Abstract
STUDY DESIGN
Controlled laboratory study, longitudinal design.
OBJECTIVE
To examine whether baseline knee flexion moment or impulse during walking is associated with the progression of osteoarthritis (OA) with magnetic resonance imaging of the patellofemoral joint (PFJ) at 1 year.
BACKGROUND
Patellofemoral joint OA is highly prevalent and a major source of pain and dysfunction. The biomechanical factors associated with the progression of PFJ OA remain unclear.
METHODS
Three-dimensional gait analyses were performed at baseline. Magnetic resonance imaging of the knee (high-resolution, 3-D, fast spin-echo sequence) was used to identify PFJ cartilage and bone marrow edema–like lesions at baseline and a 1-year follow-up. The severity of PFJ OA progression was defined using the modified Whole-Organ Magnetic Resonance Imaging Score when new or increased cartilage or bone marrow edema–like lesions were observed at 1 year. Peak external knee flexion moment and flexion moment impulse during the first and second halves of the stance phase of gait were compared between progressors and nonprogressors, and used to predict progression after adjusting for age, sex, body mass index, and presence of baseline PFJ OA.
RESULTS
Sixty-one participants with no knee OA or isolated PFJ OA were included. Patellofemoral joint OA progressors (n = 10) demonstrated significantly higher peak knee flexion moment (P = .01) and flexion moment impulse (P = .04) during the second half of stance at baseline compared to nonprogressors. Logistic regression showed that higher peak knee flexion moment during the second half of the stance phase was significantly associated with progression at 1 year (adjusted odds ratio = 3.3, P = .01).
CONCLUSION
Peak knee flexion moment and flexion moment impulse during the second half of stance are related to the progression of PFJ OA and may need to be considered when treating individuals who are at risk of or who have PFJ OA.
Keywords: bone marrow lesions, cartilage, gait, kinetics, WORMS
Patellofemoral joint (PFJ) osteoarthritis (OA) is a highly prevalent knee disease that can result in significant pain and dysfunction.17,32,35 Based on the findings of radiographic18 and magnetic resonance imaging (MRI)54 studies, 64% of adults over 50 years of age have PFJ OA, a third of whom have isolated PFJ OA. This shows that the prevalence of PFJ OA is as high as, if not higher than, tibiofemoral joint (TFJ) OA.18,39,54 Moreover, similar rates of disease progression have been reported for TFJ and PFJ OA.4,14,32,47 Though extensive research has evaluated the biomechanical risk factors associated with the progression of TFJ OA,5,11,41 biomechanical predictors of the progression of PFJ OA have not been reported. Identifying biomechanical factors related to morphological changes of PFJ OA is critical to inform clinical assessment and intervention strategies for this common knee disease.
Mechanical loading plays an important role in the onset and progression of knee OA.2,12,24,26 For example, higher knee adduction moment and adduction moment impulse, which can result in increased medial TFJ loading, have been well documented to be related to the presence,6,23,42 severity,23,33 and progression5,11,41 of medial compartment TFJ OA. At the PFJ, biomechanical factors such as knee flexion moment and flexion moment impulse can be used to estimate mechanical loading. For example, increased knee flexion moment has been reported to result in higher PFJ reaction force and stress.31,56 Moreover, knee flexion moment impulse, which takes into account both the magnitude and duration of knee flexion moment, may provide more detailed information regarding PFJ loading. As such, knee flexion moment and flexion moment impulse may be important predictors of the onset or progression of degenerative changes of the PFJ.
During gait, distinct peaks of knee flexion moment are observed during the first and second halves of the stance phase.29,31,36 Although the first peak is typically 2 to 3 times larger than the second peak, recent cross-sectional studies have shown that peak knee flexion moment during the second half of the stance phase is higher in individuals with PFJ OA.21,55 To the best of our knowledge, no study has reported biomechanical factors associated with the onset or progression of PFJ OA. Articular cartilage lesions and subarticular bone marrow edema–like lesions (BMELs) are morphological features of OA disease10,15,16,32 and have been associated with pain.3,9,16,20,37 Using MRI, semi-quantitative assessment can be performed to provide reliable and sensitive measures of these morphological characteristics over time.19,28,45,49 The purpose of this study was to examine whether knee flexion moment or flexion moment impulse during the stance phase of gait could be predictive of the onset or progression of morphological lesions (ie, cartilage lesions and BMELs) associated with PFJ OA at 1 year. We hypothesized that higher knee flexion moment and flexion moment impulse would be associated with progression of PFJ OA.
METHODS
Participants
Participants were recruited from the local community as part of a longitudinal study on knee OA. All participants were above 35 years of age and did not have (1) history of lower extremity or spine surgery, (2) total joint replacement of any lower extremity joint, (3) self-reported inflammatory arthritis, (4) any condition that would limit the ability to walk without an assistive device, and (5) contraindications to MRI.55 As part of the procedures of the knee OA study, all participants underwent a weight-bearing, posteroanterior, fixed-flexion radiograph of the TFJs. The knee with the higher Kellgren-Lawrence grade was chosen for the following MRI and biomechanical tests. When both knees presented with the same Kellgren-Lawrence grade, the test limb was determined based on participant preference. Prior to inclusion in the study, all participants signed a written informed consent approved by the Committee on Human Research at the University of California San Francisco.
Pain and Function Assessments
All participants completed the Knee injury and Osteoarthritis Outcome Score (KOOS) survey. A higher score on the KOOS, which ranges from 0 to 100, represents less pain and better function.50,51 Physical function was tested in all participants using a six-minute walk test, timed up-and-go test, and stair-climbing test. During the six-minute walk test, participants were instructed to walk as long a distance as possible during a 6-minute period.34 During the timed up-and-go test, participants were timed with a stopwatch as they rose from a standard armchair (approximate seat height, 44 cm; arm height, 68 cm from the floor), walked to a tape mark 3 m away, then returned to a sitting position with their back against the chair as fast as possible.34 During the stair-climbing test, participants were timed with a stopwatch as they ascended and descended a set of 12 stairs (step height, 18 cm) as fast as possible.48
MRI Assessment
Magnetic resonance images were acquired using a 3-T scanner (Discovery MR750w; GE Healthcare, Waukesha, WI) with an 8-channel transmit/receive knee coil (Invivo, Gainesville, FL) at baseline and 1 year. A high-resolution, 3-D fast spin-echo CUBE (GE Healthcare) sequence (repetition time/echo time, 1500/26.69 milliseconds; field of view, 16 cm; matrix, 384 × 384; slice thickness, 0.5 mm; echo train length, 32; bandwidth, 37.5 kHz; number of excitations, 0.5; acquisition time, 10.5 minutes) was used for clinical grading of OA-related morphological changes.
