resistant hypertension. For all patients with resistant hypertension, potential secondary hypertension should be screened for by medical history, symptoms, signs, and routine laboratory examinations.
-
Common types of secondary hypertension in resistant hypertension include: (1) Sleep apnea syndrome; (2) primary aldosteronism; (3) renal parenchymal hypertension; (4) renovascular hypertension; and (5) pheochromocytoma.
Uncontrolled hypertension caused by mental factors should also be considered.
Basic examinations commonly used in the identification of secondary hypertension include: Blood routine examination, urine routine examination, examinations of blood electrolytes, serum creatinine, blood glucose, 24-h urine sodium (Na) and potassium (K), and cardiac ultrasound, renal ultrasound; recording of height and weight, calculation of body mass index, and calculation of eGFR based on the Modification of Diet in Renal Disease formula.
For patients with suspected secondary hypertension, special examinations should be further performed to avoid missed and incorrect diagnoses. However, excessive examinations should also be avoided.
Special examinations mainly include: Renal artery ultrasound and computed tomography (CT); adrenal gland CT, determination of plasma aldosterone/renin and its ratio, and an aldosterone suppression or stimulation test; determination of blood and urine catecholamine levels as well as iodine131 – metaiodobenzylguanidine scintigraphic tracer; cortisol rhythm and dexamethasone suppression test; polysomnography; and psychological evaluation of patient when necessary.
Special examinations should be performed according to the specific clinical manifestation of patients with hypertension and the basic clues provided by related laboratory examinations. These tests should be conducted around the suspected causes to prevent blind screening for secondary hypertension. For secondary hypertension with a clear cause, drugs, devices, and surgical treatment should be used to improve the effectiveness and cure rate of anti-hypertensive therapy. Diagnosing the cause is very important in the selection of a therapeutic strategy and determining the prognosis of patients with secondary hypertension.
TREATMENT OF RESISTANT HYPERTENSION
Therapeutic life change
Corrective measures mainly include: Losing weight;[11,12] moderate alcohol intake defined as no more than 2 cups/day for most men (no more than 300 ml of red wine, approximately 600 ml of beer) and half of that volume for women or underweight individuals;[13] limiting salt, defined as limiting recommended salt intake <6 g/d;[14,15,16] eating a high-fiber and low-fat diet;[17] increasing physical activities consisting of aerobic exercise at a 50% maximal oxygen uptake for at least 30 min each day and being active as much as possible each week.[18,19] Meanwhile, patients should pay attention to their mental regulation, reduce their mental stress, and keep psychological balance.
Medication
Principles
In addition to therapeutic life change, the rational use of anti-hypertensive drugs should be considered. The drug selection process includes discontinuation of blood pressure–affecting drugs and the correct use of diuretics. A rational drug combination (including a single-pill stationary combination) is also necessary to achieve the maximum anti-hypertensive efficacy with minimal side effects. A long-acting preparation, for 24-h continuous anti-hypertensive efficacy should be used to effectively control nighttime blood pressure, morning blood pressure surge, and morning hypertension. Moreover, individually based principles should be observed, and applicable anti-hypertensive drugs should be used according to patients’ specific conditions and tolerance.
Methods
The combination use of three or more drugs with different antihypertensive mechanisms is required. A long-acting or fixed compound preparation should also be selected to reduce the dosing frequency and the number of pills. Whenever possible, the total daily drug amount should be divided into one or two doses (morning and night dose) to ensure all-day blood pressure control. Drugs that may affect anti-hypertensive efficacy should be avoided or reduced to a minimum, including nonnarcotic analgesics, nonsteroidal anti-inflammatory drugs (including aspirin), selective cyclooxygenase-2 inhibitor, sympathomimetic amines (decongestants, diet pills [sibutramine hydrochloride], cocaine), stimulants (methylphenidate, dexamphetamine, amphetamine, methamphetamine, modafinil), high alcohol intake, oral contraceptives, glucocorticoid, cyclosporine, erythropoietin, natural licorice, Chinese medicinal ingredients (ephedrine).
Selection
For patients with high renin and high sympathetic nerve activity (basic judgment criteria of heart rate and plasma renin activity), renin-angiotensin system inhibitor (RASI, angiotensin II receptor blocker [ARB] or angiotensin-converting enzyme inhibitor [ACEI]), and β-receptor blocker should be mainly used as treatment. For patients with an increased volume (basic judgment criteria of high salt diet, elderly person in Northern China, or natriuresis over 24 h) and poor circulating renin-angiotensin system (RAS) level, a calcium channel blocker (CCB) and diuretic should usually be administered. Additionally, for those with a high salt intake, the dosage of thiazide be appropriately increased while a strict salt limit is emphasized. For patients with an eGFR ≤30 mg·min-1·1.73 m-2, a loop diuretic should be used. For nondialysis patients with renal insufficiency, due to the limited usage or dosage of RASIs, the CCB dosage should be increased, and a dihydropyridine and a nondihydropyridine CCB can even be combined. For obese patients, the dosage of RASIs should be increased.[20] For elderly patients or those with an elevated systolic pressure, the CCB dosage should be increased.
