Summary
Annual influenza vaccination is recommended for persons with human immunodeficiency virus (HIV) infection. Recent reports indicate that immunizations may increase HIV replication in infected individuals. Generally, vaccination against influenza is well tolerated in both children and adult individuals with HIV and does not induce significant changes in viral load and CD4+ cell counts. The observed increase in viral replication is usually transient and a clear, measurable progression of the underlying HIV disease is hard to be determined. Several studies reported immunogenicity data in HIV+ population, by comparing different influenza vaccines, adjuvanted or not, and different administration routes. Data are encouraging because an adequate immune response is shown, although split/subunit vaccines do not elicite an efficient immune response in these subjects. New strategies have been evaluated to increase the immune response in immunocompromised patients.The aim of this review is to evaluate tolerability, safety, immunogenicity and efficacy of vaccines actually approved for human use and to consider latest evidence and future perspective in HIV positive subjects.
Key words: Influenza vaccination, HIV-1 RNA levels, CD4+ count
Introduction
INFLUENZA IN HIV POSITIVE PATIENTS
Influenza illness is a worldwide, public health problem of major concern. It is a highly contagious, ubiquitous disease that can lead to severe complications, especially in the elderly, debilitated or chronically ill patients, children and in immunosuppressed subjects, including those infected with the human immunodeficiency virus (HIV) and transplant recipients [1, 2]. It is difficult to estimate hospitalizations and deaths due to influenza and its complications because infections are not often confirmed virologically or specified on hospital discharge forms or death certificates [3]. For influenza disease a significant burden lies on all individuals, but hospitalization and treatment occur more frequently in high-risk patients. In addition to the clinical burden, influenza also poses a considerable economic burden. There are extensive economic analyses of the influenza burden in the literature. One study estimated a total economic burden of seasonal influenza in the United States (using 2003 population and dollars) to be $87.1 billion, including $10.4 billion in direct medical costs [4]. In addition to the direct costs of medical care, the indirect costs of influenza are substantial due to the increase morbidity. The burden of influenza varies with the age and underlying health of the patient. Estimates of the cost of influenza in the USA, France and Germany have shown that indirect costs can be five– to 10–fold higher than direct costs [5]. In particular, influenza remains a common cause of respiratory illness in adults with HIV, despite the use of novel high retroviral therapies and increase of flu vaccine coverage rate, that lead the mortality rate from 2.2 million (in 2005) to 1.8 million (in 2010) [6, 7]. The studies conducted by Neuzil et al. and Lin et al. confirmed high numbers of hospital admissions and high mortality from influenza in patients with HIV/AIDS not on Highly Active Anti Retroviral Therapy (HAART) [8, 9]. Neuzil et al., in another study reported that cardiopulmonary hospitalisations in influenza infection of patients with Acquired Immunodeficiency Syndrome (AIDS)/HIVwere very high in the pre-HAART era, with a rate of 48 per 1000 persons; in the post-HAART era hospitalisation rates decreased by 53% but remained more higher than that of the U.S. population and similar to that of the population at risk [10].
Immunization against influenza can effectively reduce the annual clinical and economic burden of influenza. Nevertheless, despite efforts to vaccinate those at highest risk of severe influenza-related complications, many still go unvaccinated [11, 12]. A study in eleven European countries showed that the highest immunization coverage for the population considered at high risk, was reached in the Netherlands (about 80% of vaccinated subjects), while the lowest rate belongs to Greece with only 25%. This data may be explained by several considerations: first, factors such as education can guide people towards a particular choice in favor of vaccination or not; second, in some countries the reimbursement for the cost of vaccination is partial; third, a smaller number of doses distributed could obviously result in a smaller number of subjects vaccinated [12]. The Advisory Committee on Immunization Practices considers HIV-infected persons to be at increased risk for influenza and recommends annual vaccination [13]. In view of mortality , morbidity and complication risk, already in 1986 there was a recommendation for influenza vaccination of patients with human T- lymphotrophic virus type III AIDS-related, and since 1988 the CDC recommended vaccination in children with acquired immunodeficiency syndrome. Current guidelines recommend that individuals infected by HIV receive yearly influenza vaccination. Since most previous studies on influenza vaccines in HIV infected individuals focused on their immunogenicity rather than on their clinical effectiveness, it is crucial to set up close post vaccination influenza monitoring to check the persistence of immune response and effective immune protection against viral strains circulating during seasonal epidemics [14-16].
The Strategic Advisory Group of Experts (SAGE) on immunization reviewed evidence on influenza disease burden, vaccine performance (efficacy and safety), and the feasibility and cost-effectiveness of implementing vaccination programmes for population groups at higher risk. In 2012, WHO published updated recommendations for seasonal influenza vaccination based on a systematic literature review performed by SAGE [17-21].
SAGE confirmed the recommendations to consider as priority groups for influenza vaccination individuals > 6 months with chronic heart or lung diseases, metabolic or renal disease, chronic liver disease, chronic neurological conditions and immunodeficiencies.
Prospective studies have looked at the long-term effect of influenza vaccination, confirming the safety and tolerability of currently used influenza vaccines, but questions remain about the immunogenicity and effectiveness of these vaccines in HIV infected patients. New roads could be opened through the use of new vaccines, such as MF59® adjuvant and those administered intradermally, that could overcome problems such as poor immune response and suboptimal effectiveness [22, 23]. The aim of this review is to evaluate tolerability, safety, immunogenicity and efficacy of vaccines actually approved for human use and to consider latest evidence and future perspective in HIV- positive subjects.
TOLERABILITY AND SAFETY
Several studies were performed to evaluate tolerability and safety of influenza vaccination in HIV positive patients showing a good tolerability profile. In different studies reported symptoms resolved without sequelae in few days. There is lack of data regarding adverse events at long-term [23, 24].
Main evidence emerged by safety and tolerability evaluation of available vaccines in the last decade; serious adverse events, systemic and local reactions are reported below.
Serious adverse events
Serious adverse reactions were defined as any untoward medical event that at any dose result in death or is lifethreatening, requires hospitalisation, results in disability or congenital anomaly [25]. From global analysis of more than 20 studies that evaluated safety and tolerability profile, no serious adverse events (SAEs) are tight associated with influenza vaccination in HIV- infected patients. Reported adverse events during follow-up of the studies were not associated with influenza vaccination but usually related to syndromes or treatment associated with HIV.
Trivalent Influenza Vaccines (TIV) were the first and the most used vaccine for immunization of HIV positive subjects. As emerged from literature data of the last two decade, TIV showed a good safety profile and no SAEs were reported [26, 27]. Durando et al., compare two influenza virus subunit vaccines with or without MF59® adjuvant showing absence of serious adverse event, except for a case of transitory ischemic attack in a men, episode that was demonstrated to be not correlate to vaccination [28]. Cooper et al., in his study, using a trivalent killed split not adjuvanted influenza vaccine in HIV infected adults, showed that vaccination is well tolerated without increase reactogenicity as consequence of higher antigen dose or boosting dose. In his study the population is divided into three groups, the first of which received one dose of influenza vaccine (0.5 mL or 15 μg hemagglutinin [HA]) in October and November 2008 followed by a booster dose 28 days later, while the second gets a double dose (30 μg HA) at the same time interval, followed by a double dose of booster 28 days later and finally, the third group received a single dose of vaccine [29].
