Abstract
Labral hypertrophy is a distinct feature in hip dysplasia. Occasionally, very small, hypotrophic labra are observed. However, there is no literature concerning this pathology. We investigated if the size of the labrum correlated with any radiologic parameters reflecting the amount of acetabular coverage. It was hypothezised that there is a negative correlation between labrum size and acetabular coverage. Labra were categorized into three groups depending on the relation between length of the articular sided surface and height of bony attachment. Labra with a height:length ratio of 2 were classified as hypotrophic, with a height:length ratio of 1 as normal and with a ratio of 0.5 as hypertrophic. Labral cross-sectional areas (CSA) were measured on radial magnetic resonance imaging-arthrography slices using the measuring tool of the PACS system of 20 hips with hypotrophic labra (group 1), 20 hips with normal labral appearance (group 2) and 10 hips with hypertrophic labra (group 3). These values were then analyzed against following parameters: neck-shaft-angle (NSA), lateral center-edge angle (LCE), acetabular index (AI), femoral extrusion index (FEI) and acetabular retroversion index (ARI). Analyses of variance were used to determine differences in mean values between the three groups. Mean labral CSA differed significantly between all groups (group 1: 12.1 ± 2.9 mm2; group 2: 25.2 ± 6.2 mm2; group 3: 41.1 ± 12.3 mm2; P < 0.001). NSA, LCE, AI and FEI all showed a significant difference between group 3 and 1 or 2. The ARI showed no difference between groups. Stepwise linear regression analyses showed a significant correlation between LCE angle and labral CSA with a corrected R2-value of 0.301. Labral CSA correlates with the LCE. No statistically significant difference between groups 1 and 2 concerning the LCE, AI or FEI could be identified. Nevertheless, group 1 had the highest mean coverage of all groups, hips with hypertrophic labra the lowest.
INTRODUCTION
The normal acetabular labrum acts as an extension of the articular surface of up to 27%, increasing acetabular volume by up to 30%, providing a seal-effect that resists distraction of the femoral head and enhances joint stability [1–4]. Furthermore, it inhibits the synovial fluid from extruding the central compartment under load, thus ensuring an equally distribution of forces across the joint cartilage and minimizing rotational friction forces [5–10]. The labral blood supply derives from radial branches of a periacetabular vascular ring, which is mainly fed by the superior and inferior gluteal arteries, with minor contributions from the medial and lateral circumflex femoral arteries and intrapelvic vessels [11]. This blood supply enables healing of the labrum after tearing or repair, as described by Audenaert et al. [12]. Nerve supply has also been reported with free nerve endings and receptors found in histological examinations, thus explaining labral pathology to cause painful symptoms [13, 14].
Several studies have shown that acetabular labra in dysplastic hips are larger than in normal control groups or in hips with femoro-acetabular impingement (FAI) [15–20]. Higher load- and shear forces at the labro-acetabular-interface due to an insufficient bony femoral coverage and thus transition of the femoral head center towards the acetabular rim are thought to lead to a compensatory labral hyperplasia as an attempt to stabilize the unstable hip joint [21].
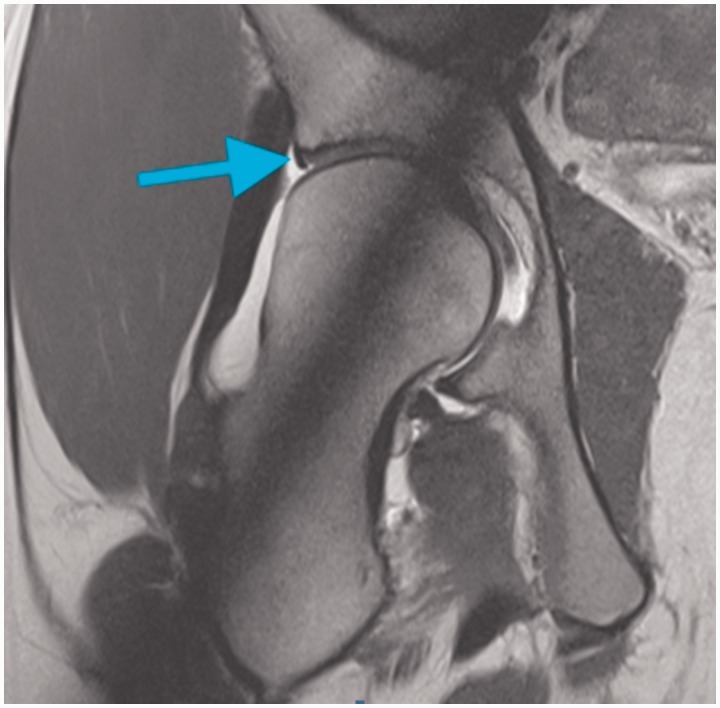
Occasionally, very small, hypotrophic labra are observed in young patients, but there is a lack of information in the literature about this condition (Fig. 1).
