Abstract
The purpose of this study is to investigate the outcomes from anchor-induced chondral damage of the hip, both with and without frank chondral penetration. A multicenter retrospective case series was performed of patients with chondral deformation or penetration during initial hip arthroscopic surgery. Intra-operative findings, post-surgical clinical courses, hip outcome scores and descriptions of arthroscopic treatment in cases requiring revision surgery and anchor removal are reported. Five patients (three females) of mean age 32 years (range, 16–41 years) had documented anchor-induced chondral damage with mean 3.5 years (range, 1.5–6.0 years) follow-up. The 1 o'clock position (four cases) and anterior and mid-anterior portals (two cases each) were most commonly implicated. Two cases of anchor-induced acetabular chondral deformation without frank penetration had successful clinical and radiographic outcomes, while one case progressed from deformation to chondral penetration with clinical worsening. Of the cases that underwent revision hip arthroscopy, all three had confirmed exposed hard anchors which were removed. Two patients have had clinical improvement and one patient underwent early total hip arthroplasty. Anchor-induced chondral deformation without frank chondral penetration may be treated with close clinical and radiographic monitoring with a low threshold for revision surgery and anchor removal. Chondral penetration should be treated with immediate removal of offending hard anchor implants. Preventative measures include distal-based portals, small diameter and short anchors, removable hard anchors, soft suture-based anchors, curved drill and anchor insertion instrumentation and attention to safe trajectories while visualizing the acetabular articular surface.
INTRODUCTION
The acetabular labrum provides a significant functional role and may be important in overall hip preservation [1–4]. Labral tears often occur in the setting of bony dysmorphisms such as dysplasia and femoroacetabular impingement (FAI). Arthroscopic surgery for FAI is a less invasive option that typically addresses bony deformities and chondrolabral pathology [5, 6]. Patients undergoing labral refixation have better outcomes than those undergoing labral debridement [7–10]. When the labrum is deficient and/or irreparable, labral reconstruction has been performed with early successful outcomes [11–15]. Current labral repair and reconstruction techniques utilize suture anchor fixation.
Suture anchors provide a common method for fixation of soft tissues to bone. In order to restore labral function including the labral fluid seal effect, the fixation device should be placed on the acetabular rim close to but not violating the articular cartilage or joint [16, 17]. Suture anchors placed too far from the articular cartilage can evert or medialize the labrum, compromising its function; anchors placed too close to the articular cartilage can cause iatrogenic cartilage injury. Complications related to suture anchors have been documented, mainly in the shoulder literature including chondrolysis, osteolysis, synovitis, articular cartilage damage and fixation failure [18–22]. Consequences from anchor-induced chondral damage may be devastating, especially in young patients, and treatment options may be suboptimal and few (e.g. arthrodesis or arthroplasty). Several studies and systematic reviews have documented complications from hip arthroscopy [23–26] however we could find no case reports or case series of anchor-induced chondral damage associated with hip arthroscopy.
The purpose of this case series is to introduce anchor-induced chondral damage as a formal complication of hip arthroscopy while presenting arthroscopic treatment options, preventative measures and outcomes.
METHODS
Five patients were identified among four high-volume arthroscopic hip surgeons (arbitrarily defined as 100+ cases per annum). Inclusion criteria were documentation in operative report of violation (penetration or deformation) of acetabular articular cartilage attributed to one or more suture anchors placed during hip arthroscopic surgery and/or arthroscopic confirmation on initial and/or revision surgery with minimum 1-year follow-up. Exclusion criteria included patients without confirmed documentation and arthroscopic confirmation of anchor-induced chondral violation or <1 year follow-up. Retrospective medical record review was performed by each respective surgeon including pre-operative diagnosis, arthroscopic procedure(s), location on acetabular rim by clockface method, number and, where known, type and size of suture anchors, portals used for anchor placement, post-operative outcomes with patient-reported outcome measure where available and type/outcome of any revision surgeries.
Case 1
A 33-year-old female recreational runner underwent hip arthroscopy for cam FAI. Diagnostic arthroscopic evaluation of the central compartment revealed an anterior labral tear at the 1–2 o'clock position. Labral repair was performed utilizing two 2.3-mm suture anchors (Osteoraptor, Smith and Nephew, Andover, MA, USA) placed via the mid-anterior portal. After placement of the suture anchors, inspection of the acetabular cartilage revealed focal ballooning of the articular chondral surface adjacent to the labral repair (Fig. 1). Post-operative rehabilitation was uneventful with protective weightbearing for 2 weeks. She returned to normal activities after 6 months without symptoms. Two-year follow-up revealed improvement of modified Harris Hip Score Hip (mHHS) (from 67 to 96), Hip Outcome Score Daily Activity Part 1 (from 88 to 100) and Sport Specific Part 2 (from 33 to 86) and post-operative radiographs revealed joint space preservation (Fig. 2).
