The kidney plays many important roles in maintaining health, ranging from activation of hormones to maintaining stable levels of key molecule in the blood to excretion of toxins. Most consider the kidneys second only to the liver in importance for toxin elimination. However, considering that 20% to 25% of cardiac output goes through these tiny organs, allowing them to filter the blood a remarkable 60 times per day, a case could be made that they are actually more important than the liver for toxin elimination. They rid the body of unwanted products of metabolism such as ammonia, urea, uric acid, creatinine, end products of hemoglobin metabolism, and hormone metabolites; toxins that have been made water soluble by phase 2 in the liver; and direct excretion of industrial toxins, such as heavy metals and a number of new-to-nature molecules. They also excrete nutrients or food constituents when consumed in excess, such as salt, vitamin C, B vitamins, and others.
One of the big challenges for the kidneys is that although they are effective at removing many toxins from the blood, some are difficult to then excrete into the urine. This means they accumulate in the kidneys and as their concentration increases, they can cause disproportionate damage to the kidneys. Cadmium illustrates this problem well.
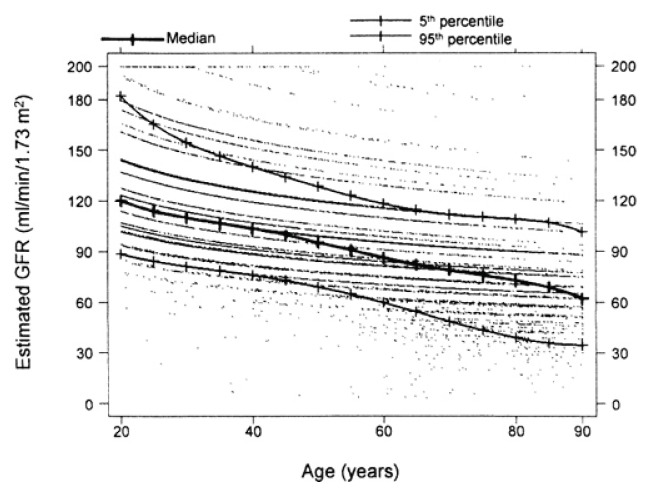
Unfortunately, we are now exposed to such a high toxic load in the modern world that loss of function with aging—as can be seen in Figure 1—is considered “normal.” A 90-year-old has only one-third to one-half of the kidney function of a 20-year-old. This means a significant decrease in ability to rid the body of many toxins and helps explain why almost everyone becomes sicker with aging. Once again, “normal” is not healthy.
Figure 1.
Deterioration in Kidney Function With Aging1
Abbreviation: GFR, glomerular filtration rate.
Because this is a huge topic, I am breaking my editorial into 2 parts: part 1, causes; and part 2, intervention. The latter will be published in volume 15, issue 1.
Kidney Excretion of Toxins
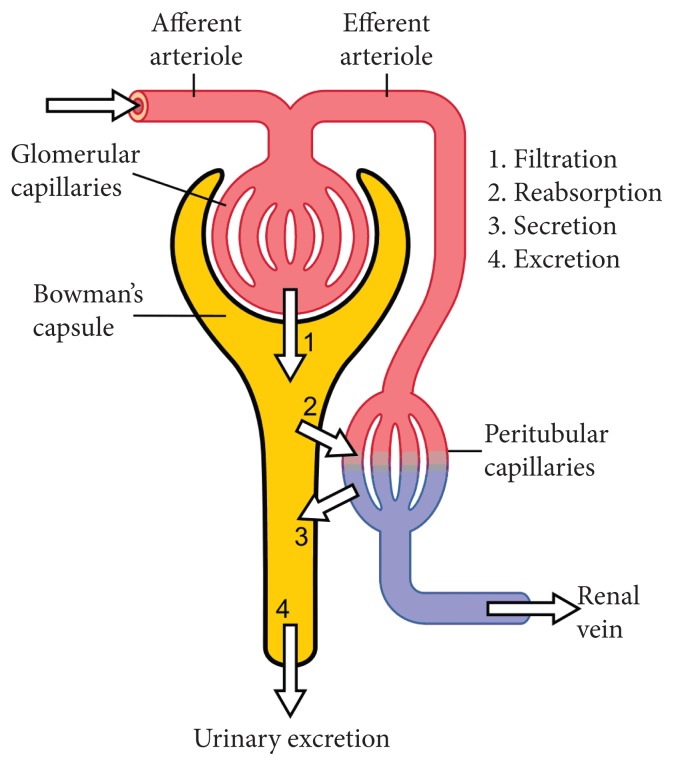
The kidney excretes toxins through essentially 3 mechanisms: (1) filtration through the glomeruli; (2) passive diffusion, typically from the distal tubules; and (3) active processes where the toxins are transported from the blood as well as into the urine. Note also in Figure 2: Some molecules are reabsorbed after being filtered by the glomeruli. This is a normal, controlled process by which the kidney maintains blood levels of key molecules within a narrow range.
