Abstract
In 2006, a previous study at our institution reported high perioperative and anesthesia-related mortality rates of 21.97 and 1.12 per 10,000 anesthetics, respectively. Since then, changes in surgical practices may have decreased these rates. However, the actual perioperative and anesthesia-related mortality rates in Brazil remains unknown. The study aimed to reexamine perioperative and anesthesia-related mortality rates in one Brazilian tertiary teaching hospital.
In this observational study, deaths occurring in the operation room and postanesthesia care unit between April 2005 and December 2012 were identified from an anesthesia database. The data included patient characteristics, surgical procedures, American Society of Anesthesiologists (ASA) physical status, and medical specialty teams, as well as the types of surgery and anesthesia. All deaths were reviewed and grouped by into 1 of 4 triggering factors groups: totally anesthesia-related, partially anesthesia-related, surgery-related, or disease/condition-related. The mortality rates are expressed per 10,000 anesthetics with 95% confidence intervals (CIs).
A total of 55,002 anesthetics and 88 deaths were reviewed, representing an overall mortality rate of 16.0 per 10,000 anesthetics (95% CI: 13.0–19.7). There were no anesthesia-related deaths. The major causes of mortality were patient disease/condition-related (13.8, 95% CI: 10.7–16.9) followed by surgery-related (2.2, 95% CI: 1.0–3.4). The major risks of perioperative mortality were children younger than 1-year-old, older patients, patients with poor ASA physical status (III–V), emergency, cardiac or vascular surgeries, and multiple surgeries performed under the same anesthetic technique (P < 0.0001).
There were no anesthesia-related deaths. However, the high mortality rate caused by the poor physical conditions of some patients suggests that primary prevention might be the key to reducing perioperative mortality. These findings demonstrate the need to improve medical perioperative practices for high-risk patients in under-resourced settings.
INTRODUCTION
Safety is a routine concern in anesthesiology. Although cardiac arrest and death rarely occur during the perioperative period, these events represent the worst patient outcomes.
A past study of our institution,1 a general tertiary teaching hospital in Brazil, which is considered a high human development country according to the Human Development Index (HDI) set by the United Nations Development Programme,2 reported overall and anesthesia-related mortality rates of 21.97 and 1.12 per 10,000 anesthetics, respectively. Furthermore, our previous perioperative and anesthesia-related mortality rates were higher than those reported in studies from very high human development countries (ranging from 3.44 to 18.9 per 10,000 anesthetics and 0.10 to 0.95 per 10,000 anesthetics, respectively) that were published during the same period;3–7 these discrepancies were partially attributable to methodology disparities, but decreased access to healthcare is also a factor in our country.
In the last decade, Brazil has experienced significant improvements in economy and human indicators, thereby decreasing the inequality in relation to very high human development countries. In addition, in the last 10 years, our institution has developed initiatives to improve the care of surgical patients, including installing anesthesia workstations with ventilators in operating rooms (ORs); monitoring oxygen, carbon dioxide, nitrous oxide, and inhaled anesthetic concentrations; monitoring ventilation, to enable adequate ventilation and anesthesia control; acquiring devices for adequate core temperature control; and increasing the number of staff anesthesiologists and adult intensive care beds. However, the actual perioperative and anesthesia-related mortality rate in Brazil remains unknown.
We hypothesized that identifying and controlling risk factors and improving healthcare conditions following broadly defined institutional initiatives would improve anesthesia care and, consequently, improve surgical patients outcomes.
To address the lack of available information concerning perioperative and anesthesia-related mortality, the aim of this study was to reexamine the rates, causes and triggering factors of deaths occurring during anesthesia and in the postanesthesia care unit (PACU) over an 8-year period in a surgical population at a single Brazilian tertiary teaching hospital.
METHODS
The study was approved by the Botucatu Medical School Human Research Ethics Committee (protocol number 3160-2009), which waived the requirement for written informed consent.
In this observational study, we analyzed all reported perioperative deaths that occurred in the OR and PACU (short stay) in 55,002 consecutive anesthetized patients at the hospital of the School of Medicine, Universidade Estadual Paulista (UNESP) from April 1, 2005 to December 31, 2012. UNESP hospital is a public tertiary teaching hospital with 450-beds with a catchment of 2 million people that perform approximately 7000 surgeries per year on people of all age groups. The patient mix includes all surgical areas, as well as, high-risk obstetric and newborn patients. The hospital has 15-bed neonatal, 10-bed pediatric, and 37-bed adult intensive care units. Anesthesia care is provided by full-time faculty anesthesiologists, staff anesthesiologists, and anesthesiology residents.
All patients were examined by an anesthesiologist immediately before all emergency and urgent surgical procedures or the day before all elective procedures. Continuous ECG monitoring and automatic noninvasive blood pressure and pulse oximetry measurements were utilized as a basic safety measure in the OR during regional and neuraxial anesthesia and sedation. For general anesthesia, the following parameters were also measured: oxygen concentration, capnography, delivered anesthetic vapor concentration, ventilation, and core temperature. Critically ill patients received direct invasive blood pressure and central venous monitoring.