Several studies conducted in HIV infected individuals immunized with A(H1N1) 2009 pandemic inactivated, unadjuvanted vaccine showed that vaccines were safe and well tolerated in this population and no SAEs were reported. Crum-Cianflone et al. evaluated a monovalent non adjuvanted 2009 influenza A/H1N1 vaccine comparing SAE in HIV positive and uninfected subjects showing that only 1 partecipant (HIV- uninfected patients) developed a serious adverse event that consist in angioedema on day 1 post vaccination and resolved after 17 days with antihistamine therapy [30]. It also occurred eight hospitalization but no one related to vaccination (seven in HIV-positive patients and one in healthy subjects) [31-41]. It has been demonstrated in studies involving a total of 892 children and 111 adults that administration of live attenuated influenza vaccine (LAIV) vaccine is safe and well tolerated and not serious adverse events related to vaccination were recorded. Furthermore, the safety profile is very similar to that previously reported in studies including other populations. Current influenza vaccination guidelines do not recommend LAIV immunization in persons with known or suspected immunodeficiency diseases, but the cited studies demonstrated that this vaccine should be evaluated for a role in immunizing HIV infected people [42-47].
Data from existing studies showed that virosomal influenza vaccination is well tolerated and no complaints of severe adverse reactions are usually reported in both children and adult HIV positive individuals [26].
Gabutti et al., and Durando et al., in their study do not show adverse serious events associated with the vaccination during the follow up period in HIV populations vaccinated both with MF59® influenza vaccine and with subunit vaccine containing 15 μg of HA per strain and administered intramuscularly [26, 28].
In the study by Launay et al., three adverse reactions are reported after 42 days post vaccination, with monovalent 2009 Influenza A/H1N1v vaccine adjuvanted with AS03®, consisting of hospitalization following the second dose of adjuvanted vaccine, one recurrent episode of depression and one increase in serum alanine transaminase value associated with other treatment [48]. Palma et al., evaluating safety and immunogenicity of monovalent adjuvanted A/H1N1 pandemic influenza vaccination reported no deaths or serious adverse event during the follow-up [49]. No correlation between SAE and influenza vaccination was observed. Many studies report that the pandemic vaccine with or without adjuvant is safe and well tolerated [32-35, 38, 39, 48, 50-52].
Gelinck et al. also reported no adverse events in the study which compares the influenza vaccine containing 0.1 ml of the 2005/2006 trivalent influenza vaccine administered intradermally and 0.5 ml administered intramuscularly in immunocompromised patients. The frequency of events is more higher in subjects who received the vaccine intramuscularly [22]. The same observation were reported by Ansaldi et al., in a study in which intradermal vaccination low-antigen – 9 μg HA per strain- and vaccine intramuscular containing a standard dose of antigen -15 μg- were administered to HIV positive patients and compared. The study, although the low population size, shows good safety for both vaccines and no SAE [53].
Systemic reactions
Systemic reactions occur after a few hours of vaccination and may last for 24-36 hours. They may be linked to various causes such as the action of endotoxins, replication "in vivo" of microorganisms , the toxicity of the adjuvant and the reactivity of the immune system. They are usually mild, but in some cases can be so severe as to require supportive therapy.
Durando et al., comparing two subunit influenza vaccines with or without MF59® adjuvant, in patients with immunodeficiency acquired, reports such as systemic event most widespread headaches and fever in both groups with percentages of 25.9% and 28.4% [28].
In different studies, adverse systemic effect in patient vaccinated with virosomal influenza vaccine are comparable to subunit influenza vaccine group. In particular Evison et al., reported in a population of immunosuppressed adults vaccinated with a subunit or a virosomal influenza vaccine that the fatigue was the most frequently reaction, followed by headache and malaise in both vaccine group [54].
Systemic reactions typically occur after a few days post vaccination and are more frequent in subjects receiving an adjuvanted vaccine. They are mild or moderate and of short duration.
Indeed, Gabutti et al., comparing two influenza vaccine containing 15 μg of superficial haemagglutinin antigen for strain, MF59®-adjuvanted influenza vaccine (group A) versus a conventional subunit vaccine (group B), reports fever in 5% of patients of group A and 10% of subjects of groups B [26].
Palma et al., reports in his study as most frequent systemic reactions headache, fatigue and chills. 8% of subjects reports fever , 11% fatigue after the first dose. Fever is not reported after the second dose, while fatigue reported by 6% of subjects [49].
Gelinck et al., comparing 156 immunocompromised patients and 41 healthy controls that were randomized to receive either 0.5mL of the 2005/2006 trivalent influenza vaccine intramuscular or 0.1mL intradermal, estimated the frequency of adverse reactions after intramuscular vaccination with symptoms going from muscle pain to fever with values ranging from 11-48% [22].
Local reactions
Local reactions are defined as reactions that occur at the site of inoculation of the vaccine and determine redness, pain, erythema, pruritus. In general the local reactions are more frequent in subjects vaccinated with adjuvanted or intradermally administered influenza vaccines.
LAIV were well tolerated and have a similar safety profile compared with TIV; nasopharyngeal symptoms were minor and of short duration.
Durando et al., comparing two subunit vaccines with or without MF59® adjuvant, in patients with immunodeficiency acquired, reports such as local event most widespread pain an induration, respectively 54.3% and 22% [28].
Among the adverse local effect in patient vaccinated with virosomal influenza vaccine, the pain is the most frequent local reaction, followed by swelling and redness. Reported adverse events were comparable with those recorded in the groups immunized with conventional vaccines.
Some studies that use an adjuvanted vaccine (MF59®) and where the population was immunodepressed (HIV positive or those with chronic illnesses) reported local reactions of mild or moderate entity [24, 41, 42]. In the study by Launay et al., use of adjuvanted vaccine with aluminum salts determine a higher rate of reactions (71%) in HIV positive subjects compared to the control group (21%) [48]. Gabutti et al., comparing the safety and immunogenicity of a subunit vaccine versus MF59®-adjuvantated vaccine in HIV-positive patients, reported pain and redness in 28% of patients vaccinated with adjuvantated vaccine and 10% of subjects vaccinated with the subunit vaccine [26].
The most frequent local effect were pain -18%-, swelling and redness -2%- at injection site. Were classified as mild and resolved in few days post vaccination, as reported by Palma et al. [49].
Ansaldi et al. in his study reported pruritus in 29% ID vs 4% IM, redness 46% vs 8%, swelling 43% vs 12%. All local events were mild or moderate and resolved without sequelae [53].
The same conclusions are reached by Gelinck et al. in their study in which they evaluated the administration of a trivalent vaccine by intradermal route (0.1 ml) or by intramuscular (0.5 ml), they reported erythema and pain at the injection site 48 hours after vaccination showing these reactions more frequently in subjects vaccinated intradermally and in the control group compared to immunocompromised patients. In general, all subjects in the control group and 69% of immunocompromised individuals who responded to all three antigens showed a local skin reaction [22].
HIV-RNA AND CD4+ CELL COUNT POST-VACCINATION
Several studies published between 1995 and 2012 reported controversial data both in favour and against the evidence of increase of viral load and a decrease of CD4+ cell count secondary to the administration of influenza vaccination in HIV infected persons with or without correlation to the immune response. Differences in used vaccines, in sample sizes and features of HIV infected populations (i.e. demographic characteristics, risk factors, stage of HIV disease, patients under anti-retroviral treatment or naıve) enrolled in the various studies as well as timing of sampling assays and different sensitivity of laboratory methods for quantification of viral load, could explain at least part of these conflicting reports [32, 41, 43].
Many authors reported an increase in viral load following influenza immunization, this data appears to be related to detectable viral load at baseline and no treatment of HAART therapy, although it is not always observed [24, 27, 55-59, 61-63]. The rebound of viral load is attributed to activation of quiescent HIV infected CD4+ cells and the up regulation of HIV viral replication [52, 58-62].
