Abstract
Recurrent lumbar disc herniation (rLDH) is a common complication following primary discectomy. This systematic review aimed to investigate the current evidence on risk factors for rLDH.
Cohort or case-control studies addressing risk factors for rLDH were identified by search in Pubmed (Medline), Embase, Web of Science, and Cochrane library from inception to June 2015. Relevant results were pooled to give overall estimates if possible. Heterogeneity among studies was examined and publication bias was also assessed.
A total of 17 studies were included in this systematic review. Risk factors that had significant relation with rLDH were smoking (OR 1.99, 95% CI 1.53–2.58), disc protrusion (OR 1.79, 95% CI 1.15–2.79), and diabetes (OR 1.19, 95% CI 1.06–1.32). Gender, BMI, occupational work, level, and side of herniation did not correlate with rLDH significantly.
Based on current evidence, smoking, disc protrusion, and diabetes were predictors for rLDH. Patients with these risk factors should be paid more attention for prevention of recurrence after primary surgery. More evidence provided by high-quality observational studies is still needed to further investigate risk factors for rLDH.
INTRODUCTION
Sciatica is one of the common causes of disability in the community. The most common cause of sciatica is lumbar disc herniation (LDH).1 Compared with conservative treatment, surgical intervention may have greater improvements2,3 or faster rates of pain relief.4 In spite of significant improvement in surgical technique, complications such as recurrent lumbar disc herniation (rLDH) do occur.5 The recurrence rate has been reported to vary between 5% and 15%.6–8 Secondary surgery will be more difficult due to epidural fibrosis and scarring. Moreover, reoperations lead to physical and psychological suffering for patients and substantial costs for society.9,10
Risk factors for rLDH are increasingly being investigated.11–27 Many estimated risk factors have been reported in previous studies, such as age, gender, body mass index (BMI), smoking, herniation type, diabetes, and herniation level. However, results in these previous studies were not always consistent. Regarding to gender, Kim et al reported that man was a risk factor for rLDH;19 however, many other observational studies did not find significant correlations between a man and rLDH.13–15,17,23,25,26 As for smoking, some studies revealed that smoking increased the risk of postoperative recurrence,11,14,18 whereas other studies found no significant difference between smokers and nonsmokers.15,19,23 Due to inconsistent results, reliable conclusions could not be drawn on these risk factors.
In order to identify the predictors for rLDH, we have carried out a systematic review and meta-analysis based on the current evidence. The pooled estimates may help health professionals at all levels including researchers, surgeons, policy makers, care givers, and patients to identify the potential population, prevent rLDH, and investigate the mechanism further.
METHODS
Search Strategy and Selection of Studies
A systematic search of Pubmed (Medline), Embase, Web of Science, and Cochrane library was performed by 2 investigators to identify all the relevant studies from inception to June 2015. The following keywords and/or corresponding MESH terms were used: risk factor∗ or prognost∗ factor∗ or epidemiologic factor∗ or multivariate analysis; and prolapsed disc or herniated disc or disc displacement or disc herniation or disc prolapse or prolapsed disk or herniated disk or disk displacement or disk herniation or disk prolapse or ∗discectomy; and recurren∗ or relapse or reoperation or rehospitalization or readmission or failure.
Two independent reviewers performed the search, with the limitation of publications in the English language. For those studies with incomplete data, we tried to contact with the authors. Additionally, manual searches of the references cited in all the relevant articles were also conducted. Disagreements were resolved by consensus, and a third reviewer was consulted if necessary. All analyses were based on previous published studies; thus no ethical approval and patient consent were required.
Selection Criteria
Only studies fulfilling the following inclusion criteria were included in this systematic review: (1) observational study (case-control or cohort study) investigating risk factors of rLDH; (2) studies reported (or enough data to calculate them) estimates of odds ratio (OR), relative risk (RR) or hazard ratio (HR) with their corresponding 95% confidence interval (CI); (3) clear diagnosis of rLDH by medical record or symptoms with radiographic findings; (4) study reported in English.
Those studies that were published for the same study population or not original studies were excluded from the current systematic review. In the event of disagreement between the 2 reviewers regarding whether a study met inclusion criteria, consensus was reached by joint review.
Data Extraction and Quality Assessment
Two reviewers independently extracted data from the selected papers including authors, published year, study location, case-control or cohort studies, number of cases and controls, related risk factors, corresponding OR, RR, or HR, and 95% CI. If the included studies reported several multivariable-adjusted effect estimates, the fully adjusted for potential confounding variables were selected. Newcastle–Ottawa Scale (NOS) was used for quality assessment. We considered studies with an NOS score of 7 or more to be high quality.
Statistical Analysis
The correlation between risk factors and rLDH was examined on the basis of OR, RR, or HR and 95% CI provided in the selected studies. The values of OR, RR, and HR were treated in the same manner and referred to as OR. For risk factors that had a consistent definition and a similar category across several studies, a meta-analysis was performed to obtain a pooled estimate. When not possible, a qualitative descriptive analysis was performed.
Heterogeneity among the studies was accessed by the Q test and I2 statistics. Where statistically significant heterogeneity was found (P < 0.1), the random effects model was used to combine results. Otherwise, the fixed effects model was used.28 Subgroup analyses were performed on the basis of the study design, study location, and surgical procedure. Study locations were categorized into Asia, Europe, and America. Surgical procedures were categorized into minimal invasive surgery and open surgery. Minimal invasive surgery included microendoscopic discectomy and percutaneous endoscopic discectomy, whereas open surgery included discectomy, laminotomy, and other open surgical procedures. Potential publication bias was accessed using Egger's test.29
All analyses and tests were conducted by Stata Version 12.0 (Stata Corp, College Station, TX). P < 0.05 was considered to indicate statistical significance.