Fig. 1.
MR-arthrography showing a hypotrophic labrum (arrow) in the anterosuperior area of the acetabulum.
Of interest may be, that hips with small labra do not have a suction seal during surgical dislocation of the femoral head, which is normally present in hips with a normal labrum [22, 23].
Up to date, there is no definition of labrum size being small, normal or hypertrophic. Several studies described the different magnetic resonance imaging (MRI) appearance of the acetabular labrum [24–28]. Most asymptomatic labra were found to have a triangular cross section (66–80%); apart from that, round (11–16%), flat (9–13%), or irregular contours were recorded. Some studies also described hypoplastic labra or even an absence (1–3% and up to 14%, respectively) [24–28]. Labral absence was only observed in patients over 50 years of age and is likely to be a result of natural degeneration during aging or progressive ossification of the labrum [27, 29]. Unfortunately, the true cross-sectional or volumetric size of the different labra have not been determined, and there has not been any effort so far to correlate the different shapes or sizes to the bony anatomy of the patients.
Our goal was to determine (i) the labral cross-sectional area (CSA) circumferentially around the acetabulum on radial MR arthrography and (ii) find out if there is any anatomical difference between the groups with respect to acetabular coverage and shape of the femoral head neck junction. It was hypothesized that hips with hypotrophic labra have more bony acetabular coverage than hips with normal or hypertrophic labra.
MATERIALS AND METHODS
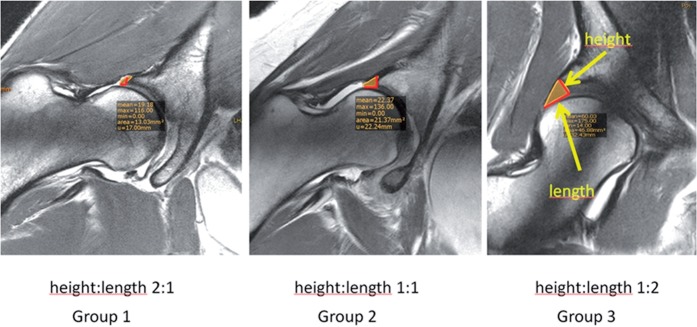
The MR-arthrographies of all patients attending our clinic between 2008 and 2013 were scrutinized for the size of the labrum and categorized into three groups. Categorization was based on the relation of height and length, height being the distance of the attachment measured from the joint surface to the perilabral recess and length the distance from the chondrolabral junction to the tip of the labrum (Fig. 2). For categorization, the size of the labrum was measured at the lateral acetabular rim on a frontal plane through the center of the femoral head. A labrum was considered hypotrophic when its length was less than half the height, normal when length and height were approximately equal and large when length was twice as large as the height. The categorization into 2:1, 1:1 and 1:2 automatically lead to a gap between the sizes which helped to obtain unambiguous, non-overlapping data. For groups 1 and 2, 20 hips were selected from the initial cohort according to the in-/exclusion criteria mentioned below. Because of the uniformity of the values in the large labrum group, all showing acetabular dysplasia, the analysis was discontinued after ten hips.
Fig. 2.
Categorization of the labra.
Inclusion criteria were a standardized anterior-posterior radiograph of the pelvis according to Siebenrock et al. [30] and closed physes on MRI (for cam deformity determination), as development of the cam-deformity is thought to take place during physeal closure [30, 31]. Exclusion criteria were lack of radial MR slices, inappropriate radiographs, severe labral changes on MRI (signal alterations Czerny 1B or higher, ganglia, ossifications, tears) in >50% of slices measured, and history of previous hip surgery, trauma or infection [32].
