Abstract
Branchial pouch-derived anomalies may arise from remnants of the first, second, or third/fourth branchial arches. Branchial pouch-related structures are found within the thyroid gland in the form of solid cell rests, epithelial lined cyst with or without an associated lymphoid component, thymic and/or parathyroid tissue, and less commonly in the form of heterotopic cartilage. We present a rare case of left solid thyroid swelling nearby two cervical nodules in a seven-year-old female with a clinical diagnosis suggestive of malignant thyroid tumor with metastasis to the cervical lymph nodes. Histopathological examination revealed that it was compatible with third/fourth branchial pouch-derived anomaly composed of mature cartilage and thymic and parathyroid tissues for clinical and radiological correlations.
Keywords: branchial pouch, anomaly, thyroid gland, thymus, parathyroid gland, cartilage
Introduction
Among the congenital masses related to embryonic remnants, ∼70% were thyroglossal duct sinuses and cysts, 25% were branchial cysts and sinuses, and 5% were cystic hygromas.1 The branchial pouch-derived anomalies represented the second major cause of the head and neck pathology in childhood, presenting about 17% of all pediatric cervical masses. Among the branchial arch-derived anomalies, the second branchial arch anomaly was the most common,2 followed by the first branchial arch anomaly. The third/fourth branchial arch anomalies, on the other hand, were the least presented cases.3 The presence of parathyroid and thymic tissues suggested that the anomaly was of the third branchial arch, as this was where inferior parathyroid gland and the thymus developed; however, as the superior parathyroid gland and accessory thymus (that could be seen in some patients) developed from the fourth branchial arch, the histopathological differentiation between the third and fourth branchial anomalies became unfavored.4 Moreover, with the surgical exploration, the differentiation might be obvious that in the third branchial arch anomaly, the congenital tract would pass above the superior laryngeal nerve, but it would be below superior laryngeal nerve in cases of fourth branchial pouch anomaly.5 Barium swallow, direct laryngoscope, and magnetic resonance imaging (MRI) with surgical exploration are the best diagnostic tools for this anomaly.6
The third/fourth branchial arch anomaly is commonly presented on the left side of the neck. The patient usually has neck abscess or acute suppurative thyroiditis.5,7
In this report, we present a rare case of third/fourth branchial pouch-derived anomaly in a seven-year-old female. The anomaly presented by solid noninflamed left thyroid and cervical neck masses instead of recurrent inflamed cystic neck lesion. The histopathological examination of the thyroid swelling revealed mature benign cartilage.
Case Report
History and examination
A seven-year-old female patient presented to the Department of Pediatric Surgery in Ain Shams University Hospital. For the past few months, she complained of progressive enlargement of neck swelling. On examination, it was found that there was left thyroid swelling that moved up and down with deglutition as well as left nearby two solid cervical nodules that were clinically suspected to be enlarged lymph nodes. The swellings were not tender with no signs of inflammation; thus, clinical suspicion of malignancy was favored.
Thyroid function tests were normal (T3, T4, and Thyroid stimulating hormone (TSH)). Neck ultrasound showed solitary solid left thyroid nodule about 2 × 2 cm with nearby left cervical two mobile nodules each about 0.5 cm in diameter. Technetium scan revealed cold solitary thyroid nodule.
Clinical general examination and investigations (complete blood count (CBC), liver function test, and kidney function test) were normal.
Management and histology
The surgeon decision was to do excision biopsy of the masses with frozen section examination. Three tissue pieces were received. The largest was the thyroid nodule measuring 3 × 3 × 1 cm with the cut section showing well-defined whitish firm glistening nodule about 2 × 2 cm surrounded by a rim of thyroid tissue. The other two pieces were small, well-defined, and tan colored, each about 0.5 cm in the longest dimension; they were totally submitted as such. Microscopic examination of the thyroid nodule revealed a well-defined mature cartilage, surrounded by unremarkable thyroid tissue (Fig. 1). Sections examined from the smaller separate tissue pieces revealed mature thymic and parathyroid tissues with tiny focus of thyroid follicles (Figs. 2 and 3). The permanent paraffin sections further confirm the histological findings that were compatible with the third/fourth branchial pouch-derived anomaly.