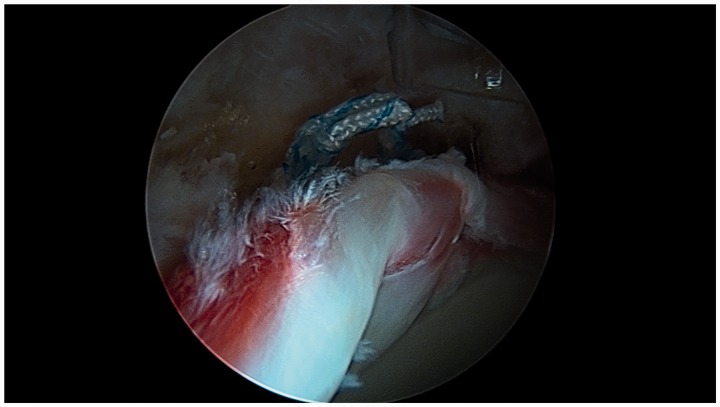
Fig. 1.
Supine arthroscopic image of right hip from anterolateral portal showing acetabular chondral elevation adjacent to the labral repair with suture anchor fixation.
Fig. 2.
Post-operative AP radiograph of right hip. Note well-preserved joint.
Case 2
A 16-year-old male high-school swimmer with mixed FAI which was treated with elective arthroscopic rim trimming and femoroplasty. During suture anchor placement via mid-anterior portal for anterosuperior labral refixation, the acetabular articular cartilage was elevated but not penetrated by a 3.5-mm knotless anchor (Push-lock, Arthrex, Naples, FL, USA). The anchor was not removed. The patient had an uneventful post-operative course and eventually resumed asymptomatic competitive swimming and intramural collegiate basketball. His pre-operative non-arthritic hip score (NAHS) was 34 and his latest post-operative NAHS was 89 at 6 years following surgery and radiographs show no joint deterioration or narrowing.
Case 3
A 30-year-old semi-professional bowler with symptomatic cam-pincer FAI underwent elective arthroscopic acetabuloplasty and femoroplasty. Labral refixation was performed via the modified mid-anterior portal [27] with 3.5-mm suture anchors (Pushlock, Arthrex, Naples, FL, USA) was performed at the 1 and 2 o’clock positions. During suture anchor placement, mild elevation of adjacent acetabular articular cartilage without implant penetration was seen. Sixteen months later, because of recurrent groin pain and index of suspicion, revision hip arthroscopy was performed at that time the suture anchor was partly visible under a ‘veil’ of thin translucent articular cartilage. Probing revealed no gross motion of the seated implant. A 4-mm unhooded burr was used to remove the encroaching longitudinal side of the anchor, initially at chondral surface level, to a subchondral level 2 mm below the articular surface. After an initial 6 weeks of protected weightbearing, he felt initial subjective improvement. But by 10 months, his pain had returned. He underwent a second revision arthroscopy. Intra-operatively, the previously burr-resected side of the anchor was exposed at the level of the adjacent chondral surfaces (Fig. 3) but not loose. Outerbridge grade 2 changes were observed at the anterior apex of the femoral head. Conservative ‘unroofing’ of marginal cartilage was done with a shaver. The anchor was dislodged using a microfracture awl and subsequently removed with a grasper through an 8-mm arthroscopic cannula without incident (Fig. 4). The remaining trough was treated with microfracture chondroplasty (Fig. 5). Pain and mechanical symptoms gradually resolved. Pre-operative NAHS of 36 decreased to a nadir of 18 at 10 months post-first revision, and increased to 88 at 2.4 years post-second revision surgery. Post-operative radiographs showed no joint narrowing. He has resumed competitive bowling and limits impact sports.
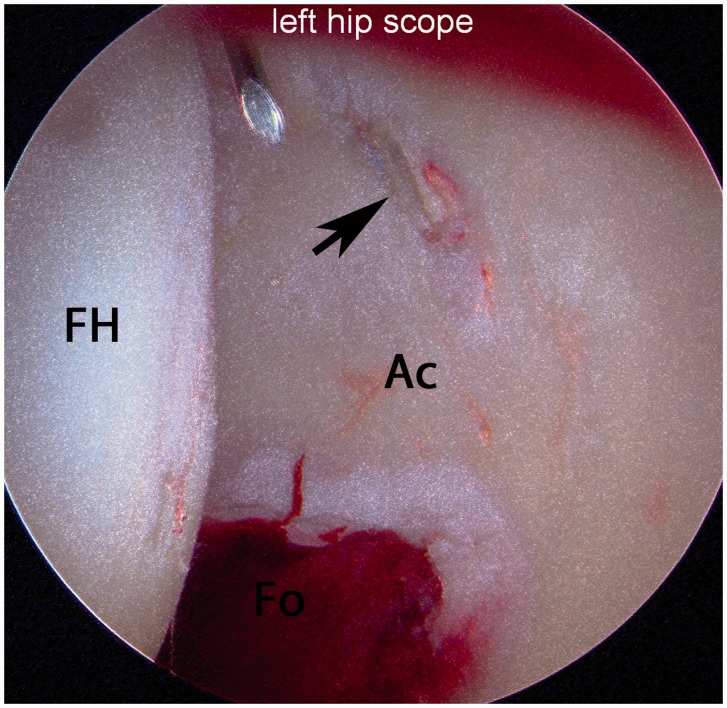
Fig. 3.