The most commonly used three-drug combination consisted of RASI, CCB, and thiazide diuretic are recommended. If the target blood pressure still cannot be achieved, additional spironolactone (risk assessment on kidney function and potential hyperkalemia is required), or combination with a β-receptor blocker, an α-β receptor blocker, or an α-receptor blocker can be considered. When the blood pressure remains uncontrolled, central nervous system depressants (clonidine, reserpine, etc.) can be selected as the fifth anti-hypertensive drug in the drug combination regimen.
Anti-hypertensive drug use principles
The three-drug combination of RASI (ARB or ACEI), CCB, and thiazide diuretic should be used as the basic medication for resistant hypertension. This combination is rational in principle and useful for the treatment of most patients with hypertension. If the blood pressure remains uncontrolled after this treatment, combination of other anti-hypertensive drugs (including a β-receptor blocker, an α-β receptor blocker, or an α-receptor blocker plus an aldosterone antagonist) can also be used according to the clinical characteristics of the individual patient. The procedure of medication is shown in Figure 1.
In the three-drug combination, drug dosage should be conventional or double the tolerated dose.
For the selection of a multi-drug combination, the one with efficacy overlapping, few adverse reactions, and high compliance should be recommended under the direction of experienced specialist physicians.
Figure 1.
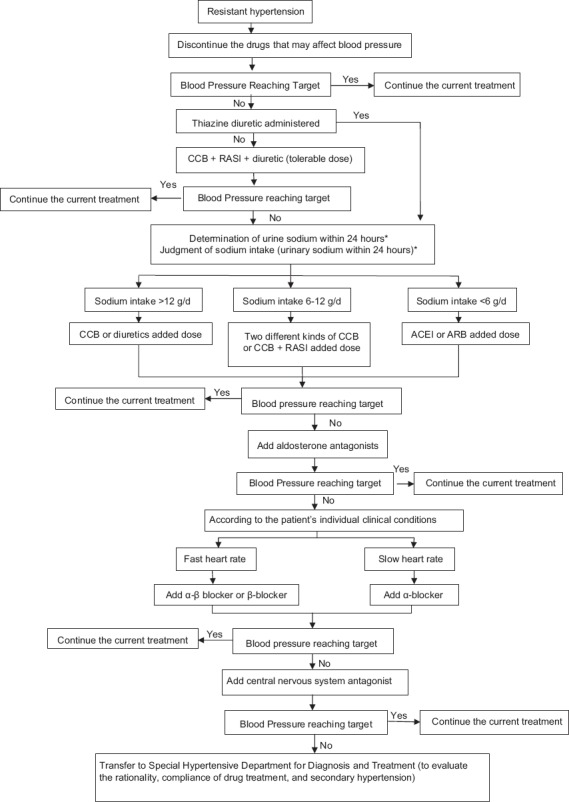
Medication for resistant hypertension. *Blood pressure target: <140/90 mmHg. CCB: Calcium channel blocker; RASI: Renin-angiotensin system inhibitor; ARB: Angiotensin II receptor blocker; ACEI: Angiotensin-converting enzyme inhibitor.
Evaluation of treatment compliance
During the drug adjustment period, a follow-up visit should occur every 2–4 weeks. Get to know the drug type(s), dosage, and dosing frequency and time by talking with the patient and family member(s). Calculate the patient's compliance according to the prescribed dosage of each time and the medication frequency. Listening to the patient's complaints and adjusting the regimen accordingly is an effective way to improve treatment compliance. Monitoring heart rate (for those taking a β-receptor blocker), blood pressure changes upon standing (for those taking an α-receptor blocker), or changes in serum uric acid and potassium (for those taking a diuretic) is another way to determine the patient's treatment compliance.
Drug therapeutic effect and safety evaluation
In addition to OBPM, HBPM, and ABPM should be combined to evaluate the anti-hypertensive efficacy. According to the dosing frequency and time, determine HBPM frequency and time. Patients with significant blood pressure fluctuations should be advised to take and record their blood pressures before taking medicine in the morning, afternoon, evening, and before going to bed and take the records with them to doctor visits. If OBPM is not consistent with HBPM or the blood pressure fluctuations are significant, it becomes necessary to determine the nighttime and all-day blood pressure stabilities; in such cases, a 24–48 h ABPM is recommended.