Semi-quantitative assessment of articular cartilage lesions and BMELs was performed by an experienced boardcertified radiologist using the modified Whole-Organ Magnetic Resonance Imaging Score (WORMS).1,45,54 Cartilage lesions were graded as follows: 0, normal thickness; 1, normal thickness (increased signal intensity); 2, a partial-thickness focal lesion less than 1 cm at greatest width; 2.5, a full-thickness focal lesion less than 1 cm at greatest width; 3, multiple areas of partial lesions less than 1 cm at greatest width or a grade 2 lesion wider than 1 cm but less than 75% of the region; 4, diffuse partial-thickness loss greater than 75% of the region; 5, multiple areas of full-thickness lesions greater than 1 cm but less than 75% of the region; and 6, diffuse full-thickness loss greater than 75% of the region.45 The BMELs were graded as follows: 0, normal; 1, mild (maximum diameter less than 5 mm); 2, moderate (5–20 mm); and 3, severe (greater than 20 mm).45 Gradings were performed at 6 regions: the patella, trochlea, medial and lateral femoral condyles, and medial and lateral tibial plateau.
The WORMS grading system has been shown to have high intrarater (intraclass correlation coefficient greater than 0.92)3 and interrater (intraclass correlation coefficient greater than 0.82)3,45 reliability and demonstrates strong agreement with other commonly used imaging scoring systems.38 The WORMS score was used to define the presence of knee OA in this study. Tibiofemoral joint OA was considered present when the WORMS score was greater than 1 for cartilage lesion of the tibia or femur.54 Patellofemoral joint OA was considered present when the WORMS score was greater than 1 for cartilage lesion of the patella or trochlea.54 End-stage PFJ cartilage lesions and BMELs were defined as a WORMS score of 6 for cartilage lesions and of 3 for BMELs. Individuals with TFJ OA were excluded from this study to prevent potential influence of TFJ OA on gait biomechanics. Individuals with end-stage PFJ cartilage lesions or BMELs were also excluded from this study because no further progression was possible.
Gait Analysis
Three-dimensional gait analysis was performed at baseline. Lower extremity kinematics were recorded using a 10-camera motion-capture system (Vicon; OMG plc, Oxford, UK) at a sampling rate of 250 Hz. Ground reaction force data were obtained using 2 embedded force platforms (Advanced Mechanical Technology, Inc, Watertown, MA) at a sampling rate of 1000 Hz. Marker and ground reaction force data were collected and synchronized using motion-capture software (Nexus; OMG plc). Participants wore shorts and their personal sneakers during the evaluation.
Prior to the walking test, retroreflective anatomical markers (14-mm spheres) were placed on the following bony landmarks: L5-S1 junction, bilateral iliac crests, anterior superior iliac spines, greater trochanters, medial and lateral femoral epicondyles, medial and lateral malleoli, and first and fifth metatarsal heads. Additionally, tracking marker clusters mounted on semi-rigid plastic plates were placed bilaterally on the lateral surfaces of the participant’s thighs, shanks, and heel counters of the shoes. A standing calibration trial was obtained to define the segment coordinate systems and joint axes. After the calibration trial, anatomical markers were removed, except for those on the L5-S1 junction, iliac crests, and anterior superior iliac spines, which served as tracking markers for the pelvis. The tracking markers remained on the participant throughout the entire data-collection session.
Participants were instructed to walk at a self-selected speed, which was described as “you have some place to be, but you are not late.” Five successful trials were obtained. A trial was considered successful when the foot of the tested limb fell within the borders of either of the force platforms from initial contact to toe-off and the speed was within ±5% of the first successful trial.
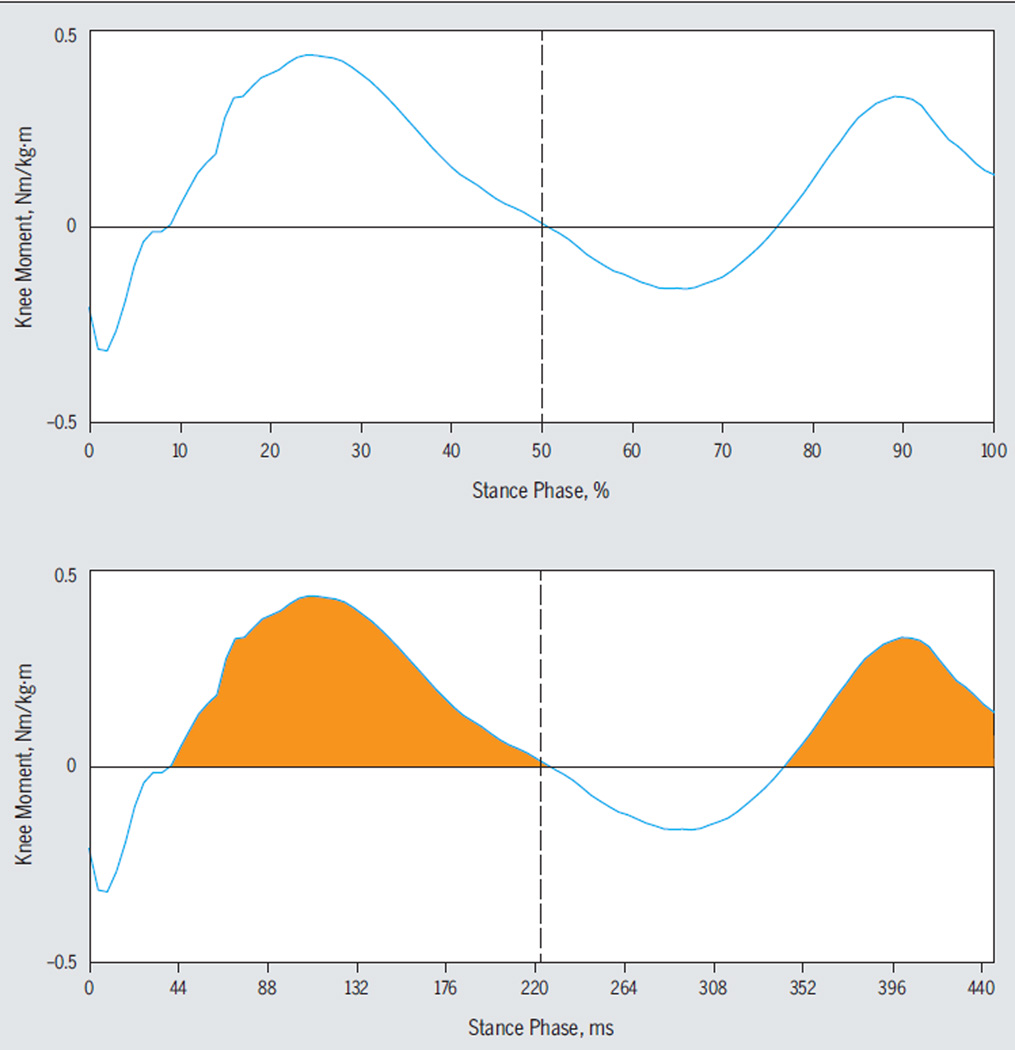