Figure 2.
Kidney Excretion of Toxins
Excretion = Filtration − Reabsorption + Secretion
Basically, the glomeruli filter out of the blood almost all of the small- and medium-sized water-soluble molecules. Some are then reabsorbed, such as sodium, to ensure stable levels, blood volume, and other factors. In the proximal tubules are several active, energy-dependent processes such as organic anion transporters (OATs), organic anion transporting polypeptides (OATPs), organic cation transporters (OCTs), multidrug resistance-associated protein (MRP), multidrug resistance protein (MDR), and multidrug and toxic compound extrusion (MATE) that transport specific toxins out of the blood and, hopefully, into the urine. Finally, there is passive diffusion of the more fat soluble toxins across the tubules into the urine. These later process are quite slow but may be important for some toxins.
Several factors determine how well specific toxins are excreted by the kidneys. First, if the toxin is large or bound to protein, it does not pass through the glomeruli, so these have to be handled in other ways. Second, for toxins that are both water and fat soluble (the octanol/water partition coefficient), as their fat soluble increases, they are more likely passively reabsorbed in the distal tubules back into the kidneys and, potentially, back into the blood. Third, the active toxin excretion pathways have limited capacity and can be easily saturated. This limitation is used sometimes to decrease the rate at which an expensive or difficult-to-obtain drug is excreted so higher blood levels can be attained at lower dosages. Finally, as the body uses adenosine triphosphate (ATP) to actively pump out specific toxins, if the kidney’s mitochondria are not working well, these active processes do not work as well as needed. Worse, when the mitochondria are not working adequately, the kidneys also cannot protect their own tissue as high concentrations of toxins can that build up in the kidneys.
How the Kidneys Are Damaged
The kidney can be damaged by (1) poor blood flow, (2) mitochondrial dysfunction, (3) overload by high total level of toxins that may not be individually very toxic but become problematic when the total amount is high, (4) indirectly by toxins that cause general tissue damage, and (5) directly by toxins that are specifically harmful to the kidney tissues. These toxins can also come from within, such as from an unhealthy gut and externally from the many metals and chemicals in our industrialized world.
Heavy Metals
Cadmium, chromium, lead, mercury, platinum, and uranium are all nephrotoxic.
Cadmium
Cadmium is a huge problem. With a worrisome half-life of more than 10 years, it is very difficult to excrete. Cadmium is especially a problem for the kidney, which holds 50% of the total body burden. Once cadmium enters the body, much of it is bound to metallothioniens. These compounds are cleared through the glomeruli but are then reabsorbed by the tubules where they then become stuck. As the metallothioniens slowly degrade, highly toxic free cadmium is constantly released. Although it then passively migrates into the urine, it also causes oxidative stress to the tubules. The cadmium damage to the kidneys helps explain why it accounts for a surprising 20% of osteoporosis. The final stage in activation of vitamin D into its most active 1,25(OH)2D3 is in the kidneys. As the kidneys degenerate, they not only lose their ability to excrete toxins, but now are less able to perform their other functions. The main sources of cadmium are smoking and conventionally grown soybeans. Both are grown with high phosphate fertilizers that are contaminated with cadmium.
Mercury
The kidneys have a high affinity for mercury. In fact, within a few hours of exposure, 50% of the mercury that gets into the blood ends up in the kidneys. Mercury damages both the glomeruli and the tubules. Much of the tissue damage appears due to poisoning of the kidney mitochondria so there is not enough ATP for the cells to protect themselves from the toxins they are excreting. The main sources of mercury are so-called “silver” fillings, which are actually 55% mercury and eating large fish. (See my editorials from February 20092 and April 20093.)