MRI’s were obtained as follows: Intraarticular injection of contrast material with fluoroscopic guidance was performed prior to the MR examination in a standardized fashion in the radiology department. One to two milliliters of a local anaesthetic (lidocaine hydrochloride 10 mg/ml 1%, Rapidocain, Sintetica, Mendrisio, Switzerland), 1–2 ml of iodinated contrast media (Iopamiro 300, Bracco, Milano, Italy) and approximately 10 ml of MR contrast agent (gadoteric acid, 0.0025 mmol/ml, Artirem, Guerbet, Villepinte, France) were applied. MR images were obtained on a 3 Tesla scanner (Achieva 3.0T; Philips Healthcare, Best, The Netherlands) with a six-channel SENSE cardiac coil (Philips Healthcare, Best, The Netherlands).
The routine protocol for MR arthrography included a transverse T1-weighted turbo spin-echo sequence, a coronal and sagittal intermediate-weighted turbo spin-echo sequence, a radial intermediate-weighted turbo spin-echo sequence, a transverse THRIVE (T1-weighted high resolution isotropic volume examination) or DESS (dual-echo steady state) sequence and a rapid transverse T1-weighted sequence over the proximal and distal femur for antetorsion measurement.
The radial sequence was planned on a scout image perpendicular to the long axis of the femoral neck using the center of the femoral neck as the axis of rotation, with a section thickness of 4 mm, which led to 25 slices.
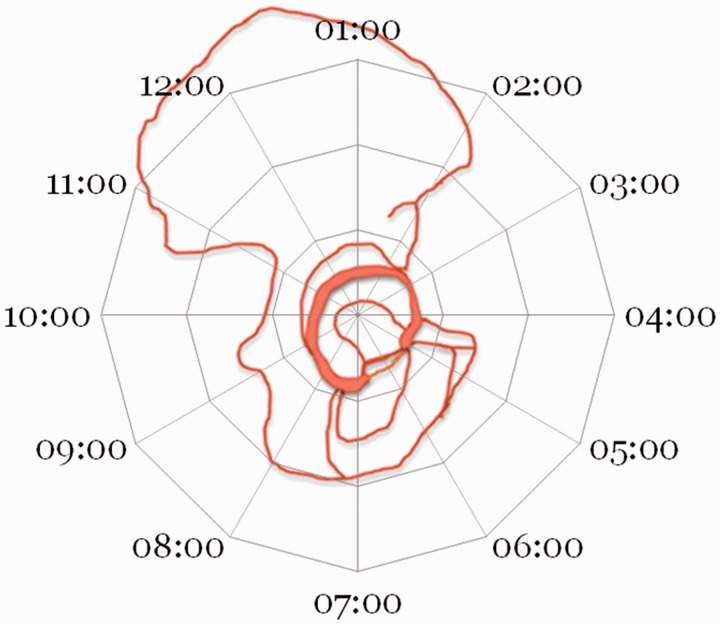
For analysis only the 12 values corresponding to the clock system were used, 12 o’clock position being superior, 3 o’clock anterior, 6 o’clock inferior (transverse ligament) and 9 o’clock posterior (Fig. 3). For easier analysis and presentation, the data of the left hips were converted into right hips and presented in a clockwise fashion.
Fig. 3.
Clockwise orientation of the analized planes around the acetabulum.
The CSA of the labrum was measured on the radial images at each position around the acetabulum, except in the area of the transverse ligament, using the area-measuring-tool of the PACS-System-software (Phönix Merlin PACS, Phönix-PACS GmbH, Emmy-Noether-Straße 2, D-79110 Freiburg). At each position the mean area (±SD) was calculated and analysed. Differences of labral size at each of the positions were compared between the groups. In a second step, the mean circumferential CSA-values of the labrum for each group were averaged.
Changes of the acetabular rim and labrum were also recorded (labral base ossfications, ganglia, signal alterations and tears). To assess the presence of a cam deformity, the asphericity of the head neck junction was measured using the alpha angle as described by Nötzli at the 3 o’clock position and the asphericity angle at the 1:30 position as recommended by Rakhra and Pfirrmann [33–35]. The cutoff value for the angle of asphericity, representing a cam deformity, was set at 55° according to recent recommendations [36, 37].