Günthard et al. and Staprans et al. showed that effects of trivalent influenza vaccine on viral replication in HIV positive adults determined transient increase of plasma HIV-RNA levels [58, 64]. Therefore, the simultaneous decrease in pro-viral DNA and memory phenotype CD4+ cells in association with increased plasma HIV RNA after vaccination in patients with < 400 RNA copies/ ml at baseline suggested that in vivo mobilization of the latently infected cell reservoir may occur during potent antiretroviral therapy [58]. The same conclusion has been reported by Fuller et al. and Madhi et al. [56, 65].
Study conducted in HIV infected children reported controversial data about increase of viral load after immunization with trivalent influenza vaccine.
Kosalaraska et al. showed an increase in HIV-RNA levels in children aged ≥ 6 months to < 18 years: authors stated that increase in plasma HIV-RNA was a transient phenomenon and did not have any clinical significance [66]. Machado et al. showed no increase neither in viral load nor in CD4+ cell count in a population of children with a mean age of 12 years [67].
In the study by Tasker et al. CD4+ cell count and viral load are evaluated in HIV positive subjects vaccinated with LAIV influenza vaccine. They showed an increased HIV replication and a decrease in CD4%: according to the authors, this effect is probably due to the absence of treatment with antiretroviral therapy [63].
Levin et al., showed, instead, no significant increase from baseline in plasma HIV viral load and no change in CD4% in HIV infected children aged ≥ 5 months to < 18 years old [44]. Studies in HIV-positive adults immunized with a monovalent unadjuvanted influenza vaccine (H1N1) administered with a single dose, reported no significant change in plasma HIV RNA levels or CD4+ cell count [30, 32].
Tanzi et al. evaluating effects of a virosomal influenza vaccine on viral replication and T-cell activation in HIV–infected children, receiving HAART, observed no increase in plasma HIV-1 RNA or HIV-1 pro-viral DNA and the immunophenotype analyses demonstrated that CD4+ cell counts and percentages and activated lymphocytes remain stable for about a month after immunization [68].Same results have been obtained by Zuccotti et al., Zanetti et al. and Esposito et al. [24, 69, 70]. In the study by Amendola et al., the mean viral RNA levels did not change in HIV infected and uninfected adults as well as no difference have been showed in HIV proviral DNA levels [25].
However, more recent and better designed studies have not documented a substantial increase in the replication of HIV, immune stimulation resulting from influenza vaccination did not significantly change the levels of plasma virus, CD4+ cell counts, or activation-induced apoptosis in HIV-infected individuals. An increase in the T-cell response to influenza and spontaneous apoptosis, and increase in plasma HIV-1 RNA level following influenza vaccination are rare and transient phenomenon [43-45, 52, 56, 60, 61].
Different studies evaluated the effects of adjuvanted seasonal and pandemic influenza vaccine on HIV viral load and CD4+ cell count in HIV positive subjects. Vaccines used in this studies were adjuvanted with oil-in-water emulsion, in particular with MF59® and AS03®, the only adjuvants approved for human use. Gabutti et al. by comparing groups mean lymphocyte count for time points after immunisation didn't reveal any statically significant changes in HIV positive adults immunized with MF59 adjuvant or conventional influenza vaccine, with the exception of subjects with lymphocyte counts < 200 cells/mm3, vaccinated with conventional subunit vaccine, whose counts showed a progressive increase after immunization [26]. Durando et al. in HIV positive adults showed a decrease of HIV RNA and an increase of CD4 cells in subjects immunized with adjuvant vaccine compared to patients immunized with conventional not adjuvanted influenza vaccine [28]. Iorio et al. reported, no substantial change in viral load and transitory increase of HIV replication in subjects immunized with a conventional vaccine although the study population were immunized with the same formulation of the above-mentioned study [71]. Palma et al., in HIV positive children and adults immunized with a monovalent pandemic adjuvanted influenza vaccine, showed no altered CD4 count and HIV viral load levels [49]. As regard as influenza vaccines adjuvanted with AS03®, Calmy et al., Tremblay et al. and Launay et al. observed a transient increase of HIV-1 RNA replication within days of the vaccination, but neither increased risk of disease progression nor long-term effects on CD4+ cell counts, viral load, or progression to AIDS or death have been reported [48, 51, 52].
Lack of data exists in the literature regarding the effect of influenza vaccination with intradermal delivered; therefore, further studies of this preparation are needed.
IMMUNOGENICITY
Typically, to evaluate the immunogenicity of influenza vaccines are considered the following parameters:
Geometric mean titres (GMTs), mean- fold increase in titres (MFI; ratio of post to pre- vaccination titre), seroprotection rate, defined as the percentage of subjects achieving a significant increase in titre from a non-negative pre-vaccination titre (≥ 1:10) or a rise from < 1:10 to ≥ 1:40 in those who were seronegative), and seroconversion rate defined as either a negative pre-vaccination titer (≤ 10) to a post-vaccination titer ≥ 40, or at least a fourfold increase between pre-and post-vaccination titers where the pre-vaccination titer is ≥ 10. The Committee for Medicinal Products for Human Use (CHMP; formerly CPMP) criteria for approval of influenza vaccine in adults younger than 60 years includes that at least one of the following criteria are met: seroprotection rate > 40%, MFI > 2.5 or seroconversion rate > 70% [72]. As recommended by the WHO the test used to assess the immunogenicity of influenza vaccine are the inhibition of hemagglutination (HI) and microneutralization (MN) assay [17].
The HI assay has been used as the primary means to measure serum antibody responses to influenza vaccines due to the ease of conducting the assay and a generally accepted correlation with seroprotection. However, the information imparted by a demonstration of neutralization capacity is different from that of HI, which measures disruption of binding to red cells without assessing prevention of infection. Although definitive human studies are lacking, animal models suggest that neutralization capacity predicts prevention of infection, while HI correlates with prevention of disease [45, 46]. In clinical trials of vaccines, MN assays may be more sensitive in detecting antibody and demonstrating seroconversion [54, 73] , including in immunocompromised subjects. HIV infection is associated with deficiencies in both humoral and cell-mediated immunity, which can alter the course of common infections and influence vaccine immunogenicity [74]. Generally in HIV-infected patients immunogenicity correlates directly with CD4+ cell count and inversely with HIV viral load [57, 58].
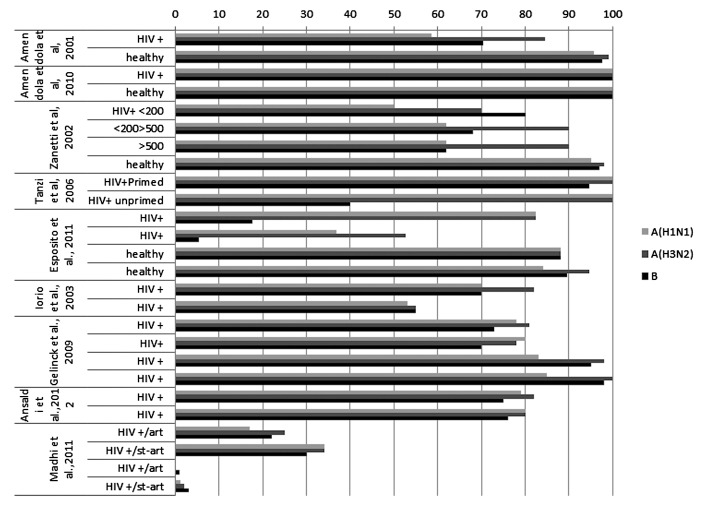
Most studies emphasized the importance of a high CD4+ cell count, treatment HAART therapy and use of adjuvant influenza vaccine to increase vaccine response rate; The immune response is closely correlated to the degree of immunosuppression [28, 35, 71, 75]. Hatayema et al., instead, in his study observed no correlation between plasma HIV RNA levels and HI antibody response [31]. Figure 1 shows the seroprotection rates of some studies reported in this review.