Supine arthroscopic image from anterolateral portal of left hip during establishment of modified mid-anterior portal (note entry needle and stylet). One can see an exposed hard anchor (arrow) that has penetrated the anterior acetabular articular cartilage. Ac, acetabulum, FH, femoral head.
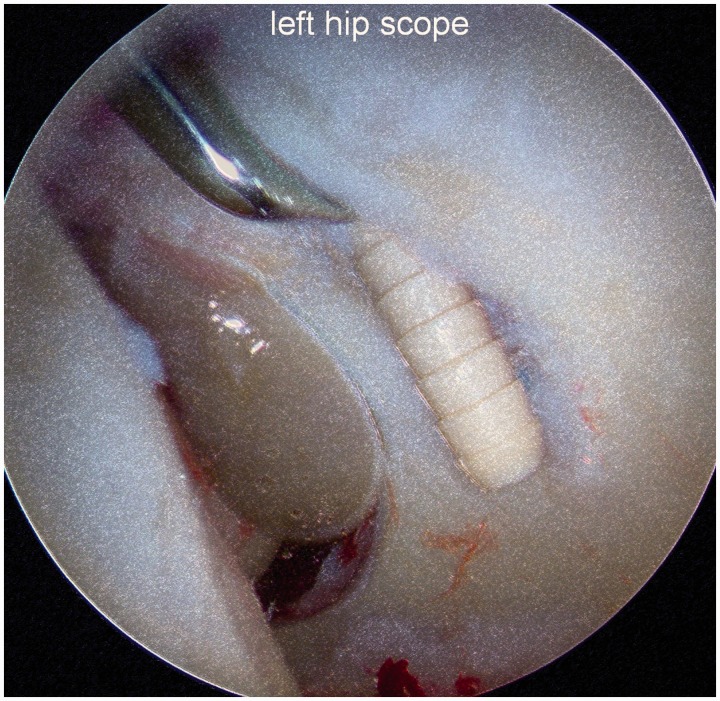
Fig. 4.
Arthroscopic image of left hip showing a microfracture awl displacing the embedded but exposed anchor.
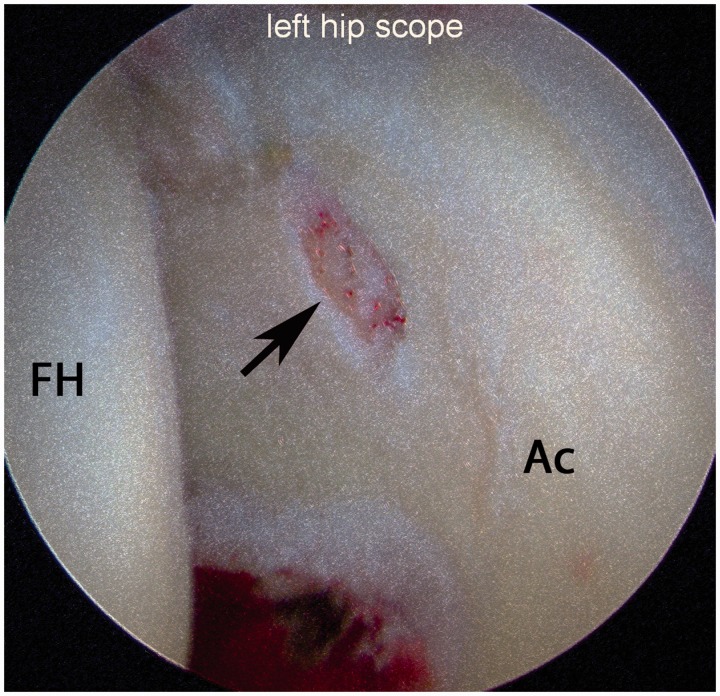
Fig. 5.
Arthroscopic image of left hip after anchor removal and microfracture chondroplasty. Ac, acetabulum, FH, femoral head.
Case 4
A 40-year-old active woman underwent arthroscopic femoral osteoplasty, acetabuloplasty and labral refixation. She complained of more pain following surgery than prior to surgery, had some radiographic medial joint narrowing (initial pre-operative radiographs were unavailable). She elected revision hip arthroscopy, where her anterosuperior labral repair had failed, and she had full thickness articular cartilage flaps and exposed bone. A suture was noted in this area on the articulating surface, and followed to an anchor on the mid-articular surface. The angle of the suture anchor appears that it had entered the acetabular rim at the 1 o’clock position and no distal-based portals had been used in the initial hip arthroscopy. In addition, there was wearing of the articular cartilage on the central femoral head. The patient had the anchor and sutures removed as well as the articular cartilage and labrum debrided. The degree of articular cartilage loss was deemed too excessive to justify microfracture chondroplasty. She subjectively feels 90% of normal and does not feel limited by her hip. At 1.5 years, she had improvement of the IHOT-33 score (from 11.2 to 68.8, with global change rating of 90) and mHHS (from 30.8 to 84.7). Radiographs demonstrate some progression of her medial joint space narrowing.
