Abstract
Background:
In this prospective randomized study, we compared the predicted blood and effect-site C50 for propofol and remifentanil target-controlled infusion (TCI) and the bispectral index (BIS) values at loss of consciousness (LOC) and response to a standard noxious painful stimulus (LOS) in elderly and young patients, respectively. We hypothesized that the elderly patients will require lower target concentration of both propofol and remifentanil at above two clinical end-points.
Methods:
There were 80 American Society of Anesthesiologists (ASA) physical status I–II unpremedicated patients enrolled in this study, they were divided into elderly group (age ≥65 years, n = 40) and young group (aged 18–64 years, n = 40). Propofol was initially given to a predicted blood concentration of 1.2 μg/ml and thereafter increased by 0.3 μg/ml every 30 s until Observer's Assessment of Alertness and Sedation score was 1. The propofol level was kept constant, and remifentanil was given to provide a predict blood concentration of 2.0 ng/ml, and then increased by 0.3 ng/ml every 30 s until loss of response to a tetanic stimulus. BIS (version 3.22, BIS Quattro sensor) was also recorded.
Results:
In elderly group, the propofol effect-site C50 at LOC of was 1.5 (1.4–1.6) μg/ml, was significantly lower than that of young group, which was 2.2 (2.1–2.3) μg/ml, the remifentanil effect-site C50 at LOS was 3.5 (3.3–3.7) ng/ml in elderly patients, was similar with 3.7 (3.6–3.8) ng/ml in young patients. Fifty percent of patients lost consciousness at a BIS value of 57.3 (56.4–58.1), was similar with that of young group, which was 55.2 (54.0–56.3).
Conclusion:
In elderly patients, the predicted blood and effect-site concentrations of propofol at LOC were lower than that of young patients. At same sedation status, predicted blood and effect-site concentrations of remifentanil required at LOS were similar in elderly and young patients. BIS were not affected by age. Low-propofol/high-opioid may be optional TCI strategy for elderly patients.
Keywords: Bispectral Index, Painful Stimulus, Propofol-remifentanil, Target-controlled Infusion
INTRODUCTION
Intravenous anesthesia with propofol, especially target-controlled infusion (TCI) systems are commonly used in clinical practice and became widely used in elderly patients. There were many investigations about pharmocodynamic or pharmacokinetic data of propofol and remifentanil in adult, healthy Caucasians and as well as Chinese patients. However, there is few published pharmocodynamic data of propofol and remifentanil through repeatable standard noxious stimulus method by TCI in elderly patients. Therefore, we designed this prospective clinical study to compare the predicted effect-site concentration of propofol at loss of consciousness (LOC) and predicted effect remifentanil concentration required for no response to a standard noxious painful stimulus in elderly and young patients, further to quantify this concentration difference to modify the optimal application of such technique in elderly people.
METHODS
Ethical approval for this study (Ethical Committee No. ChiECRCT-20140044) was provided by the Chinese Ethics Committee of Registering Clinical Trials.
Eighty patients were enrolled. They were divided into two groups: Young (18–64 years, n = 40) and elderly (≥65, n = 40). Exclusion criteria included recent administration of sedative or opioid drugs, body weight <80% of >120% of ideal weight, age <18 years, and impairment of cardiac, respiratory, hepatic or renal function, known allergy to propofol or its lipid emulsion, general anesthesia 7 days before surgery, history of mental disorders, and American Society of Anesthesiologists (ASA) physical status Ш or over. After the insertion of a 20G venous canula, patients received Ringer's lactate solution 10 ml/kg. Bispectral index (BIS) was monitored with a BIS XP (A-2000, Aspect Medical System, USA, software version 3.22, BIS Quattro sensor). Noninvasive arterial blood pressure, SpO2, electrocardiogram, and tidal volume were monitored routinely.
A TCI of propofol (Diprivan 1% AstraZeneca Corp., with a prefilled syringe) was administered using the Diprifusor™ (Software version 2.0, Graseby 3500 Syringe Pump, Smiths Medical, Watford, UK), which uses the Marsh pharmacokinetic model. Remifentanil was administered using a microcomputer-controlled pump (SLGO High-tech Development Co., Beijing, China), which uses the Minto pharmacokinetic model. These systems display both the predicted blood concentration and the effect-site concentration. The propofol infusion was started so as to provide a blood concentration of 1.2 μg/ml and increase by 0.3 μg/ml every 30 s until the Observer's Assessment of Alertness and Sedation was 1, that is, no response. This point was defined as LOC. BIS and predicted blood and effect-site propofol concentrations were recorded at this point. This predicted blood propofol concentration was kept stable for 3 min and then remifentanil TCI begun. The predicted blood remifentanil concentration was started at 2.0 ng/ml and increased by 0.3 ng/ml every 30 s until no purposeful movement was observed after a tetanic stimulus (50 Hz, 80 mA, 0.25 ms pulses for 4 s), which was applied to the wrist using a peripheral nerve stimulator. Twisting or jerking the head was considered a purposeful movement, but twitching or grimacing was not. This point was defined as “no response to a painful stimulus.” BIS and remifentanil concentrations were recorded, and thereafter surgery proceeded as per normal. The protocol was same in both young and elderly group.