Fig. 1.
Seroprotection rate in studies involving HIV + population.
Conventional and LAIV influenza vaccines
As regard as non-adjuvanted A(H1N1)2009 pandemic vaccine, several studies evaluated antibody responses elicited by this vaccine in different populations of HIV infected individuals. Most of study participants followed an antiretroviral therapy with an high median CD4+ Tcells counts and fully suppressed HIV-RNA levels. Despite a good safety and tolerability profile, antibody responses elicited by conventional pandemic vaccine were insufficient to confer adequate protection in this immunosuppressed, hyporesponsive, at high risk subjects [30, 41].
The collected data regarding the administration of influenza unadjuvanted vaccine are controversial: Lagler et al. and Hatakeyama et al., reported in HIV positive adults a low immune response after two doses of pandemic influenza vaccine, while Bickel et al. and Cooper et al., demonstrate the effect of a booster dose of pandemic influenza vaccine in HIV-positive adults plays a fundamental role to increase the immunogenicity in immunodepressed population [31, 39, 41, 76]. Some authors evaluated the effect of a single dose of non-adjuvanted pandemic vaccine obtaining controversial results: some authors reported an adequate immunogenicity while others suggested that new strategies would be evaluated [30 32, 34, 36, 37, 40, 77]. As regards the evaluation of the immunogenicity of nonadjuvanted pandemic vaccine in children, Phongsamart et al., Flynn et al. and Hakim et al. reported an adequate immune response after two doses. Phongsamart et al., in his study showed a low level of cross reacting antibody to seasonal H1N1 [33, 35, 38].
Immunogenicity evaluations of LAIV in HIV infected population derived from a few studies.
In HIV infected children further evaluations of LAIV are needed, because conflicting data exist about antibody responses to vaccination. Two comparative studies showed that TIV elicited a seroconversion rate higher than LAIV, although the proportions of subjects with protective titers were similar between groups. In particular Weinberg A et al., demonstrated that TIV was more immunogenic than LAIV both against homotypic and heterosubtypic viruses, using microneutralization and haemagglutination inhibition assays. A study by King JC et al., showed a similar seroconversion rate after two doses of LAIV immunization both in HIV infected and uninfected children. In HIV infected adults only one study reported data about immunogenicity elicited by LAIV vaccine, but the low size of study population does not allow appropriate conclusions [42, 46].
A limited number of studies reported results of immunogenicity for virosomal influenza vaccination, in populations of adults and children. All studies reported that HIV positive subjects show lower immune responses to influenza vaccination in comparison with immunocompetent individuals. Seroconversion rates of HIV infected populations elicited by virosomal influenza vaccines do not differ significantly from that produced by trivalent conventional vaccines.
Tanzi et al., showed that use of the virosomal influenza vaccine is moderately immunogenic in HIV infected children. Because there are no EMEA defined criteria for children, immunogenicity was evaluated using criteria for adult. Humoral immune response were adequate for all three influenza strains in primed children and adequate for the two A strains in groups of the unprimed [68].
Oil-in-water emulsion adjuvanted influenza vaccines
Immunogenicity of MF59 adjuvanted influenza vaccine has been evaluated in different HIV positive populations. The different studies were designed and carried out in different manners: in literature there are comparative and not comparative, prospective trials, and populations involved varied from infected/uninfected children to infected/uninfected young adults and adults. Several studies showed that MF59 adjuvanted influenza vaccine had good safety and immunogenicity profiles similar or better than conventional influenza vaccine. All studies underlined that CD4+ cell count and HAART treatment play a key role in determining antibody response in influenza vaccination. Three studies reported a comparison between MF59 adjuvanted and conventional non adjuvanted seasonal influenza vaccine in HIV positive adults.
In the study by Durando et al. an assessment of humoral and cell-mediated immune responses elicited by the two influenza vaccines was made. Immunocompromised individuals vaccinated with MF59 adjuvanted vaccine showed a better antibody response and also a statistically significant increase in the frequency of proliferating T cells at 30 days after immunization, compared with patients vaccinated with non adjuvanted vaccine. HIVnegative subjects mounted a stronger antibody response than HIV-positive subjects [28].
The same results were obtained by Iorio et al. by comparing the immune response elicited by the same vaccines in HIV patients under antiretroviral therapy [14]: MF59 adjuvanted influenza vaccine induced a better immune responses as compared with conventional vaccine in HIV positive HAART treated subjects [71].
Gabutti et al. compared the antibody responses elicited by an MF59 adjuvanted and a conventional subunit influenza vaccine in 37 HIV positive patients population, showing not significant differences between the two immunised groups and as regard as the three different influenza strains. An important aspect of the study was the prolonged persistence of specific antibodies versus all the vaccine strains: 51.7% of MF59 patients and 59.7% of subunit patients showed a seroprotective level of antibodies even 180 days after immunization [26]. During the last three years, several studies evaluated the performance of MF59 adjuvanted pandemic vaccine in HIV positives children and adults [49, 75, 78, 79, 81]. Both in adults and in children the immune response stimulated by a single or two doses of pandemic MF59 adjuvanted influenza vaccine was comparable in HIV infected patients and in healthy controls. In the study by Kajaste-Rudnitski et al. the seroconversion rate observed after a single dose of MF59®-adjuvanted influenza vaccine was lower in the HIV positive individuals as compared with HIV negative controls; however, the seroprotection rates were similar in both study groups [80]. Soonawala et al. reported the induction of cross reactive antibodies to pH1N1 after vaccination with seasonal TIV in HIV infected adults: authors hypothesized that HIV infected patients could produce larger quantities of cross reactive antibodies after vaccination because of a less well regulated B-cell immune response [75]. Palma et al. and Viganò et al. evaluated the immunogenicity of MF59®-adjuvanted pandemic influenza vaccine in HIV positive children and young adults, showing adequate levels of seroprotection already after a single dose; however, authors suggested a two-dose vaccination schedule in this population, in order to optimize and obtain a long-term antibody response [49, 81].
Thus, MF59®-adjuvanted influenza vaccine should be considered for use in HIV positive adults and children, because it could improve the effectiveness of influenza vaccination programmes in this population, who are at high-risk of influenza-related complications.
Another oil-in-water emulsion used as adjuvant in influenza vaccine is the AS03 adjuvant system. The AS03® adjuvant consisted of a 10% oil-in-water emulsion based adjuvant system, containing 5% dl-α-tocopherol (11.86 mg) and squalene (10.69 mg) in the oil phase and 2% of the non-ionic detergent Tween®80 (4.86 mg) in the aqueous phase. Recently, the AS03® adjuvant has been adopted in the licensed formulation of a H1N1 2009 pandemic vaccine. Some authors [51, 82] reported seroprotection rates lower after one dose of AS03 adjuvanted vaccine (61% to 75%) in HIV infected adults [51, 82, 83], while a second dose determines an increase up to 97.7% [76, 84]. According to these authors this difference could be attributed to the different timing of immunization during the pandemic outbreak, in relation to higher baseline or follow-up seroprotection rates. Concerning the seroconversion rates, other studies reported values of 88% to 95.3% after a single dose in HIV positive patients [48, 84, 85]. The collected data regarding the administration of a single dose of influenza AS03 adjuvanted vaccine are controversial: Manuel et al., reported a similar immune response in HIV patients and healthy control, while Kelly et al., showed that immune response correlate with a pre- existing antibodies and a single dose may be insufficient to induce protective immunity [86, 87]. Okike et al., reported that the use of ASO3 adjuvant in HIV positive children have likely played an important role in eliciting the high sero-response rates [50]. In general, the use of AS03 adjuvanted pandemic vaccine in HIV positive immunocompromised patients may lead to the expansion of coverage and increase the immune response [55, 83].