Cardiac arrest was defined as the cessation of cardiac mechanical activity, with the loss of effective circulation, as determined by the absence of a palpable central pulse. Resuscitation was performed according to the interventions and protocols of the Advanced Cardiovascular Life Support guidelines. Patient deaths were identified from an anesthesia database, which was developed using a quality assessment form, which was part of the mandatory documentation for each anesthetic procedure. This database includes all procedures performed in the OR and PACU. The recorded data included the date and location (OR or PACU), patient characteristics, surgical procedures (elective, urgent, or emergency surgery), American Society of Anesthesiologists (ASA) physical status classification,8 medical specialty team, surgery type, anesthesia type, anesthesia provider information and a 95-item checklist of airway, respiratory, cardiovascular, neurological, renal, and miscellaneous events. When regional and general anesthesia were combined, general anesthesia was considered to be the technique used. In the cases of perioperative mortality, the anesthesiologist responsible for each case was asked to review the case and to provide a written summary for peer review.
Medical and anesthesia record data, written summaries, and, when applicable, the necropsy records of the patients who died during anesthesia or in the PACU were analyzed by the Anesthesia Cardiac Arrest and Mortality Study Commission, which is composed of 3 of the authors, who are faculty members in the Department of Anesthesiology (JRCB, NSPM, and LGB). The deaths were independently analyzed by all 3 board members in early 2014 and in early 2015 (final review) for a more detailed analysis. The triggering factors leading to mortality were assigned to 1 of 4 groups: totally related to anesthesia (ie, anesthesia was the only or major contributory factor); partially related to anesthesia (ie, the patient disease/condition or surgical procedure was a contributory factor, but the anesthesia represented an additional factor); totally related to surgery; or totally related in the to the patient's disease or condition. For the majority of the deaths, there was unanimity regarding the cause of the event. After the final review, disagreements among the 3 members were resolved by discussion; in all cases, an agreement or consensus was reached when at least 2 of the 3 members agreed on the event's cause.
Statistical Analysis
The mortality rates (expressed per 10,000 anesthetics) and 95% confidence intervals (CIs) were compared with χ2 test (ie, sex) or Tukey's test for multiple comparisons among proportions9 (ie, age group, ASA physical status, surgical procedure, anesthesia technique, and triggering factors). The factors predicting perioperative mortality (ie, age group, ASA physical status, surgical procedure, and surgery type) were analyzed with multivariate forward stepwise logistical regression, with odds ratios and 95% CIs. Data were considered to be significant when P < 0.05. The statistical analyses were performed using SPSS software, version 17.1 (SPSS Inc., Chicago, IL).
RESULTS
During the 8-year study period, 55,002 consecutive patients were anesthetized. Eighty-eight deaths (16.0 per 10,000 anesthetics; 95% CI: 13.0–19.7) representing all triggering factors were identified during the perioperative period in the OR and PACU. The majority of deaths occurred in the OR (96.6%) compared with the PACU (3.4%).
The highest estimated mortality rates occurred in children younger than 1 year of age, patients aged 65 years and older, and patients aged between 51 and 64 years, but mortality rates were not different between males and females (Table 1). Mortality rates also varied according to ASA physical status, surgery procedures, and type of anesthesia (Tables 2–3). In addition, the highest estimated mortality rates occurred in multiple surgeries performed under the same anesthetic technique (507.2 per 10,000 anesthetics; 95% CI: 141.1–873.3), cardiac (206.3 per 10,000 anesthetics; 95% CI: 114.5–298.1), vascular (108.4 per 10,000 anesthetics; 95% CI: 69.8–147.0), neurological (24.2 per 10,000 anesthetics; 95% CI: 6.3–42.1), gastroenterological (19.8 per 10,000 anesthetics; 95% CI: 9.8–29.8), and pediatric surgeries (16.8 per 10,000 anesthetics; 95% CI: 3.3–30.3).
TABLE 1.