Data are expressed as mean ± standard deviation (SD). SPSS 13.0 (IBM Corp., New York, USA) statistical software was used to perform statistical analysis. P < 0.05 was considered as statistically significant. One-way analysis of variance and two-sample t-test were used to compare values at baseline, LOC, loss of response to a stimulus (LOS) after testing continuous data (heart rate [HR], mean arterial blood pressure [MAP], and SpO2) for normality. A quantal response model (probit analysis) was used to calculate C05, C50 and C95 (concentrations associated with 5%, 50% and 95% probabilities, respectively) at each end-point based on predicted blood and effect-site concentrations of the two drugs. An identical method was applied to calculate C05, C50 and C95 at each end-point of BIS.
RESULTS
The mean age was 70 ± 4 years in elderly patients and 42 ± 9 years in young patients. Their characteristics are shown in Table 1. In both age groups, HR and MAP decreased during the infusion of propofol and decreased sharply during the infusion of remifentanil, the changes were obviously in elderly group, and were significantly more than that in young group [Table 2]. Induction of anesthesia was carried out smoothly in all patients.
Table 1.
Patients characteristics
| Variables | Young patients | Elderly patients |
|---|---|---|
| Weight, kg | 42 (9) | 70 (4)* |
| Male/female, n | 19/33 | 25/27 |
| Height, cm | 164 (7) | 164 (8) |
Data are mean (SD). Young group: n=40. Elderly group: n=40. *Compared with young patients t=2.601, P<0.05. SD: Standard deviation.
Table 2.
Cardiovascular response
| Variables | Group | Baseline | LOC | LOS |
|---|---|---|---|---|
| HR, bpm | Young | 79.7 (12.8) | 73.4 (8.8)* | 60.8 (8.4)† |
| Elderly | 81.4 (13.1) | 63.4 (9.2)‡ | 64.0 (7.3)¦ | |
| MAP, mmHg | Young | 99.8 (14.3) | 78.7 (11.5)|| | 71.9 (11.3)¶ |
| Elderly | 107.4 (13.9)** | 89.9 (12.3)†† | 77.2 (11.6)‡‡ |
Data are mean (SD). Young group: n=40. Elderly group: n=40. *Compared with baseline t=0.930, P=0.000; †Compared with baseline t=4.580, P=0.000. Compared with LOC P=0.000; ‡Compared with baseline t=3.590, P=0.000. Compared with young group t=2.708, P=0.01; §Compared with baseline t=3.780, P=0.000. Compared with LOC t=2.801, P=0.007; ||Compared with baseline t=3.790, P=0.000; ¶Compared with baseline t=3.601, P=0.000. Compared with LOC t=3.621, P=0.000; **Compared with young group t=2.610, P=0.018; ††Compared with the point of baseling t=3.801, P=0.000. Compared with young group t=4.503, P=0.000; ‡‡Compared with baseline t=5.302, P=0.000. Compared with LOC t=3.680, P=0.000. Compared with young group t=3.351, P=0.043. LOC: Loss of consciousness; LOS: Loss of response to titanic stimulus; HR: Heart rate; MAP: Mean arterial blood pressure; SD: Standard deviation.
Most patients had respiratory depression before they lost response to a painful stimulus. A facemask was used to deliver oxygen to all patients.
C50 of propofol was lower in elderly patients at LOC
The effect-site propofol concentrations associated with a 50% probability of LOC was 1.5 (1.4–1.6) μg/ml in elderly patients, was significantly lower than 2.2 (2.1–2.3) μg/ml in young patients [Table 3 and Figure 1]. The effect-site propofol concentrations associated with 5% and 95% probability of LOC were 1.0 (0.9–1.1) and 2.0 (1.9–2.1) μg/ml in elderly patients, 1.6 (1.4–1.7) and 2.9 (2.7–3.3) μg/ml in young patients, respectively [Table 3].
Table 3.