RESULTS
Studies Selection
Four hundred and fifteen articles were identified using our search strategy, 119 were excluded for duplication. Then 254 articles were excluded for screening based on titles and abstracts. After the assessment of full-text articles, 25 of the remained 42 studies were excluded. Finally, 17 studies were included in this systematic review. The results of the database search were shown in a flowchart (Figure 1 ).
FIGURE 1.
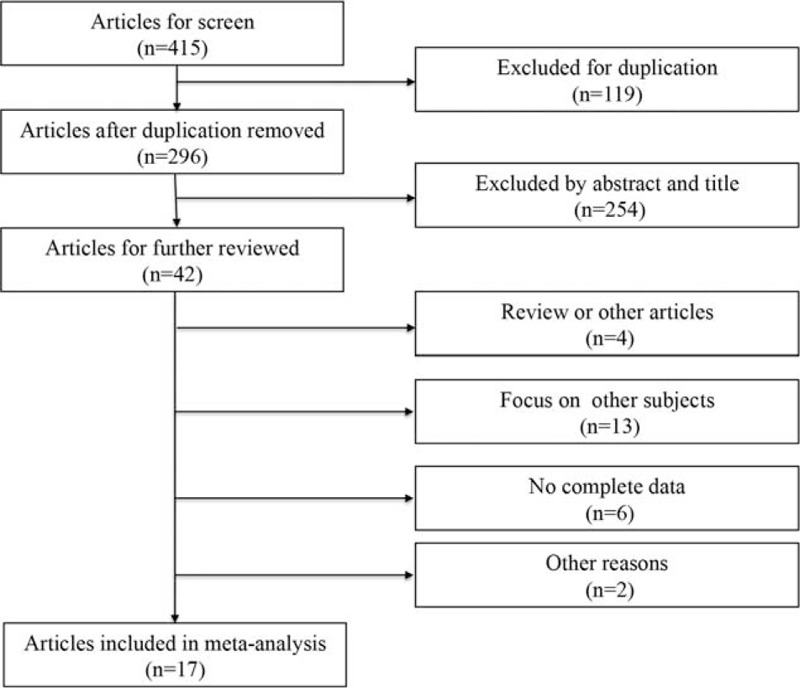
Flow diagram of study selection and identification process.
Studies Characteristics and Results
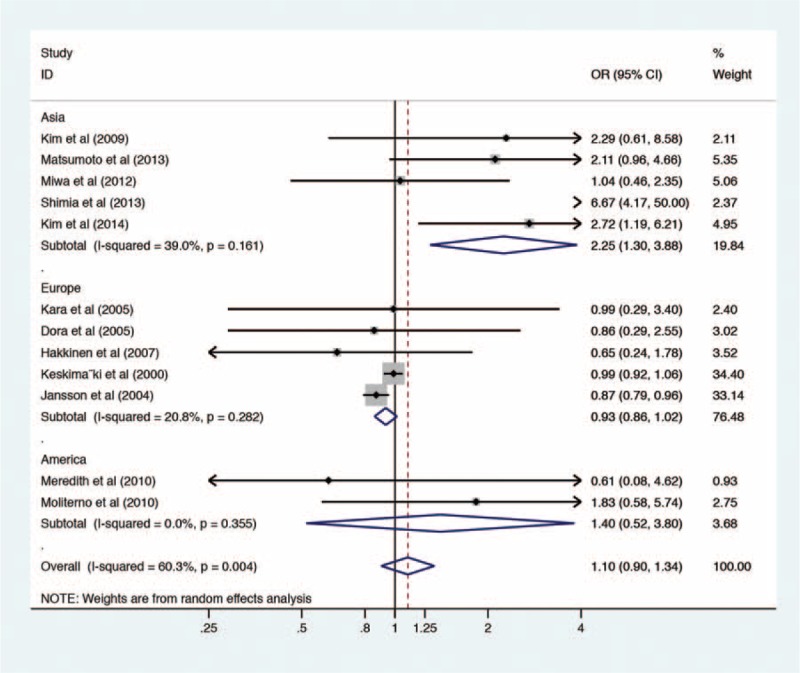
There were 13 case-control and 4 cohort studies included in this systematic review. The general characteristics of the included studies are presented in Table 1. Meta-analysis was performed to obtain pooled estimates for 7 risk factors. As judged by Egger's test, there was no evidence of publication bias being present at 5% significance level for any of the risk factors with P value of 0.105.
TABLE 1.