Perioperative Mortality Rates in 55,002 Anesthetics According to Age and Sex
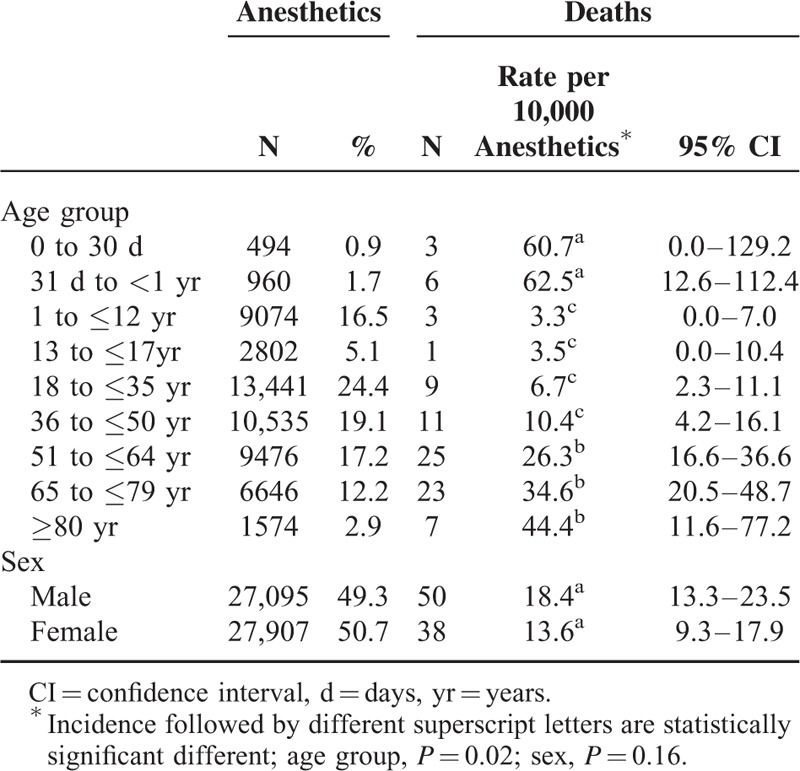
TABLE 2.
Perioperative Mortality Rates in 55,002 Anesthetics According to the ASA Physical Status and Surgical Procedures
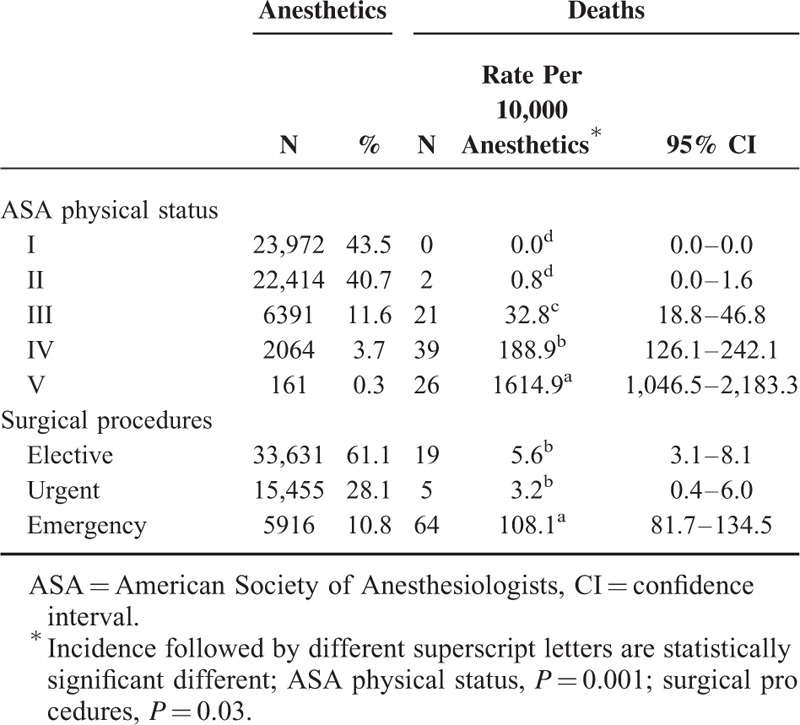
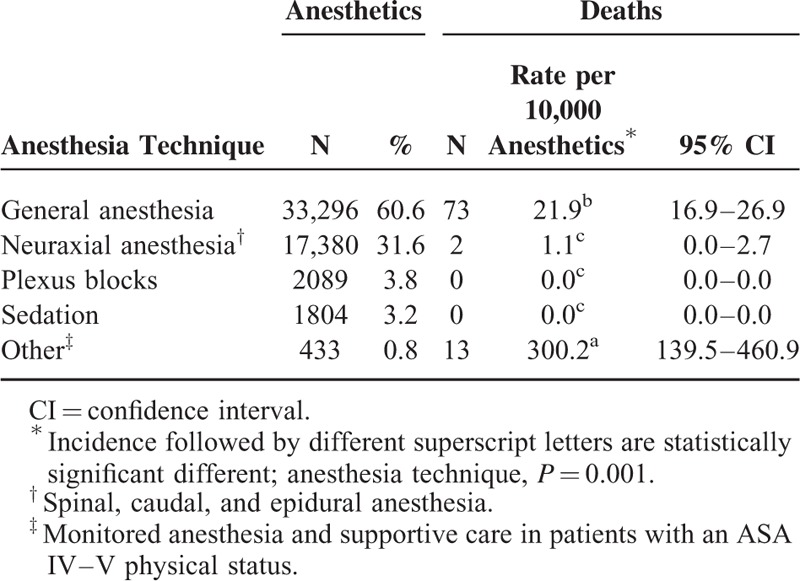
TABLE 3.