Persistent Organic Pollutants
The persistent organic pollutants (POPs) are new-to-nature molecules specifically designed for special purposes and to be difficult to break down. They range from herbicides and pesticides, to nonstick coatings, to fire retardants. Our patients are as contaminated with these chemicals as the environment. As they are typically mostly fat soluble they are particularly damaging to the kidneys. Research is still early on their long-term health effects as many have been created relatively recently.
Many of these chemicals are classified as halogenated hydrocarbons and are so difficult to detoxify or excrete that they have half-lives measured in months to years. Following is a brief discussion of just a few of those with serious nephrotoxicity.
Fluorinated Hydrocarbons
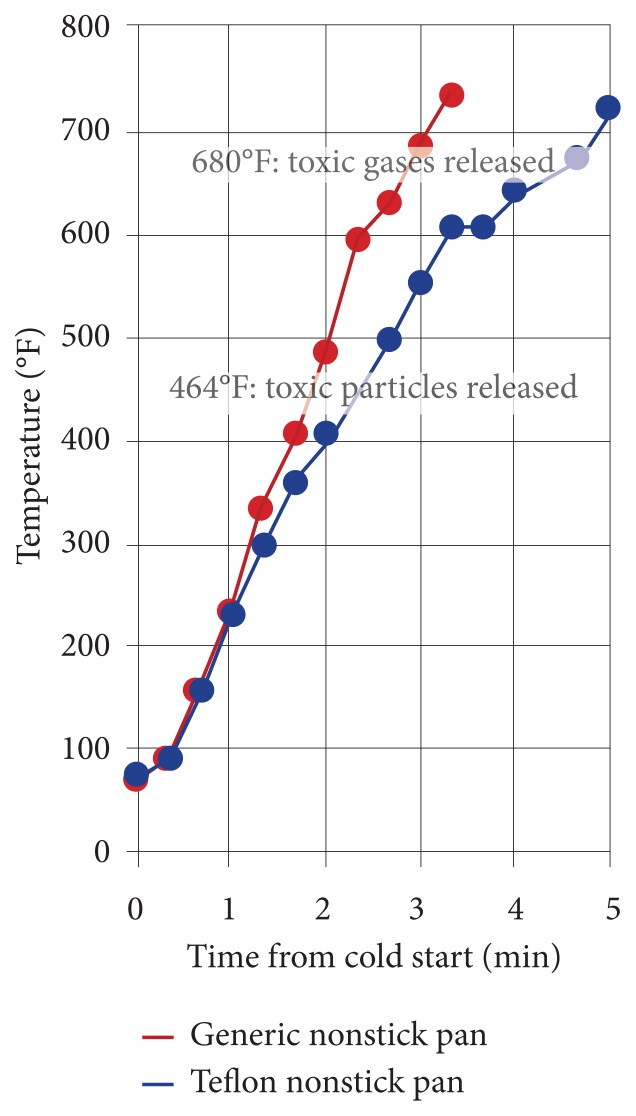
Tetrafluoroethylene and similar compounds are polymerized to produce polytetrafluoroethylene (PTFE) polymers, such as Teflon. This class of compounds is used as nonstick coatings on pots and pans; in clothing that is waterproof, but breathable; for stain prevention on carpet and upholstery; and for other purposes. Although these nonstick coatings are supposedly inert, the reality is quite different. When nonstick surfaces are heated to high temperatures on a stovetop, they emit toxic gases. Figure 3, work commissioned and reviewed by the Environmental Working Group, shows that within only 2 minutes on a hot stove, the nonstick coatings start to release toxic gases. The lowest temperature at which this starts to occur is 392°F, a temperature commonly achieved in the typical kitchen.5 The temperature at which most oils start to smoke is high enough for the polymers to start breaking down.
Figure 3.
Nonstick Pan Coatings Release Toxic Gases
They damage the kidneys primarily by passive diffusion into the tubules, where they poison the mitochondria. This results in inadequate energy production so active excretion is impaired, increasing oxidative stress as the damaged mitochondria leak highly oxidative high-energy electrons and oxygen and, eventually, cell death resulting in progressive loss of kidney function.6 Other examples in this toxic class include perflurooctanoic acid (PFOA) and perflourooctanesulfonic (PFOS) acid.