Kinematic and kinetic data were computed using Visual3D (C-Motion, Inc, Germantown, MD) and MATLAB software (The MathWorks, Inc, Natick, MA). Marker trajectory data were low-pass filtered using a fourth-order Butterworth filter with a cutoff frequency of 6 Hz. The pelvis was modeled with 6 degrees of freedom relative to the laboratory coordinate system.40 The hip, knee, and ankle joints were assigned 3 degrees of freedom for rotations.57 Joint kinematics were calculated using a Cardan rotation sequence in the order of flexion/extension, abduction/adduction, and internal/external rotation.57 Net joint moments were reported as external moments and normalized to each participant’s body mass (kg) and height (m). The positive and negative values of the sagittal plane knee moment were used to indicate knee flexion and extension moments, respectively (FIGURE 1). Knee flexion moment impulse was calculated as the integral of knee flexion moment (Nm/kg·m) with respect to time (milliseconds) when sagittal plane knee moment was positive for each walking trial (FIGURE 1). The stance phase of gait was defined during the time when the vertical ground reaction force was greater than 20 N. Variables of interest, peak knee flexion moment, and knee flexion moment impulse were computed for the first 50% and second 50% of the stance phase. Averaged data from 5 successful trials were used for statistical analyses.
FIGURE 1.
Sagittal plane knee moment curve during the stance phase of walking of a sample trial. Joint moment is expressed as external moment. Positive and negative values indicate knee flexion and extension moments, respectively. The vertical dotted line indicates 50% of the stance phase. Peak knee flexion moment and flexion moment impulse are computed during the first and second halves of the stance phase. Knee flexion moment impulse was calculated as the integral of knee flexion moment (Nm/kg·m) with respect to time (milliseconds) when sagittal plane knee moment was positive (orange area).
PFJ OA Progression
Participants were stratified into progressors and nonprogressors based on OA-related morphological changes observed on magnetic resonance images obtained at 1 year compared to baseline images. Progression of PFJ OA was defined as an increase in WORMS score of at least 1 grade on the cartilage or BMEL grading systems, except for an increase from 0 to 1.
Statistical Analysis
Chi-square and independent t tests were used to compare demographic, symptom, and functional data between progressors and nonprogressors. Walking speed was compared between the progression and nonprogression groups using an independent t test. To account for any significant group difference in walking speed, adjustments to the subsequent statistical analyses were planned but not performed, as no significant group difference was found.
Peak knee flexion moment and knee flexion moment impulse during the first and second halves of the stance phase were compared between progressors and nonprogressors using analyses of covariance, with age, sex, body mass index (BMI), and presence of baseline PFJ OA as covariates.
Binary logistic regression was used to identify whether baseline peak knee flexion moment and knee flexion moment impulse during the first and second halves of the stance phase predicted progression of PFJ OA at 1 year. Models were performed with and without adjustment for age, sex, BMI, and presence of baseline PFJ OA. All ordinal data were converted into standardized scores before entering the logistic regression models. All analyses were performed using IBM SPSS Statistics Version 22.0.0 software (IBM Corporation, Armonk, NY), with a significance level set at .05.
RESULTS
Eighty-four participants completed MRI and gait analysis at baseline and MRI at 1 year. Among these participants, 23 presented TFJ OA on baseline MRI and were excluded from statistical analysis. A total of 61 participants (41 female, 20 male; mean ± SD age, 51.3 ± 9.9 years; BMI, 24.4 ± 3.3 kg/m2) were included in the statistical analysis. Twenty-eight (45.9%) of the 61 participants were diagnosed with PFJ OA at baseline. At 1-year follow-up, 10 (16.4%) of the 61 participants demonstrated progression of PFJ OA. Among the 10 progressors, 6 demonstrated progressions in cartilage lesions, 3 had progressions in BMELs, and 1 demonstrated progressions in both cartilage lesions and BMELs. Demographic, pain, and functional activity data of the progressors and nonprogressors at baseline are presented in TABLE 1. A higher percentage of women (P = .02) and individuals who presented with baseline PFJ OA (P = .03) were among the progressors. No significant differences were observed in age, BMI, and symptom and functional ability between progressors and nonprogressors (TABLE 1). In addition, there was no significant difference (P = .79) in self-selected walking speed during gait analysis between progressors (mean ± SD, 1.53 ± 0.22 m/s) and nonprogressors (1.55 ± 0.22 m/s).
TABLE 1.