Perioperative Mortality Rates in 55,002 Anesthetics According to Anesthesia Technique
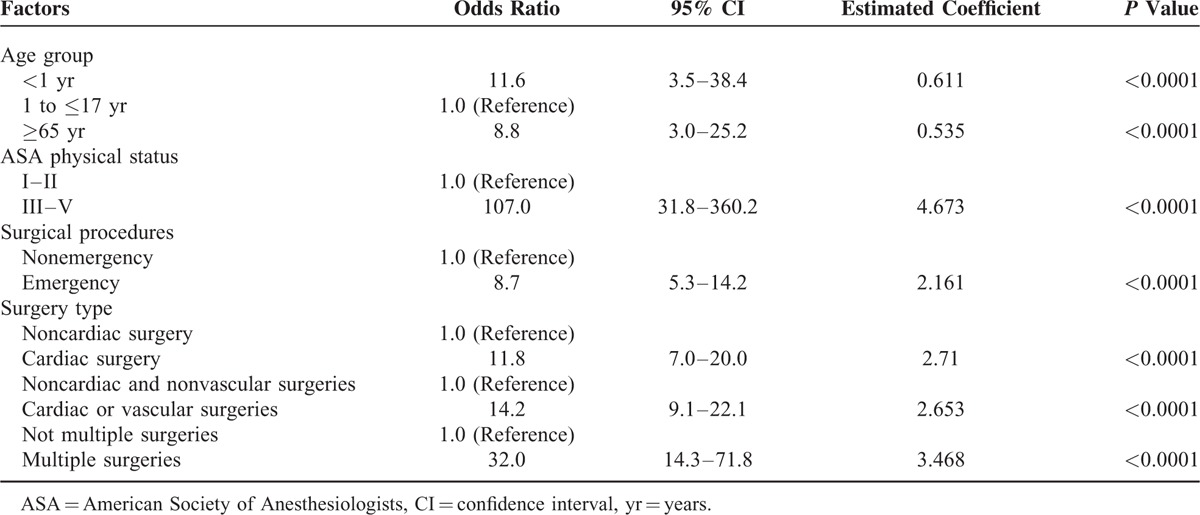
After adjustment, higher mortality rates were identified in children younger than 1 year of age and patients aged 65 years and older, compared with children between 1 and 17 years of age; patients with ASA physical status III–IV compared with I–II; emergency compared with nonemergency surgery; cardiac or vascular surgeries compared with other types of surgery; and multiple surgeries during the sampling period compared with one surgery (Table 4).
TABLE 4.
Multivariate Analysis of Predictors of Perioperative Mortality in Surgical Patients
The patient's disease or condition was the most important triggering factor for mortality (86.4% of the perioperative deaths), followed by surgery-related (13.6%) (P = 0.02). No cases of anesthesia-related mortality were recorded (Table 5).
TABLE 5.
Triggering Factors Contributing to Mortality in 55,002 Anesthetics
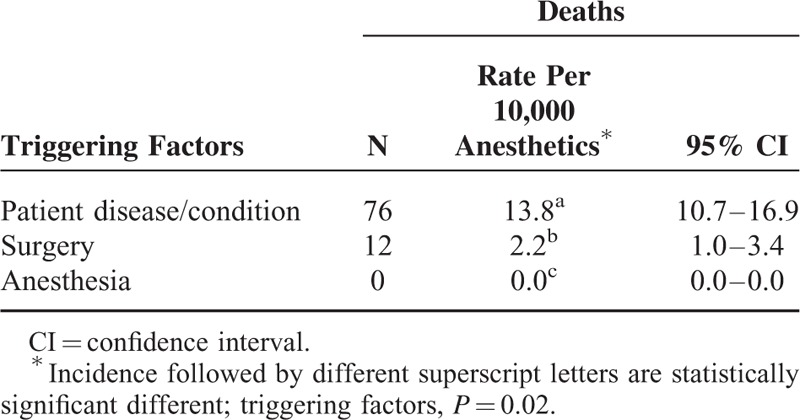
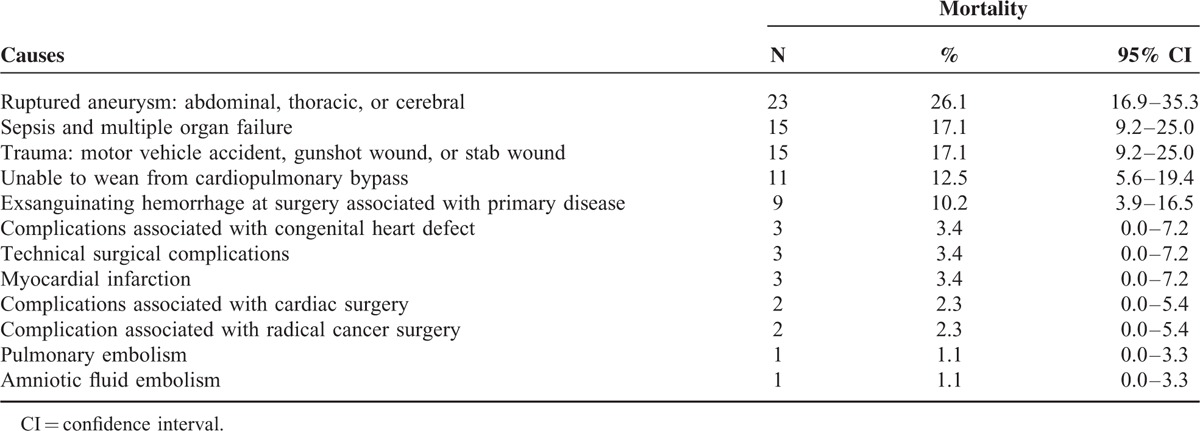
Table 6 provides additional information concerning the 88 deaths attributable to patient disease/condition or surgery-related factors. The most frequent causes were ruptured aneurysm, followed by complications associated with cardiac surgery (including the inability to wean the patients from cardiopulmonary bypass and complications associated with congenital heart defects), sepsis and multiple organ dysfunction syndrome, and trauma.