Case 5
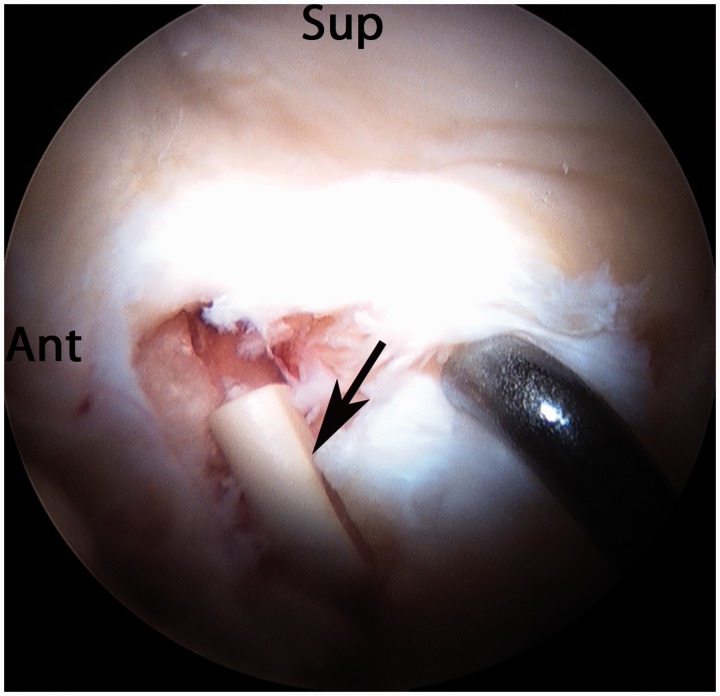
A 41-year-old woman had unrelenting pain and locking following right hip arthroscopy with a 2-anchor labral repair performed by another physician 3 months prior. No distal-based portals had been used in that surgery. Her radiographs showed preserved joint space with residual cam and pincer FAI, which was not treated in her previous procedure. The patient elected revision surgery to address her worsening pain and unaddressed FAI. During revision hip arthroscopy, both of her previous anchors for her labral repair were found to have penetrated her subchondral bone, had become intra-articular, and significantly damaged the cartilage on the acetabulum at the 12 o’clock and 2 o’clock positions (Fig. 6). Arthroscopic removal of the two anchors and debridement of the joint was performed. The chondral and labral damage was deemed too excessive to justify labral reconstruction. Her pain continued to worsen and given the extensive damage to the joint, the decision was made to proceed with total hip replacement at 42 years of age.
Fig. 6.
Supine arthroscopic image of right hip from anterolateral portal showing extensive acetabular chondral damage from one (arrow) of two penetrating hard anchors. Ant, anterior, Sup, superior.
RESULTS
Five patients (three females) of mean age 32 years (range, 16–41 years) had documented anchor-induced chondral damage with mean 3.5 year (range, 1.5–6.0 years) follow-up. All cases involved various hard suture anchors placed in along the anterosuperior acetabular rim with the 1 o’clock position most commonly involved (four cases). Various portals were utilized for anchor placement (two each via anterior portal and mid-anterior portal, one via modified mid-anterior portal). Two cases of anchor-induced acetabular chondral deformation without frank penetration had successful clinical and radiographic outcomes at 2 and 6 years (Cases 1 and 2), while one case (Case 3) progressed from deformation to chondral penetration with clinical worsening. Of the cases that underwent revision hip arthroscopy for worsening symptoms, all three had confirmed exposed hard anchors which were removed using arthroscopic techniques. Two patients (Cases 3 and 4) have had clinical improvement reflected in increased patient-reported outcome scores and one patient underwent early total hip arthroplasty (Case 5). These findings are summarized in Table I.
Table I.
Study findings
| Patient | Age (years) | Anchor type | Guide | Portal | Location (O'Clock) | Chondral damage | Pre-op PROS | Post-op PROS | Post-revision PROS | PROM |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 33 | Hard | Straight | MAP | 2 | PT | 67 | 96 | mHHS | |
| 2 | 16 | Hard | Straight | MAP | 1 | PT | 34 | 89 | NAHS | |
| 3 | 30 | Hard | Straight | mMAP | 2 | PT–>FT | 36 | 18 | 88 | NAHS |
| 4 | 40 | Hard | Straight | AP | 1 | FT | 31 | 85 | mHHS | |
| 5 | 41 | Hard | Straight | AP | 12, 2 | FT |
MAP = mid-anterior portal, mMAP = modified mid-anterior portal, AP = anterior portal, PT = partial thickness, FT = full thickness, PROS = patient-measured outcome score, PROM = patient measured outcome measure, mHHS = modified Harris Hip Score, NAHS = Non-arthritic Hip Score.
