Summary
The goal of Occupational Medicine and Hygiene is that of ensuring safety, health and well-being at workplaces, mainly assessing and preventing existing occupational risks. Scientific research in this field can provide useful arguments and further evidence upon which effective, efficient and sustainable policies and preventive measures have to be chosen and applied by the occupational physician in work-life. This paper summarizes four original studies, conducted in different professional settings across Italy, focusing on critical items, such as stress and violence, biological risks and sleep hygiene. The knowledge obtained can be useful to orientate proper preventive programs aimed at improving workplace health.
Key words: Stress and violence, Biological risk, Sleep hygiene
Introduction
Applied research in the field of Occupational Medicine and Hygiene can provide arguments and scientific evidences to properly choose and implement effective, efficient and sustainable policies and preventive measures in order to ensure safety, health and well-being at workplaces. In this way, a strong basis for the development, application and constant monitoring of practical methods and tools can be provided to the occupational physician at the company level, both in the public and private settings.
Occupational Hygiene has a broad scope, in that deals with the protection, safety and health of workers from work-related hazards, systematically anticipating, recognizing, evaluating and controlling the risks, which can be subdivided into biological, chemical, physical, ergonomic and psychosocial ones [1].
In this article, four original researches performed in different workplaces across Italy, focused on some critical issues in the field of occupational safety and health and the main categories of work-related risks (i.e., the assessment and management of the risks associated to stress, violence, and biological exposure in workers employed in health-care settings, together with those associated with sleep disorders and sleepiness among truck drivers), are summarized below.
These studies represent the scientific activity carried out by the National Working Group in Occupational Hygiene born within the Italian Society of Hygiene, Preventive Medicine and Public Health (SItI), with the collaboration of both occupational medicine and hygiene units. The highly interdisciplinary nature of this Working Group is reflected by its effort of integrating the knowledge, the goals and skills of the two disciplines for the sake of safety of the worker in different workplaces.
Study 1: Risk assessment of stress and violence in an Italian regional referral Hospital
INTRODUCTION
The work-related stress is a significant aspect in the management of health and safety in healthcare, both because of the peculiarity of the sector and because of the progressive reduction of resources, particularly human ones, resulting in continuous and repeated linear cuts to spending. This type of spending review acts indifferently on both not perfectly efficient areas and on areas with an appropriate allocation of resources, without a prior analysis and reorganization of the processes; the consequences are, often, an unjustified increase in the workload, feeling of inadequacy, and frustration [2, 3].
The actual legislation requires the employer to evaluate all risks for health and safety, including those caused by work-related stress, and refers to the indications of the Standing Advisory Commission on health and safety at work for the details of such assessment (Law Decree 81/2008, art.28, comma 1-bis) [4, 5].
The Commission has identified the criteria to be considered: sentinel events (accident rates, sick leave, turnover, reports of physicians); job characteristics (environments and workloads, working hours and shifts, limited knowledge of the procedures and/or inadequate skill); and correspondence between worker skills and job requirements [6].
A special role is played by the episodes of aggression towards workers, both verbal and physical, increased in the last years [7]. Occupational or work-related violence in health-care settings is a growing phenomenon that can be defined as an incident in which a perpetrator abuses, threatens, or assaults a health-care worker (HCW) in work-related circumstances. Gillespie and collaborators have reviewed the main HCW risk factors: these are gender, age, years of experience, workload, relationship status, and previous workplace violence training [8].
METHODS
The IRCCS AOU San Martino-IST of Genoa, Italy, the Regional teaching and research hospital of Liguria Region, established an internal working group to assess the work-related stress and the specific risk factors represented by attacks on workers. The group consists of the Occupational Medicine Unit, the Prevention and Protection Service, the Clinical Psychology Unit, the Psychiatric Unit, the Workers' Representatives for safety (RLS), and the various components of the Executive Board. In the absence of a National or Regional benchmark, the Working Group decided to stratify the risk levels within the IRCCS, in order to obtain a priority scale of remedial measures.
The group elaborated a set of indicators divided into three areas:
risk indicators: hours worked, missed holidays, overtime, night and holidays shifts, tasks breaks, characteristics of the environments, complex postures and positions, medical restriction, adverse events and complaints, performance during emergencies, critical patients, etc.;
disclosure indicators: days of absence, number of accidents, questions of internal mobility and transfers, appeals to the reception, occupational stress, etc.;
contrast indicators: internal communication system and methods for the reception of new employees, training, internal audits.
The indicators were measured at the level of the single operating units and normalized by the number of workers; then, for each one, the average or median, depending on their distribution, was computed. For each operating unit, the indicator was considered expression of the risk if placed in the negative side respecting to the central position index; the percentage of negative indicators out of the total of the available indicators provided a measure of the level of work-related stress in the operative unit, considering the IRCCS as benchmark.