TABLE 6.
Causes of Perioperative Mortality Related to Patient Disease/Condition or Surgery Factors in 55,002 Anesthetized Patients
There was no perioperative death in patient with ASA I physical status. However, there were 2 perioperative deaths in patients with ASA II physical status. The first 1 was an obstetric patient who had a hydatiform mole and underwent uterine curettage under general anesthesia during the early postpartum period. During the procedure, the patient developed sudden severe hypoxemia, followed by cardiovascular collapse and cardiac arrest. This patient passed away in the OR. The necropsy report revealed an amniotic fluid embolism. The second case was an elderly patient who underwent cholecystectomy under general anesthesia. During the surgical procedure, it was observed an abnormal neovascularization in the gallbladder and hepatic hilum, there was an excessive bleeding and the patient passed away in the OR.
DISCUSSION
Compared with our previous study,1 the main findings in this study were as follows: the current perioperative mortality rates (16.0 per 10,000 anesthetics) were lower than those from the 1996 to 2005 period (21.97 per 10,000 anesthetics; 95% CI: 18.3–26.3); the current anesthesia-related (zero per 10,000 anesthetics; 95% CI: 0.0–0.0) and surgery-related (2.2 per 10,000 anesthetics; 95% CI: 1.0–3.4) mortality rates were lower than those previously reported (ie, 1.12 per 10,000 anesthetics; 95% CI: 0.5–2.4 and 5.96 per 10,000 anesthetics; 95% CI: 4.2–8.4, respectively); and neonates, infants, and older patients continue to exhibit the highest perioperative mortality rates.
We confirmed the hypothesis that our institutional perioperative and anesthesia-related mortality rates have decreased over the last 8 years.
Although our perioperative mortality rate was lower (28.2%) than those reported in the 2000s,1 it was higher than those reported in the last years in very high human development countries (from 0.64 to 14.11 deaths per 10,000 anesthetics).3,5,10–12 It is difficult to compare perioperative and anesthesia-related mortality rates in our study with the results of previous studies because of considerable variation in the methods and patients populations among these studies. Some perioperative and anesthesia-related mortality studies excluded patients with ASA V physical status,13 patients younger than 20 years old11 or younger than 16 years old,12 and trauma patients,12 as well as cardiac11,12,14 and transplant surgeries.12
The inclusion of all types of surgeries and patients with poorer ASA physical status certainly influenced our mortality rates. Preexisting morbidities, such as traumatic injury and sepsis, which have high incidences and mortality rates in Brazil,15,16 also influenced our perioperative mortality rates. In studies that included children, the perioperative mortality rates are higher in cardiac surgery compared with noncardiac surgery.17,18 Cardiac surgery had a perioperative mortality risk factor that was 42-fold higher than noncardiac surgeries in patients younger than 18 years old.17 The current study revealed that cardiac surgery exhibited a greater risk of perioperative mortality compared with noncardiac surgery (11.8-fold), as well as cardiac or vascular surgeries compared with noncardiac and nonvascular surgery (14.2-fold) and multiple surgeries compared with not multiple surgeries (32-fold).