Learn about the patient's discomfort, especially postural dizziness and amaurosis, as well as their drug tolerance and adverse reactions. For patients with impaired renal function who are treated with RASI, an aldosterone antagonist, or a combination treatment with a loop diuretic, serum potassium, and serum creatinine must be regularly monitored and the eGFR should be calculated.
Invasive interventional therapy
Since the cardiovascular risk for patients with resistant hypertension increases significantly, blood pressure control has been an important part and target in treatment. After the standard and rational intensive treatment intervention for patients with resistant hypertension, blood pressure control remains unsatisfactory in some patients. In recent years, as a model of interventional treatment, renal denervation (RDN) has gradually attracted worldwide attention with the promise of the development of a novel therapy for patients with resistant hypertension that is poorly controlled with drugs.
Since excessive activation of the renal sympathetic nerve has been an important pathological and physiological basis of hypertension onset and maintenance and renal sympathetic nerve fibers mainly access the kidneys through the renal artery adventitia, such anatomical characteristics determine that RDN could selectively denervate most of the renal sympathetic nerve fibers. Energy is released through the radiofrequency catheter inserted into the renal artery, and through the inner medium membranes of the renal artery and a portion of the renal sympathetic nerve fibers is selectively destroyed, which reduces renal sympathetic nerve activity.[21]
Several recent small sample prospective studies (Symplicity HTN-1, Symplicity HTN-2, etc.)[22,23,24] showed that after RDN therapy, most patients with resistant hypertension responded to the treatment in the short- and medium-term (defined as a decrease in systolic blood pressure in OBPM ≥10 mmHg after therapy) without evident procedural complications, after which the antihypertensive drugs doses were somewhat reduced (however, some of the patients were still in need of multi-antihypertensive drugs to control their blood pressure). This method may possibly have some efficacy for conditions involving excessive sympathetic nerve activation such as insulin resistance, sleep apnea syndrome, ventricular arrhythmia, and chronic kidney disease. However, in the Symplicity HTN-3 trial, no significant decrease in blood pressure was observed after RDN therapy.[25] It remains necessary to carry out targeted research in the larger scale and perform longer-term follow-up visits to determine RDN effectiveness and safety. For those patients with true resistant hypertension confirmed by a clinical diagnosis, who could not tolerate multiple antihypertensive drug combination treatment, or with hypertension and poor compliance, after a strict evaluation, RDN implantation with patient consent could be considered.[26]
CLINICAL ADVICE FOR RESISTANT HYPERTENSION
For the determination of blood pressure level in patients with resistant hypertension, OBPM should be used in combination with HBPM and 24-h ABPM. Accordingly, patients whose blood pressure level remains above the target level after combination treatment with more than three kinds of medicines (including a diuretic) at optimal doses and formulations for at least 1-month could be diagnosed with resistant hypertension.
For patients with resistant hypertension, the rationality and compliance of anti-hypertensive medicine treatment should be assessed, and the primary and secondary factors resulting in the poor control of blood pressure should also been screened and identified to enable the detection of true resistant hypertension. For patients with resistant hypertension and impairment of multiple organs and the co-existence of various diseases such as diabetes, heart failure, coronary heart disease, cerebral apoplexy, and chronic kidney diseases, it is necessary to comprehensively intervene multiple risk factors and more actively control the blood pressure.
While medicines are taken to control blood pressure, it is necessary to adhere to the intensified lifestyle treatment, mainly including limiting salt, performing aerobic exercise, quitting smoking, and losing weight.
Use the optimized drug combination (CCB + RASI + diuretic) and the optimal tolerable doses for treatment. Accordingly, if the blood pressure still fails to be controlled at the target level, aldosterone antagonists (renal function permitting) or a β-blocker, an α-β blocker, or an α-blocker and central nervous system antagonists could be further applied according to the patient's individual clinical conditions.
With the instructions from professional hypertensive physicians and their diagnosis and treatment, for those patients diagnosed with resistant hypertension and poor drug control, or those with resistant hypertension who are incapable of tolerating more than four kinds of medicines for treatment (very poor treatment compliance) and are at high cardiovascular risk, on the basis of sufficient informed consent, RDN treatment may be considered. However, since RDN remains in the research stage and long-term follow-up visit data are still lacking in China, it is necessary to cautiously, discreetly, and strictly observe the operation procedures before carrying out RDN treatment. Figure 2 shows the procedure of diagnosis and treatment.