Characteristics of Included Studies
AGE
A total of 14 studies gave the results of age. There were 9 studies reported age as baseline data without effect size.11,13,16,18–20,23,25,26 Of the 9 studies, 8 studies showed similar age without statistical difference between recurrent and nonrecurrent group, and only 1 study by Kim20 demonstrated that patients in the recurrent group were older than those in the nonrecurrent group after percutaneous endoscopic discectomy. For the other 5 studies, it was impossible to pool the effect size due to different categorizations. A large cohort study by Jansson et al reported that patients between 40 and 59 years had a higher risk of reoperation than those <40 years, whereas the risk turned lower among patients >60 years.24 Another large cohort study by Keskimaki, however, showed significantly higher risk for patients aged <50 years compared with the older group.22
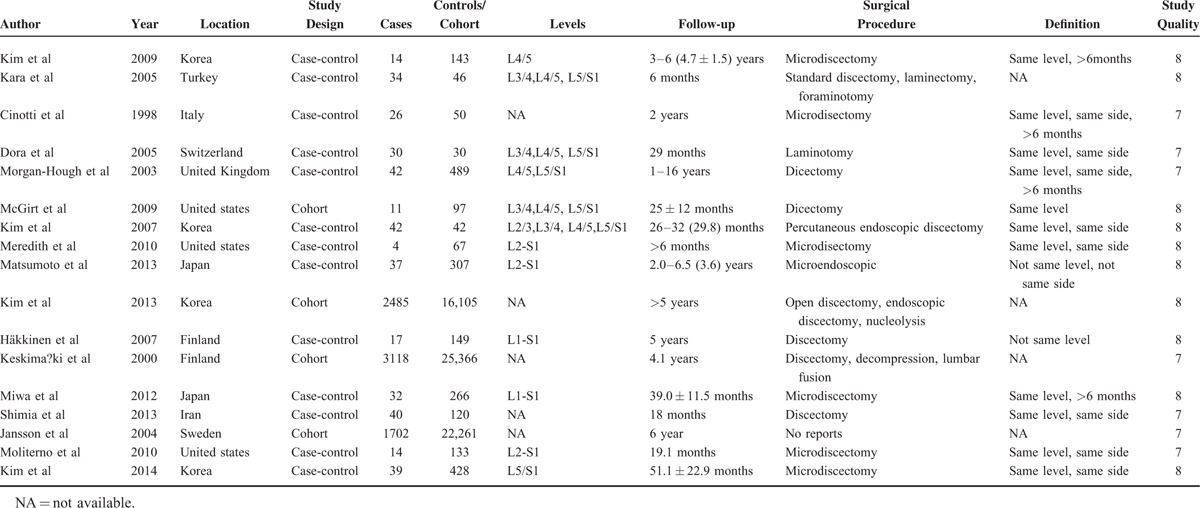
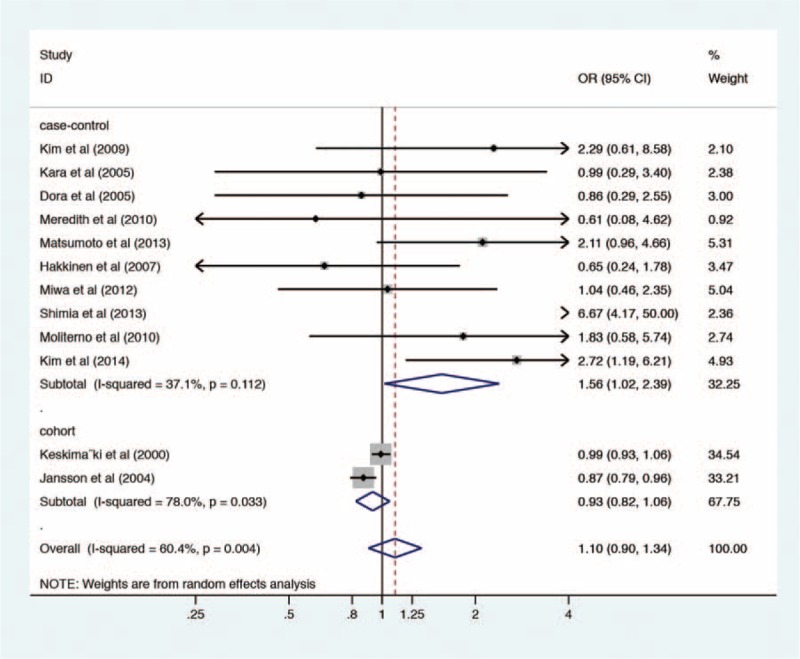
GENDER
There were 12 studies including 10 case-control studies11,13–15,17–19,23,25,26 and 2 cohort studies22,24 reporting the gender effect size. For case-control studies alone, the pooled OR for men was 1.56 (95% CI, 1.02–2.39, Z = 2.03, P = 0.042) with heterogeneity (P = 0.112, I2 = 37.1%), whereas for cohort studies, the pooled OR for men was 0.93 (95% CI, 0.82–1.06, Z = 1.09, P = 0.275) with heterogeneity (P = 0.033, I2 = 78.0%) (Figure 2). The overall estimate of men as a risk factor was 1.10 (95% CI, 0.90–1.34, Z = 0.95, P = 0.340), with heterogeneity (P = 0.004, I2 = 60.4%) (Figure 2), suggesting that no significant difference was detected between men and women in the probability of rLDH. When the included studies were classified by study location, the pooled effect size of men in Asia was 2.25 (95% CI, 1.30–3.88, Z = 2.90, P = 0.004) with heterogeneity (P = 0.161, I2 = 39.0%), in Europe was 0.93 (95% CI, 0.86–1.02, Z = 1.59, P = 0.111) with heterogeneity (P = 0.282, I2 = 20.8%), in America was 1.40 (95% CI, 0.52–3.80, Z = 0.66, P = 0.506) with heterogeneity (P = 0.355, I2 = 0%) (Figure 3). When the included studies were classified by the surgical procedure, the pooled effect size of men in the minimal invasive surgery group was 1.78 (95% CI, 1.19–2.66, Z = 2.79, P = 0.005) with heterogeneity (P = 0.539, I2 = 0.0%), in the open surgery group was 0.96 (95% CI, 0.80–1.15, Z = 0.48, P = 0.633) with heterogeneity (P = 0.013, I2 = 65.6%) (Figure 4).
FIGURE 2.
Forest plot of gender and recurrent lumbar disc herniation. OR = odds ratio.
FIGURE 3.
Forest plot of subgroup analysis by study location for gender and recurrent lumbar disc herniation. OR = odds ratio.
FIGURE 4.