In our study, many surgical patients arrived at the OR without optimization of their disease management. For some of these patients, intraoperative mortality might have been prevented by adequate primary care and preoperative assessments. These findings demonstrate a persistent need to improve the quantity and quality of resource utilization and healthcare access, which are still inadequate in Brazil19 and other low and medium human development countries.20 In addition, to initiate multidisciplinary discussions of adverse effects and to implement evidence-based safety protocols that improve perioperative patient care, it is necessary to adopt perioperative medical practices to have demonstrable effectiveness.21,22
Both ASA physical status and emergency surgery are recognized predictive factors of mortality.23 Approximately 98% of the perioperative deaths in our study occurred in patients with poorer ASA physical status (III–V). Our study demonstrated that surgical patients exhibiting a poorer ASA physical status (III–V) were more likely (107-fold) to experience perioperative mortality than patients with ASA I–II physical status. Our study also demonstrated that patients who underwent emergency surgery exhibited an 8.7-fold higher risk of perioperative mortality compared with patients who underwent nonemergency surgery. This result may be due, in part, to the fact that it is difficult to evaluate and optimize a patient before surgical emergencies, especially in cases of a ruptured aortic aneurysm or severe trauma.15
A meta-analysis24 revealed that the baseline risk status of surgical patients, as demonstrated by the ASA physical status, has increased over recent decades. However, overall rates of perioperative and anesthesia-related mortality have declined significantly over the past 50 years being the greatest and most consistent decline in developed countries compared with developing countries. According to the authors, these results suggest continuous safety improvements for surgical patients, specially in developed countries.
Patient disease/condition remained the major triggering factor for perioperative mortality, followed by surgery. The mortality risk conferred by surgery in the current study was 2.7-fold lower compared with the previous study.1 Advances in medical practices favor best outcomes but may result in a greater number of procedures in patients with more comorbidities, as well as older and high risk patients. Patients with highly complex diseases who were once considered unfit for anesthesia are increasingly undergoing surgery.18
Despite methodology differences, most studies published in the last decade3,5,10,13,25–27 and from 2010 to present11,28 have reported anesthesia-related mortality rates in surgical patients of <1.0 per 10,000 anesthetics (from 0.0 to 0.95 per 10,000 anesthetics), which represents a 2- or 3-fold improvement compared with studies performed in the 1980s.29,30 Our study confirmed this trend (ie, zero anesthesia-related deaths per 10,000 anesthetics). Two recent studies from our institution highlighted the lack of anesthesia-related mortality in children31 and older patients between 2006 and 2010.32 In the literature, only 2 studies have reported no anesthesia-related deaths.11,33 Both studies excluded cardiac surgeries11,33 and one of the studies excluded patients younger than 20 years old.11 Thus, our study is the first to report no anesthesia-related deaths without excluding any patients.
The influence of age on perioperative mortality rates has been demonstrated by some studies, which have cited the subpopulations of neonates, infants, and older patients as those at higher risk.1,3,11,34 Immaturity and congenital diseases in neonates and infants and chronic disease (eg, cancer, cardiovascular disease) contribute decisively to the high-risk status of these populations.18,31,32,35 Thus, in our study, a ruptured aneurysm was the first important cause of perioperative mortality in older patients, whereas complications associated with cardiac surgery were an important cause of mortality in children and older patients.
Despite the healthy trend of higher life expectancy of the women36 and some reports of male predisposing to cardiac arrest and death in perioperative period,3,28 our findings corroborated with other studies6,11,12 demonstrated no evidence of sex predisposing perioperative death.
The higher frequency of perioperative mortality in patients receiving general anesthesia does not necessarily imply that general anesthesia is less safe. Instead, this correlation may reflect the fact that many high-risk surgeries (eg, cardiac, thoracic, gastroenterological, and neurological) were performed under general anesthesia. Another possible confounding factor in this case is that the anesthesiologist often prefers to give general anesthesia to the most fragile patients, independent of the type of surgery.
There may have been some methodological weaknesses in the present study. First, the data are derived from adverse event reports. Underreporting is likely in this situation, although in each case, it was mandatory to complete the form. To minimize the risk of underreporting a death, the information was crosschecked with the operating theatre records and hospital administration records. Second, this study is representative of the experience of a single hospital. Certain practices specific to our institution may have influenced our results. However, our institution is a public tertiary hospital similar to many other public hospitals from our country. Thus, the findings may represent the entire spectrum of the general surgical Brazilian population.
Global measurements of patient safety, including the main outcomes of anesthesia, such as cardiac arrest37 and mortality24 should be provided more consistently in all countries, but especially in those with low, medium, and high human development countries due to the lack of available data in the literature.
In conclusion, this observational study demonstrates that despite the improvements achieved in patient anesthesia safety (ie, no anesthesia-related death and an important reduction in the surgery-related deaths rate), the perioperative mortality rate of 16.0 per 10,000 anesthetics (while lower compared with a previous study) is higher than the rates in developed countries. Significant predictors of perioperative mortality included ASA, age (with neonates, infants, and older patients at a greater mortality risk), and emergency, cardiac or vascular surgeries, and multiple surgeries. The high perioperative mortality rate in surgical patients due to poor physical status suggests that primary prevention may be important in reducing perioperative mortality. These findings demonstrate the need to improve medical perioperative practices for high-risk patients in under-resourced settings.