Regarding the attacks on workers, a preliminary analysis of some operating units (medicine, neurology, emergency room, intensive care, infectious diseases, and psychiatry) was carried out through the Overt Aggression Scale (OAS) questionnaire filled in by the operators over a period of four months. The questionnaire, which allows the description of the various aspects of each episode of violence, has been entered in a database and subjected to statistical analysis using multidimensional techniques, like Correspondence analysis, which enables to display categorical data in two-dimensional graphical form.
RESULTS
The stress evaluation with the method described above during three years allowed us to identify the areas at greatest risk inside the IRCCS (namely, medicine, neurology, emergency room, intensive care, infectious diseases, and psychiatry) on which work was carried out through focus groups and further investigation by the operative unit of Clinical Psychology. In addition, the table of risk stratification has facilitated the redeployment of workers to which the Occupational Medicine Unit ordered exposure restriction to this specific factor, for pre-existing pathological conditions or individual hypersensitivity (insufficient coping strategies).
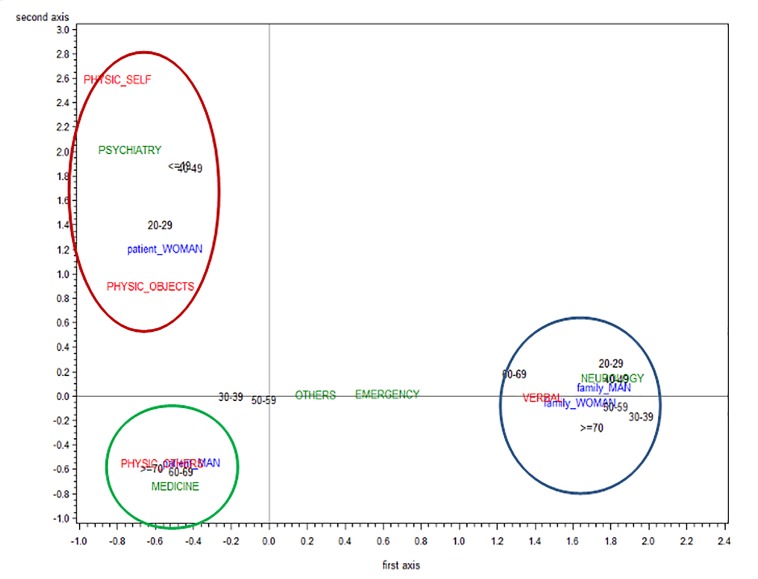
The recording of OAS questionnaires on violence has enabled the analysis of 267 episodes, of which approximately 50% with physical aggression (towards the operators, but also objects and oneself). The distribution of their characteristics: aggressor (patient, family or other persons), kind of event (physical aggression preceded or not by verbal aggression) and the victim (the operator, the objects, the aggressor himself, in various combinations) was significantly different depending on the type of departments. The various features were also associated with each other in an absolutely not random way; in the departments of medicine, there were mainly aggression by elderly male patients, while in the departments of neurology, patient's relatives of both sex verbally assaulted staff; in psychiatry unit, it was mainly the young female patient to implement violence mostly to herself and to the objects (Fig. 1). Even the temporal distribution during the day differed significantly in various types of departments. In particular, peaks in early morning, afternoon/ early evening could be noticed in psychiatry and emergency room departments, respectively. No peaks could be detected in neurology ward, whilst distribution in medicine wards was varied throughout the day.
Fig. 1.
Correspondence analysis. Distribution of event characteristics: type and age of the aggressor, type of the aggression, setting of the aggression (hospital unit).
Notes: Data collected with Overt Aggression Scale (OAS) questionnaire; statistical analysis performed with SAS procedures rel.9.2
CONCLUSIONS
The evaluation of work-related stress made in a structured way, through indicators and specific questionnaires, is a valuable tool to identify areas at risk and their characteristics. It enables the development of preventive measures and identifies their key-objectives as well as facilitates the management of workers with limitations.
Study 2: Sleep disorders and sleepiness: major risk factors in road accidents and injuries for truck drivers
INTRODUCTION
Excessive daytime sleepiness (EDS) is a common condition in our society that can be caused by both physiological and pathological factors. The physiological origin of EDS comes from a modern irregular lifestyle and is due to the rhythms of our "24 hours society" and work organization (shift work, night work, extratime, overtime), that causes sleep debt and the disruption of the circadian sleep-wake rhythm. The pathological causes of EDS are various but the main one is Obstructive Sleep Apnea Syndrome (OSAS). OSAS is a chronic breathing disorder, characterized by recurrent episodes of partial or complete obstruction (hypopnea / apnea) of the upper respiratory airways during sleep, that lead to a decrease in nocturnal oxygen saturation and micro-awakenings. Accordingly, OSAS causes sleep fragmentation, non-restorative sleep and EDS; moreover, it is the main risk factor for serious diseases, such as metabolic disorders, diabetes and cardio/cerebra-vascular disorders [9].