Baseline Demographic, Symptom, and Functional Data for the PFJ OA Nonprogressors and Progressors*
| Nonprogressors | Progressors | P Value† | |
|---|---|---|---|
| Demographics | |||
| Sex (male/female), n | 20/31 | 0/10 | .02 |
| Age, y | 50.6 ± 9.9 | 55.0 ± 9.5 | .20 |
| BMI, kg/m2 | 24.6 ± 3.1 | 22.7 ± 3.8 | .09 |
| PFJ OA‡ (yes/no), n | 20/31 | 8/2 | .03 |
| Pain and function | |||
| KOOS pain, % | 89.4 ± 11.2 | 86.4 ± 18.4 | .50 |
| KOOS activities of daily living, % | 94.0 ± 8.9 | 93.4 ± 9.5 | .85 |
| Timed up-and-go test, s | 5.8 ± 0.9 | 5.6 ± 0.6 | .50 |
| Timed stairs, s | 11.6 ± 1.8 | 11.5 ± 2.2 | .93 |
| Six-minute walk test, m | 642.0 ± 83.5 | 664.4 ± 90.0 | .45 |
Abbreviations: BMI, body mass index; KOOS, Knee injury and Osteoarthritis Outcome Score; OA, osteoarthritis; PFJ, patellofemoral joint.
Values are mean ± SD unless otherwise indicated.
Independent t test for ordinal variables and chi-square for categorical variables.
Cartilage lesions of the trochlea or patella with a score of greater than 1 on the modified Whole-Organ Magnetic Resonance Imaging Score (WORMS).
Analyses of covariance revealed significant differences in knee kinetics during the second half of the stance phase between progressors and nonprogressors (TABLE 2, FIGURE 2). Patellofemoral joint OA progressors demonstrated significantly higher peak knee flexion moment (P = .01, Cohen d = 1.17) and knee flexion moment impulse (P = .04, Cohen d = 1.02) during the second half of the stance phase compared to the nonprogressors. No significant difference was observed for knee flexion moment and flexion moment impulse during the first half of stance between the 2 groups (TABLE 2).
TABLE 2.
Baseline Values for Knee Kinetics During the First and Second Halves of the Stance Phase for the PFJ OA Nonprogressors and Progressors
| Nonprogressors* | Progressors* | P Value† | |
|---|---|---|---|
| Knee flexion moment: first peak, Nm/kg·m | 0.37 ± 0.14 | 0.29 ± 0.13 | .23 |
| Knee flexion moment impulse: first half, Nm·ms/kg·m | 43.1 ± 18.5 | 32.4 ± 15.2 | .31 |
| Knee flexion moment: second peak, Nm/kg·m | 0.13 ± 0.05 | 0.20 ± 0.07 | .01 |
| Knee flexion moment impulse: second half, Nm·ms/kg·m | 9.1 ± 6.2 | 16.4 ± 8.8 | .04 |
Abbreviations: OA, osteoarthritis; PFJ, patellofemoral joint.
Values are mean ± SD.
Analysis of covariance adjusted for age, sex, body mass index, and presence of baseline PFJ OA.
FIGURE 2.
Sagittal plane knee moments during the stance phase of walking for progressors and nonprogressors of patellofemoral joint osteoarthritis. Values are mean ± SD (error bars). *Significant group difference in the peak knee flexion moment during the second half of the stance phase.
Logistic regression unadjusted for demographic variables revealed that higher peak knee flexion moment (odds ratio [OR] = 3.30, P = .003) and flexion moment impulse (OR = 2.45, P = .008) during the second half of stance at baseline were significantly associated with progression of PFJ OA at 1 year (TABLE 3). When adjusted for age, sex, BMI, and presence of baseline PFJ OA, higher peak knee flexion moment (adjusted OR = 3.30, P = .014) during the second half of stance at baseline was significantly associated with PFJ OA progression at 1 year. Knee flexion moment impulse during the second half of stance was also approaching significance in its association with progression of PFJ OA (adjusted OR = 2.52, P = .06). Knee flexion moment and impulse during the first half of the stance phase were not significantly associated with PFJ OA progression at 1 year, based on the unadjusted and adjusted models.
TABLE 3.
Results of Logistic Regression Analysis
| Univariate Analysis | Multivariate Analysis* | |||
|---|---|---|---|---|
| Odds Ratio† | P Value | Odds Ratio† | P Value | |
| Knee flexion moment: first peak, Nm/kg·m | 0.53 (0.24, 1.14) | .10 | 0.63 (0.26, 1.52) | .31 |
| Knee flexion moment impulse: first half, Nm·ms/kg·m | 0.51 (0.23, 1.13) | .10 | 0.63 (0.26, 1.55) | .32 |
| Knee flexion moment: second peak, Nm/kg·m | 3.30 (1.51, 7.18) | .003 | 3.30 (1.27, 8.54) | .01 |
| Knee flexion moment impulse: second half, Nm·ms/kg·m | 2.45 (1.26, 4.78) | .008 | 2.52 (0.95, 6.70) | .06 |
Adjusted for age, sex, body mass index, and presence of patellofemoral joint osteoarthritis at baseline.
Values in parentheses are 95% confidence interval.
DISCUSSION
This is the first study to reveal biomechanical risk factors associated with morphological progressions of PFJ OA. Our findings suggest that higher knee flexion moment and flexion moment impulse during walking may contribute to morphological progression of PFJ OA. In particular, we found that individuals who demonstrated a progression of PFJ OA at 1 year exhibited higher peak knee flexion moment and knee flexion moment impulse during the second half of stance phase at baseline. Peak knee flexion moment during the second half of stance was predictive of progression of PFJ OA at 1 year after adjusting for age, sex, BMI, and presence of baseline PFJ OA. Peak knee flexion moment and knee flexion moment impulse during the first half of the stance phase were not related to PFJ OA progression at 1 year.