Intradermal influenza vaccines
Between strategies implemented to increase the immunogenicity of influenza vaccination in HIV patients, intradermal approach is also to be mentioned. In persons with impaired immunity intradermal vaccination is of particular interest because of different immunologic advantages.
The dermis harbours a network of antigen presenting cells, constituting up to 2% of all dermal cells, which forms an optimal environment to deliver a vaccine. In the study by Gelinck et al., 39 HIV positives adults received the 2005/2006 trivalent influenza vaccine delivered intradermally according to the CDC guidelines, using an intradermal injection syringe (BD Micro-Fine 0.5 ml U-100 insulin syringe) and needle (29G), also used for intradermal tuberculin injections. The intradermal vaccine dose contained 3 mg of haemaglutinin of the three strains. The intradermal vaccination with a low dose resulted in similar postvaccination titers as compared to standard intramuscular vaccination in the study groups: in particular only the HIV group had higher titers after intradermal vaccination. Results suggested that the intradermal vaccination is more efficient in inducing an immune response compared to intramuscular vaccination in HIV infected patients [22].
The superiority of the immune response elicited by the intradermal vaccine is shown by the values of the rates of seroprotection, seroconversion, and MFI/GMRT all higher than the vaccine administered intramuscularly to the controls. Ansaldi et al., in his study compared immunogenicity of licensed intradermal trivalent inactivated split vaccine delivered by licensed microsystem device with a lower antigen content (9 μg HA per strain) against the conventional intramuscular (15μg) influenza vaccine in a population of 54 HIV infected adults. Both vaccines meet the criteria for MFI and seroprotection rate but not for seroconversion against the B virus, there are no differences in terms of post-vaccination GMT /MFI, seroprotection and seroconversion rates comparing the two vaccines. The results of this trial showed that the licensed low antigen content ID vaccine was safe and immunogenic in HIV positive adults, although the small sample size of the study [53].
Conclusions
Influenza is a major cause of death, hospitalization and disability in immunocompromised population, resulting in an health and economic burden that may be reduced implementing annual vaccination as recommended by WHO guidelines.
The considerable experience accumulated about influenza vaccination refers a good safety and tolerability profile, in fact the adverse events reported are usually mild and resolve in a few days after their appearance.
About the vexed question of viral load increase, conflicting data are reported in literature. However, when this increase occurs, it is of transient nature and typically did not associate in CD4+ T cell counts changes.
Some studies reported immunogenicity data in HIV+ population, in which are compared different influenza vaccines, adjuvanted and not, and different administration routes.
The data are encouraging because an adequate immune response is shown, although split/subunit vaccine do not elicited an efficient immune response in these subjects.
New strategies were evaluated to increase the immune response in immunocompromised patients, as increase dosage, multiple dose vaccination, use of vaccine adjuvant, immunostimulant patches (the skin, especially its epidermal layer, is an accessible and competent immune environment and an attractive target for vaccine delivery, through transcutaneous delivery or immunostimulant patches) and different routes of vaccine delivery transcutaneous immunization, a topical vaccine application, combines the advantages of needle-free delivery while targeting the immunologically rich milieu of the skin [64, 70, 88, 89]. The administration of an MF59®- adjuvanted influenza subunit vaccine has been shown to improve immunogenicity and to elicited good immune responses and protective antibody [28, 91, 92]. Several studies estimated safety, tolerability and immunogenicity of intradermal influenza vaccine, the majority of which were conducted in elderly population; only one study was conducted on a population of immunocompromised patients. A dose-response relationship together with more efficient antibody response for intradermal vaccine was demonstrated using only a fifth of the normal dose evaluating the humoral response of intradermal influenza vaccination versus intramuscular vaccination. Local skin reactions can be used as predictors for the success of vaccination by identifying patients who may need a booster [54].
In general, the immunogenicity studies have shown encouraging results for the HIV positive subjects with antibody titres protecting, data on safety and tolerability are encouraging reporting only a few cases of serious effects on the population considered (about 10% of patients).
Definitely the most promising data concern the use of vaccine adjuvants, in particular with MF59®, and the use of new vaccine intradermal administration should be more extensively examined.
In the light of data reported in this review, there still is much to do about vaccination in immunocompromised patients. More extensive effectiveness studies are needed, to assess the impact of influenza vaccination and to prevent complications associated with it.
References
- 1.Beck CR, McKenzie BC, Hashim AB, et al. Influenza vaccination for immunocompromised patients:systematic review and meta-analysis from a public health policy perspective. PLoS One. 2011;6:e29249–e29249. doi: 10.1371/journal.pone.0029249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beck CR, McKenzie BC, Hashim AB, et al. Influenza vaccination for immunocompromised patients: systematic review and meta-analysis by etiology. J Infect Dis. 2012;206:1250–1259. doi: 10.1093/infdis/jis487. [DOI] [PubMed] [Google Scholar]
- 3.Kunisaki KM, Janoff EN. Influenza in immunosuppressed populations: a review of infection frequency, morbidity, mortality, and vaccine responses. Lancet Infect Dis. 2009;9:493–504. doi: 10.1016/S1473-3099(09)70175-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scuffham PA, West PA. Economic evaluation of strategies for the control and management of influenza in Europe. Vaccine. 2002;20:2562–2578. doi: 10.1016/s0264-410x(02)00154-8. [DOI] [PubMed] [Google Scholar]
- 5.Szucs T. The socio-economic burden of influenza. J Antimicrob Chemother. 1999;44(Suppl B):11–15. doi: 10.1093/jac/44.suppl_2.11. [DOI] [PubMed] [Google Scholar]
- 6.AIDS Day Report. UNAIDS World. 2011.
- 7.Klein MB, Lu Y, DelBalso L, et al. Influenza virus infection is a primary cause of febrile respiratory illness in HIV-infected adults, despite vaccination. Clin Infect Dis. 2007;45:234–240. doi: 10.1086/518986. [DOI] [PubMed] [Google Scholar]
- 8.Neuzil KM, Reed GW, Mitchel EF, Jr, et al. Influenza-associated morbidity and mortality in young and middle-aged women. JAMA. 1999;281:901–907. doi: 10.1001/jama.281.10.901. [DOI] [PubMed] [Google Scholar]
- 9.Lin JC, Nichol KL. Excess mortality due to pneumonia or influenza during influenza seasons among persons with acquired immunodeficiency syndrome. Arch Intern Med. 2001;161:441–446. doi: 10.1001/archinte.161.3.441. [DOI] [PubMed] [Google Scholar]
- 10.Neuzil KM, Coffey CS, Mitchel EF, Jr, et al. Cardiopulmonary hospitalizations during influenza season in adults and adolescents with advanced HIV infection. J Acquir Immune Defic Syndr. 2003;34:304–307. doi: 10.1097/00126334-200311010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25:5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 12.Loerbroks A, Stock C, Bosch JA, et al. Influenza vaccination coverage among high-risk groups in 11 European countries. Eur J Public Health. 2012;22:562–568. doi: 10.1093/eurpub/ckr094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Center for Disease Control and Prevention, author. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP)
- 14.Amendola A, Pariani E, Viganò A, et al. Influenza surveillance in a cohort of HIV-infected children and adolescents immunized against seasonal influenza. Vaccine. 2010;28:2700–2704. doi: 10.1016/j.vaccine.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 15.Fiore AE, Shay DK, Haber P, et al. Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC), author Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007. 2007 Jul 13;56(RR-6):1–54. [PubMed] [Google Scholar]
- 16.Atashili J, Kalilani L, Adimora AA. Efficacy and clinical effectiveness of influenza vaccines in HIV-infected individuals: a meta-analysis. BMC Infect Dis. 2006;6:138–138. doi: 10.1186/1471-2334-6-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. http://www.euro.who.int/__data/assets/pdf_file/0006/175254/WHO-Europe-recommendations-on-influenza-vaccinationduring- the-2012-2013-winter-season.pdf.