Propofol concentrations at LOC
| Fraction not responding | Group | Cp, μg/ml | Ce, μg/ml |
|---|---|---|---|
| C05 | Young | 3.2 (3.0–3.3) | 1.6 (1.4–1.7) |
| Elderly | 2.5 (2.3–2.6)* | 1.0 (0.9–1.1)† | |
| C50 | Young | 4.0 (3.9–4.1) | 2.2 (2.1–2.3) |
| Elderly | 3.1 (3.1–3.2)‡ | 1.5 (1.4–1.6)§ | |
| C95 | Young | 5.0 (4.8–5.3) | 2.9 (2.7–3.3) |
| Elderly | 3.8 (3.7–3.9)|| | 2.0 (1.9–2.1)¶ |
Values in parentheses are 95% CI. Young group: n=40. Elderly group: n=40. *Compared with young group t=3.761, P=0.000; †Compared with young group t=4.602, P=0.000; ‡Compared with young group t=5.012, P=0.000; §Compared with young group t=4.342, P=0.000; ||Compared with young group t=5.643, P=0.000; ¶Compared with young group t=6.168, P=0.000. Cp: Predicted plasma concentration; Ce: Predicted effect-site concentration; CI: Confidence interval; LOC: Loss of consciousness.
Figure 1.
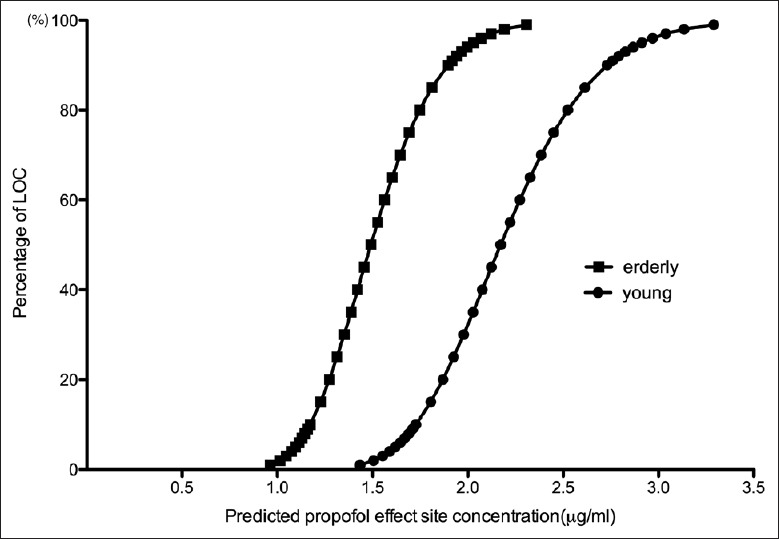
Comparison of predicted effect-site concentration of propofol (μg/ml) versus cumulative percent of being unconscious in young and elderly patients.
C50 of remifentanil was similar in both young and elderly patients at LOS
The effect-site remifentanil concentrations associated with a 50% probability of LOS was 3.5 (3.3–3.7) ng/ml in elderly patients, was similar with 3.7 (3.6–3.8) ng/ml in young patients [Table 4 and Figure 2]. The effect-site remifentanil concentrations associated with 5% and 95% probability of LOS were 1.8 (1.5–2.1) ng/ml and 5.4 (5.2–5.6) ng/ml in elderly patients, were lower than 2.3 (2.1–2.5) ng/ml and 5.9 (5.6–6.2) ng/ml in young patients, respectively [Table 4].
Table 4.
Remifentanil concentrations at LOS
| Fraction not responding | Group | Cp, ng/ml | Ce, ng/ml |
|---|---|---|---|
| C05 | Young | 3.1 (2.8–3.4) | 2.3 (2.1–2.5) |
| Elderly | 2.9 (2.6–3.1) | 1.8 (1.5–2.1) | |
| C50 | Young | 4.8 (4.7–5.0) | 3.7 (3.6–3.8) |
| Elderly | 4.8 (4.7–4.9) | 3.5 (3.3–3.7) | |
| C95 | Young | 6.5 (6.3–6.8) | 5.9 (5.6–6.2) |
| Elderly | 6.8 (6.6–7.1) | 5.4 (5.2–5.6) |
Values in parentheses are 95% CI. Young group: n=40. Elderly group: n=40. Cp: Predicted plasma concentration; Ce: Predicted effectsite concentration; CI: Confidence interval; LOS: Loss of response to titanic stimulus.
Figure 2.