Findings of this study support the importance of mechanical loading in the progression of morphological changes associated with OA.2,12,24,26 Previously, frontal plane knee kinetics, such as knee adduction moment and adduction moment impulse, have been identified as being predictive of the progression of cartilage loss and of BMELs in medialcompartment TFJ OA.5,11,41 Our findings indicate that sagittal plane knee kinetics, specifically knee flexion moment and knee flexion moment impulse, are associated with progression of PFJ cartilage lesions and BMELs. Based on the results of the adjusted ORs, every 1-SD (approximately 33%) increase in peak knee flexion moment during the second half of stance is related to a 3.3-times-higher chance of PFJ OA progression occurring at 1 year. Moreover, every 1-SD increase in knee flexion moment impulse during the second half of stance is related to a 2.5-times-greater occurrence of the progression of PFJ OA at 1 year. Increased knee flexion moment is suggestive of greater quadriceps force requirements and, thus, higher PFJ reaction force and stress.31,56 Moreover, increased knee flexion moment impulse can result from increased magnitude and/or duration of knee flexion moment. Based on the ensemble average curves of knee moments (FIGURE 2), higher knee flexion moment impulse observed in the progressors was contributed from both increased amplitude and duration of knee flexion moment. This suggests that PFJ OA progressors experienced higher PFJ loading over longer periods during each stride. As such, it is reasonable to suggest that these sagittal plane knee kinetic variables may be related to progression of cartilage lesions and BMELs at the PFJ.
The results of this study add to current knowledge regarding the biomechanical risk factors of PFJ OA. Recent studies have shown that individuals with isolated PFJ OA55 and combined PFJ and TFJ OA21 demonstrate higher knee flexion moment and flexion moment impulse during the second half of the stance phase. The findings of the current study also show these biomechanical factors to be related to the progression of PFJ OA. The second peak of knee flexion moment typically occurs during the second period of double-limb support, during which the knee continues to flex and body weight is transferred to the contralateral limb. An increased knee flexion moment can be a result of increased knee flexion angle and/or ground reaction force. The observed difference in the magnitude of knee flexion moment and impulse during the second half of stance was relatively small, which is consistent with the difference previously observed between individuals with and without PFJ OA.21,55 Given the highly repetitive nature of walking during daily activities, even a small increase in knee flexion moment over each step may result in a large increase in the cumulative loading on the PFJ over time. It must be kept in mind, however, that participants in this study presented with a high level of function. As such, they might have been more susceptible to a small increase in knee loading. Together, our findings show that increased knee flexion moment and impulse during late stance are associated not only with the presence but also with the progression of PFJ OA.
Based on the findings of this study, knee flexion moment and impulse during the first half of the stance phase were not associated with morphological progression of PFJ OA at 1 year. Although nonsignificant, PFJ OA progressors showed 22% and 25% lower peak knee flexion moment and flexion moment impulse, respectively, during the first half of the stance phase compared to nonprogressors (TABLE 2, FIGURE 2). This finding concurs with previous cross-sectional studies that reported nonsignificant but lower knee flexion moment55 and vasti force13 during the first half of the stance phase in individuals with PFJ OA compared to healthy controls. During loading response, the quadriceps contract eccentrically to perform shock absorption.44 The reduction in knee flexion moment and vasti force suggests a deficiency in quadriceps performance in individuals who have or show progression of PFJ OA. Further studies are warranted to investigate the relationship between lower extremity muscle performance and knee kinetics in this population.
The progression of PFJ OA, defined as changes in cartilage lesions and BMELs between baseline and 1 year, was assessed with a semi-quantitative MRI scoring system (WORMS). Though radiographic images are commonly used in clinical settings and have also been used in previous studies to determine the severity of PFJ OA,13,17,21,22,30 they do not allow direct assessment of cartilage morphology or the detection of early-stage OA.25,28,43,52 The MRI-based scoring system, WORMS, on the other hand, provides reliable measurements on subtle morphological changes associated with knee OA.28,45,49 As such, by utilizing WORMS, the findings of this study may better inform researchers of the biomechanical risk factors associated with early-stage or subtle progression of PFJ OA.
The observed percentage of participants who showed progression of morphological changes associated with PFJ OA was lower in this study (16.4%) compared to that reported in the previous study, which had a combined cohort of those with PFJ and TFJ OA.5,46 This might have been due to participants in this study being younger and having less severe baseline OA, which was reflected in a lower level of pain and a higher level of function (TABLE 1). As age and OA severity have been associated with OA progression,7 it is reasonable that a lower progression rate was observed in this study than in other studies. The progression group consisted of a relatively higher percentage of women. This is in agreement with the literature that women have a higher risk of developing PFJ disorders and show a higher progression rate of OA.8,27,53 Consistent with previous literature,7 our data show that individuals with existing PFJ OA demonstrate higher progression rates. More than one quarter of those who presented with baseline PFJ OA (28.5%) showed progression of the disease at 1 year, whereas only 6.1% of the individuals without baseline PFJ OA showed morphological changes related to PFJ OA at 1 year.
Certain limitations should be considered when interpreting the results of this study. First, a relatively small sample size and short follow-up times were used. Future studies may consider expanding the follow-up times beyond 1 year to explore more significant progression of OA that would likely affect a larger percentage of the study sample. Second, the observed differences in knee flexion moment and impulse between the progressors and nonprogressors are relatively small, despite a large effect size for group differences (Cohen d greater than 1). Further research is needed to investigate the relationship of knee flexion moment and impulse with clinical symptoms (ie, pain, function, quality of life). Third, because a greater proportion of female participants (67.2%) were recruited in this study, caution should be taken when generalizing the findings to the overall population. Finally, individuals with TFJ OA, defined by cartilage lesions shown on MRI, were excluded from this study to eliminate potential interference of TFJ OA with gait biomechanics. Further investigations are warranted to verity whether the observed relationships occur in individuals with combined PFJ and TFJ OA.
CONCLUSION
The findings of this study indicate that PFJ OA progressors exhibit higher peak knee flexion moment and flexion moment impulse during the second half of the stance phase at baseline. Logistic regression analysis showed that higher peak knee flexion moment during the second half of the stance phase was associated with progression of PFJ OA at 1-year follow-up. Knee flexion moment and moment impulse during the first half of stance were not associated with PFJ OA progression.