Glyphosate
The herbicide glyphosate appears to be a huge problem for the kidneys. It is heavily used in conventional agriculture and around the home under names such as Roundup. Epidemiological research has found a very strong correlation between glyphosate use and the kidney failure epidemic. Of course, association does not prove causation. Animal research shows that chronic exposure at very low dosages causes kidney damage. A 2-year study in rats’ drinking water with 0.1 PPB of glyphosate resulted in cellular kidney abnormalities.
Researchers in Sri Lanka found that those who drink well water contaminated with glyphosate have a higher incidence of kidney failure in proportion to concentration starting at 0.7 PPB. Farmers spraying glyphosates in the fields have a 5.4-fold increased incidence.7 The European standard for water contamination is 0.1 PPB, whereas the US Environmental Protection Agency (EPA) standard is an inexplicable 700 PPB!8
Strangely, I was unable to find definitive current measures of the amount of glyphosate or its main metabolite, aminomethylphosphonic acid (AMPA), in US water supplies. It had to be current because the amount in use has increased rapidly the past 2 decades. The best I could find was a study commissioned by Moms Across America, published in 2014.9 This study lacks scientific rigor in that they tested only 21 drinking water samples with no apparent methodology for ensuring a representative distribution. Nonetheless, the results are alarming. Thirteen of the samples had glyphosate levels ranging from 85 to 330 PPB. Especially worrisome is that they found 76 to 166 PPB in all the breast milk samples they tested.
Some researchers are speculating that glyphosates may also be a big part of the problem with genetically modified organism (GMO) foods. They are genetically modified specifically to be resistant to glyphosate. This means more is sprayed around them and, thus, into the food supply, water, and breast milk.
Smoking
As would be expected, smoking damages the kidneys. It is high in cadmium and nicotine constricts the blood vessels going into the kidneys, thus decreasing glomerular filtration. It also increases generation of reactive oxygen species and activation of fibrotic pathways in the kidneys.
Nonsteroidal Anti-inflammatory Drugs
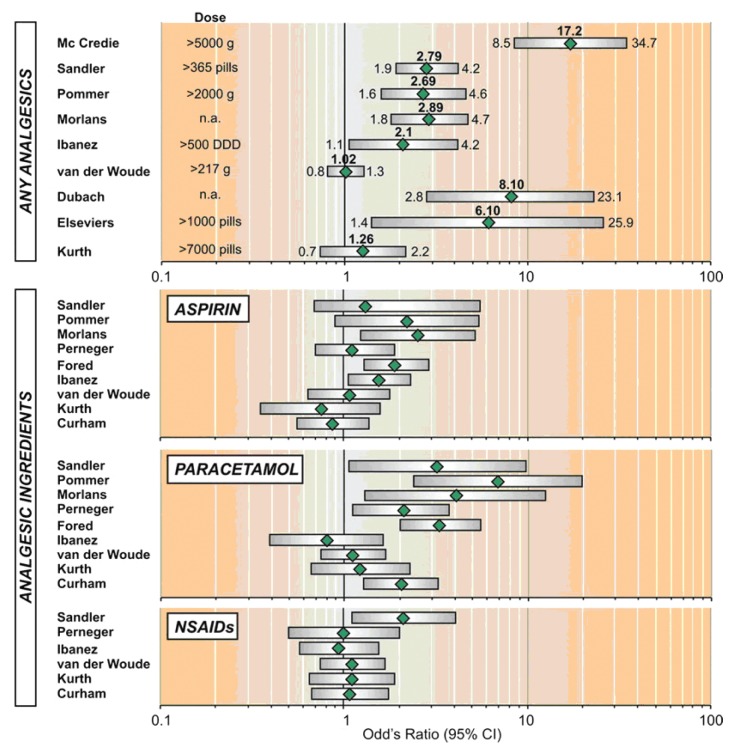
This one is a bit of a surprise and quite serious. Most nonsteroidal anti-inflammatory drugs (NSAIDs) were initially available only by prescription and then became available over the counter when their patents ran out. Many of these now readily available drugs have long-term side effects that are not adequately appreciated by most people. Virtually all safety studies are short term, so many toxic effects are not detected during the research and development stages and are now showing up in population studies. Acetaminophen, aspirin, ibuprofen, naproxen, indomethacin, and COX-2 inhibitors have now all been shown to cause kidney damage when used chronically.
Chronic consumption (>3 y) of single and combinations of NSAIDs are now known to cause typically irreversible analgesic nephropathy. Figure 4 summarizes the risks. As can be clearly seen, these classes of drugs greatly increase the risk of kidney failure. Please be clear, this is end-stage kidney failure we are looking at. Obviously, loss of kidney function is much more prevalent.