- 18. http://www.cdc.gov/mmwr/preview/mmwrhtml/00033693.htm.
- 19. http://www.cdc.gov/hiv/resources/reports/mmwr/1986.htm.
- 20. http://www.salute.gov.it/influenza/influenza.jsp.
- 21. http://www.euro.who.int/en/what-we-do/health topics communicable diseases/influenza/publications/2011/who europerecommendations- on-influenza-vaccination.
- 22.Gelinck LB, Bemt BJ, Marijt WA, et al. Intradermal influenza vaccination in immunocompromized patients is immunogenic and feasible. Vaccine. 2009;27:2469–2474. doi: 10.1016/j.vaccine.2009.02.053. [DOI] [PubMed] [Google Scholar]
- 23.Glenn GM, Thomas DN, Poffenberger KL, et al. Safety and immunogenicity of an influenza vaccine A/H5N1(A/Vietnam/ 1194/2004) when coadministered with a heat-labile enterotoxin (LT) adjuvant patch. Vaccine. 2009;27(Suppl 6):G60–G66. doi: 10.1016/j.vaccine.2009.10.031. [DOI] [PubMed] [Google Scholar]
- 24.Zanetti AR, Amendola A, Besana S, et al. Safety and immunogenicity of influenza vaccination in individuals infected with HIV. Vaccine. 2002;20(Suppl 5):B29–B32. doi: 10.1016/s0264-410x(02)00511-x. [DOI] [PubMed] [Google Scholar]
- 25.Amendola A, Boschini A, Colzani D, et al. Influenza vaccination of HIV-1-positive and HIV-1-negative former intravenous drug users. J Med Virol. 2001;65:644–648. doi: 10.1002/jmv.2085. [DOI] [PubMed] [Google Scholar]
- 26.Gabutti G, Guido M, Durando P, et al. Safety and immunogenicity of conventional subunit and MF59®-adjuvanted influenza vaccines in human immunodeficiency virus-1-seropositive patients. J Int Med Res. 2005;33:406–416. doi: 10.1177/147323000503300406. [DOI] [PubMed] [Google Scholar]
- 27.O'Brien WA, Grovit-Ferbas K, Namazi A, et al. Human immunodeficiency virus-type 1 replication can be increased in peripheral blood of seropositive patients after influenza vaccination. Blood. 1995;86:1082–1089. [PubMed] [Google Scholar]
- 28.Durando P, Fenoglio D, Boschini A, et al. Safety and immunogenicity of two influenza virus subunit vaccines, with or without MF59® adjuvant, administered to human immunodeficiency virus type 1-seropositive and -seronegative adults. Clin Vaccine Immunol. 2008;15:253–259. doi: 10.1128/CVI.00316-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cooper C, Klein M, Walmsley S, et al. High-level immunogenicity is achieved vaccine with adjuvanted pandemic H1N1(2009) and improved with booster dosing in a randomized trial of HIVinfected adults. HIV Clin Trials. 2012;13:23–32. doi: 10.1310/hct1301-023. [DOI] [PubMed] [Google Scholar]
- 30.Crum-Cianflone NF, Iverson E, Defang G, et al. Impact of the type of seasonal influenza vaccine on immune responses to the 2009 pandemic influenza A (H1N1) vaccine. Vaccine. 2011;29:9294–9295. doi: 10.1016/j.vaccine.2011.05.043. [DOI] [PubMed] [Google Scholar]
- 31.Hatakeyama S, Iwatsuki-Horimoto K, Okamoto K, et al. Unadjuvanted pandemic H1N1 influenza vaccine in HIV-1-infected adults. Vaccine. 2011;29:9224–9228. doi: 10.1016/j.vaccine.2011.09.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crum-Cianflone NF, Eberly LE, Duplessis C, et al. Immunogenicity of a monovalent 2009 influenza A (H1N1) vaccine in an immunocompromised population: a prospective study comparing HIV-infected adults with HIV-uninfected adults. Clin Infect Dis. 2011;52:138–146. doi: 10.1093/cid/ciq019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Phongsamart W, Sirisanthana V, Wittawatmongkol O, et al. Immunogenicity and safety of monovalent influenza A (H1N1) 2009 in HIV-infected Thai children. Vaccine. 2011;29:8705–8711. doi: 10.1016/j.vaccine.2011.08.101. [DOI] [PubMed] [Google Scholar]
- 34.Miraglia JL, Abdala E, Hoff PM, et al. Immunogenicity and reactogenicity of 2009 influenza A (H1N1) inactivated monovalent non-adjuvanted vaccine in elderly and immunocompromised patients. PLoS One. 2011;6:e27214–e27214. doi: 10.1371/journal.pone.0027214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hakim H, Allison KJ, Velde LA, et al. Immunogenicity and safety of inactivated monovalent 2009 H1N1 influenza A vaccine in immunocompromised children and young adults. Vaccine. 2012;30:879–880. doi: 10.1016/j.vaccine.2011.11.105. [DOI] [PubMed] [Google Scholar]
- 36.Maruszak H, Jeganathan S, Smith DE, et al. Improved serological response to H1N1 monovalent vaccine associated with viral suppression among HIV-1-infected patients during the 2009 influenza (H1N1) pandemic in the Southern Hemisphere. HIV Med. 2012;13:352–357. doi: 10.1111/j.1468-1293.2011.00987.x. [DOI] [PubMed] [Google Scholar]
- 37.Kikuchi T, Iwatsuki-Horimoto K, Adachi E, et al. Improved neutralizing antibody response in the second season after a single dose of pandemic (H1N1) 2009 influenza vaccine in HIV- 1-positive adults. Vaccine. 2012;30:3819–3823. doi: 10.1016/j.vaccine.2012.03.083. [DOI] [PubMed] [Google Scholar]
- 38.Flynn PM, Nachman S, Muresan P, et al. Safety and immunogenicity of 2009 pandemic H1N1 influenza vaccination in perinatally HIV-1-infected children, adolescents, and young adults. J Infect Dis. 2012;206:421–430. doi: 10.1093/infdis/jis360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lagler H, Grabmeier-Pfistershammer K, Touzeau-Römer V, et al. Immunogenicity and tolerability after two doses of nonadjuvanted, whole-virion pandemic influenza A (H1N1) vaccine in HIV-infected individuals. PLoS One. 2012;7:e36773–e36773. doi: 10.1371/journal.pone.0036773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chotirosniramit N, Sugandhavesa P, Aurpibul L, et al. Immune response to 2009 H1N1 vaccine in HIV-infected adults in Northern Thailand. Hum Vaccin Immunother. 2012;8 doi: 10.4161/hv.21820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cooper CL. Pandemic H1N12009 influenza and HIV: a review of natural history, management and vaccine immunogenicity. Curr Opin Infect Dis. 2012;25:26–35. doi: 10.1097/QCO.0b013e32834ef56c. [DOI] [PubMed] [Google Scholar]
- 42.Weinberg A, Song LY, Walker R, et al. Anti-influenza serum and mucosal antibody responses after administration of live attenuated or inactivated influenza vaccines to HIV-infected children. J Acquir Immune Defic Syndr. 2010;55:189–196. doi: 10.1097/QAI.0b013e3181e46308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weinberg A, Song LY, Fenton T, et al. T cell responses of HIVinfected children after administration of inactivated or live attenuated influenza vaccines. AIDS Res Hum Retroviruses. 2010;26:51–59. doi: 10.1089/aid.2009.0163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Levin MJ, Song LY, Fenton T, et al. Shedding of live vaccine virus, comparative safety, and influenza-specific antibody responses after administration of live attenuated and inactivated trivalent influenza vaccines to HIV-infected children. Vaccine. 2008;26:4210–4217. doi: 10.1016/j.vaccine.2008.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.King JC, Jr, Fast PE, Zangwill KM, et al. Safety, vaccine virus shedding and immunogenicity of trivalent, cold-adapted, live attenuated influenza vaccine administered to human immunodeficiency virus-infected and noninfected children. Pediatr Infect Dis J. 2001;20:1124–1131. doi: 10.1097/00006454-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 46.King JC, Jr, Treanor J, Fast PE, et al. Comparison of the safety, vaccine virus shedding, and immunogenicity of influenza virus vaccine, trivalent, types A and B, live cold-adapted, administered to human immunodeficiency virus (HIV)-infected and non-HIV-infected adults. J Infect Dis. 2000;181:725–728. doi: 10.1086/315246. [DOI] [PubMed] [Google Scholar]
- 47. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5306a1.htm.