KEY POINTS.
FINDINGS
Patellofemoral joint OA progressors demonstrated higher peak knee flexion moment and flexion moment impulse during the second half of stance at baseline compared to nonprogressors. Logistic regressions showed that higher peak knee flexion moment during the second half of the stance phase was significantly associated with PFJ OA progression at 1 year (adjusted OR = 3.3).
IMPLICATIONS
An increase in knee flexion moment and impulse during the second half of the stance phase may need to be considered when treating individuals with or at risk of PFJ OA.
CAUTION
The observed difference in knee kinetics is relatively small and the 1-year follow-up was relatively brief. Some morphological changes of OA may develop over a longer period.
Acknowledgments
The authors would like to thank Cynthia Conti for her assistance with data collection and Danielle C. Kassimatis for her assistance with data analysis and management.
This research was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases grants R01AR062370, R01AR046905, and P50 AR060752.
Footnotes
The protocol for this study was approved by the Committee of Human Research at the University of California San Francisco.
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article.
REFERENCES
- 1.Alizai H, Virayavanich W, Joseph GB, et al. Cartilage lesion score: comparison of a quantitative assessment score with established semiquantitative MR scoring systems. Radiology. 2014;271:479–487. doi: 10.1148/radiol.13122056. http://dx.doi.org/10.1148/radiol.13122056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Favre J. The nature of in vivo mechanical signals that influence cartilage health and progression to knee osteoarthritis. Curr Rheumatol Rep. 2014;16:463. doi: 10.1007/s11926-014-0463-2. http://dx.doi.org/10.1007/s11926-014-0463-2. [DOI] [PubMed] [Google Scholar]
- 3.Baum T, Joseph GB, Arulanandan A, et al. Association of magnetic resonance imaging-based knee cartilage T2 measurements and focal knee lesions with knee pain: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 2012;64:248–255. doi: 10.1002/acr.20672. http://dx.doi.org/10.1002/acr.20672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baum T, Stehling C, Joseph GB, et al. Changes in knee cartilage T2 values over 24 months in subjects with and without risk factors for knee osteoarthritis and their association with focal knee lesions at baseline: data from the Osteoarthritis Initiative. J Magn Reson Imaging. 2012;35:370–378. doi: 10.1002/jmri.22834. http://dx.doi.org/10.1002/jmri.22834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bennell KL, Bowles KA, Wang Y, Cicuttini F, Davies- Tuck M, Hinman RS. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis. 2011;70:1770–1774. doi: 10.1136/ard.2010.147082. http://dx.doi.org/10.1136/ard.2010.147082. [DOI] [PubMed] [Google Scholar]
- 6.Bennell KL, Creaby MW, Wrigley TV, et al. Bone marrow lesions are related to dynamic knee loading in medial knee osteoarthritis. Ann Rheum Dis. 2010;69:1151–1154. doi: 10.1136/ard.2009.118182. http://dx.doi.org/10.1136/ard.2009.118182. [DOI] [PubMed] [Google Scholar]
- 7.Blagojevic M, Jinks C, Jeffery A, Jordan KP. Risk factors for onset of osteoarthritis of the knee in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2010;18:24–33. doi: 10.1016/j.joca.2009.08.010. http://dx.doi.org/10.1016/j.joca.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 8.Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20:725–730. doi: 10.1111/j.1600-0838.2009.00996.x. http://dx.doi.org/10.1111/j.1600-0838.2009.00996.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buck RJ, Wirth W, Dreher D, Nevitt M, Eckstein F. Frequency and spatial distribution of cartilage thickness change in knee osteoarthritis and its relation to clinical and radiographic covariates – data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2013;21:102–109. doi: 10.1016/j.joca.2012.10.010. http://dx.doi.org/10.1016/j.joca.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Carnes J, Stannus O, Cicuttini F, Ding C, Jones G. Knee cartilage defects in a sample of older adults: natural history, clinical significance and factors influencing change over 2.9 years. Osteoarthritis Cartilage. 2012;20:1541–1547. doi: 10.1016/j.joca.2012.08.026. http://dx.doi.org/10.1016/j.joca.2012.08.026. [DOI] [PubMed] [Google Scholar]
- 11.Chehab EF, Favre J, Erhart-Hledik JC, Andriacchi TP. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:1833–1839. doi: 10.1016/j.joca.2014.08.009. http://dx.doi.org/10.1016/j.joca.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheung PP, Gossec L, Dougados M. What are the best markers for disease progression in osteoarthritis (OA)? Best Pract Res Clin Rheumatol. 2010;24:81–92. doi: 10.1016/j.berh.2009.08.009. http://dx.doi.org/10.1016/j.berh.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 13.Crossley KM, Dorn TW, Ozturk H, van den Noort J, Schache AG, Pandy MG. Altered hip muscle forces during gait in people with patellofemoral osteoarthritis. Osteoarthritis Cartilage. 2012;20:1243–1249. doi: 10.1016/j.joca.2012.07.011. http://dx.doi.org/10.1016/j.joca.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 14.Ding C, Cicuttini F, Scott F, Boon C, Jones G. Association of prevalent and incident knee cartilage defects with loss of tibial and patellar cartilage: a longitudinal study. Arthritis Rheum. 2005;52:3918–3927. doi: 10.1002/art.21474. http://dx.doi.org/10.1002/art.21474. [DOI] [PubMed] [Google Scholar]