Figure 2.
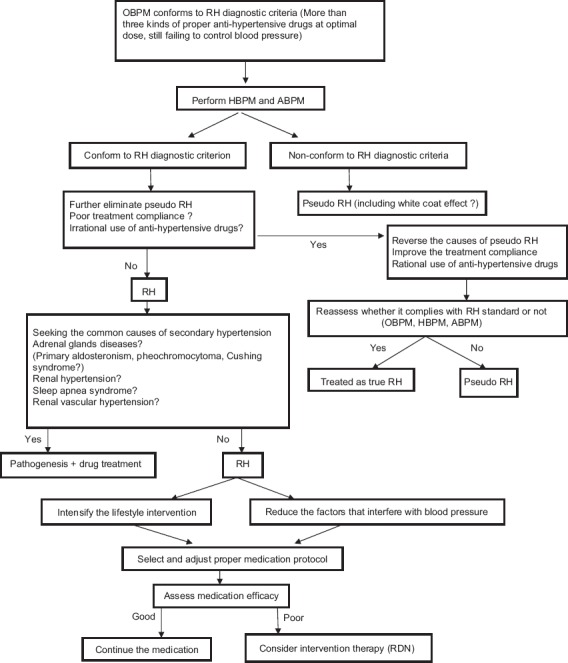
Diagnosis and treatment of resistant hypertension. HBPM: Home blood pressure measurement; ABPM: Ambulatory blood pressure monitoring; OBPM: Office blood pressure measurement; RDN: Renal denervation.
CONCLUSIONS
Resistant hypertension is a hypertensive phenomenon that results in the progression of cardiovascular and cerebrovascular diseases. Definite diagnosis and effective treatment are of the utmost importance. However, it is necessary to carefully discriminate the pathogenesis, among which, insufficient and irrational drug treatment doses, improper drug application time, a harmful lifestyle, and poor treatment compliance, etc., are all important factors. Secondary hypertension would also lead to uncontrolled blood pressure. ABPM and HBPM are crucial to clearly defining the blood pressure levels of patients with resistant hypertension. Therefore, they should serve as important diagnostic methods. Strict lifestyle interventions could improve blood pressure while rational, optimal multi-drug combinations (including a diuretic) at tolerable doses is the key to controlling blood pressure. In the combination, the application of diuretic, spironolactone, and an α-β blocker as well as a central nervous system antagonist could not be ignored. For patients with true resistant hypertension that is unresponsive to drugs, interventional RDN is a possible treatment method. However, since it remains in the research stage, it is necessary to strictly select indications for and discreetly and sequentially perform the operation according to standard protocols. Planned prospective studies are also encouraged.
Consensus Specialists
Li-Sheng Liu, Hai-Yan Wang, Run-Lin Gao, Lu-Yuan Chen, Ji-Yan Chen, Yun-Dai Chen, Ping-Jin Gao, Jun-Bo Ge, Yong Huo, Xiong-Jing Jiang, Hong-Wei Li, Nan-Fang Li, Xue-Wang Li, Yong Li, Cheng-Zhi Lu, Jian-Jun Mu, Yi-Pu Chen, Ning-Ling Sun, Jun Tao, Ji-Guang Wang, Jian-An Wang, Wei-Min Wang, Wen Wang, Yu Wang, Hai-Ying Wu, Zhao-Su Wu, Liang-Di Xie, Xiao-Wei Yan, Chun-Yu Zeng, Shu-Yang Zhang, Yu-Qing Zhang, Lian-You Zhao, Zhi-Ming Zhu, Yang Xi, Wei Ma
Footnotes
Edited by: Xin Chen
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: Diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–19. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 2.Liu LS. Writing Group of Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension (in Chinese) Chin J Cardio. 2011;39:579–615. [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 4.Dahlöf B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): A multicentre randomised controlled trial. Lancet. 2005;366:895–906. doi: 10.1016/S0140-6736(05)67185-1. [DOI] [PubMed] [Google Scholar]
- 5.Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359:2417–28. doi: 10.1056/NEJMoa0806182. [DOI] [PubMed] [Google Scholar]
- 6.Tsioufis C, Kordalis A, Flessas D, Anastasopoulos I, Tsiachris D, Papademetriou V, et al. Pathophysiology of resistant hypertension: The role of sympathetic nervous system. Int J Hypertens. 2011;2011:642416. doi: 10.4061/2011/642416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barajas L, Liu L, Powers K. Anatomy of the renal innervation: Intrarenal aspects and ganglia of origin. Can J Physiol Pharmacol. 1992;70:735–49. doi: 10.1139/y92-098. [DOI] [PubMed] [Google Scholar]
- 8.Hering D, Mahfoud F, Walton AS, Krum H, Lambert GW, Lambert EA, et al. Renal denervation in moderate to severe CKD. J Am Soc Nephrol. 2012;23:1250–7. doi: 10.1681/ASN.2011111062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laurent S, Schlaich M, Esler M. New drugs, procedures, and devices for hypertension. Lancet. 2012;380:591–600. doi: 10.1016/S0140-6736(12)60825-3. [DOI] [PubMed] [Google Scholar]