Figure 4.
Risk of Kidney Failure From Long-term Use of NSAIDs10
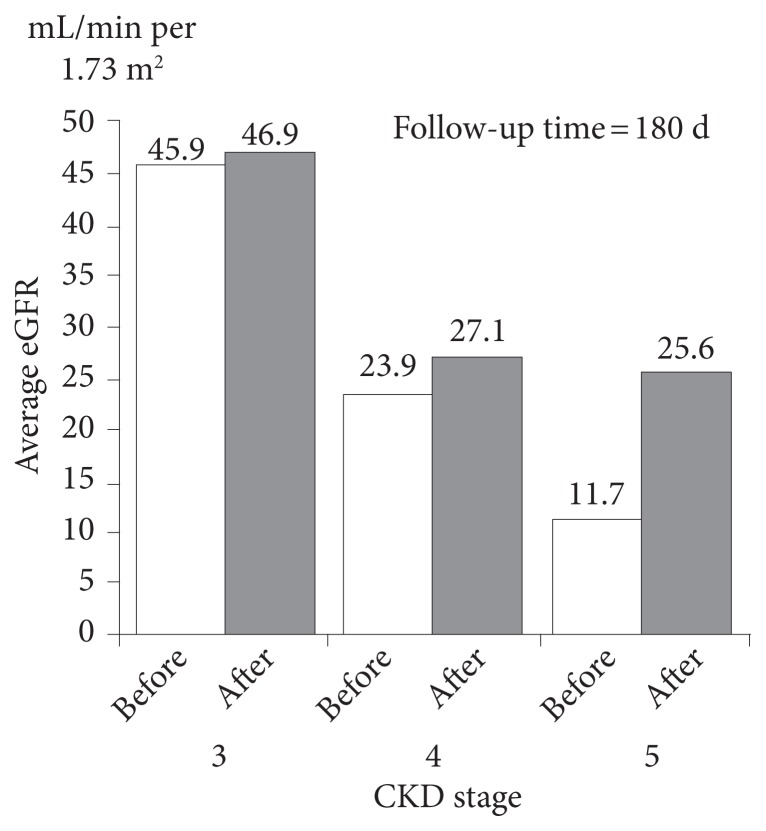
The good news is that even in patients with kidney failure, stopping the use of NSAIDs results in some recovery of function. As shown in Figure 5, after 6 months, those with the most damaged kidneys enjoy more than a doubling of kidney function.
Figure 5.
Stopping NSAID Use Greatly Improves Function in Patients With Kidney Failure11
Abbreviations: eGFR, estimated glomerular filtration rate; CKD, chronic kidney disease.
Toxins From the Gut
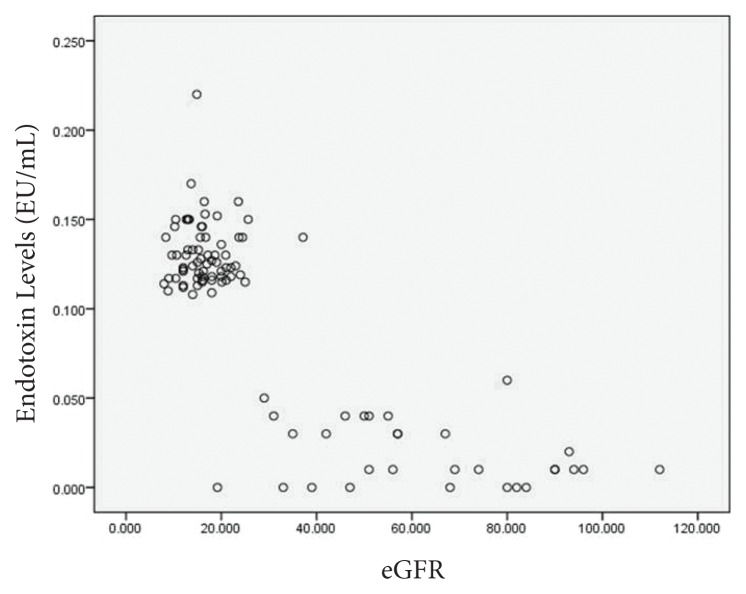
Long-time subscribers will likely remember my editorial on the role of the gut in chronic disease. At the time, I had not adequately appreciated how hard endotoxins are on the kidneys. This is a bit of a chicken-and-egg issue as damaged kidneys also have trouble clearing endotoxins. Figure 6 clearly demonstrates what happens to endotoxin levels as kidney function declines.