Studies conducted over the past twenty years show a significant relationship between sleep disorders, EDS and accidents/injuries [10]. EDS is indeed the cause of more than 20% of all traffic accidents [11] and increases the risk of being the victim of a fatal accident eightfold [10]. Truck drivers are considered the group of workers most exposed to the risk of EDS-related accidents. This is mainly due to the high prevalence of OSAS among professional drivers [12], the work rhythms and the sleep habits of these workers. The aim of this study, done for the first time in Europe in a mobile medical clinic equipped with advanced technology, was to evaluate the prevalence of sleep debt, OSAS, EDS and traffic accidents in a sample of truck drivers.
METHODS
This study was carried out as part of "CNH Iveco Industrial Check-Stop Project", an international program of prevention and information for road safety in collaboration with the Departments of Neuroscience and Health Sciences of the University of Genoa, and sponsored by the Ministry of Transport, the Unione Interporti Riuniti and the Italian Association of Sleep Medicine (AIMS).
The research was carried out in 2014, in the major Italian trucking hubs (Turin, Novara, Verona, Bologna, Rome and Naples). The clinical protocol included different phases:
standardized and validated questionnaires (Epworth Sleepiness Scale - ESS; Berlin Questionnaire) and a structured interview about sleep habits, sleep disorders (sleep disorders score - SDS) and driving safety and accidents that have occurred in the past three years;
semeiotic and clinical evaluation, and screening for sleep disorders and EDS;
identification of potential subjects with suspected OSAS and / or EDS;
information / education for each participant who resulted negative in the sleep disorder and EDS screening, regarding sleep hygiene and healthy lifestyle behaviors for the prevention of accidents and EDSrelated injuries.
RESULTS
The data presented in this study are preliminary and based on a sample composed of 728 drivers. The participants were all males, from across the country but belonging to different ethnic groups, with a range of age between 18 to 81 (mean 44.2 ± 10.2 years) and a BMI (body mass index) average of 28.5. The presence of at least one co-morbidity, such as hypertension, dyslipidemia and diabetes, was found in 36.3% of participants.
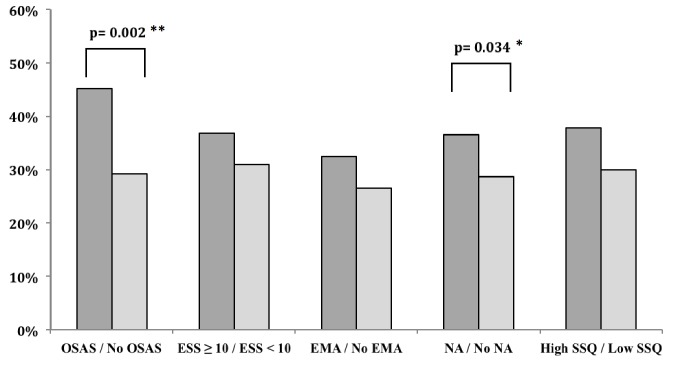
A condition of sleep debt because of nighttime awakenings or early morning awakenings was found in 21.3% of the analyzed sample. Only 31.4% of participants were satisfied with the quality of their sleep. EDS was reported in 10% and for 37.2% was expressed a suspicion of OSAS; of these, 57% had at least one co-morbidity, such as hypertension, dyslipidemia and diabetes. 31.5% had at least one accident / injury in the last 3 years. Figure 2 shows the association between OSAS, sleep debt, EDS and traffic accidents.
Fig. 2.
Accidents at workplace in participant with and without OSAS, EDS, sleep debt, and poor subjective sleep quality.
CONCLUSIONS
The preliminary data obtained confirm the high prevalence of sleep debt and OSAS in truck drivers reported in the literature. From the results emerges an important relationship between sleep debt and the presence of traffic accidents [13]. These results confirm the urgent need for a prior assessment focused on EDS and OSAS in the activities of primary prevention and health surveillance [14] especially in the categories of workers that require high levels of alertness and therefore at greater risk of accidents/injuries. It is important to manage the health risks and safety of professional drivers by minimizing risk factors inducing EDS through screening of sleep disorders together with other lifestyle approaches.