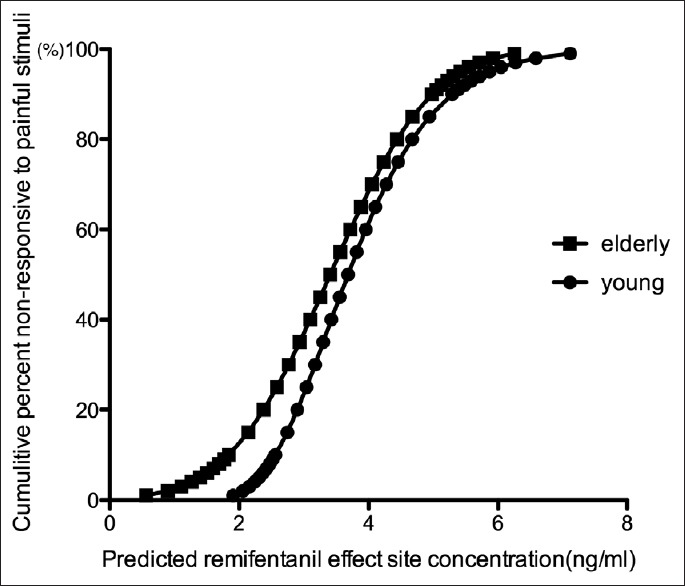
Comparison of predicted effect-site concentration of remifentanil (ng/ml) versus cumulative percent of being not responding to painful stimulus in young and elderly patients.
Bispectral index at LOC and LOS were similar in both young and elderly patients
Before induction, the BIS values at baseline were same. The BIS associated with a 50% probability of LOC was 57.3 (56.4–58.1) in elderly patients, 55.2 (54.0–56.3) in young patients, 5% and 95% patients lost consciousness at BIS values of 77.2 (75.3–79.4) and 37.3 (35.1–39.2) in elderly patients, at 79.1 (76.1–82.9) and 38.5 (36.6–40.2) in young patients [Table 5 and Figure 3].
Table 5.
BIS values at LOC and LOS
| Group | Base line | LOC (95% CI) | LOS (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| BIS Mean (SD) | BIS05 | BIS50 | BIS95 | BIS05 | BIS50 | BIS95 | |
| Young | 97 (1) | 79.1 (76.1–82.9) | 55.2 (54.0–56.3) | 38.5 (36.6–40.2) | 78.7 (76.8–80.9) | 62.4 (61.5–63.2)† | 46.0 (43.6–48.0)‡ |
| Elderly | 96 (0.6) | 77.2 (75.3–79.4) | 57.3 (56.4–58.1) | 37.3 (35.1–39.2) | 85.6 (83.8–87.6) * | 66.8 (66.0–67.6)§ | 48.0 (46.0–50.0)|| |
Young group: n=40. Elderly group: n=40. *Compared with young group t=2.426, P=0.02, compared with LOC t=4.342 P=0.000, compared with baseline t=5.890, P=0.000; †Compared with LOC t=3.767, P=0.000, compared with baseline t=6.002, P=0.000; ‡Compared with LOC t=5.034, P=0.000, compared with baseline t=6.901, P=0.000; §Compared with young group t=2.101, P=0.044, compared with LOC t=4.890, P=0.000, compared with baseline t=5.340, P=0.000; ||Compared with LOC t=4.340, P=0.000, compared with baseline t=5.640, P=0.000. 95% CI: 95% confidence intervals; LOC: Loss of consciousness; LOS: Loss of response to titanic stimulus; SD: Standard deviation; BIS: Bispectral index.
Figure 3.
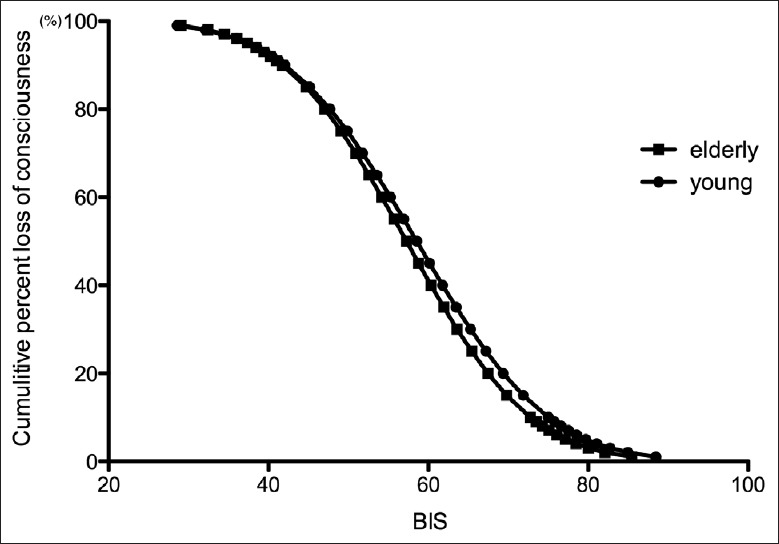
Comparison of bispectral index values versus cumulative percent of being unconscious in young and elderly patients.