Acknowledgments
The authors thank the American Journal Experts (C2CA-9649-0A4B-B966-1537) to correct our manuscript.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists; CI = confidence interval; OR = operating room; PACU = postanesthesia care unit.
This study was supported by funds from Department of Anesthesiology, Botucatu Medical School, UNESP – University Estadual Paulista, Botucatu, São Paulo State, Brazil. WP was granted a scholarship from Coordination of Improvement for Higher Academic Staff (CAPES). PSK was granted scholarship from grant #2009/51468-7, São Paulo Research Foundation (FAPESP). MPM was granted scholarship from The National Council for Scientific and Technological Development (CNPq/PIBIC). CAPES, FAPESP, and CNPq are Brazilian governmental agencies dedicated to promoting scientific research.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Braz LG, Módolo NS, Do Nascimento P, Jr, et al. Perioperative cardiac arrest: a study of 53,718 anaesthetics over 9 yr from a Brazilian teaching hospital. Br J Anaesth 2006; 96:569–575. [DOI] [PubMed] [Google Scholar]
- 2.United Nations Development Programme. Human Development Report 2014. New York, 2014. Available at http://hdr.undp.org/en/2014-report [Accessed October 29, 2014]. [Google Scholar]
- 3.Newland MC, Ellis SJ, Lydiatt CA, et al. Anesthetic-related cardiac arrest and its mortality: a report covering 72,959 anesthetics over 10 years from a US teaching hospital. Anesthesiology 2002; 97:108–115. [DOI] [PubMed] [Google Scholar]
- 4.Lagasse RS. Anesthesia safety: model or myth? A review of the published literature and analysis of current original data. Anesthesiology 2002; 97:1609–1617. [DOI] [PubMed] [Google Scholar]
- 5.Kawashima Y, Seo N, Morita K, et al. Anesthesia-related mortality and morbidity in Japan (1999). J Anesth 2002; 16:319–331. [DOI] [PubMed] [Google Scholar]
- 6.Sprung J, Warner ME, Contreras MG, et al. Predictors of survival following cardiac arrest in patients undergoing noncardiac surgery: a study of 518,294 patients at a tertiary referral center. Anesthesiology 2003; 99:259–269. [DOI] [PubMed] [Google Scholar]
- 7.Irita K, Kawashima Y, Iwao Y, et al. Annual mortality and morbidity in operating rooms during 2002 and summary of morbidity and mortality between 1999 and 2002 in Japan: a brief review. Masui 2004; 53:320–335. [PubMed] [Google Scholar]
- 8.American Society of Anesthesiologists (ASA) physical status classification system. Available at https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system [Accessed February 2, 2015]. [Google Scholar]
- 9.Zar JH. Zar JH. Dichotomous variables. Biostatistical Analysis 5th ed.Upper Saddle River, NJ: Prentice-Hall; 2010. 557–558. [Google Scholar]
- 10.Kawashima Y, Takahashi S, Suzuki M, et al. Anesthesia-related mortality and morbidity over a 5-year period in 2,363,038 patients in Japan. Acta Anaesthesiol Scand 2003; 47:809–817. [DOI] [PubMed] [Google Scholar]
- 11.An JX, Zhang LM, Sullivan EA, et al. Intraoperative cardiac arrest during anesthesia: a retrospective study of 218,274 anesthetics undergoing non-cardiac surgery. Chin Med J (Engl) 2011; 124:227–232. [PubMed] [Google Scholar]
- 12.Goswami S, Brady JE, Jordan DA, et al. Intraoperative cardiac arrests in adults undergoing noncardiac surgery: incidence, risk factors, and survival outcome. Anesthesiology 2012; 117:1018–1026. [DOI] [PubMed] [Google Scholar]
- 13.Biboulet P, Aubas P, Dubourdieu J, et al. Fatal and non fatal cardiac arrests related to anesthesia. Can J Anesth 2001; 48:326–332. [DOI] [PubMed] [Google Scholar]
- 14.Sebbag I, Carmona MJ, Gonzalez MM, et al. Frequency of intraoperative cardiac arrest and medium-term survival. Sao Paulo Med J 2013; 131:309–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carlucci MT, Braz JR, do Nascimento P, Jr, et al. Intraoperative cardiac arrest and mortality in trauma patients. A 14-yr survey from a Brazilian tertiary teaching hospital. PLoS One 2014; 9:e90125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silva E, Cavalcanti AB, Bugano DD, et al. Do established prognostic factors explain the different mortality rates in ICU septic patients around the world? Minerva Anestesiol 2012; 78:1215–1225. [PubMed] [Google Scholar]