Study 3: Assessment of the compliance with hygiene and safety procedures, and their perception by professionals, within a network of dental practices in Rome, Italy
INTRODUCTION
A number of studies has been published regarding the critical issues on the health and safety at workplace within dental practices. In recent years, notwithstanding the technical progress made, problems, including injuries by percutaneous exposure, exposure to bioaerosols, radiations, chemical agents and noise, persist in this setting [15]. Other professional items, such as muscular-skeletal disorders, dermatitis, eye and psychological problems, have also been notified [16]. Strategies aimed at reducing the number of unfavourable events include on-going education, hygiene of the premises, personal protection equipments, adequate sterilization and other high-level disinfection techniques. Some studies, mainly based upon self-administered questionnaires, have investigated procedures, educational programmes, hygiene conditions and the complications associated to HBV, HCV and HIV infections reported among dentists in various Regions and cities in Italy. Table I summarizes these studies searched in a systematic way, looking up for a proper string of key-words such as "hygiene", "dentist" and "questionnaire", using Medical Sub- Headings (MeSH) terms where adequate [17-22]. In a dental working environment a number of procedures can generate bacterial aerosol and droplets and concentrations appear to be higher during interventions involving ultrasonic ablation, or during procedures using high speed drills: it is therefore possible that airborne infectious agents may be transmitted to staff and patients, especially if the overall hygiene procedures in the work-place are not adequate [23]. Some procedures, such as pre-procedural rinsing performed by patients with mouthwash and electrostatic extraction of aerosol during dental procedures, certainly represent useful preventive measures. Further, adherence of the professionals to recommended vaccinations and the proper use of personal protective equipment can reduce the contact with bacterial droplets and aerosols, particularly during invasive and prolonged interventions.
Tab. I.
Summary of the studies, undertaken by questionnaires, investigating the safety and the hygiene conditions in dental practices across Italy.
| Parameters | M.G. Galli et al., 2000 |
C. Germinario et al., 2001 |
M.T. Montagna et al., 2003 |
L. Veronesi et al., 2004 |
F. Vitale et al., 2005. |
Fabiani et al., 2006 |
M.L. Cristina et al., 2009 |
|---|---|---|---|---|---|---|---|
| STUDY CONTEXT Dental studios | Public and privates in Milan | Privates in Bari | Privates in 11 Italian cities | Privates in Parma | Privates in Palermo | Privates in L'Aquila | Private and public sector in Genoa |
| OBJECTIVES Evaluation of | Awareness of risk factors of different nature (chemical, physical, biological) | Awareness and practice for prevention of infection | Awareness of infection risks and control procedures | Awareness and measures adopted within procedures of infection control | Awareness, aptitude and measures adopted for control of infections and programming of awareness and educational intervention | Awareness and measures adopted within procedures of infection control | Procedures and measures adopted for control and prevention of infections |
| MATERIALS & METHODS | Anonymous questionnaire to be returned + telephone survey | Anonymous questionnaire to complete and return | Anonymous questionnaire to complete and return | Questionnaire sent by email | Anonymous questionnaire to complete and return | Validated questionnaires to complete and return | Questionnaire by interview or sent by post |
| SUBJECTS RECRUITED Responders/ Total (%) | 116/231(50.2%) | 94/200 (47.0%) | 444/1000 (44.4%) | 122/400 (30.5%) | 254/675 (37.6%) | 82/127 (64.6%) | 106/176 (60.2%) |
| PERSONAL DATA RESPONDERS | |||||||
| Average age ( ±DS) | 40 years (range 25-68) | 40 years | 42.2 years (DS=9.4) | 43years (DS=9.7) | 43.6 years (±DS=9.7) | 41 years (DS=8) | < 30 years in 10.4% of cases, 30-50 years in 73.6% of cases, >50 years in 16% of cases |
| - Degree | 47% with a degree in Medicine and a specialization in Stomatology, 28% with a degree in Medicine, 25% with a degree in Dentistry | 76.6% degree in Medicine | 60.4% degree in Medicine | 62% degree in Medicine | 47.7% degree in Medicine | 53% degree in Medicine, 34.9% degree in Dentistry, 47% in odontology and dental prosthesis | NA |
| - Work experience (average years ± DS) | 1-42 years | 13.3 years | 14.2 years | 15 years | 14.5 years | 13 years (DS = 7) | NA |
| - Hours worked (average hours/ week) | < 20 hours/week in 10% of cases, 20-29 hours/week in 11% of cases, 30-39 hours/week in 25% of cases, 40-49 hours/week in 38% of cases, > 50 hours/week in 16% of cases | 27.8 hours/week | 20-49 hours in 69.2% | 20-49 hours | 30-50 hours in 57.7% | 13.5% about 20 hours/ week, 78% 20-49 hours/ week, 8.5% > 50 hours/ week | NA |
| Number of patients/day (average) | NA | NA | NA | NA | NA | NA | < 10 patients/day in 26.4% of cases, 10-20 patients/day in 36.8% of cases, >20 patients/ day in 36.8% of cases |
| BIOLOGICAL RISK: KNOWLEDGE, EVALUATION (Focus on) | Epidemiological (transmission and exposure, comparative risk evaluation) | Epidemiological (transmission and exposure, comparative risk evaluation) | Epidemiological (exposure, risk categories) | Risk perception and knowledge | Epidemiological (transmission, biological samples, categories at risk, comparative risk evaluation) | Epidemiological (exposure, risk categories) | Risk awareness |
| VACCINE | 76% vaccinated for HBV, seroconversion verified in 72% of subjects Diagnostic checks for HBV (72%), HCV (70%), HIV (70%) |
75% HBV and 53% has immunized staff | 79.5% HBV, only 55.2% verified seroconversion Diagnostic checks for HBV (67.8%), HCV(67.8%) HIV (57,6%) |
89% HBV and 72% seroconversion | 76.2% believe HBV necessary | 82% HBV and 70% seroconversion Diagnostic checks: for HBV (76.5%) for HCV (78%) and for HIV (69.5%) |
86.8% HBV |
| PROFESSIONAL INJURIES / ILLNESSES | Accidental exposure to hazards (20% wound by needles at least once in last years, 13% at least twice in last years, 8% at least 3 times) Professional illness (5 cases of HBV, 2 cases of HSV) |
Accidental injuries with needles or sharp (63% yes, sometimes and 1% frequent) | Accidental (38.5% with needles) Infective disease (1,9% hepatitis) |
Accidental injuries with needles or other within last 5 years (73% yes) Professional illness (HBV 1.6%, HSV1 0.8%) | Pricks and cuts in last year (43.1% rarely / often) | NA | NA |
METHODS
This report deals with the assessment of the compliance with hygiene and safety procedures, and their perception by professionals, within a network of dental practices in Rome, as found during 'expert' inspections undertaken by the Health Surveillance Authority (SISP-ASL). As part of this investigation, 100 questionnaires, containing 37 multiple-choice questions, were used and completed by dentists belonging to 76 different dental practices.