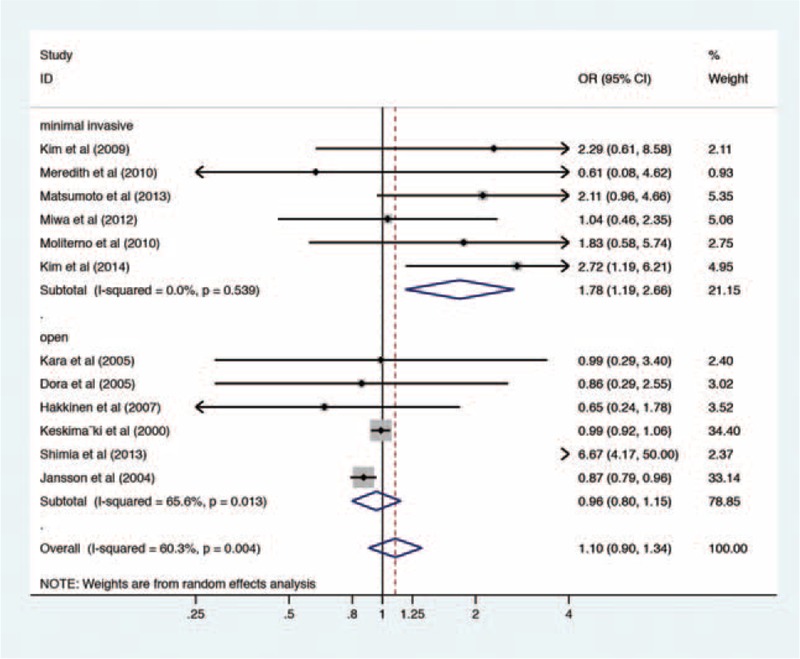
Forest plot of subgroup analysis by the surgical procedure for gender and recurrent lumbar disc herniation. OR = odds ratio.
BMI
Ten studies compared BMI between recurrent and nonrecurrent groups.11,13–15,18–20,23,25,26 The pooled analysis was only conducted in 2 studies with effect size of BMI >25 and the combined OR was 1.11 (95% CI, 0.57–2.16, Z = 0.30, P = 0.764) with heterogeneity (P = 0.543, I2 = 0.0%).13,14 The other 8 studies reported BMI as baseline data. Of the 8 studies, 2 demonstrated a higher BMI in the recurrent group15,20 and 6 showed no difference in BMI between recurrent and nonrecurrent group.11,18,19,23,25,26
SMOKING
Six case-control studies provided the effect size of smoking.11,14,15,18,19,23 The result of meta-analysis showed a low level of heterogeneity (P = 0.378, I2 = 6.0%,) and the fixed effect model was used. The pooled OR was 1.99 (95% CI, 1.53–2.58, Z = 5.15, P = 0.000), which indicated smoking increased risk of postoperative recurrence (Figure 5). Subgroup analysis was conducted based on the surgical procedure (Figure 6).
FIGURE 5.
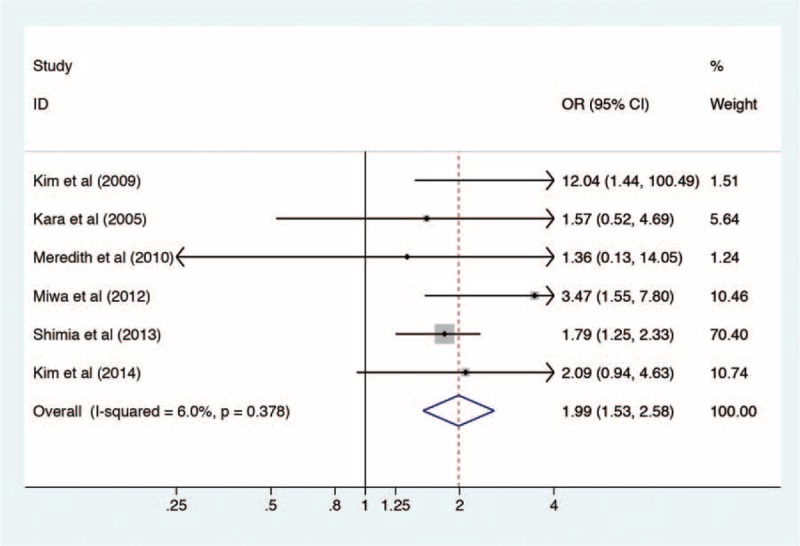
Forest plot of smoking and recurrent lumbar disc herniation. OR = odds ratio.
FIGURE 6.
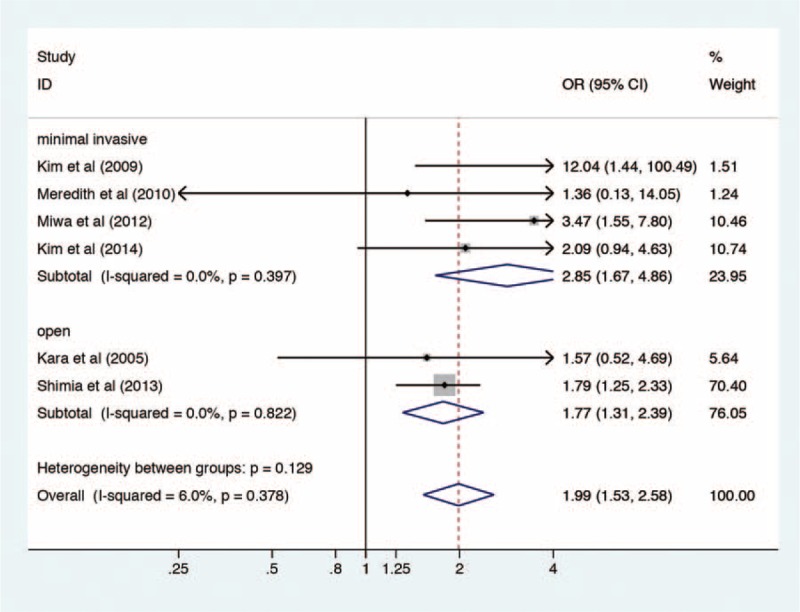
Forest plot of subgroup analysis by the surgical procedure for smoking and recurrent lumbar disc herniation. OR = odds ratio.
Type of Disc Herniation
Various classification techniques are available for LDH. In this systematic review, only classification of protrusion, extrusion, and sequestration were available to obtain pooled estimate. Data combination was based on 4 case-control studies.12,14,19,20 Due to low level of heterogeneity (P = 0.141, I2 = 45.0%), the fixed effect model was used. The pooled estimate of contained LDH was 1.79 (95% CI, 1.15–2.79, Z = 2.58, P = 0.010), suggesting that disc protrusion was a predictor for rLDH (Figure 7).