DISCUSSION
To our knowledge, this is the first series of this heretofore undocumented complication of hip arthroscopy. Anchor-induced chondral damage of the hip may occur in three potential forms: acetabular chondral deformation, chondral penetration with intra-articular implant exposure and loose anchor implant (whole or in pieces). Indeed, these forms may represent progressive stages. At least three of the cases (Cases 1, 2 and 3) had documented anchor-induced chondral deformation without penetration with resultant ballooning or elevation of acetabular cartilage implying violation of subchondral bone and focal chondral delamination. Of these, two cases demonstrated clinical improvement (Cases 1 and 2) without radiographic hip degeneration at short- and mid-term, while one case experienced clinical deterioration prompting revision arthroscopy with confirmed progression to chondral penetration (Case 3).
Revision hip arthroscopy may be helpful in select patients. Three patients underwent revision hip arthroscopy including anchor removal for persistent or worsening symptoms; of two patients demonstrating clinical improvement, one retained normal radiographic joint appearance (Case 3) and the other had progressive partial medial joint narrowing (Case 4). The one patient who failed revision hip arthroscopy (Case 5) had two exposed anchors and major chondral damage. She ultimately improved with total hip arthroplasty albeit at a young age. It is unknown whether earlier anchor removal may prevent/delay joint deterioration.
Treatment options, many learned from shoulder arthroscopy, depend on whether the offending anchor is hard or soft, threaded or barbed, fully or partially seated at the acetabular rim or loose and causing chondral deformation versus penetration. All errant anchors in this case series were non-threaded non-metallic hard anchors which were fully seated. It seems reasonable to remove an embedded errant anchor immediately in the case of gross chondral penetration or chondral deformation if surgically amenable to such treatment without causing excessive bone removal and/or further chondral damage. Hard anchors with threaded designs facilitate removal by reversing the rotatory direction of insertion. Partially seated barbed anchors may possibly be removed in a retrograde manner using a grasper that fits through an arthroscopic cannula. If the anchor can be disengaged in alignment with the grasper and cannula, it may be extracted through the retained cannula. An alternative is to use a slotted cannula, extracting the grasped anchor in unison with the slotted cannula. (This technique also enables arthroscopic removal of loose or foreign bodies too big to fit through conventional cannulas.) A trephine or 6-mm osteochondral autograft transfer system harvester may be tamped over the anchor and turned in a counterclockwise manner [28]. This technique, however, may cause extensive osteochondral collateral damage and perhaps should be considered a last resort. Anterograde advancement of a penetrating anchor may permit its removal via the central compartment, perhaps causing less chondral damage. If the offending anchor is not removable, one may burr down the exposed surface however fixation strength may be compromised leading to loss of fixation and/or an intra-articular loose implant. If not overly proud, loose and/or impinging, one may leave the anchor as-is, perhaps modifying post-operative rehabilitation and monitoring (see below).
Arthroscopic removal of a fully seated hard anchor that penetrates the articular cartilage may be removed en bloc or piecemeal under hip distraction via the central compartment (Table II). En bloc removal may require limited debridement of immediately adjacent articular cartilage and the use of a small angled curette or microfracture awl as presented in Case 3. Once excavated from its osteochondral bed, the anchor may be removed with aforementioned arthroscopic techniques. Partial or complete piecemeal removal of a non-metallic hard anchor may be facilitated with a burr. In some cases, an unhooded or retractable sheath burr (Smith and Nephew, Andover, MA, USA) may aid visualization and arthroscopic resection. During burr resection, one may find that the anchor becomes disengaged so that it can be removed. A final option is to burr down the proud anchor to a stable subchondral position. Arthroscopic ‘anchor-plasty’ was attempted in Case 3, however clinical improvement was temporary. Arthroscopic lavage of the hip to remove debris that could cause synovitis or third body wear is then performed. If damage to the hip is extensive, conversion hip arthroplasty may be performed (Case 5).
Table II.
Treatment options for anchor-induced chondral penetration
| Arthroscopic reduction anchor-plasty (only if stable anchor) |
| Burr resection of encroaching region of anchor to subchondral level |
| Arthroscopic anchor removal |
| En Bloc |
| Retrograde |
| Unscrew threaded anchor |
| Arthroscopic grasper |
| Trephine over fixated anchor |
| Anterograde |
| Remove once loose in central compartment |
| Piecemeal (unhooded or retractable sheath burr) and lavage |
| Consider microfracture base of defect |
We have no experience with a detached anchor in the hip but agree with treatment recommendations in the shoulder. If the anchor is intra-articular, we agree with arthroscopic surgery for anchor removal and treatment of any associated chondrolabral pathology. If the anchor is in an intra-capsular but safe extra-articular location and appears stationary on serial MRIs, surgical removal may not be necessary. If not easily amenable to removal, retention of a non-penetrating errant anchor causing chondral elevation may be closely monitored, perhaps altering post-operative rehabilitation and monitoring (Table III). Until proven otherwise, it seems prudent to recommend treating patients with anchor-induced chondral elevation with prolonged restricted weightbearing, perhaps similar to protocols following microfracture chondroplasty, and to minimize future impact activities. It is also our opinion that relatively frequent post-operative clinic visits supplemented with interval radiographic assessment are merited. A low threshold for revision hip arthroscopy with timely anchor removal may minimize irreversible joint damage from third body wear.