- 48.Launay O, Desaint C, Durier Cer, et al. Safety and immunogenicity of a monovalent 2009 influenza A/H1N1v vaccine adjuvanted with AS03® or unadjuvanted in HIV-infected adults: a randomized, controlled trial. J Infect Dis. 2011;204:124–134. doi: 10.1093/infdis/jir211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Palma P, Romiti ML, Bernardi S, et al. Safety and immunogenicity of a monovalent MF59®-adjuvanted A/H1N1 vaccine in HIV-infected children and young adults. Biologicals. 2012;40:134–139. doi: 10.1016/j.biologicals.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 50.Okike IO, Yung C, Ladhani S, et al. The immunogenicity of a novel A (H1N1) vaccine in HIV-infected children. Vaccine. 2011;29:6636–6640. doi: 10.1016/j.vaccine.2011.06.103. [DOI] [PubMed] [Google Scholar]
- 51.Tremblay CL, Rouleau D, Fortin C, et al. Immunogenicity and tolerability of an inactivated and adjuvanted pandemic H1N1 influenza vaccine, in HIV-1-infected patients. Vaccine. 2011;29:1359–1363. doi: 10.1016/j.vaccine.2010.12.023. [DOI] [PubMed] [Google Scholar]
- 52.Calmy A, Bel M, Nguyen A, et al. Strong serological responses and HIV RNA increase following AS03-adjuvanted pandemic immunization in HIV-infected patients. HIV Med. 2012;13:207–218. doi: 10.1111/j.1468-1293.2011.00961.x. [DOI] [PubMed] [Google Scholar]
- 53.Ansaldi F, Valle L, Florentiis D, et al. Phase 4 randomized trial of intradermal low-antigen-content inactivated influenza vaccine versus standard-dose intramuscular vaccine in HIV-1- infected adults. Hum Vaccin Immunother. 2012;8:1048–1052. doi: 10.4161/hv.20347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Evison J, Farese S, Seitz M, et al. Randomized, doubleblind comparative trial of subunit and virosomal influenza vaccines for immunocompromised patients. Clin Infect Dis. 2009;48:1402–1412. doi: 10.1086/598193. [DOI] [PubMed] [Google Scholar]
- 55.Ho J, Moir S, Wang W, et al. Enhancing effects of adjuvanted 2009 pandemic H1N1 influenza A vaccine on memory B-cell responses in HIV-infected individuals. AIDS. 2011;25:295–302. doi: 10.1097/QAD.0b013e328342328b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fuller JD, Craven DE, Steger KA, et al. Influenza vaccination of human immunodeficiency virus (HIV)-infected adults: impact on plasma levels of HIV type 1 RNA and determinants of antibody response. Clin Infect Dis. 1999;28:541–547. doi: 10.1086/515170. [DOI] [PubMed] [Google Scholar]
- 57.Couch RB. Influenza, influenza virus vaccine, and human immunodeficiency virus infection. Clin Infect Dis. 1999;28:548–550. doi: 10.1086/515171. [DOI] [PubMed] [Google Scholar]
- 58.Günthard HF, Wong JK, Spina CA, et al. Effect of influenza vaccination on viral replication and immune response in persons infected with human immunodeficiency virus receiving potent antiretroviral therapy. J Infect Dis. 2000;181:522–523. doi: 10.1086/315260. [DOI] [PubMed] [Google Scholar]
- 59.Skiest DJ, Machala T. Comparison of the effects of acute influenza infection and Influenza vaccination on HIV viral load and CD4 cell counts. J Clin Virol. 2003;26:307–315. doi: 10.1016/s1386-6532(02)00047-1. [DOI] [PubMed] [Google Scholar]
- 60.Fowke KR, D'Amico R, Chernoff DN, et al. Immunologic and virologic evaluation after influenza vaccination of HIV-1--infected patients. AIDS. 1997;11:1013–1021. doi: 10.1097/00002030-199708000-00010. [DOI] [PubMed] [Google Scholar]
- 61.Glesby MJ, Hoover DR, Farzadegan H, et al. The effect of influenza vaccination on human immunodeficiency virus type 1 load: a randomized, double-blind, placebo-controlled study. J Infect Dis. 1996;174:1332–1336. doi: 10.1093/infdis/174.6.1332. [DOI] [PubMed] [Google Scholar]
- 62.Pinto LA, Blazevic V, Anderson SA, et al. Influenza virus-stimulated generation of anti-human immunodeficiency virus (HIV) activity after influenza vaccination in HIV-infected individuals and healthy control subjects. J Infect Dis. 2001;183:1000–1008. doi: 10.1086/319277. [DOI] [PubMed] [Google Scholar]
- 63.Tasker SA, O'Brien WA, Treanor JJ, et al. Effects of influenza vaccination in HIV-infected adults: a double-blind,placebocontrolled trial. Vaccine. 1998;16:1039–1042. doi: 10.1016/s0264-410x(97)00275-2. [DOI] [PubMed] [Google Scholar]
- 64.Staprans SI, Hamilton BL, Follansbee SE, et al. Activation of virus replication after vaccination of HIV-1-infected individuals. J Exp Med. 1995;182:1727–1737. doi: 10.1084/jem.182.6.1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Madhi SA, Maskew M, Koen A, et al. Trivalent inactivated influenza vaccine in African adults infected with human immunodeficient virus: double blind,randomized clinical trial of efficacy, immunogenicity, and safety. Clin Infect Dis. 2011;52:128–137. doi: 10.1093/cid/ciq004. [DOI] [PubMed] [Google Scholar]
- 66.Kosalaraksa P, Srirompotong U, Newman RW, et al. Serological response to trivalent inactive influenza vaccine in HIVinfected children with different immunologic status. Vaccine. 2011;29:3055–3060. doi: 10.1016/j.vaccine.2011.01.091. [DOI] [PubMed] [Google Scholar]
- 67.Machado AA, Machado CM, Boas LS, et al. Short communication: immunogenicity of an inactivated influenza vaccine and postvaccination influenza surveillance in HIV-infected and non-infected children and adolescents. AIDS Res Hum Retroviruses. 2011;27:999–1003. doi: 10.1089/AID.2010.0306. [DOI] [PubMed] [Google Scholar]
- 68.Tanzi E, Esposito S, Bojanin J, et al. Immunogenicity and effect of a virosomal influenza vaccine on viral replication and T-cell activation in HIV-infected children receiving highly active antiretroviral therapy. J Med Virol. 2006;78:440–445. doi: 10.1002/jmv.20559. [DOI] [PubMed] [Google Scholar]
- 69.Zuccotti GV, Zenga A, Durando P, et al. Immunogenicity and tolerability of a trivalent virosomal influenza vaccine in a cohort of HIV-infected children. J Int Med Res. 2004;32:492–499. doi: 10.1177/147323000403200506. [DOI] [PubMed] [Google Scholar]
- 70.Esposito S, Tagliaferri L, Daleno C, et al. Pandemic influenza A/H1N1 vaccine administered sequentially or simultaneously with seasonal influenza vaccine to HIV-infected children and adolescents. Vaccine. 2011;29:1677–1682. doi: 10.1016/j.vaccine.2010.12.047. [DOI] [PubMed] [Google Scholar]