FIGURE 7.
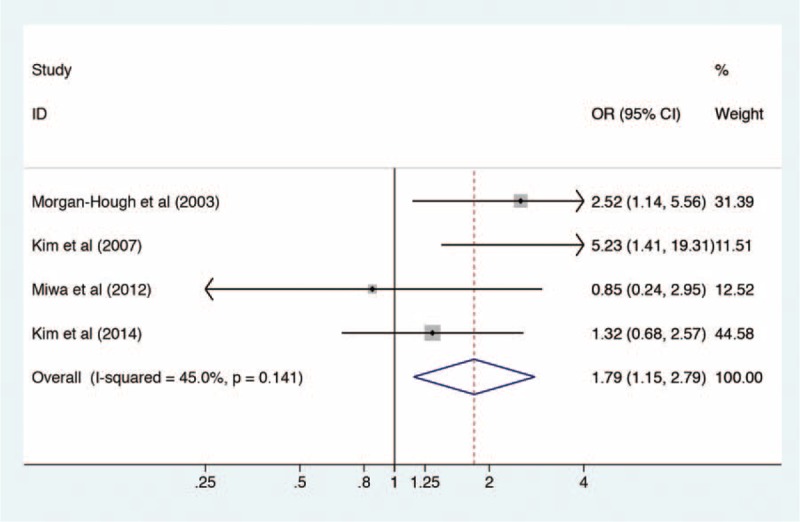
Forest plot of lumbar disc protrusion and recurrent lumbar disc herniation. OR = odds ratio.
DIABETES
One cohort and 3 case-control studies were included.11,18,19,21 The fixed effect model was used due to little heterogeneity (P = 0.388, I2 = 0.8%). The pooled OR was 1.19 (95% CI, 1.06–1.32, Z = 3.06, P = 0.002), which revealed correlation between diabetes and rLDH (Figure 8).
FIGURE 8.
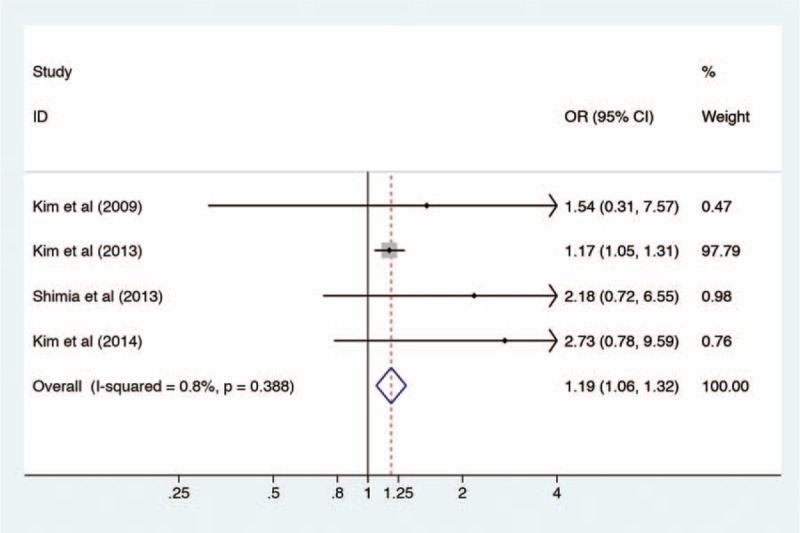
Forest plot of diabetes and recurrent lumbar disc herniation. OR = odds ratio.
Level and Side of Disc Herniation
The most commonly affected levels of LDH were L4/5 and L5/S1.With regard to the 2 levels, 4 case-control studies provided the effect size.12,13,17,25 The pooled estimate of L5/S1 level by the fixed effect model was 1.28 (95% CI, 0.84–1.96, Z = 1.15, P = 0.250), with heterogeneity (P = 0.324, I2 = 13.7%) (Figure 9). As to side of disc herniation, pooled OR of right side by 2 case-control studies was 0.91 (95% CI, 0.50–1.65, Z = 0.31, P = 0.755), with heterogeneity (P = 0.871, I2 = 0.0%).17,25 Hence, neither level nor side was a predictor for rLDH (Figure 10).
FIGURE 9.
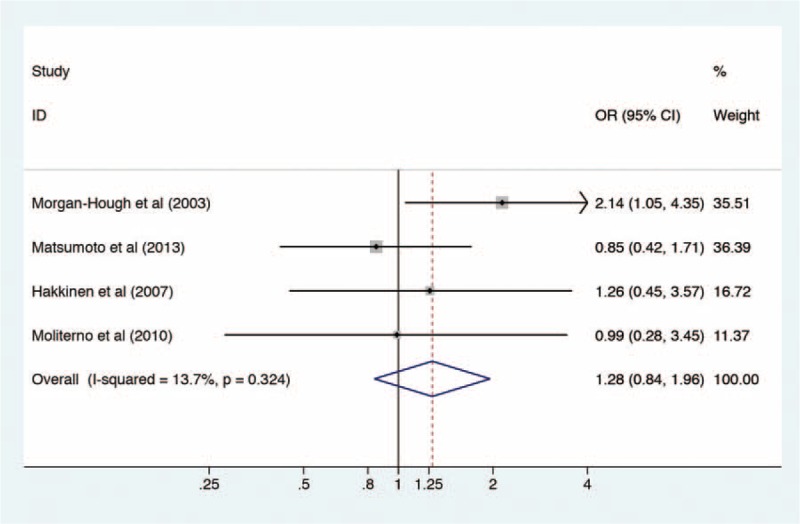
Forest plot of L5/S1 disc herniation and recurrent lumbar disc herniation. OR = odds ratio.
FIGURE 10.