Figure 1.
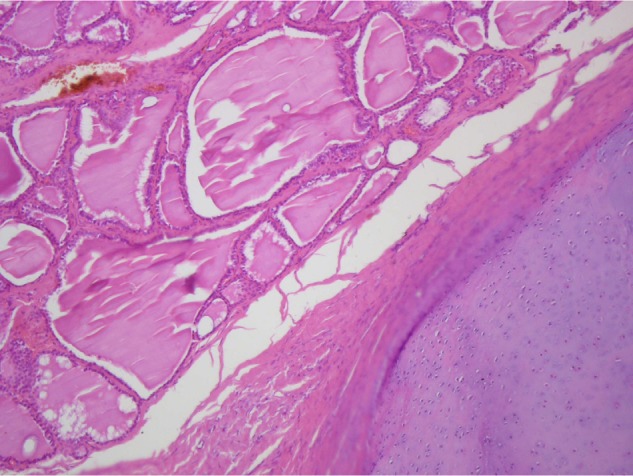
Well-defined mature cartilage surrounded by thyroid tissue (H&E, ×100).
Figure 2.
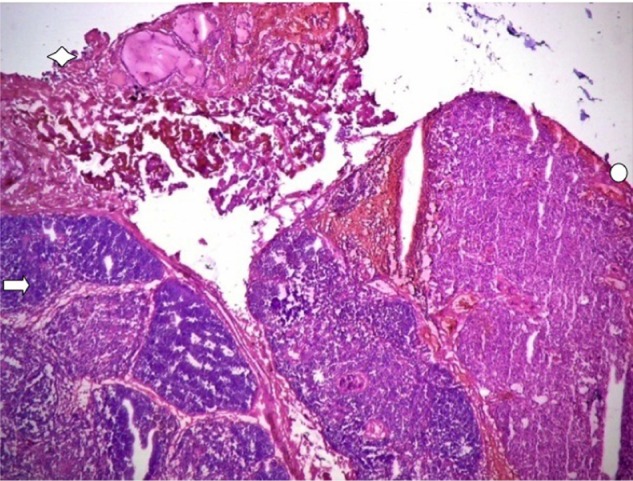
Thyroid tissue (up, labeled with a star), thymic tissue (labeled with an arrow), and parathyroid tissue (labeled with a circle) (H&E, ×40).
Figure 3.
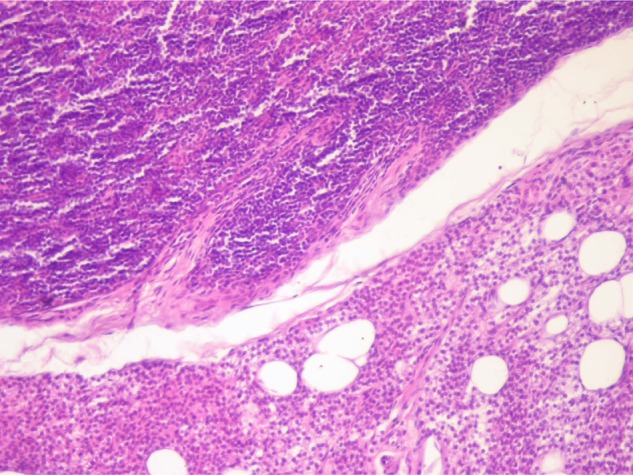
Thymic tissue (top) and parathyroid tissue (bottom) (H&E, ×200).