Figure 6.
Endotoxins and the Kidneys12
Abbreviation: eGFR, estimated glomerular filtration rate.
Further supporting the concept that a toxic gut damages the kidney is the research showing a direct correlation between the level of indoles in the blood and loss of kidney function.13 A long-term prospective study also found a correlation between rate of death and indole levels in dialysis patients.14
Excessive Salt in the Diet
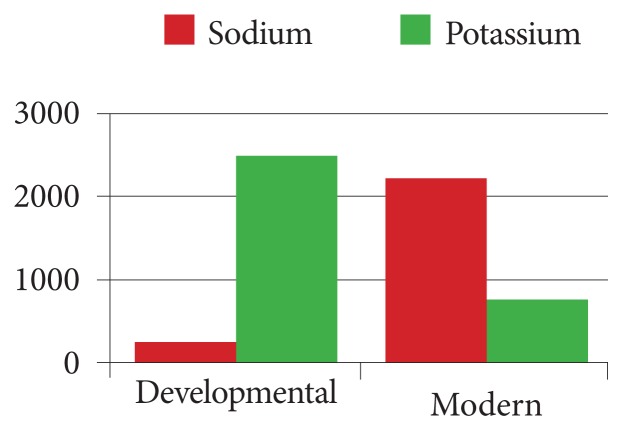
Another big problem for the kidneys, and some researchers are suggesting may be an important contributing cause to their degeneration, is excessive salt consumption. The 2 to 6 excessive grams of salt the average person consumes every day appears to overload the kidneys enough to impair their ability to eliminate other toxins, especially acidic metabolic waste products. In the millennia as we evolved as a species, salt was not readily available so we had developed effective mechanisms for retaining salt. As shown in Figure 7, we went from an evolutionary diet that had a Na/K ratio of 1:10, to one that is more than 3:1.
Figure 7.
The Dramatic Increase in Sodium and Decrease in Potassium Found in the Modern Diet
Excessive Phosphates in the Diet
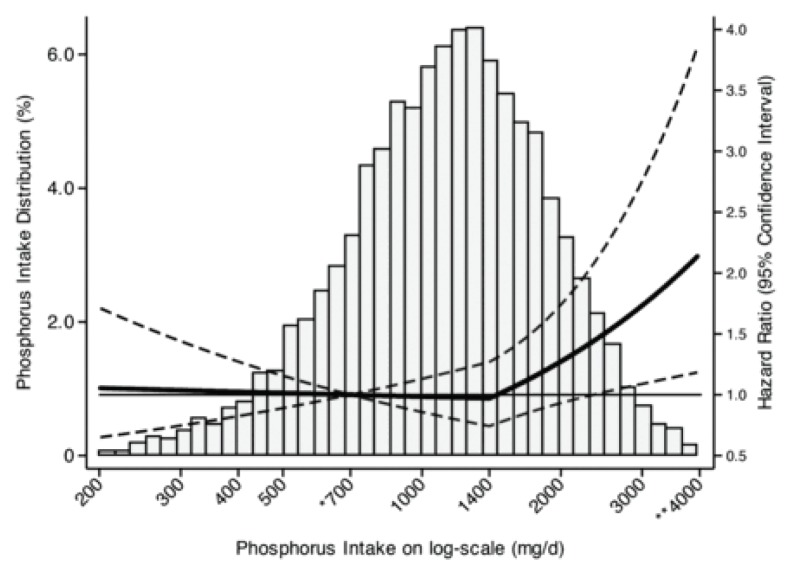
The average American consumes far more phosphorus than the Recommended Dietary Allowance (RDA) of 700 mg/d for adults. As the amount of phosphorous added to prepared foods is under reported. See Lara Pizzorno’s article in issue 14.4 for a full discussion of this problem.15 It is difficult to be definitive, but it appears that a substantial portion of the population consumes more than the tolerable upper limit of 4000 mg/d.
As clearly shown in Figure 8 (which underestimates actual phosphate consumption), the vast majority of the population consumes way more phosphorous than recommended. What is worse, though, is that at least 40% of Americans consume at least twice the recommended daily allowance of phosphorous, a level known to as much as double all-cause mortality.