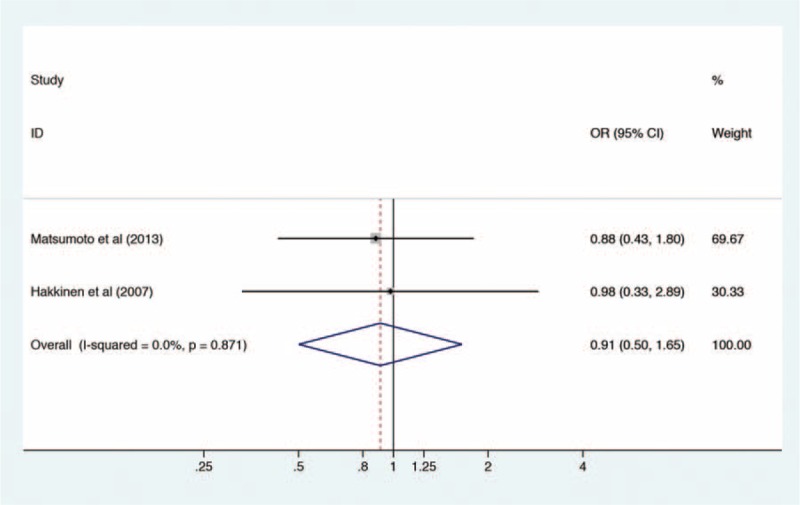
Forest plot of right-side disc herniation and recurrent lumbar disc herniation. OR = odds ratio.
Occupational Work
Three case-control studies investigated difference between light work and strenuous work.11,15,23 The pooled OR of light work were 0.91 (95% CI, 0.41–2.01, Z = 0.21, P = 0.837), with heterogeneity (P = 0.841, I2 = 0.0%).
Other Risk Factors
Kara et al reported that the lack of regular physical exercise was a significant predictor for rLDH.23 Dora et al concluded that minor disc degeneration was a risk factor for rLDH.26 Kim et al found that the recurrent group had a higher disc height index (DHI) and a more range of motion (ROM).18
DISCUSSION
This systematic review was to investigate the current evidence on risk factors for rLDH. Previous studies have explored many potential risk factors for rLDH, such as age, gender, BMI, smoking, diabetes, type of LDH, occupational work, and so on. However, pooled estimates demonstrated that only smoking, disc protrusion, and diabetes had significantly association with rLDH. With regard to gender, when subgroup analysis was based on different study locations, we found that for male patients it was more likely to suffer from rLDH when they were Asian people. When subgroup analysis was based on the surgical procedure, we found that for male patients it was more likely to suffer from rLDH when they underwent minimal invasive surgery. Concerning smoking, we speculated that for smokers it was more likely to suffer from rLDH when they underwent minimal invasive surgery by subgroup analysis.
The overall result for men showed a relatively higher heterogeneity (I2 = 60.4%). It could be found that the subgroup heterogeneity declined when subgroup analysis was based on study locations. Also we found subgroup heterogeneity in the minimal invasive surgery group disappeared when subgroup analysis was based on surgical procedures. We speculated that the heterogeneity might lie in study location and different open surgical procedures.
Smoking has been reported to contribute to many pathological processes. Many complications such as wound healing, cardiopulmonary complications after elective orthopedic surgery were related to smoking.30 This systematic review demonstrated that smoking also significantly correlated with rLDH. However, it should be noted that the weight of the study conducted by Shimia et al accumulated to 70.40%11. Hence we compared the overall result with that removing the dominant study. The pooled estimates were 1.99 (95%CI, 1.53–2.58) and 2.54 (95%CI, 1.57–4.11) respectively, which indicated that the dominant study did not have significant impact on the overall results.
The exact mechanism why smoking leads to rLDH is still incompletely understood. Previous studies have explored the potential mechanism. The defect in the annulus fibrosus and posterior longitudinal ligament after discectomy is thought to heal in normal physiological conditions. However, those toxins generated by cigarette smoking may impair or delay these normal conditions.31 Previous study demonstrated that nicotine affected disc annulus nutrition and oxygenation.32 Gill et al compared the ligament healing process in passively smoking mice with nonsmoking mice and found that cellular density in the injured ligament was significantly lower in the smoking mice. Also, the smoking mice exhibited lower type I collagen expression in the injured ligament, which was identified as the major structural component of extracellular matrix.33 Nemoto et al subjected 4-week-old rats to passive smoking for 8 weeks. They found that intervertebral discs exhibited cracks, tears, and misalignment of the annulus fibrosus and the level of interleukin-1beta in intervertebral discs was higher in the smoking group than in the nonsmoking group.34 Besides cellular and molecular changes, repetitive cough caused by smoking increased intervertebral pressure, which may also partly contribute to rLDH.35
Lumbar disc protrusion without a herniated fragment or defect in the annulus was reported to have the highest risk of rLDH by Carragee et al.7 The current meta-analysis reinforced the previous study. Pooled estimates in this meta-analysis revealed that combined OR of disc protrusion was 1.79 (95% CI, 1.15–2.79). It has been speculated that disc protrusion represents the beginning of a process of serial fragmentation of disc material, whereas extrusion and sequestration are an end-stage of this process.12 One other potential reason could be that lump removal was possible in most cases with disc extrusion or sequestrations, whereas relatively less disc removal is performed in most cases with disc protrusion.12
This systematic review also showed that diabetes correlated with rLDH, with the pooled OR 1.19 (95% CI, 1.06–1.32). It should also be noted that the weight of study by Kim et al was up to 97.79%.21 Likewise, pooled results with and without the dominant study were compared. The pooled estimates were 1.19 (95%CI, 1.06–1.32) and 2.19 (95%CI, 1.05–4.57) respectively, which indicated that the results did not reverse when the dominant study was trimmed. Previous studies have explored the mechanisms. Robinson et al compared the intervertebral discs between nondiabetic and diabetic patients using discarded discs from operations. They found that the proteoglycans from diabetic subjects were banded at a lower buoyant density, which indicated a lowered glycosylation rate and a lower number of sugar side chains per core protein. They also found that there was a slight increase in the chain length of chondroitin sulfate in the diabetic group and further analysis of the glycosaminoglycan chains showed a decreased amount of keratan sulfate glycosaminoglycan.36 They concluded that these changes might lead to increased susceptibility to disc prolapse. Besides that, as Carragee reported, the competence of annulus fibrosis might be valuable for the prediction of the recurrence after lumbar discectomy.7 For diabetic subjects, annulus fibrosis healing might take longer time and not be as sturdy as nondiabetic subjects.