The BIS associated with a 50% probability of LOS was 66.8 (66.0–67.6) in elderly patients, 62.4 (61.5–63.2) in young patients, the BIS values associated with 5% and 95% probability of LOS were of 85.6 (83.8–87.6) and 48.0 (46.0–50.0) in elderly patients, at 78.7 (76.8–80.9) and 46.0 (43.6–48.0) in young patients. There was no difference between elderly and young groups about the BIS50 associated with LOC, BIS50 of elderly patients in LOS was higher than that of young patients (P < 0.05). [Table 5 and Figure 4].
Figure 4.
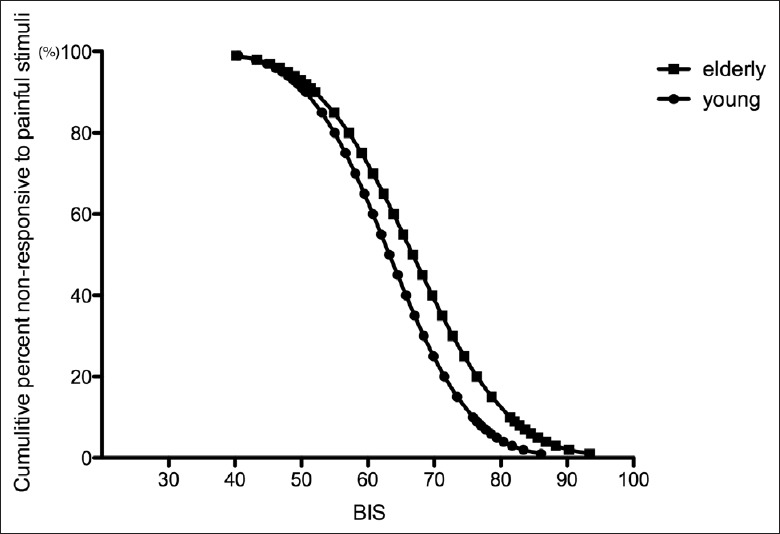
Comparison of bispectral index values versus cumulative percent of being not responding to a painful stimulus (LOS) in young and elderly patients.
In both age groups, the BIS values at LOC dropped down from awake status (P = 0.000), and increased after tetanic stimuli over that at LOC (P = 0.000).
DISCUSSION
Previous clinical studies reported that predicted blood and effect-site propofol and remifentanil concentrations and values of BIS, based on Caucasian data, are also useful for predicting whether a Chinese patient is unconscious and unresponsive to painful stimulus (population aged from 18 to 65 years).[1] In this study, we continued to investigate and compare predicted blood and effect-site concentrations of propofol and remifentanil, values of BIS at two clinical end-points – LOC and LOS in elderly and young Chinese patients.