Figure 8.
The Excessive Phosphorous Intake in the Typical Diet Increases All-cause Mortality16
Research has shown that excessive phosphorous consumption significantly disrupts hormonal regulation of phosphorus, calcium, and vitamin D, causing disordered mineral metabolism; osteoporosis; cardiovascular disease; and impaired kidney function.17
Anything that decreases blood flow to the kidneys results in decreased excretion of toxins. Excessive phosphates damage the tubules, increase fibrosis blocking the blood vessels, and decrease glomerular filtration rate. Getting rid of phosphates is a huge problem for the kidneys, with one of the early signs of kidney failure being increasing phosphate levels in the blood.
The primary sources of “hidden” phosphates are additives used as processing aids, such as acid balancing (especially in carbonated beverage); leavening of bread; color and moisture retention; anticaking; and flavorings. Assessing total phosphate load is difficult as current databases underestimate the phosphorus content of processed foods by at least 25% to 30%.18 The primary sources of phosphates can be found in Lara’s article.
Summary
As I worked on this editorial, I was quite surprised to find that so much of our kidney’s normal function is being used up by everyday chemicals we eat, such as salt and phosphates, and commonly doctor- and self-prescribed NSAIDs. When environmental toxins such as cadmium, glyphosate, and halogenated hydrocarbons are added to the burden, the kidney function loss epidemic goes from inexplicable to predictable.
Although, with the exception of workplace exposure, none of these toxic factors alone is the big problem, together they overwhelm and progressive damage the kidneys. I am coming to the conclusion that strengthening and protecting kidney function is one of the best antiaging strategies we can recommend to our patients.
In the next issue, I will discuss ways of protecting the kidneys and actually increasing function even in “normal” people.
In This Issue
We start this issue with another interesting commentary by Associate Editor Jeff Bland, phd. The concept of “disease” and how it has shaped the evolution of medical practice is a fascinating story. On the one hand, the standardization of disease, its diagnosis, and treatment played a substantial role in the efficacy of conventional medicine in many areas. On the other hand, the implicit standardization of humans to make this concept work is the root cause of many of the limitations of conventional medicine as well.
I think John Weeks’ work compiling documentation of the cost-effectiveness of integrative medicine is very important. It was powerfully validated during a meeting I had earlier today when an insurance broker asked me for documentation on why she should recommend integrative medicine to her corporate clients as a way of corralling spiraling health care costs.
The potential of immunotherapy in the treatment of cancer has seemed a great idea for a long time. However, the implementation has been much more complex than expected. Managing Editor Craig Gustafson interviewed Bernard Fox, phd, to help us better understand the challenges and successes. Dr Fox will be speaking at the annual conference of the Oncology Association of Naturopathic Physicians (OncANP) in Phoenix, Arizona, February 26 through 28, 2016.
I am very excited that with the great leadership of David Riley, md, we are now regularly publishing case reports—2 for this issue, a pace I hope we can maintain. All readers are invited to submit cases using the CARE guidelines he created (you can access these standards at http://www.imjournal.com). Kara Fitzgerald, nd, presents us an insightful intervention for a teenager with eosinophilic gastroenteritis. With concepts echoing Dr Bland’s commentary, Dr Fitzgerald’s case is a great example of diagnosing and treating the “disease” versus understanding the multiple functional disturbances that are the actual problem. Scott Shannon, md; and Janet Opila-Lehman, nd, collaborate to provide us an intriguing way of helping patients addicted to marijuana. I find particularly intriguing the concept of anxiety reduction being an important driver of excessive marijuana use.
Our clinician interview is with Kara N. Fitzgerald, nd. Craig Gustafson discusses with her the importance for clinicians of well-constructed case reports. Her recommendations on how busy clinicians can share their insights in this fashion and the templates she has created are extremely helpful and I am grateful for her sharing.
As usual, Associate Editor Bill Benda, md, finishes the issue with his, as usual, provocative BackTalk. All I can say is, “Are you sure, Bill?”