- 15.Dore D, Martens A, Quinn S, et al. Bone marrow lesions predict site-specific cartilage defect development and volume loss: a prospective study in older adults. Arthritis Res Ther. 2010;12:R222. doi: 10.1186/ar3209. http://dx.doi.org/10.1186/ar3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Driban JB, Lo GH, Lee JY, et al. Quantitative bone marrow lesion size in osteoarthritic knees correlates with cartilage damage and predicts longitudinal cartilage loss. BMC Musculoskelet Disord. 2011;12:217. doi: 10.1186/1471-2474-12-217. http://dx.doi.org/10.1186/1471-2474-12-217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. Does isolated patellofemoral osteoarthritis matter? Osteoarthritis Cartilage. 2009;17:1151–1155. doi: 10.1016/j.joca.2009.03.016. http://dx.doi.org/10.1016/j.joca.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 18.Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis—it all depends on your point of view. Rheumatology (Oxford) 2006;45:757–760. doi: 10.1093/rheumatology/kei270. http://dx.doi.org/10.1093/rheumatology/kei270. [DOI] [PubMed] [Google Scholar]
- 19.Eckstein F, Cicuttini F, Raynauld JP, Waterton JC, Peterfy C. Magnetic resonance imaging (MRI) of articular cartilage in knee osteoarthritis (OA): morphological assessment. Osteoarthritis Cartilage. 2006;14:46–75. doi: 10.1016/j.joca.2006.02.026. http://dx.doi.org/10.1016/j.joca.2006.02.026. [DOI] [PubMed] [Google Scholar]
- 20.Eckstein F, Cotofana S, Wirth W, et al. Greater rates of cartilage loss in painful knees than in pain-free knees after adjustment for radiographic disease stage: data from the Osteoarthritis Initiative. Arthritis Rheum. 2011;63:2257–2267. doi: 10.1002/art.30414. http://dx.doi.org/10.1002/art.30414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farrokhi S, O’Connell M, Fitzgerald GK. Altered gait biomechanics and increased knee-specific impairments in patients with coexisting tibiofemoral and patellofemoral osteoarthritis. Gait Posture. 2015;41:81–85. doi: 10.1016/j.gaitpost.2014.08.014. http://dx.doi.org/10.1016/j.gaitpost.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fok LA, Schache AG, Crossley KM, Lin YC, Pandy MG. Patellofemoral joint loading during stair ambulation in people with patellofemoral osteoarthritis. Arthritis Rheum. 2013;65:2059–2069. doi: 10.1002/art.38025. http://dx.doi.org/10.1002/art.38025. [DOI] [PubMed] [Google Scholar]
- 23.Foroughi N, Smith R, Vanwanseele B. The association of external knee adduction moment with biomechanical variables in osteoarthritis: a systematic review. Knee. 2009;16:303–309. doi: 10.1016/j.knee.2008.12.007. http://dx.doi.org/10.1016/j.knee.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 24.Griffin TM, Guilak F. The role of mechanical loading in the onset and progression of osteoarthritis. Exerc Sport Sci Rev. 2005;33:195–200. doi: 10.1097/00003677-200510000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Guermazi A, Roemer FW, Felson DT, Brandt KD. Motion for debate: osteoarthritis clinical trials have not identified efficacious therapies because traditional imaging outcome measures are inadequate. Arthritis Rheum. 2013;65:2748–2758. doi: 10.1002/art.38086. http://dx.doi.org/10.1002/art.38086. [DOI] [PubMed] [Google Scholar]
- 26.Guilak F, Fermor B, Keefe FJ, et al. The role of biomechanics and inflammation in cartilage injury and repair. Clin Orthop Relat Res. 2004:17–26. doi: 10.1097/01.blo.0000131233.83640.91. [DOI] [PubMed] [Google Scholar]
- 27.Hanna FS, Teichtahl AJ, Wluka AE, et al. Women have increased rates of cartilage loss and progression of cartilage defects at the knee than men: a gender study of adults without clinical knee osteoarthritis. Menopause. 2009;16:666–670. doi: 10.1097/gme.0b013e318198e30e. http://dx.doi.org/10.1097/gme.0b013e318198e30e. [DOI] [PubMed] [Google Scholar]
- 28.Hayashi D, Guermazi A, Kwoh CK. Clinical and translational potential of MRI evaluation in knee osteoarthritis. Curr Rheumatol Rep. 2014;16:391. doi: 10.1007/s11926-013-0391-6. http://dx.doi.org/10.1007/s11926-013-0391-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heino Brechter J, Powers CM. Patellofemoral stress during walking in persons with and without patellofemoral pain. Med Sci Sports Exerc. 2002;34:1582–1593. doi: 10.1097/00005768-200210000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Hinman RS, Lentzos J, Vicenzino B, Crossley KM. Is patellofemoral osteoarthritis common in middle-aged people with chronic patellofemoral pain? Arthritis Care Res (Hoboken) 2014;66:1252–1257. doi: 10.1002/acr.22274. http://dx.doi.org/10.1002/acr.22274. [DOI] [PubMed] [Google Scholar]
- 31.Ho KY, Blanchette MG, Powers CM. The influence of heel height on patellofemoral joint kinetics during walking. Gait Posture. 2012;36:271–275. doi: 10.1016/j.gaitpost.2012.03.008. http://dx.doi.org/10.1016/j.gaitpost.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 32.Hunter DJ, March L, Sambrook PN. The association of cartilage volume with knee pain. Osteoarthritis Cartilage. 2003;11:725–729. doi: 10.1016/s1063-4584(03)00160-2. http://dx.doi.org/10.1016/S1063-4584(03)00160-2. [DOI] [PubMed] [Google Scholar]
- 33.Kean CO, Hinman RS, Bowles KA, Cicuttini F, Davies-Tuck M, Bennell KL. Comparison of peak knee adduction moment and knee adduction moment impulse in distinguishing between severities of knee osteoarthritis. Clin Biomech (Bristol, Avon) 2012;27:520–523. doi: 10.1016/j.clinbiomech.2011.12.007. http://dx.doi.org/10.1016/j.clinbiomech.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 34.Kennedy D, Stratford PW, Pagura SM, Walsh M, Woodhouse LJ. Comparison of gender and group differences in self-report and physical performance measures in total hip and knee arthroplasty candidates. J Arthroplasty. 2002;17:70–77. doi: 10.1054/arth.2002.29324. http://dx.doi.org/10.1054/arth.2002.29324. [DOI] [PubMed] [Google Scholar]
- 35.Kornaat PR, Bloem JL, Ceulemans RY, et al. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology. 2006;239:811–817. doi: 10.1148/radiol.2393050253. http://dx.doi.org/10.1148/radiol.2393050253. [DOI] [PubMed] [Google Scholar]