Discussion
Presentation and differential diagnosis of lateral neck swellings
The reported case was presented by neck swelling that moved upward with deglutition with nearby cervical nodules. The swellings were solid rather than cystic with no signs of inflammation or previous history of recurrent infection. This presentation increased the likelihood of cancer diagnosis. Moreover, the clinical diagnosis of branchial pouch-derived anomalies was not considered, especially the finding that the largest swelling was inside the thyroid gland, which was an uncommon location.8
Third/fourth pharyngeal pouch-derived anomaly is the rarest among the branchial anomalies.6 It may cause wide range of clinical manifestations; it may show minimal or serious obstructive symptoms with few cases that may be presented by thyroid swelling.9 They are usually presented as cystic lesions, so they must be differentiated from other similar lesions of the neck, such as cystic hygromas, thyroglossal cyst, dermoid cyst, cervical bronchogenic cysts, cystic neuromas, and abscesses. Rarely, they are solid with many differential diagnostic lesions, including primary and metastatic tumors, lipomas, and fibrous hamartoma of infancy.10
Ultrasound, CT, and MRI scans are helpful in the assessment of the solid and cystic cervical swellings.11 Together with the histological evaluation, the final diagnosis can be made.6
Diagnosis of the third/fourth branchial pouch anomaly
The thyroid lesion was examined in the frozen sections that were further fixed for the preparation of paraffin sections; it showed mature cartilage with no cytological features of malignancy within unremarkable thyroid tissue.
In the further examination of the other two left lateral cervical nodules, they showed mature thymic and parathyroid tissues with small foci of thyroid tissue that also revealed no cytological criteria of malignancy. No sinus tract with epithelial lining could be identified. As our case was a child, the possibilities of congenital anomaly or tumor of a childhood were considered, and thyroid teratoma was one of the differential diagnoses of this case; the presence of cartilage within the thyroid gland and the age of the patient together with the clinical suggestion of thyroid neoplasia all favored this diagnosis. However, thyroid teratoma is a rare neoplastic lesion that can develop within the thyroid gland of the children with the benign variant being more common than the malignant.12 Therefore, many deeper sections were examined searching for any other components of teratoma, such as glial tissue, respiratory or gastric glands, and muscular or adipose tissue. Also, we tried to find out any primitive neuroepithelial elements that characterize immature teratoma, but we found nothing.
Although the clinical impression of the cold thyroid nodule was neoplastic when considering the lateral cervical nodules as metastatic, the combined histopathological findings of the parathyroid, thymic tissue, and mature cartilage favored the diagnosis of the congenital anomaly of the third/fourth branchial pouch. Rosai and Ackerman12 reported that cartilage, thymic, and parathyroid tissues can be components of the branchial pouch anomaly in the thyroid. Moreover, Prasad et al.6 reported that branchial pouch anomaly can be presented as a cold thyroid nodule. They added that this type of anomaly was the least common among other branchial arch anomalies presenting <1% of cases.
Differences in results in relation to other studies
In spite of the fact that branchial pouch anomalies are congenital lesions, they are usually present late in life. In our case, the child was seven- years old that was in concordance with the mean age found in a study by Thomas et al.13 They reported that the mean age of the third or fourth branchial anomaly was 84.6 months (about seven years).
The absence of signs of inflammation or discharging fistula in our case challenged the surgeons to suspect branchial pouch anomalies. In a study done by Choi and Zalzal,14 they found that the most common presenting features of these anomalies were discharging sinuses, cervical mass, and repeated infection. Moreover, Hallak et al.15 added that the left neck side being more affected than the right.
Conclusion
We should be minded that branchial pouch-derived anomalies are the second common causes for pediatric cervical swellings after the thyroglossal anomalies. Although third/fourth branchial arch anomaly is rare, it should be considered when a child is presented by cold thyroid nodule especially on the left side.
Footnotes
ACADEMIC EDITOR: Dama Laxminarayana, Editor in Chief
PEER REVIEW: Six peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1,284 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE). Provenance: the authors were invited to submit this paper.