RESULTS
The sample was mainly composed of males (78% of subjects), professionals aged 50 years or above (59%); 50% of the doctors participating in the study had a degree in dentistry (many also had a further specific qualification), 30% had a degree in medicine and surgery, and/ or a second degree in dentistry and/or a special qualification in dentistry, 17% had a degree in medicine and surgery together with other specific courses in dentistry, and, finally, 3% did not provide an answer.
Having a degree or having "work experience" (defined as less than and over 20 years of professional activity) do not appear to influence the perception of the risk of infection due to HBV and HIV: the percentages of those who answered stating that the risk was "high only for surgery manoeuvres" resulted 27% and 41% for the two pathogens, respectively. Preliminary analyses of the answers of the questionnaires highlighted a trend: the higher the work experience was, the lower the percentage of those who underwent vaccination or performed periodical check-ups for HBV infection was recorded. Furthermore, it appears that knowledge is insufficient among professionals (28-32%) regarding recent regulations aimed at preventing injuries from needles and sharp objects (Law Decree 19.2.2014 n.189 which modifies Law Decree 81/2008): 62% of the sample stated to always put the cap back on the needles and 2% re-caps them occasionally.
With respect to the knowledge about the prevention of blood-borne viral infections, 46% of the study sample believed that previous information on the HIV-seropositive status of the patient was always indispensable, while 18% declared the same only when the assistance was given to high-risk subjects (i.e., intravenous drug users, chronic patients and carriers). Behaviours regarding prevention and safety in this field could be improved also with respect to the proper use of goggles, worn only in 60% of the dental treatments.
With respect to professional training and education, more than 95% of the dentists stated that the source of knowledge was represented by academic or scientific sources or by scientific congresses and meetings.
Analytical control of the water system was carried out only in nearly half of the dental practices surveyed, even if 90% of the interviewed stated they used some filtration system at the workplace. Tweaks and works were undertaken mainly with resins and aspiration in 54% of the treatments; a microbiological assessment of the work-environment contamination inside the studio was performed in 32% of the dental practices. The formal assignment and the real activity of an Occupational physician resulted to occur in 67% of the dental studios.
By applying Regional check-lists regarding the adequacy of the furnishings and work environments, it was found that the environments (cure / acceptance / waiting room) were perfectly separated in 65% of the practices, while proximity between administrative and medical spaces was found in 35%. The presence of expired pharmaceuticals resulted in 15% of the practices and the regular stocking of waste materials was performed in 60% of the cases. A surface with windows or the aeration unit with adequate air replacement was identified in 65% of the cases, whilst automated washbasins were not present in 80% of the studios. Class B autoclave was missing in 2% of the studios, and instrumental non-compliance of the studios and an insufficient quality of clinical records and the risk assessment document were identified in 2% of the dental practices, with more than 25% of these shortcomings regarding emergency and maintenance procedures.
Various cases highlighted the advantageous and adequate use of high-technologies such as thermal destruction of needles used or the reclaiming of water through disinfection; flushing procedures were adopted in many cases. A lack in the proper management of physical risk factors (i.e., artificial optical radiation, hand arm vibrations, work-related musculoskeletal disorders - WMSDs for use of cutters and drills) was generally observed.
CONCLUSIONS
The results of the investigations suggest that further efforts are required in dental practices regarding both the assessment and the management of some occupational risks (i.e., biological exposure to blood-borne and airborne infectious agents, environmental issues and technical procedures) and the compliance of professionals with the existing recommendations and laws aimed at preventing exposure to different hazards. Although the standards of the working environment appeared generally acceptable in this work-place, another critical issue is represented by the fact that not all the needed safety procedures are always available, formalized and routinely updated and verified in the risk assessment document of the company.