Joseph Pizzorno, nd, Editor in Chief
drpizzorno@innovisionhm.com
References
- 1.Frassetto LA, Morris RC, Jr, Sebastian A. Effect of age on blood acid-base composition in adult humans: role of age-related renal functional decline. Am J Physiol. 1996;271(6/2):F1114–F1122. doi: 10.1152/ajprenal.1996.271.6.F1114. [DOI] [PubMed] [Google Scholar]
- 2.Pizzorno J. Is mercury toxicity an epidemic? (Part I) Integr Med Clin J. 2009;8(1):8–10. [Google Scholar]
- 3.Pizzorno J. Is mercury toxicity an epidemic? (Part II) Integr Med Clin J. 2009;8(2):8–12. [Google Scholar]
- 4.Canaries in the kitchen: Teflon toxicosis. Environmental Working Group Web site. [Accessed November 16, 2015]. No author listed. http://www.ewg.org/research/canaries-kitchen. Published May 15, 2003.
- 5.Seidel WC, Scherer KV, Jr, Cline D, Jr, et al. Chemical, physical, and toxicological characterization of fumes produced by heating tetrafluoroethene homopolymer and its copolymers with hexafluoropropene and perfluoro(propyl vinyl ether) Chem Res Toxicol. 1996;4(2):229–236. doi: 10.1021/tx00020a017. [DOI] [PubMed] [Google Scholar]
- 6.Groves CE, Lock EA, Schnellmann RG. Role of lipid peroxidation in renal proximal tubule cell death induced by haloalkene cysteine conjugates. Toxicol Appl Pharmacol. 1991;107(1):54–62. doi: 10.1016/0041-008x(91)90330-h. [DOI] [PubMed] [Google Scholar]
- 7.Jayasumana C, Paranagama P, Agampodi S, et al. Drinking well water and occupational exposure to herbicides is associated with chronic kidney disease, in Padavi-Sripura, Sri Lanka. Environ Health. 2015 Jan;14:6. doi: 10.1186/1476-069X-14-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Environmental Protection Agency. Basic information about glyphosate in drinking water. [Accessed November 18, 2015]. http://water.epa.gov/drink/contaminants/basicinformation/glyphosate.cfm#four. Updated February 9, 2014.
- 9.Honeycutt Z, Rowlands H. Glyphosate testing full report: Findings in American mothers’ breast milk, urine and water. Moms Across America Web site. [Accessed November 18, 2015]. http://www.momsacrossamerica.com/glyphosate_testing_results. Published April 7, 2014.
- 10.De Broe ME, Elseviers MM. Over-the-counter analgesic use. J Am Soc Nephrol. 2009;20(10):2098–2103. doi: 10.1681/ASN.2008101097. [DOI] [PubMed] [Google Scholar]
- 11.Wei L, MacDonald TM, Jennings C, et al. Estimated GFR reporting is associated with decreased nonsteroidal anti-inflammatory drug prescribing and increased renal function. Kidney Int. 2013;84(1):174–178. doi: 10.1038/ki.2013.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McIntyre CW1, Harrison LE, Eldehni MT, et al. Circulating endotoxemia: A novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(1):133–141. doi: 10.2215/CJN.04610510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin CJ, Chen HH, Pan CF, et al. p-Cresylsulfate and indoxyl sulfate level at different stages of chronic kidney disease. J Clin Lab Anal. 2011;25(3):191–197. doi: 10.1002/jcla.20456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu IW, Hsu KH, Hsu HJ, et al. Serum free p-cresyl sulfate levels predict cardiovascular and all-cause mortality in elderly hemodialysis patients—a prospective cohort study. Nephrol Dial Transplant. 2012;27(3):1169–1175. doi: 10.1093/ndt/gfr453. [DOI] [PubMed] [Google Scholar]
- 15.Pizzorno L. Nothing boring about boron. Integr Med Clin J. 2015;14(4):35–48. [PMC free article] [PubMed] [Google Scholar]
- 16.Chang AR, Lazo M, Appel LJ, Gutiérrez OM, Grams ME. High dietary phosphorus intake is associated with all-cause mortality: Results from NHANES III. Am J Clin Nutr. 2014;99(2):320–327. doi: 10.3945/ajcn.113.073148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pizzorno L. Canaries in the phosphate-toxicity coal mines. Integr Med Clin J. 2014;13(6):24–32. [PMC free article] [PubMed] [Google Scholar]
- 18.Calvo MS, Uribarri J. Contributions to total phosphorus intake: All sources considered. Semin Dial. 2013;26(1):54–61. doi: 10.1111/sdi.12042. [DOI] [PubMed] [Google Scholar]