Pharmacodynamic changes of propofol in elderly patients
Although age-related changes in the pharmacology of propofol are now well demonstrated,[2] but age is still not taken into account by the Marsh pharmacokinetic model incorporated in the diprifusor device. However, it has been reported that TCI propofol with Marsh parameters could be applied to Chinese elderly patients safely and efficiently.[3] For remifentanil, we used the TCI system made by SLGO Corporation, which is widely used in China. The remifentanil model uses the Minto pharmacokinetic model, which has been demonstrated as adequately accurate in predicting plasma and effect-site concentrations of remifentanil.[4,5]
Elderly patients are reported to be more sensitive to propofol than are young patients.[2,6,7] However, there was few study determining the C50 of propofol and remifentanil that elderly patients required during TCI at LOC and painful stimulus in either Caucasian or Chinese populations. The effect-site C50 and C95 of propofol at LOC have been shown to be 2.8 and 4.1 μg/ml in adult Caucasian populations.[8] However, in a study by Xu et al., effect-site C50 and C95 of propofol at LOC were 2.2 and 3.2 μg/ml in the Chinese adult populations (aged ≤65 years). As results of our study, the C50 and C95 for effect-site propofol concentration at LOC was 1.5 μg/ml and 2.0 μg/ml in elderly patients, 2.2 μg/ml and 2.9 μg/ml in young patients respectively, the results of our study were similar to those of Liu et al., which showed that predicted effect-site concentration (Ce) of propofol with (1.9 ± 0.3) μg/ml may make the elderly patients unconscious.[9] Therefore, confirmed to previous studies we found that the effect-site concentration required for unconsciousness was obviously lower in Chinese than the Caucasian population and was significantly lower in elderly patients than young patients. The reason of pharmacodynamic aspect has been proved by Schüttler and Ihmsen et al. that central volume (V1) and elimination clearance (CL1) of propofol reduced in elderly patients, and was linearly decreased with age for the patients older than 60 years.[10,11]
Pharmacodynamic changes of remifentanil in elderly patients
Tetanic stimulation of the ulnar nerve has the advantage of ease of performance, repeatability, re-producibility and is frequently used in lieu of skin incision, is a standard method in pain research.[12,13,14]
Unique features of remifentanil are its rapid clearance and rapid react, resulting in a rapid onset and offset of drug effect, and without in vivo accumulative characteristics. It is tempting to speculate that these characteristics will make remifentanil an easy drug to titrate and that clinicians will not need to consider that patient covariates including age when choosing a dosing regimen. Previous studies have reported conflicting findings concerning the influence of age and gender on the pharmacokinetics of opioids. Studies from Caucasians and as well as Chinese showed that the values of elimination half-time (t1/2ß), volume distilbution (Vd) and clearance (CL) were significantly higher in elderly patients. So, it is for pharmacodynamic reasons (the 50% reduction in C50 in the elderly) that remifentanil bolus doses should be decreased in the elderly.[5,15] But, results from pharmacodynamic research, Xu et al. found there were no age-related difference in 405 Chinese patients <65 years.[16] Our study demonstrated that effect-site C50 and C95 of remifentanil at nonresponse to painful stimulus was 3.5 ng/ml and 5.4 ng/ml in elderly, that was similar with 3.7 ng/ml and 5.9 ng/ml in young group. The one reason which probably can explain why no significant difference was found between groups as to the predicted effect-site remifentanil concentrations required is that because we chose the Minto pharmacokinetic model, which does take into account some co-variables such as height, weight and age; the other one reason might be the effects of drug interactions between propofol and remifentanil. Compared with young group, elderly patients needed lower propofol concentration for keeping LOC, so they would need combine comparative higher remifentanil concentration to inhibit painful stimulus, our results support this supposition of Lichtenbelt et al., that was a kind of high-opioid/low-propofol anesthesia.[17] Sample size was limited in this research and was still be considered.
The MAP and HR decreased significantly during TCI infusing propofol at LOC, before achieving no response to tetanic stimulus, MAP and HR further decreased due to administration of remifentanil, the hemodynamic changes was greater in elderly patients than that of young patients, but were in clinical acceptable range. Therefore, during anesthesia induction using TCI propofol combined with remifentanil, we should modify the target concentration or the TCI technique, such as step-wise (two stepwise or three step-wise) technique or a step-by-step technique, can result in stable hemodynamic, especially for the elderly patients, or in those with the cardiovascular diseases.[18,19,20]
The bispectral index changes in elderly patient
Several investigators have studied the sensitivity of BIS as a measure of sedation and anesthesia in adult and elderly patients receiving propofol infusions.[21,22,23] It has been shown to be a useful monitor of propofol sedation and anesthesia. Barakat et al. identified that the changes of both the sedation score and BIS index correlated better with the predicted Ce in using the Marsh model than in using the Schnider model, so Marsh model was chosen for our study. Two previous studies have evaluated the BIS values at LOC when TCI propofol is used.[1,8] From our study, we found that there was no difference found about BIS between young and elderly groups at baseline, LOC clinical end-points, it meant that BIS values were not affected by age obviously, although BIS is monitor of hypnotic level derived from the processed electroencephalogram (EEG), and EEG changes with age, this confirms a review of the literature that concluded that age-related changes in the EEG do not affect BIS,[24,25] it just can reflect sedative status level such as LOC and loss of response to tetanic stimuli, so maybe it was reason why there were no differences between elderly and young groups at resting, non tetanic stimuli situation.
The BIS50 and BIS95 at LOC were 71 and 53 respectively in Caucasians,[8] whereas the values were 58 and 39 respectively in Chinese.[1] We noted that the predicted blood and effect-site propofol concentrations in our Chinese population were lower than that in Caucasians at LOC. Our results therefore suggested that the correlation between the predicted blood or effect-site propofol concentrations and BIS in Chinese patients differ from that in Caucasians[16,22,23,26] and that the standard BIS values to predict the depth of hypnosis may not be suitable for Chinese patients.