- 36.Landry SC, McKean KA, Hubley-Kozey CL, Stanish WD, Deluzio KJ. Knee biomechanics of moderate OA patients measured during gait at a self-selected and fast walking speed. J Biomech. 2007;40:1754–1761. doi: 10.1016/j.jbiomech.2006.08.010. http://dx.doi.org/10.1016/j.jbiomech.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Lo GH, McAlindon TE, Niu J, et al. Bone marrow lesions and joint effusion are strongly and independently associated with weight-bearing pain in knee osteoarthritis: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2009;17:1562–1569. doi: 10.1016/j.joca.2009.06.006. http://dx.doi.org/10.1016/j.joca.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lynch JA, Roemer FW, Nevitt MC, et al. Comparison of BLOKS and WORMS scoring systems part I. Cross sectional comparison of methods to assess cartilage morphology, meniscal damage and bone marrow lesions on knee MRI: data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2010;18:1393–1401. doi: 10.1016/j.joca.2010.08.017. http://dx.doi.org/10.1016/j.joca.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McAlindon TE, Snow S, Cooper C, Dieppe PA. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Ann Rheum Dis. 1992;51:844–849. doi: 10.1136/ard.51.7.844. http://dx.doi.org/10.1136/ard.51.7.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McLean SG, Su A, van den Bogert AJ. Development and validation of a 3-D model to predict knee joint loading during dynamic movement. J Biomech Eng. 2003;125:864–874. doi: 10.1115/1.1634282. http://dx.doi.org/10.1115/1.1634282. [DOI] [PubMed] [Google Scholar]
- 41.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. http://dx.doi.org/10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mündermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–2844. doi: 10.1002/art.21262. http://dx.doi.org/10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 43.Palmer AJ, Brown CP, McNally EG, et al. Noninvasive imaging of cartilage in early osteoarthritis. Bone Joint J. 2013;95-B:738–746. doi: 10.1302/0301-620X.95B6.31414. http://dx.doi.org/10.1302/0301-620X.95B6.31414. [DOI] [PubMed] [Google Scholar]
- 44.Perry J, Burnfield JM. Gait Analysis: Normal and Pathological Function. 2nd. Thorofare, NJ: SLACK Incorporated; 2010. [Google Scholar]
- 45.Peterfy CG, Guermazi A, Zaim S, et al. Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage. 2004;12:177–190. doi: 10.1016/j.joca.2003.11.003. http://dx.doi.org/10.1016/j.joca.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 46.Phan CM, Link TM, Blumenkrantz G, et al. MR imaging findings in the follow-up of patients with different stages of knee osteoarthritis and the correlation with clinical symptoms. Eur Radiol. 2006;16:608–618. doi: 10.1007/s00330-005-0004-5. http://dx.doi.org/10.1007/s00330-005-0004-5. [DOI] [PubMed] [Google Scholar]
- 47.Prasad AP, Nardo L, Schooler J, Joseph GB, Link TM. T1ρ and T2 relaxation times predict progression of knee osteoarthritis. Osteoarthritis Cartilage. 2013;21:69–76. doi: 10.1016/j.joca.2012.09.011. http://dx.doi.org/10.1016/j.joca.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rejeski WJ, Ettinger WH, Jr, Schumaker S, James P, Burns R, Elam JT. Assessing performance-related disability in patients with knee osteoarthritis. Osteoarthritis Cartilage. 1995;3:157–167. doi: 10.1016/s1063-4584(05)80050-0. http://dx.doi.org/10.1016/S1063-4584(05)80050-0. [DOI] [PubMed] [Google Scholar]
- 49.Roemer FW, Kwoh CK, Hannon MJ, et al. Semiquantitative assessment of focal cartilage damage at 3 T MRI: a comparative study of dual echo at steady state (DESS) and intermediate-weighted (IW) fat suppressed fast spin echo sequences. Eur J Radiol. 2011;80:e126–e131. doi: 10.1016/j.ejrad.2010.07.025. http://dx.doi.org/10.1016/j.ejrad.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 50.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. http://dx.doi.org/10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) – validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17. doi: 10.1186/1477-7525-1-17. http://dx.doi.org/10.1186/1477-7525-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schiphof D, Oei EH, Hofman A, Waarsing JH, Weinans H, Bierma-Zeinstra SM. Sensitivity and associations with pain and body weight of an MRI definition of knee osteoarthritis compared with radiographic Kellgren and Lawrence criteria: a population-based study in middle-aged females. Osteoarthritis Cartilage. 2014;22:440–446. doi: 10.1016/j.joca.2013.12.017. http://dx.doi.org/10.1016/j.joca.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 53.Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769–781. doi: 10.1016/j.joca.2005.04.014. http://dx.doi.org/10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 54.Stefanik JJ, Niu J, Gross KD, Roemer FW, Guermazi A, Felson DT. Using magnetic resonance imaging to determine the compartmental prevalence of knee joint structural damage. Osteoarthritis Cartilage. 2013;21:695–699. doi: 10.1016/j.joca.2013.02.003. http://dx.doi.org/10.1016/j.joca.2013.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Teng HL, MacLeod TD, Kumar D, Link TM, Majumdar S, Souza RB. Individuals with isolated patellofemoral joint osteoarthritis exhibit higher mechanical loading at the knee during the second half of the stance phase. Clin Biomech (Bristol, Avon) 2015;30:383–390. doi: 10.1016/j.clinbiomech.2015.02.008. http://dx.doi.org/10.1016/j.clinbiomech.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Teng HL, Powers CM. Sagittal plane trunk posture influences patellofemoral joint stress during running. J Orthop Sports Phys Ther. 2014;44:785–792. doi: 10.2519/jospt.2014.5249. http://dx.doi.org/10.2519/jospt.2014.5249. [DOI] [PubMed] [Google Scholar]
- 57.Wu G, Siegler S, Allard P, et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—part I: ankle, hip, spine. J Biomech. 2002;35:543–548. doi: 10.1016/s0021-9290(01)00222-6. http://dx.doi.org/10.1016/S0021-9290(01)00222-6. [DOI] [PubMed] [Google Scholar]