Study 4: Risk assessment of Health-care Associated Infections among Health-Care Workers in a Local Health Authority in Sardinia Region, Italy
INTRODUCTION
Health care workers (HCWs) are more prone than other workers to biohazard related to potentially infectious biological agents. Transmission in the health-care settings can occur through several ways, mainly blood-borne and airborne/droplets, and it can affect both HCWs and patients [24].
In the last twenty years, scientific organizations and authors set several alerts on the need to proper risk assessment and management of biohazard in the health-care sector [25, 26]. In spite of these alerts, some critical issues still remain unsolved in hospitals and other health services.
Objective of the study was to assess the risk of Healthcare Associated Infections (HAIs) in HCWs of a Sardinian Local Health Authority, in order to identify proper and tailored preventive interventions to control this existing risk.
METHODS
A risk assessment campaign was conducted from May to October 2014 according to the recommendations of the Italian Society of Occupational Health and Industrial Hygiene (SIMLII) [27].
We considered as HCWs all employees working in healthcare settings with potential exposure to patients and/or to infectious materials, including physicians, nurses, nursing assistants, therapists, technicians, emergency medical personnel, pharmacists, laboratory personnel. The blood-borne risk assessment entails data collection on: (1) identification of the infectious agents at the workplace; (2) identification of the source and description of the pattern of transmission; (3) surveillance of the infections among HCWs; (4) surveillance of the accidental exposures; (5) characteristics of the work environment, medical devices, personal protective equipment, organization of the preventive system.
The identification of the infectious agents has been made through consultation of scientific evidences, national and local epidemiological data. We collected transmission modalities through the analysis of exposure procedures performed in each unit (stratified by job task). Data on immunization coverage among HCWs, presence of infectious diseases and injuries were collected from the database of the Occupational Physician, whereas data on protective equipment and disposals were collected during inspections in the units. Exposure procedures and injuries were collected following the recommendations provided by the CDC of Atlanta and the Society for Healthcare Epidemiology of America [27, 28].
Risk assessment for tuberculosis (TB) was limited only to three hospitals, due to the absence of data from the country health services. Number of beds in the structure and notifications of TB cases in the period 2010-2014 were considered, following the algorithm of the guidelines proposed by the CDC [29]. The TB infection risk was then stratified per year and unit following the indications from the Italian Ministry of Health.
Data on seasonal influenza vaccination coverage and characteristics of risk communication adopted by health management were collected.
Seroprevalence ratios of antibodies against measles, mumps, rubella and varicella among HCWs were estimated from the medical records of the health surveillance service. Data on outbreaks in the community and in hospitals in the last three years were collected from the Local Public Health Unit.
The presence of procedures for scabies, Neisseria meningitidis and Ebola and their adherence to international scientific recommendations were also assessed.
RESULTS
Overall, 2,661 HCWs were enrolled in the study. Bloodborne biological agents considered were HBV, HCV, HIV and Ebola. Exposure prone procedures were more frequently performed by medical doctors in surgery, emergency and intensive care units, whereas procedure considered at lower risk were more frequently performed by nursing staff in all clinical units. The seroprevalence of blood-borne pathogens among HCWs was < 1% for HBV, < 2% for HCV, and > 0.1% for HIV. Among blood-borne-positive HCWs, there were not specific clusters by job task and unit. Seroprotection for HBV was lower than 70%. Blood-borne injuries represented the most common cases (2011-2013: 130/283; 45%). The majority of them were percutaneous (n = 116; 89%) and occurred during intravenous injections and recapping or disposing of needles (41%), while 7% during exposure prone procedures. Nurses were more exposed to risk of blood-borne injuries, especially in emergency and intensive care units. Personal protective equipments were widespread in all units, whereas medical and surgical disposal with protective devices were not. In some units these disposals were present but not fit to medical and surgical procedures performed. The system of reporting and follow up of injuries proved to be effective, but not all HCWs were aware of all aspects of the post exposure procedures (in particular with respect to the correct timing of reporting). Procedures for the management of Ebola cases were available and coherent with the guidelines of the Italian Ministry of Health. No patients with diagnosed or suspected Ebola were ever hospitalized in the authority.
The risk of TB resulted high in one of the three hospitals with a mean of 3.2 TB cases (range 2-4 in 2010- 10/2014) per year. Specific preventive procedures and collective protective devices to reduce TB risk were not systematically applied. Emergency and radio-diagnostic units resulted to be at highest risk due to the frequency of contacts with patients with active TB and the lack of adherence to preventive measures compared with other units. In that hospital, in the last two years, three HCWs resulted positive at the in vitro test after a contact with a TB patient: protective procedures were not completely applied in all patients with TB.
The influenza vaccination campaign was conducted by communication to units and nurses managers and resulted in vaccination coverage rate less than 10% in the 2013-2014 season.