- 10.Writing Group of Chinese guidelines for the blood pressure measuring. Chinese guidelines for the blood pressure measuring. Chin J Hypertens. 2011;19:1101–15. [Google Scholar]
- 11.Aucott L, Poobalan A, Smith WC, Avenell A, Jung R, Broom J. Effects of weight loss in overweight/obese individuals and long-term hypertension outcomes: A systematic review. Hypertension. 2005;45:1035–41. doi: 10.1161/01.HYP.0000165680.59733.d4. [DOI] [PubMed] [Google Scholar]
- 12.Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: A meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 13.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 14.He FJ, Markandu ND, MacGregor GA. Modest salt reduction lowers blood pressure in isolated systolic hypertension and combined hypertension. Hypertension. 2005;46:66–70. doi: 10.1161/01.HYP.0000171474.84969.7a. [DOI] [PubMed] [Google Scholar]
- 15.Vollmer WM, Sacks FM, Ard J, Appel LJ, Bray GA, Simons-Morton DG, et al. Effects of diet and sodium intake on blood pressure: Subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001;135:1019–28. doi: 10.7326/0003-4819-135-12-200112180-00005. [DOI] [PubMed] [Google Scholar]
- 16.Singer DR, Markandu ND, Sugden AL, Miller MA, MacGregor GA. Sodium restriction in hypertensive patients treated with a converting enzyme inhibitor and a thiazide. Hypertension. 1991;17:798–803. doi: 10.1161/01.hyp.17.6.798. [DOI] [PubMed] [Google Scholar]
- 17.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 18.Kokkinos PF, Narayan P, Colleran JA, Pittaras A, Notargiacomo A, Reda D, et al. Effects of regular exercise on blood pressure and left ventricular hypertrophy in African-American men with severe hypertension. N Engl J Med. 1995;333:1462–7. doi: 10.1056/NEJM199511303332204. [DOI] [PubMed] [Google Scholar]
- 19.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: A meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 20.Jordan J, Yumuk V, Schlaich M, Nilsson PM, Zahorska-Markiewicz B, Grassi G, et al. Joint statement of the European Association for the Study of Obesity and the European Society of Hypertension: Obesity and difficult to treat arterial hypertension. J Hypertens. 2012;30:1047–55. doi: 10.1097/HJH.0b013e3283537347. [DOI] [PubMed] [Google Scholar]
- 21.DiBona GF, Esler M. Translational medicine: The antihypertensive effect of renal denervation. Am J Physiol Regul Integr Comp Physiol. 2010;298:R245–53. doi: 10.1152/ajpregu.00647.2009. [DOI] [PubMed] [Google Scholar]
- 22.Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, et al. Catheter-based renal sympathetic denervation for resistant hypertension: A multicentre safety and proof-of-principle cohort study. Lancet. 2009;373:1275–81. doi: 10.1016/S0140-6736(09)60566-3. [DOI] [PubMed] [Google Scholar]
- 23.Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: Durability of blood pressure reduction out to 24 months. Hypertension. 2011;57:911–7. doi: 10.1161/HYPERTENSIONAHA.110.163014. [DOI] [PubMed] [Google Scholar]
- 24.Symplicity HTN- Investigators. Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): A randomised controlled trial. Lancet. 2010;376:1903–9. doi: 10.1016/S0140-6736(10)62039-9. [DOI] [PubMed] [Google Scholar]
- 25.Bakris GL, Townsend RR, Liu M, Cohen SA, D’Agostino R, Flack JM, et al. Impact of renal denervation on 24-hour ambulatory blood pressure: Results from SYMPLICITY HTN-3. J Am Coll Cardiol. 2014;64:1071–8. doi: 10.1016/j.jacc.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 26.Schmieder RE, Redon J, Grassi G, Kjeldsen SE, Mancia G, Narkiewicz K, et al. ESH position paper: Renal denervation – An interventional therapy of resistant hypertension. J Hypertens. 2012;30:837–41. doi: 10.1097/HJH.0b013e328352ce78. [DOI] [PubMed] [Google Scholar]