Author Contributions
Conceived and designed the experiments: MHAN, EAI, SASE. Analyzed the data: MHAN, EAI, SASE. Wrote the first draft of the manuscript: SASE. Contributed to the writing of the manuscript: EAI, SASE. Agree with manuscript results and conclusions: MHAN, EAI, SASE. Jointly developed the structure and arguments for the paper: EAI, SASE. Made critical revisions and approved final version: MHAN, EAI, SASE. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Thomaidis V, Seretis K, Tamiolakis D, Papadopoulos N, Tsamis I. Branchial cysts. A report of 4 cases. Acta Dermatovenerol Alp Pannonica Adriat. 2006;15(2):85–9. [PubMed] [Google Scholar]
- 2.Berseth CL, Poenaru D. Structural anomalies of GIT. In: Tacusch HW, Ballard RA, Gleason CA, editors. Avery’s Diseases of the Newborn. 8th ed. Philadelphia, PA: WB Saunders; 2005. pp. 1086–7. [Google Scholar]
- 3.Al-Mufarrej FM, Stoddard DG, Bite U. Branchial arch anomalies: rates of recurrence and malignant degeneration. Plast Reconstr Surg. 2012;130(5S–1):1–7. [Google Scholar]
- 4.Al-Shaiji AS, Bukhari MA. Endoscopic management of fourth branchial arch anomaly: a case report. Egypt J Ear Nose Throat Allied Sci. 2013;14(1):33–6. [Google Scholar]
- 5.Nicoucar K, Giger R, Pope HG, Jr, Jaecklin T, Dulguerov P. Management of congenital fourth branchial arch anomalies: a review and analysis of published cases. J Pediatr Surg. 2009;44(7):1432–9. doi: 10.1016/j.jpedsurg.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 6.Prasad SC, Azeez A, Thada ND, Rao P, Bacciu A, Prasad KC. Branchial anomalies: diagnosis and management. Int J Otolaryngol. 2014;2014:237015. doi: 10.1155/2014/237015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kucur C, Kinis V, Eren Y, Gursel AO. Bilateral branchial cleft anomaly type two and type three seen together. J Clin Exp Invest. 2012;3(1):99–101. [Google Scholar]
- 8.Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th ed. Philadelphia, PA: Elsevier Saunders; 2005. [Google Scholar]
- 9.Vaidya S, Pagare RS, Sharma VK. Lateral cervical cyst. Internet J Otorhinolaryngol. 2008;7:1–6. [Google Scholar]
- 10.Yoo TK, Kim SH, Kim HS, Kim HY, Park KW. Fourth branchial anomaly presenting with a lateral neck mass in a neonate. J Neonatal Surg. 2014;3(3):34. [PMC free article] [PubMed] [Google Scholar]
- 11.Patel AB, Hinni ML. The fourth branchial complex anomaly: a rare clinical entity. Case Rep Otolaryngol. 2011;2011:958652. doi: 10.1155/2011/958652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosai J, Ackerman LV. Rosai and Ackerman’s Surgical Pathology. 11th ed. Vol. 2. Elsevier Mosby; St. Louis, MO, USA: 2011. [Google Scholar]
- 13.Thomas B, Shroff M, Frote V, Blaser S, James A. Revisiting imaging features and the embryologic basis of third and fourth branchial anomalies. AJNR Am J Neuroradiol. 2010;31(4):755–60. doi: 10.3174/ajnr.A1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi SS, Zalzal GH. Branchial anomalies: a review of 52 cases. Laryngoscope. 1995;105(9 pt 1):909–13. doi: 10.1288/00005537-199509000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Hallak B, Bouayed S, Leishman C, Sandu K. Residual fistula of fourth branchial arch anomalies and recurrent left side cervical abscess: clinical case and review of literature. Case Rep Otolaryngol. 2014;2014:931279. doi: 10.1155/2014/931279. [DOI] [PMC free article] [PubMed] [Google Scholar]