Overall about the 50% of total HCWs was tested for exanthematic diseases. The sero-prevalence ratios were lower than 95% for measles (1105/1163) and varicella (1100/1159), 84% for mumps (996/1179) and 90% for rubella (1115/1241), resulting in more than 400 susceptible HCWs for at least one of the four viruses. About 100 seronegative HCWs were employed in units with higher risk of transmission (i.e. pediatric and emergency units) and in those with higher risk for patients (oncological, cardiological and nephrology and dialysis units). In 2014, an outbreak of measles occurred in one hospital with four HCWs infected. Procedures for Neisseria meningitidis and scabies were not available.
CONCLUSIONS
Risk assessment of biohazard in HCWs represents one of the main issues for occupational health professionals in the healthcare sector. The SIMLII recommendations did not allow to establish an overall risk levels for all biological agents considered, however it was useful to identify specific areas of preventive intervention in order to control the risk. In particular, results highlight the need of intervention for training nurses and nursing aides in specific units, focused on both high and low risk procedures, the possible under-reporting of biological injuries of medical HCWs during high-risk procedures, lack of diffusion of medical and surgical disposal with protective devices, inadequate HBV, influenza, and exanthematic disease seroprotection rates, lack of adherence with protective procedures in case of TB exposure, lack of data on TB exposure in country services, and procedures to contain the risk of scabies and Neisseria meningitidis transmission. Further efforts have to be done in order to properly manage biohazard in the health-care settings, in order to optimize protection of both HCWs and patients' safety and health.
Conclusions and future perspectives
This article is the summary deriving from the application of different research approaches, conducted in different professional settings across Italy, aimed at improving the knowledge of the specific risks in the workplace, as a necessary step towards their proper management, according to guidelines and standardized procedures. The knowledge obtained can be useful to orientate proper preventive programs aimed at improving workplace health. Implementation of evidence-based sanitary surveillance programs is mandatory for the promotion and protection of workers in this setting.
Footnotes
Funding: Only the study by Garbarino et al. was partially funded by Iveco-CNH Industrial, Torino, Italy.
Contributor Information
Collaborators:
Maria Gabriella Mavilia, Marta Cartosio, Alessandra Toletone, Dimitri Sossai, Ottavia Guglielmi, Francesca Bersi, Guglielmo Dini, Giuliana Gelsomino, Serena Secchini, Gabriele Di Reto, Vito Cerabona, Arianna Di Nezza, Paola Abetti, Felice Giordano, Nicola Mascia, Natalia Angius, Daniele Fabbri, Luigi Isaia Lecca, and Patrizia Virgona
References
- 1.Vincent JH. Occupational hygiene science and its application in occupational health policy, at home and abroad. Occup Med (Lond) 1999;49:27–35. doi: 10.1093/occmed/49.1.27. [DOI] [PubMed] [Google Scholar]
- 2. European Agency for Safety and Health at Work , author. Factsheet 22: Work-related stress. Safety and Health at Work - EUOSHA; 2002. [Google Scholar]
- 3.Wiskow C. Guidelines on workplace violence in the health sector – Comparison of major known national guidelines and strategies: United Kingdom, Australia, Sweden, USA. Geneva: ILO/ ICN/WHO/PSI; Joint Programme on Workplace Violence in the Health Sector, forthcomingworking paper. [Google Scholar]
- 4.Natali E, Martini A, Ronchetti M, et al. Book of Proceedings of the IX Conference of the European Academy of Occupational Health Psychology (EAOHP) Rome. Italy: 2010. Mar 29, HSE Management Standards and work-related stress: Italia translation and validation of the Indicator Tool. 31. [Google Scholar]
- 5.Zoni S, Lucchini R, Alessio L. Integration of subjective and objective methods for stress related risks evaluation in the health care sector. G Ital Med Lav Erg. 2010;32:332–336. 3, [PubMed] [Google Scholar]
- 6. Commissione consultiva permanente per la salute e la sicurezza nei luoghi di lavoro. Lettera circolare in ordine alla approvazione delle indicazioni necessarie alla valutazione del rischio da stress lavoro-correlato di cui all'articolo 28, comma 1-bis, del decreto legislativo 9 aprile 2008, n.81, Lettera circolare del Ministero del lavoro e delle politiche sociali, 2010. [Google Scholar]
- 7. Coordinamento dei Servizi di Prevenzione e Protezione e dei Medici Competenti della Regione Emilia Romagna, Coordinamento dei Servizi di Prevenzione e Protezione e Coordinamento dei Medici Competenti della Regione Liguria. Linea di indirizzo regionale per la valutazione del rischio da stress lavorocorrelato nelle aziende sanitarie. Documento di lavoro, 2009. [Google Scholar]