Table III.
Treatment options for anchor-induced chondral deformation
| Leave as-is but do not advance further |
| Remove if accessible and removal does not cause more damage |
| Close post-operative monitoring (Clinical, radiographic, MRI) |
| Modified post-operative rehabilitation |
If errant anchor placement leads to chondral penetration with visualized exposure of the hard implant, we recommend immediate removal of that implant. If, however, chondral elevation without penetration is detected and the anchor is not readily removable, frequent clinical and radiographic monitoring, perhaps supplemented with magnetic resonance imaging of non-metallic anchors may be reasonable. If clinical worsening, especially if pain with non-impinging hip positions (e.g. extension), even minimal joint narrowing and/or anchor penetration is demonstrated, timely arthroscopic surgery with anchor removal is suggested prior to potentially irreversible osteoarthrosis or intra-articular loose body generation.
Several technical pearls may help prevent the errant suture anchor and its potentially devastating consequences. A distal-based arthroscopic working portal can improve the trajectory of anchor placement by better matching the specific skeletal geometry of the acetabular rim [29]. Compared with the mid-anterior portal, the modified mid-anterior and the distal anterolateral (DALA) portal is progressively more posterior [30]. Although anchor trajectory improves with these portals, occasional obstruction by the femoral head occurs, especially with the DALA portal [27]. The modified mid-anterior portal may be the best compromise. However, one case of anchor-induced chondral damage did occur using this portal so no portal may be infallible. Some surgeons may also use percutaneous accessory portals to improve the trajectory for suture anchor placement. Suggested preventative measures based upon our collective experience, preference and opinions are listed in Tables IV and V.
Table IV.
Suggested preventative techniques
| Distal portal (e.g. MAP, MMAP, DALA) |
| Clear rim of obstructing capsule and synovium |
| Pilot hole (microfracture awl) |
| Zone-specific drilling (see Table V) |
| Visualize from central compartment during drilling and anchor placement |
| Listen for change in drill sound |
| Feel for increase drill resistance if engage subchondral bone |
| Extra caution at 3 o’clock (direct anterior) rim and/or thin articular cartilage |
| Rim trimming |
| Soft (e.g. suture-based) anchors |
| Small diameter anchors |
| Short anchors |
| Increasing radius of curvature of curved anchor systems |
MAP, mid-anterior portal, MMAP, modified mid-anterior portal, DALA, distal anterolateral accessory.
Table V.
Zone-specific chondrophobic acetabular rim drilling*
| Anterior zone | Drill path parallel to floor |
| Superior zone | Fluoroscopic divergent drill path |
| Posterior zone | Divergent drill path** |
*via mid-anterior or modified mid-anterior portal. **The posterior-most drill site is the most challenging and should be done before the final drill site. If done as the final drill site, anchor spacing may dictate that far-posterior drilling is done in a region most susceptible to posterior wall fracture with compromised labral refixation.
The margin of error (i.e. safety angle) for anchor placement increases with rim trimming, smaller diameter, shorter or soft suture-based anchors and greater radius of curvature of curved anchor systems [31, 32]. Moreover, the direct anterior or 3 o’clock rim position had the least tolerance to errant drilling/anchor placement [32]. This case series did not have any anchors placed at 3 o’clock; the 1 o’clock position was most commonly associated with this complication. If an anchor can be acceptably placed at 2 o’clock rather than 3 o’clock, especially after rim trimming in appropriate cases, risk of anchor-induced chondral damage may be lessened. Furthermore, in areas with thin articular cartilage, one may consider small and/or soft anchor options.
Another preventative measure is sufficient clearance of capsular and synovial tissues from the area of planned anchor fixation. Beyond using a shaver, a radiofrequency wand and/or burr in reverse spin may aid this process, permitting improved arthroscopic visualization for accurate drill hole and anchor placement close to but not in violation of the articular cartilage. A tip is to make a shallow divot with a microfracture awl at the desired rim starting point so that the subsequent drill tip does not wander from its intended starting point.
Rim preparation may be done with zone-specific chondrophobic drilling (Table V) [27, 33]. At the superolateral rim or 12 o’clock position, two-dimensional AP fluoroscopic spot imaging can confirm a drill path engaging bone while diverging from the articular cartilage. Desiring suture anchor placement close to but not in violation of the acetabular articular cartilage, the anterior drill hole(s) are made with the drill positioned parallel to the floor. If pelvic orientation has been standardized at the onset of surgery (e.g. using the fluoroscopic templating technique) [34], anterior chondral damage may be avoided even at the narrow 3 o’clock position. Arthroscopic visualization of the adjacent acetabular cartilage from the central compartment (with hip distraction) while engaging tactile and auditory senses to detect even subtle changes during drill advancement (which might be an indicator of subchondral bone encroachment or penetration) encourages safe anterior suture anchor placement. For the posterior rim, the drill path is inherently chondroprotective when done via the MAP or MMAP; by nature of its posterior vector, drill trajectory diverges from the posterior chondral surface. However, the posterior rim may be particularly thin and posterior wall ‘blow-out’ with compromised anchor fixation may occur [27, 33].