In order to observe the purposed movement to tetanic stimulus, we could not give the muscle relaxants until intubation, but BIS will be infulenced by myoelectrical activity, that might be a reason why BIS50 at LOS was higher than that at LOC. Further studies on relationship of propofol concentration and sedative level, acurate monitoring index of sedation is surely warrented.
Limitations
Biological aging often does not correlate with chronological age, resulting in considerable physiological, pharmacokinetic and pharmacodynamic differences between patients. This contributes to large variation in interindividual response to propofol and remifentanil and increased sensitivity to their adverse effects. Elderly patients tend to have multiple comorbidities and to present a high peri-operative risk.[27] Although we took step by step titrated way to avoid hemodynamic intensive fluctuation, considering clinical safety we only chose ASA physical status I - II into elderly group, if patients had co-existing diseases such as old cerebral infarction, transient cerebral ischemic attack or poor ASA status, and hence that results from this study was limited for such clinical situations.
Because the plasma concentration of propofol was not measured in all studies above, it is impossible to know whether these inconsistent results were due to pharmacokinetic or pharmacodynamic differences among the populations of different races and age.
In conclusion, the findings from our study suggest that an adjustment of propofol – remifentanil TCI in elderly patients should be applied: It's safe to titrate both propofol and remifentanil properly according to BIS and hemodynamic changes during anesthesia induction; to choose high-opioid/low-propofol anesthesia may be associated with increased hemodynamic stability during induction of anesthesia.
ACKNOWLEDGEMENTS
Assistance with the study: We would like to thank Prof. Philip Bickler (Department of Anesthesia, University of California Medical Center at San Francisco) for his polishment and recommendations for this article.
Footnotes
Edited by: Ya-Lin Bao
Source of Support: This work was supported by the Department of Anesthesiology, Beijing Hospital, Beijing, China.
Conflict of Interest: None declared.
REFERENCES
- 1.Xu Z, Liu F, Yue Y, Ye T, Zhang B, Zuo M, et al. C50 for propofol-remifentanil target-controlled infusion and bispectral index at loss of consciousness and response to painful stimulus in Chinese patients: A multicenter clinical trial. Anesth Analg. 2009;108:478–83. doi: 10.1213/ane.0b013e31818f8a30. [DOI] [PubMed] [Google Scholar]
- 2.Schnider TW, Minto CF, Shafer SL, Gambus PL, Andresen C, Goodale DB, et al. The influence of age on propofol pharmacodynamics. Anesthesiology. 1999;90:1502–16. doi: 10.1097/00000542-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Xu CY, Wu XM, Jiang JY. Target-controlled infusions of remifentanil and propofol in elderly patients. J Peking Univer (Health Sci) 2005;37:513–5. [PubMed] [Google Scholar]
- 4.Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997;86:10–23. doi: 10.1097/00000542-199701000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology. 1997;86:24–33. doi: 10.1097/00000542-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Jun Z, Jian W, Linli L, Henglin S. The guidance of bispectral index on administered dose of propofol of elderly patients during anesthetic induction. Mod Prev Med. 2007;34:3977–82. [Google Scholar]
- 7.Kirkpatrick T, Cockshott ID, Douglas EJ, Nimmo WS. Pharmacokinetics of propofol (diprivan) in elderly patients. Br J Anaesth. 1988;60:146–50. doi: 10.1093/bja/60.2.146. [DOI] [PubMed] [Google Scholar]
- 8.Milne SE, Troy A, Irwin MG, Kenny GN. Relationship between bispectral index, auditory evoked potential index and effect-site EC50 for propofol at two clinical end-points. Br J Anaesth. 2003;90:127–31. doi: 10.1093/bja/aeg035. [DOI] [PubMed] [Google Scholar]
- 9.Liu SH, Wei W, Ding GN, Ke JD, Hong FX, Tian M. Relationship between depth of anesthesia and effect-site concentration of propofol during induction with the target-controlled infusion technique in elderly patients. Chin Med J. 2009;122:935–40. [PubMed] [Google Scholar]