- 8.Gillespie GL, Gates DM, Miller M, et al. Workplace violence in healthcare settings: risk factors and protective strategies. Rehabil Nurs. 2010;35:177–184. doi: 10.1002/j.2048-7940.2010.tb00045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jordan AS, McSharry DG, Malhotra A. Adult obstructive sleep apnoea. Lancet. 2014;383:736–747. doi: 10.1016/S0140-6736(13)60734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smolensky MH, Milia L, Ohayon MM, et al. Sleep disorders, medical conditions, and road accident risk. Accid Anal Prev. 2011;43:533–548. doi: 10.1016/j.aap.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Garbarino S, Nobili L, Carli F, et al. The contributing role of sleepiness in highway vehicle accidents. Sleep. 2001;24:203–206. [PubMed] [Google Scholar]
- 12.Garbarino S. Sleep disorders and road accidents in truck drivers. G Ital Med Lav Ergon. 2008;30:291–296. [PubMed] [Google Scholar]
- 13.Carter N, Ulfberg J, Nyström B, et al. Sleep debt, sleepiness and accidents among males in the general population and male professional drivers. Accid Anal Prev. 2003;35:613–617. doi: 10.1016/s0001-4575(02)00033-7. [DOI] [PubMed] [Google Scholar]
- 14.Garbarino S, Magnavita N. Obstructive sleep apnea syndrome (OSAS), metabolic syndrome and mental health in small enterprise workers. Feasibility of an action for health. PLoS One. 2014;9:e97188–e97188. doi: 10.1371/journal.pone.0097188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leggat Pa, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: a review. Ind Health. 2007;45:611–611. doi: 10.2486/indhealth.45.611. [DOI] [PubMed] [Google Scholar]
- 16.Ayers KMS, Thomson WM, Newton JT, et al. Self-reported occupational health of general dental practitioners. Occup Med (Lond) 2009;59:142–148. doi: 10.1093/occmed/kqp004. [DOI] [PubMed] [Google Scholar]
- 17.Veronesi L, Bonanini M, Dell'Aglio P, et al. Health hazard evaluation in private dental practices: a survey in a province of northern Italy. Acta Biom. 2004;75:50–55. [PubMed] [Google Scholar]
- 18.Germinario C, Fanelli M, Chironna M, et al. Occupational risk for HIV and HBV: KAP survey in a sample of dentists. Ann Ig. 2001;13:281–290. [PubMed] [Google Scholar]
- 19.Cristina ML, Spagnolo AM, Sartini M, et al. Investigation of organizational and hygiene features in dentistry: a pilot study. J Prev Med Hyg. 2009;50:175–180. [PubMed] [Google Scholar]
- 20.Vitale F, Benedetto MA, Casuccio A, et al. The influence of professional degree on the knowledge of HIV, HBV and HCV infections in dentistry practice. Ann Ig. 2005;17:185–196. [PubMed] [Google Scholar]
- 21.Galli MG, Tesauro M, Consonni M. Hygiene-sanitary risks associated with dentistry in the city of Milan. Questionnairebased survey. Minerva Stomatol. 2000;49:267–280. [PubMed] [Google Scholar]
- 22.Fabiani L, Mosca G, Giuliani AR. Hygiene in dental practices. Eur J Paediatr Dent. 2006;7:93–97. [PubMed] [Google Scholar]
- 23. CDC , author. Guidelines for Infection Control in Dental Health-Care Settings. MMWR. 2003 Dec 19; [Google Scholar]
- 24.Haagsma JA, Tariq L, Heederik DJ, et al. Infectious disease risks associated with occupational exposure: a systematic review of the literature. Occup Environ Med. 2012;69:140–146. doi: 10.1136/oemed-2011-100068. [DOI] [PubMed] [Google Scholar]
- 25.Beltrami EM, Williams IT, Shapiro CN, et al. Risk and management of blood-borne infections in health care workers. Clin Microbiol Rev. 2000;13:385–407. doi: 10.1128/cmr.13.3.385-407.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Polato R, Bacis M, Belotti L, et al. Focus on risk assessment in health environments: results and perspectives of a multicenter working group. G Ital Med Lav Ergon. 2010;32:240–244. [PubMed] [Google Scholar]
- 27. Centers for Disease Control and Prevention , author. Immunization of healthcare workers: recommendation of the Advisory Committee on Immunization Practices (ACIP) and the Hospital Infection Control Practices Advisory Committee (HICPAC) MMWR Recomm Rep. 1997;46:1–42. [PubMed] [Google Scholar]
- 28.Henderson DK, Dembry L, Fishman NO, et al. SHEA Guideline for Management of Healthcare Workers Who Are Infected with Hepatitis B Virus, Hepatitis C Virus, and/or Human Immunodeficiency Virus. Infect Control Hosp Epidemiol. 2010;31:203–232. doi: 10.1086/650298. [DOI] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention , author. Guidelines for preventing the transmission of Mycobacterium tuberculosis in healthcare settings, 2005. MMWR Recomm Rep. 2005;54:RR-17–RR-17. [PubMed] [Google Scholar]