Curved or angled anchor guides, drills and inserters may aid safe anchor placement. A recent study has demonstrated improved divergence from the chondral surface compared with a straight guide [30]. Interestingly, whereas curved systems may be utilized so as to diverge from the adjacent acetabular cartilage surface, they may be used in a convergent manner (aimed anteriorly) to avoid posterior wall blowout when performing posterior labral repair or reconstruction [27, 33].
Recent studies on acetabular safe angles of anchor insertion have demonstrated a wider margin of safety for acetabular suture anchor placement with shorter drill depths, smaller drill diameters, rim trimming and curved guides [31, 32]. Hence, future technical and equipment developments may incorporate some or all of these findings.
Soft suture-based deforming anchors offer an alternative to hard non-absorbable or bioabsorbable suture anchors. We have successfully used soft anchors for labral refixation and labral reconstruction. The small diameter (1.4 and 1.5 mm) drills with short drill depths and short deployed implants near the peripheral rim permit anchor placement in desired proximity to the chondral surface while maximizing the margin of safety. Furthermore, the flexible nitinol wire permits drilling via curved guides. By aiming the curved guide away from the acetabular articular cartilage during rim preparation, suture anchor fixation may occur in desired proximity to the osteochondral junction while diverging from the cartilage for safe anchor placement [27, 30]. If this anchor detaches or violates the joint, the likelihood of degenerative damage to the femoral head may be less because of the deforming nature of these small soft implants. Finally, computer-assisted navigation may also play a future role in safe drilling and anchor placement.
Two of the five cases did not have confirmatory documentation of anchor-induced chondral damage (Cases 4 and 5). This may have been from non-recognition or non-reporting. Because of the potential for severe degenerative consequences from this complication, and because modified post-operative rehabilitation and close monitoring may be beneficial, we strongly encourage surgeons to be cognizant of this complication, employ aforementioned techniques to minimize its occurrence, remove offensive anchors when prudent, accurately document and inform the patient.
Limitations
Limitations of this case series include the lack of a control group and the inability to apply valid statistical analysis given the small number of patients and inconsistent hip score instruments. Although two patients with chondral deformation are doing well at 2 and 6 years, a larger long-term controlled study is needed to determine the durability of clinical improvement and to substantiate conclusions in this subtype.
CONCLUSION
Anchor-induced chondral deformation without frank chondral penetration may be treated with close clinical and radiographic monitoring with a low threshold for revision surgery and anchor removal. Chondral penetration should be treated with immediate removal of offending hard anchor implants. Preventative measures include distal-based portals, small diameter and short anchors, removable hard anchors, soft suture-based anchors, curved drill and anchor insertion instrumentation and attention to safe trajectories while visualizing the acetabular articular surface.
REFERENCES
- 1.Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res 2007; 465:16–22. [DOI] [PubMed] [Google Scholar]
- 2.Ferguson SJ, Bryant JT, Ganz R, et al. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech 2003; 36: 171–8. [DOI] [PubMed] [Google Scholar]
- 3.Haemer JM, Carter DR, Giori NJ. The low permeability of healthy meniscus and labrum limit articular cartilage consolidation and maintain fluid load support in the knee and hip. J Biomech 2012; 45: 1450–6. [DOI] [PubMed] [Google Scholar]
- 4.Song Y, Ito H, Kourtis L, et al. Articular cartilage friction increases in hip joints after the removal of acetabular labrum. J Biomech 2012; 45: 524–30. [DOI] [PubMed] [Google Scholar]
- 5.Matsuda DK, Carlisle JC, Arthurs SC, et al. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy 2011; 27: 252–69. [DOI] [PubMed] [Google Scholar]
- 6.Botser IB, Smith TW, Nasser R, et al. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy 2011; 27: 270–78. [DOI] [PubMed] [Google Scholar]
- 7.Espinosa N, Rothenfluh DA, Beck M, et al. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am 2006; 88: 925–35. [DOI] [PubMed] [Google Scholar]
- 8.Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med 2012; 40: 1015–21. [DOI] [PubMed] [Google Scholar]
- 9.Krych AJ, Thompson M, Knutson Z, et al. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy 2013; 29: 46–53. [DOI] [PubMed] [Google Scholar]