- 17.Flick RP, Sprung J, Harrison TE, et al. Perioperative cardiac arrests in children between 1988 and 2005 at a tertiary referral center: a study of 92,881 patients. Anesthesiology 2007; 106:226–237. [DOI] [PubMed] [Google Scholar]
- 18.Van der Griend BF, Lister NA, McKenzie IM, et al. Postoperative mortality in children after 101,885 anesthetics at a tertiary pediatric hospital. Anesth Analg 2011; 112:1440–1447. [DOI] [PubMed] [Google Scholar]
- 19.Paim J, Travassos C, Almeida C, et al. The Brazilian health system: history, advances, and challenges. Lancet 2011; 377:1778–1797. [DOI] [PubMed] [Google Scholar]
- 20.Kushner AL, Cherian MN, Noel L, et al. Addressing the Millennium Development Goals from a surgical perspective: essential surgery and anesthesia in 8 low- and middle-income countries. Arch Surg 2010; 145:154–159. [DOI] [PubMed] [Google Scholar]
- 21.Pearse RM, Holt PJ, Grocott MP. Managing perioperative risk in patients undergoing elective non-cardiac surgery. BMJ 2011; 343:d5759. [DOI] [PubMed] [Google Scholar]
- 22.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg 2008; 248:189–198. [DOI] [PubMed] [Google Scholar]
- 23.Morray JP, Geiduschek JM, Ramamoorthy C, et al. Anesthesia-related cardiac arrest in children: initial findings of the Pediatric Perioperative Cardiac Arrest (POCA) Registry. Anesthesiology 2000; 93:6–14. [DOI] [PubMed] [Google Scholar]
- 24.Bainbridge D, Martin J, Arango M, et al. Perioperative and anaesthetic-related mortality in developed and developing countries: a systematic review and meta-analysis. Lancet 2012; 380:1075–1081. [DOI] [PubMed] [Google Scholar]
- 25.Chan RP, Auler Junior JO. Retrospective study of anesthetic deaths in the first 24 hours: review of 82,641 anesthesias. Rev Bras Anestesiol 2002; 52:719–727. [PubMed] [Google Scholar]
- 26.Aroonpruksakul N, Raksakiatisak M, Thapenthai Y, et al. Perioperative cardiac arrest at Siriraj Hospital between 1999-2001. J Med Assoc Thai 2002; 85 Suppl 3:S993–S999. [PubMed] [Google Scholar]
- 27.Lienhart A, Auroy Y, Péquignot F, et al. Survey of anesthesia-related mortality in France. Anesthesiology 2006; 105:1087–1097. [DOI] [PubMed] [Google Scholar]
- 28.Ellis SJ, Newland MC, Simonson JA, et al. Anesthesia-related cardiac arrest. Anesthesiology 2014; 120:829–838. [DOI] [PubMed] [Google Scholar]
- 29.Ruiz Neto PP, Amaral RV. Cardiac arrest during anesthesia in a multicenter hospital: a descriptive study. Rev Bras Anestesiol 1986; 36:149–158. [Google Scholar]
- 30.Tiret L, Desmonts JM, Hatton F, et al. Complications associated with anaesthesia – a prospective survey in France. Can Anaesth Soc J 1986; 33:336–344. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez LP, Braz JR, Módolo MP, et al. Pediatric perioperative cardiac arrest and mortality: a study from a tertiary teaching hospital. Pediatr Crit Care Med 2014; 15:878–884. [DOI] [PubMed] [Google Scholar]
- 32.Nunes JC, Braz JR, Oliveira TS, et al. Intraoperative and anesthesia-related cardiac arrest and its mortality in older patients: a 15-year survey in a tertiary teaching hospital. PLoS One 2014; 9:e104041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murakawa T, Matsuki A. Survey of cardiac arrests during and following anesthesia and surgery for the past seven years. Masui 1991; 40:1551–1558. [PubMed] [Google Scholar]
- 34.Morita K, Kawashima Y, Irita K, et al. Perioperative mortality and morbidity in the year 2000 in 520 certified training hospitals of Japanese Society of Anesthesiologists: with a special reference to age-report of Japanese Society of Anesthesiologists Committee on Operating Room Safety. Masui 2002; 51:1285–1296. [PubMed] [Google Scholar]
- 35.Odegard KC, Bergersen L, Thiagarajan R, et al. The frequency of cardiac arrests in patients with congenital heart disease undergoing cardiac catheterization. Anesth Analg 2014; 118:175–182. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization (WHO). World healthy statistics: life expectancy Available at http://apps.who.int/gho/data/node.main.688?lang=en [Accessed June 22, 2013]. [Google Scholar]
- 37.Koga FA, El Dib R, Wakasugui W, et al. Anesthesia-related and perioperative cardiac arrest in low- and high-income countries: a systematic review with meta-regression and proportional meta-analysis. Medicine (Baltimore) 2015; 94:e1465. [DOI] [PMC free article] [PubMed] [Google Scholar]