- 10.Schüttler J, Ihmsen H. Population pharmacokinetics of propofol: A multicenter study. Anesthesiology. 2000;92:727–38. doi: 10.1097/00000542-200003000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Kazama T, Ikeda K, Morita K, Ikeda T, Kikura M, Sato S. Relation between initial blood distribution volume and propofol induction dose requirement. Anesthesiology. 2001;94:205–10. doi: 10.1097/00000542-200102000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Ortolani O, Conti A, Chan YK, Sie MY, Ong GS. Comparison of propofol consumption and recovery time in Caucasians from Italy, with Chinese, Malays and Indians from Malaysia. Anaesth Intensive Care. 2004;32:250–5. doi: 10.1177/0310057X0403200215. [DOI] [PubMed] [Google Scholar]
- 13.Saidman LJ, Eger EI., 2nd Effect of nitrous oxide and of narcotic premedication on the alveolar concentration of halothane required for anesthesia. Anesthesiology. 1964;25:302–6. doi: 10.1097/00000542-196405000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kopman AF, Lawson D. Milliamperage requirements for supramaximal stimulation of the ulnar nerve with surface electrodes. Anesthesiology. 1984;61:83–5. [PubMed] [Google Scholar]
- 15.Zhang MH, Gao JG, Zhou XM. Age difference of remifentanil in pharmacokinetics. J Clin Anesthesiol. 2010;26:127–8. [Google Scholar]
- 16.Xu Z, Liu F, Yue Y, Ye T, Zhang B, Zuo M, et al. The effect of gender and age on bispectral index and effective concentration 50 for propofol-remifentanil target-controlled infusion at two clinical end-points – A multi-center clinical research. Int J Anesth Resusc. 2006;27:144–8. [Google Scholar]
- 17.Lichtenbelt BJ, Mertens M, Vuyk J. Strategies to optimise propofol-opioid anaesthesia. Clin Pharmacokinet. 2004;43:577–93. doi: 10.2165/00003088-200443090-00002. [DOI] [PubMed] [Google Scholar]
- 18.Yu BW, Peng ZL, Zhao YQ. Changes in the effect compartment concentration and bispectra index during a step-by-step TCI of propofol in the elderly (in Chinese) Chin J Anesthesiol. 2002;22:711–4. [Google Scholar]
- 19.Struys MM, De Smet T, Depoorter B, Versichelen LF, Mortier EP, Dumortier FJ, et al. Comparison of plasma compartment versus two methods for effect compartment – Controlled target-controlled infusion for propofol. Anesthesiology. 2000;92:399–406. doi: 10.1097/00000542-200002000-00021. [DOI] [PubMed] [Google Scholar]
- 20.Wakeling HG, Zimmerman JB, Howell S, Glass PS. Targeting effect compartment or central compartment concentration of propofol: What predicts loss of consciousness? Anesthesiology. 1999;90:92–7. doi: 10.1097/00000542-199901000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Liu J, Singh H, White PF. Electroencephalographic bispectral index correlates with intraoperative recall and depth of propofol-induced sedation. Anesth Analg. 1997;84:185–9. doi: 10.1097/00000539-199701000-00033. [DOI] [PubMed] [Google Scholar]
- 22.Kearse LA, Jr, Rosow C, Zaslavsky A, Connors P, Dershwitz M, Denman W. Bispectral analysis of the electroencephalogram predicts conscious processing of information during propofol sedation and hypnosis. Anesthesiology. 1998;88:25–34. doi: 10.1097/00000542-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Gan TJ, Glass PS, Windsor A, Payne F, Rosow C, Sebel P, et al. Bispectral index monitoring allows faster emergence and improved recovery from propofol, alfentanil, and nitrous oxide anesthesia. BIS Utility Study Group. Anesthesiology. 1997;87:808–15. doi: 10.1097/00000542-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Renna M, Venturi R. Bispectral index and anaesthesia in the elderly. Minerva Anestesiol. 2000;66:398–402. [PubMed] [Google Scholar]
- 25.Arnold G, Kluger M, Voss L, Sleigh J. BIS and Entropy in the elderly. Anaesthesia. 2007;62:907–12. doi: 10.1111/j.1365-2044.2007.05149.x. [DOI] [PubMed] [Google Scholar]
- 26.Leslie K, Sessler DI, Schroeder M, Walters K. Propofol blood concentration and the Bispectral Index predict suppression of learning during propofol/epidural anesthesia in volunteers. Anesth Analg. 1995;81:1269–74. doi: 10.1097/00000539-199512000-00025. [DOI] [PubMed] [Google Scholar]
- 27.Story DA, Fink M, Leslie K, Myles PS, Yap SJ, Beavis V, Kerridge RK, McNicol PL. Perioperative mortality risk score using pre- and postoperative risk factors in older patients. Anaesth Intensive Care. 2009;37:392–8. doi: 10.1177/0310057X0903700310. [DOI] [PubMed] [Google Scholar]