There are several other most commonly mentioned risk factors such as age, gender, BMI, occupational work, level of disc herniation, and so on. Due to different categorizations, pooled effect size of age was unavailable. The included studies had inconsistent results11,13,14,16–20,22–26 and a conclusion could not be drawn based on the current evidence. As for gender, pooled OR in case-control studies showed men were more likely to suffer from rLDH. However, the results were not significant when combined with cohort studies. BMI was another widely concerned risk factor. Most included studies compared BMI as baseline data and these inconsistent results could not come to a conclusion. The combined OR of BMI >25 by 2 case-control studies still found no significant relations between BMI and rLDH. With respect to occupational status, it is generally accepted that heavy physical labor leads to increased loading of lumbar disc, which may contribute to rLDH.35,37,38 However, pooled estimates in the systematic review did not show a correlation between work status and rLDH. The L5/S1 level was detected to be related to higher recurrence rate by Morgan-Hough.12 But pooled effect size did not reveal a higher risk of recurrence in patients with L5/S1 LDH. Likewise, no significant difference was detected between the left and the right side for rLDH.
Several limitations in this systematic review should be pointed out. First, the definition of rLDH in the included studies was incomplete consistent. Clinically, it is more appropriate to define rLDH as reherniation at the same level and same side. However, some of the included studies defined the rLDH regardless of the length of pain-relief period and some regardless of herniation side (Table 1). Regarding the surgical procedures, the selected studies included discectomy, microdiscectomy, and percutaneous transforaminal endoscopic discectomy as shown in Table 1. Various definitions of rLDH and different surgical procedures may both generate heterogeneity. Second, OR and RR were treated in the same way in this systematic review. Generally, it is reasonable to combine OR with RR when the incidence was low (<10%). With the incidence turning higher, combination of OR and RR is more likely to generate bias.39 For rLDH, the incidence has been reported to varied from 5% to 15%,which may potentially give rise to bias. Third, some risk factors in this meta-analysis were limited by a small number of included studies. Besides, not all the selected studies reported estimates of risk adjusted for confounders and some ORs were calculated by the crosstab data without adjustment. Hence the pooled estimates may include some confounding of the true relationship between risk factors and rLDH. Fourth, although recommended by the Cochrane Collaboration,40 the NOS was argued about unclear weighting scheme, which might lead to a limited exploration of the studies quality.41
CONCLUSION
This meta-analysis revealed that smoking, disc protrusion, and diabetes were predictors for rLDH. Patients with these risk factors should be paid more attention for prevention of rLDH. The exact mechanism between risk factors and rLDH warrants further investigation. Due to a limited number of literature, more evidence provided by high-quality observational studies are still needed to investigate risk factors for rLDH further.
Acknowledgments
The authors are grateful to the researchers of the included studies in this meta-analysis.
Footnotes
Abbreviations: BMI = body mass index; CI = confidence interval; DHI = disc height index; HR = hazard ratio; LDH = lumbar disc herniation; NOS = Newcastle–Ottawa Scale; OR = odds ratio; rLDH = recurrent lumbar disc herniation; ROM = range of motion; RR = relative risk.
Author contribution: XCY conceived the idea and contributed to design. WMH and ZWH ran the searches and extracted data. WMH and JL assessed the methodological quality. WMH, JL, and LLY conducted the meta-analysis. WMH and ZWH wrote the manuscript. All authors approved the final version of the manuscript.