- 10.Haddad B, Konan S, Haddad FS. Debridement versus re-attachment of acetabular labral tears: a review of the literature and quantitative analysis. Bone Joint J 2014; 96: 24–30. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda DK, Burchette RJ. Arthroscopic hip labral reconstruction with a gracilis autograft versus labral refixation: 2-year minimum outcomes. Am J Sports Med 2013; 41: 980–7. [DOI] [PubMed] [Google Scholar]
- 12.Matsuda DK. Arthroscopic hip labral reconstruction: graft choices, techniques, and advances. Tech Orthop 2012; 27: 184–92. [Google Scholar]
- 13.Geyer MR, Philippon MJ, Fagrelius TS, et al. Acetabular labral reconstruction with an iliotibial band autograft: outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med 2013; 41: 1750–6. [DOI] [PubMed] [Google Scholar]
- 14.Domb BG, El Bitar YF, Stake CE, et al. Arthroscopic labral reconstruction is superior to segmental resection for irreparable labral tears in the hip: a matched-pair controlled study with minimum 2-year follow-up. Am J Sports Med 2014; 42: 122–30. [DOI] [PubMed] [Google Scholar]
- 15.Boykin RE, Patterson D, Briggs KK, et al. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med 2013; 41: 2296–301. [DOI] [PubMed] [Google Scholar]
- 16.Kelly BT, Weiland DE, Schenker ML, et al. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy 2005; 21: 1496–504. [DOI] [PubMed] [Google Scholar]
- 17.Philippon MJ, Schroder e Souza BG, Briggs K. Labrum: resection, repair and reconstruction sports medicine and arthroscopy review. Sports Med Arthrosc 2010; 18: 76–82. [DOI] [PubMed] [Google Scholar]
- 18.Athwal GS, Shridharani SM, O’Driscoll SW. Osteolysis and arthropathy of the shoulder after use of bioabsorbable knotless suture anchors: a report of four cases. J Bone Joint Surg Am 2006; 88: 1840–5. [DOI] [PubMed] [Google Scholar]
- 19.Kaar TK, Schenck RC, Jr, Wirth MA, et al. Complications of metallic suture anchors in shoulder surgery: a report of 8 cases. Arthroscopy 2001; 17: 31–7. [DOI] [PubMed] [Google Scholar]
- 20.Levy JC, Virani NA, Frankle MA, et al. Young patients with shoulder chondrolysis following arthroscopic shoulder surgery treated with total shoulder arthroplasty. J Shoulder Elbow Surg 2008; 17: 380–8. [DOI] [PubMed] [Google Scholar]
- 21.Pateder DB, Park HB, Chronopoulos E, et al. Humeral head osteonecrosis after anterior shoulder stabilization in an adolescent. J Bone Joint Surg Am 2004; 86: 2290–3. [DOI] [PubMed] [Google Scholar]
- 22.Sassmannshausen G, Sukay M, Mair SD. Broken or dislodged poly-l-lactic acid bioabsorbable tacks in patients after SLAP lesion surgery. Arthroscopy 2006; 22: 615–9. [DOI] [PubMed] [Google Scholar]
- 23.Harris JD, McCormick FM, Abrams GD, et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy 2013; 29: 589–95. [DOI] [PubMed] [Google Scholar]
- 24.Chan K, Farrokhyar F, Burrow S, et al. Complications following hip arthroscopy: a retrospective review of the McMaster experience (2009–2012). Can J Surg 2013; 56: 422–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clarke MT, Villar RN. Hip arthroscopy: complications in 1054 cases. Clin Orthop 2003; 406: 84–8. [DOI] [PubMed] [Google Scholar]
- 26.Kowalczuk M, Bhandari M, Farrokhyar F, et al. Complications following hip arthroscopy: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2013; 21: 1669–75. [DOI] [PubMed] [Google Scholar]
- 27.Matsuda DK, Villamor A. The modified midanterior portal for hip arthroscopy. Arthrosc Tech 2014; 3: e469–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grutter PW, McFarland EG, Zikria BA, et al. Techniques for suture anchor removal in shoulder surgery. Am J Sports Med 2010; 38: 1706–10. [DOI] [PubMed] [Google Scholar]
- 29.Freehill MT, Safran MR. The labrum of the hip: diagnosis and rationale for surgical correction. Clin Sports Med 2011; 30: 293–315. [DOI] [PubMed] [Google Scholar]
- 30.Nho SJ, Freedman RL, Federer AE, et al. Computed tomographic analysis of curved and straight guides for placement of suture anchors for acetabular labral refixation. Arthroscopy 2013; 29: 1623–7. [DOI] [PubMed] [Google Scholar]
- 31.Lertwanich P, Ejnisman L, Torry MR, et al. Defining a safety margin for labral suture anchor insertion using the acetabular rim angle. Am J Sports Med 2011; 39(Suppl): 111S–6S. [DOI] [PubMed] [Google Scholar]
- 32.Hernandez JD, McGrath BE. Safe angle for suture anchor insertion during acetabular labral repair. Arthroscopy 2008; 24: 1390–4. [DOI] [PubMed] [Google Scholar]
- 33.Matsuda DK, Hanami D, Gupta N. Hip arthroscopy for challenging deformities: global pincer femoroacetabular impingement. Arthrosc Tech 2013; 2: e45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matsuda DK. Fluoroscopic templating technique for precision arthroscopic rim trimming. Arthroscopy 2009; 25: 1175–82. [DOI] [PubMed] [Google Scholar]