- 71.Iorio AM, Francisci D, Camilloni B, et al. Antibody responses and HIV-1 viral load in HIV-1-seropositive subjects immunised with either the MF59-adjuvanted influenza vaccine or a conventional non-adjuvanted subunit vaccine during highly active antiretroviral therapy. Vaccine. 2003;21:3629–3637. doi: 10.1016/s0264-410x(03)00408-0. [DOI] [PubMed] [Google Scholar]
- 72.Committee for Proprietary Medicinal Products (CPMP), author Note for guidance on harmonisation of requirements for influenza vaccines. 1997 Mar; http://www.ema.europa.eu/ema/ [Google Scholar]
- 73.Gorse GJ, Otto EE, Powers DC, et al. Induction of mucosal antibodies by live attenuated and inactivated influenza virus vaccines in the chronically ill elderly. J Infect Dis. 1996;173:285–290. doi: 10.1093/infdis/173.2.285. [DOI] [PubMed] [Google Scholar]
- 74.Boyce TG, Gruber WC, Coleman-Dockery SD, et al. Mucosal immune response to trivalent live attenuated intranasal influenza vaccine in children. Vaccine. 1999;18:82–88. doi: 10.1016/s0264-410x(99)00183-8. [DOI] [PubMed] [Google Scholar]
- 75.Soonawala D, Rimmelzwaan GF, Gelinck LB, et al. Response to 2009 pandemic influenza A (H1N1) vaccine in HIV-infected patients and the influence of prior seasonal influenza vaccination. PLoS One. 2011;6:e16496–e16496. doi: 10.1371/journal.pone.0016496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bickel M, Hentig N, Wieters I, et al. Immune response after two doses of the novel split virion, adjuvanted pandemic H1N1 influenza A vaccine in HIV-1-infected patients. Clin Infect Dis. 2011;52:122–127. doi: 10.1093/cid/ciq003. [DOI] [PubMed] [Google Scholar]
- 77.Tebas P, Frank I, Lewis M, et al. Poor immunogenicity of the H1N1 2009 vaccine in well controlled HIV-infected individuals. AIDS. 2010;24:2187–2192. doi: 10.1097/QAD.0b013e32833c6d5c. [DOI] [PubMed] [Google Scholar]
- 78.Fabbiani M, Giambenedetto S, Sali M, et al. Immune response to influenza A (H1N1)v monovalent MF59-adjuvanted vaccine in HIV-infected patients. Vaccine. 2011;29:2836–2839. doi: 10.1016/j.vaccine.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 79.Pariani E, Boschini A, Amendola A, et al. Response to 2009 pandemic and seasonal influenza vaccines co-administered to HIV-infected and HIV-uninfected former drug users living in a rehabilitation community in Italy. Vaccine. 2011;29:9209–9213. doi: 10.1016/j.vaccine.2011.09.103. [DOI] [PubMed] [Google Scholar]
- 80.Kajaste-Rudnitski A, Galli L, Nozza S, et al. Induction of protective antibody response by MF59-adjuvanted 2009 pandemic A/H1N1v influenza vaccine in HIV-1-infected individuals. AIDS. 2011;25:177–183. doi: 10.1097/QAD.0b013e328341afa8. [DOI] [PubMed] [Google Scholar]
- 81.Viganò A, Giacomet V, Pariani E, et al. Long-term immunogenicity after one and two doses of a monovalent MF59- adjuvanted A/H1N1 Influenza virus vaccine coadministered with the seasonal 2009-2010 nonadjuvanted Influenza virus vaccine in HIV-infected children, adolescents, and young adults in a randomized controlled trial. Clin Vaccine Immunol. 2011;18:1503–1509. doi: 10.1128/CVI.05200-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bickel M, Wieters I, Khaykin P, et al. Low rate of seroconversion after vaccination with a split virion, adjuvanted pandemic H1N1 influenza vaccine in HIV-1-infected patients. AIDS. 2010;24:F31–F35. doi: 10.1097/QAD.0b013e3283398da1. [DOI] [PubMed] [Google Scholar]
- 83.Siegrist CA, Delden C, Bel M, et al. Higher memory responses in HIV-infected and kidney transplanted patients than in healthy subjects following priming with the pandemic vaccine. PLoS One. 2012;7:e40428–e40428. doi: 10.1371/journal.pone.0040428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nielsen AB, Nielsen HS, Nielsen L, et al. Immune response after one or two doses of pandemic influenza A (H1N1) monovalent, AS03-adjuvanted vaccine in HIV infected adults. Vaccine. 2012;30:7067–7071. doi: 10.1016/j.vaccine.2012.09.052. [DOI] [PubMed] [Google Scholar]
- 85.Orlando G, Pariani E, Mazza F, et al. Pandemic influenza vaccine in adult HIV-1-infected patients. AIDS. 2010;24:2142–2143. doi: 10.1097/QAD.0b013e32833cfcb0. [DOI] [PubMed] [Google Scholar]
- 86.Manuel O, Pascual M, Hoschler K, et al. Humoral response to the influenza A H1N1/09 monovalent AS03-adjuvanted vaccine in immunocompromised patients. Clin Infect Dis. 2011;52:248–256. doi: 10.1093/cid/ciq104. [DOI] [PubMed] [Google Scholar]
- 87.Kelly D, Burt K, Missaghi B, et al. Responses to pandemic ASO3-adjuvanted A/California/07/09 H1N1 influenza vaccine in human immunodeficiency virus-infected individuals. BMC Immunol. 2012;13:49–49. doi: 10.1186/1471-2172-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ragni MV, Ruben FL, Winkelstein A, et al. Antibody responses to immunization of patients with hemophilia with and without evidence of human immunodeficiency virus (human T-lymphotropic virus type III) infection. J Lab Clin Med. 1987;109:545–549. [PubMed] [Google Scholar]
- 89.Kroon FP, Dissel JT, Jong JC, et al. Antibody response after influenza vaccination in HIV-infected individuals: a consecutive 3-year study. Vaccine. 2000;18:3040–3049. doi: 10.1016/s0264-410x(00)00079-7. [DOI] [PubMed] [Google Scholar]
- 90.Glenn GM, Kenney RT, Hammond SA, et al. Transcutaneous immunization and immunostimulant strategies. Immunol Allergy Clin North Am. 2003;23:787–813. doi: 10.1016/s0889-8561(03)00094-8. [DOI] [PubMed] [Google Scholar]
- 91.Glenn GM, Taylor DN, Li X, et al. Transcutaneous immunization: a human vaccine delivery strategy using a patch. Nat Med. 2000;6:1403–1406. doi: 10.1038/82225. [DOI] [PubMed] [Google Scholar]
- 92.Nicholson KG, Colegate AE, Podda A, et al. Safety and antigenicity of non-adjuvanted and MF59®-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a randomised trial of two potential vaccines against H5N1 influenza. Lancet. 2001;357:1937–1943. doi: 10.1016/S0140-6736(00)05066-2. [DOI] [PubMed] [Google Scholar]