Funding: No funds were received in support of this work. No benefits have been or will be received from a commercial party related to the subject of this manuscript.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Ropper AH, Zafonte RD. Sciatica. New Engl J Med 2015; 372:1240–1248. [DOI] [PubMed] [Google Scholar]
- 2.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA 2006; 296:2451–2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT). Spine 2008; 33:2789–2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peul WC, van Houwelingen HC, van den Hout WB, et al. Surgery versus prolonged conservative treatment for sciatica. New Engl J Med 2007; 356:2245–2256. [DOI] [PubMed] [Google Scholar]
- 5.McGirt MJ, Ambrossi GL, Datoo G, et al. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery 2009; 64:338–344.discussion 344–335. [DOI] [PubMed] [Google Scholar]
- 6.Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus 2003; 15:E10. [DOI] [PubMed] [Google Scholar]
- 7.Carragee EJ, Han MY, Suen PW, et al. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am 2003; 85:102–108. [PubMed] [Google Scholar]
- 8.Leven DM, Passias PG, Errico TJ, et al. Risk factors for reoperation in patients treated surgically for intervertebral disc herniations: a subanalysis of the eight-year data from the sport trial. Spine J 2014; 14:S95–S96. [Google Scholar]
- 9.Ambrossi GL, McGirt MJ, Sciubba DM, et al. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery 2009; 65:574–578. [DOI] [PubMed] [Google Scholar]
- 10.Legrand E, Bouvard B, Audran M, et al. Sciatica from disk herniation: medical treatment or surgery? Joint Bone Spine 2007; 74:530–535. [DOI] [PubMed] [Google Scholar]
- 11.Shimia M, Babaei-Ghazani A, Sadat BE, et al. Risk factors of recurrent lumbar disk herniation. Asian J Neurosurg 2013; 8:93–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan-Hough CV, Jones PW, Eisenstein SM. Primary and revision lumbar discectomy: a 16-year review from one centre. J Bone Joint Surg Br 2003; 85:871–874. [PubMed] [Google Scholar]
- 13.Moliterno JA, Knopman J, Parikh K, et al. Results and risk factors for recurrence following single-level tubular lumbar microdiscectomy: clinical article. J Neurosurg—Spine 2010; 12:680–686. [DOI] [PubMed] [Google Scholar]
- 14.Miwa S, Yokogawa A, Kobayashi T, et al. Risk factors of recurrent lumbar disc herniation: a single center study and review of the literature. J Spinal Disord Tech 2013; 28:E265–E269. [DOI] [PubMed] [Google Scholar]
- 15.Meredith DS, Huang RC, Nguyen J, et al. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J 2010; 10:575–580. [DOI] [PubMed] [Google Scholar]
- 16.McGirt MJ, Eustacchio S, Varga P, et al. A prospective cohort study of close interval computed tomography and magnetic resonance imaging after primary lumbar discectomy: factors associated with recurrent disc herniation and disc height loss. Spine 2009; 34:2044–2051. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto M, Watanabe K, Hosogane N, et al. Recurrence of lumbar disc herniation after microendoscopic discectomy. J Neurol Surg 2013; 74:222–227. [DOI] [PubMed] [Google Scholar]
- 18.Kim KT, Park SW, Kim YB. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation. Spine 2009; 34:2674–2678. [DOI] [PubMed] [Google Scholar]
- 19.Kim KT, Lee DH, Cho DC, et al. Preoperative risk factors for recurrent lumbar disc herniation in L5-S1. J Spinal Disord Tech 2014; 28:E571–E577. [DOI] [PubMed] [Google Scholar]
- 20.Kim JM, Lee SH, Ahn Y, et al. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invas Neurosur 2007; 50:82–85. [DOI] [PubMed] [Google Scholar]
- 21.Kim CH, Chung CK, Park CS, et al. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine 2013; 38:581–590. [DOI] [PubMed] [Google Scholar]
- 22.Keskimaki I, Seitsalo S, Osterman H, et al. Reoperations after lumbar disc surgery. Spine 2000; 25:1500–1508. [DOI] [PubMed] [Google Scholar]
- 23.Kara B, Tulum Z, Acar U. Functional results and the risk factors of reoperations after lumbar disc surgery. Eur Spine J 2005; 14:43–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jansson KA, Nemeth G, Granath F, et al. Surgery for herniation of a lumbar disc in Sweden between 1987 and 1999: an analysis of 27,576 operations. J Bone Joint Surg Br 2004; 86:841–847. [DOI] [PubMed] [Google Scholar]
- 25.Hakkinen A, Kiviranta I, Neva MH, et al. Reoperations after first lumbar disc herniation surgery: a special interest on residives during a 5-year follow-up. BMC Musculoskel Dis 2007; 8:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dora C, Schmid MR, Elfering A, et al. Lumbar disk herniation: do MR imaging findings predict recurrence after surgical diskectomy? Radiology 2005; 235:562–567. [DOI] [PubMed] [Google Scholar]
- 27.Cinotti G, Roysam GS, Eisenstein SM, et al. Ipsilateral recurrent lumbar disc herniation: a prospective, controlled study. J Bone Joint Surg Br 1998; 80:825–832. [DOI] [PubMed] [Google Scholar]
- 28.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moller AM, Pedersen T, Villebro N, et al. Effect of smoking on early complications after elective orthopaedic surgery. J Bone Joint Surg Br 2003; 85:178–181. [DOI] [PubMed] [Google Scholar]
- 31.Neaton JD, Wentworth D. Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316,099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med 1992; 152:56–64. [PubMed] [Google Scholar]
- 32.Yildiz D. Nicotine, its metabolism and an overview of its biological effects. Toxicon 2004; 43:619–632. [DOI] [PubMed] [Google Scholar]
- 33.Gill CS, Sandell LJ, El-Zawawy HB, et al. Effects of cigarette smoking on early medial collateral ligament healing in a mouse model. J Orthop Res 2006; 24:2141–2149. [DOI] [PubMed] [Google Scholar]
- 34.Nemoto Y, Matsuzaki H, Tokuhasi Y, et al. Histological changes in intervertebral discs after smoking and cessation: experimental study using a rat passive smoking model. J Orthop Sci 2006; 11:191–197. [DOI] [PubMed] [Google Scholar]
- 35.Kelsey JL, Githens PB, O’Conner T, et al. Acute prolapsed lumbar intervertebral disc: an epidemiologic study with special reference to driving automobiles and cigarette smoking. Spine 1984; 9:608–613. [DOI] [PubMed] [Google Scholar]
- 36.Robinson D, Mirovsky Y, Halperin N, et al. Changes in proteoglycans of intervertebral disc in diabetic patients: a possible cause of increased back pain. Spine 1998; 23:849–855. [DOI] [PubMed] [Google Scholar]
- 37.Mundt DJ, Kelsey JL, Golden AL, et al. An epidemiologic study of non-occupational lifting as a risk factor for herniated lumbar intervertebral disc. The Northeast Collaborative Group on Low Back Pain. Spine 1993; 18:595–602. [DOI] [PubMed] [Google Scholar]
- 38.Schmidt H, Kettler A, Heuer F, et al. Intradiscal pressure, shear strain, and fiber strain in the intervertebral disc under combined loading. Spine 2007; 32:748–755. [DOI] [PubMed] [Google Scholar]
- 39.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. Jama 1998; 280:1690–1691. [DOI] [PubMed] [Google Scholar]
- 40.Higgins JPT GS. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011 [Google Scholar]
- 41.Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25:603–605. [DOI] [PubMed] [Google Scholar]