Pelvic radiographs for each patient were analysed and the neck-shaft-angle (NSA), the lateral center-edge-angle (LCE), the acetabular index (AI) and the femoral extrusion index (FEI) were recorded [38–50]. Radiological signs of acetabular retroversion [crossing sign, posterior wall sign, ischial spine sign and acetabular retroversion index (ARI)] were also recorded [51, 53]. All measurements were done on the PACS-software (Phönix Merlin PACS, Phönix-PACS GmbH, Emmy-Noether-Straße 2, D-79110 Freiburg).
Statistical analyses were performed with IBM SPSS software program (version 20.1). Analyses of variance were used to determine differences in mean values between the three groups concerning all measured items, including post hoc Bonferroni correction. Simple and multivariate linear regression analyses were performed to investigate a correlation between the measured parameters and labral volume. Level of significance was set at P < 0.05.
RESULTS
Group 1 includes 20 hips with a very small (hypotrophic) labrum, group 2 includes 20 hips with normal labrum and group 3 includes 10 hips with a large labrum. There was no significant difference concerning mean age, although the average age in group 1 was slightly younger than in the other two groups (1:2: P = 0.213/1:3: P = 0.382/2:3: P = 1.0). There was no gender difference between group 1 and 2; however, there was a clear preponderance for female hips in the hypertrophic group. Patient characteristics are shown in Table I.
Table I.
Demographics of the patients of the three groups
| Male | Female | n | Mean age | |
|---|---|---|---|---|
| Hypotrophic | 7 | 13 | 20 | 22.7 (15–31, ±4.6) |
| Normal | 6 | 14 | 20 | 26.2 (16–35, ±6.6) |
| Hypertrophic | 2 | 8 | 10 | 26.3 (17–40, ±7.1) |
| Σ = | 15 | 35 | 50 | 25.1 (15–40, ±6.1) |
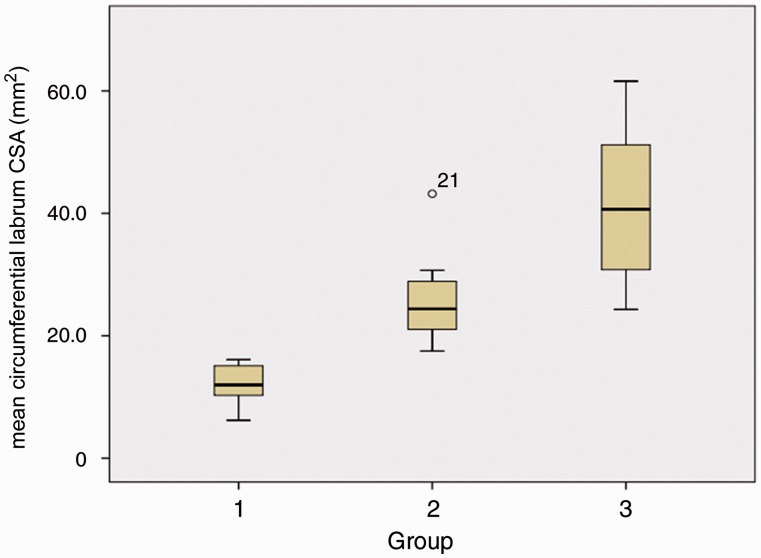
Mean overall labral CSA differed significantly (1:2: P < 0.001; 1:3: P < 0.001; 2:3: P < 0.001) between all groups (Table IV and Fig. 4).
Table IV.
Overview of the different radiographic parameters in relation to the three groups
| G1: hypotrophic | G2: normal | G3: hypertrophic | P value (1:2/1:3/2:3) | |
|---|---|---|---|---|
| Mean labrum CSA (range) | 12.1 ± 2.9 mm2 (6.2–16.1) | 25.2 ± 6.2 mm2 (17.5–43.2) | 41.1 ± 12.3 mm2 (24.3 to 61.6) | <0.001 |
| NSA | 134 ± 6.8 | 132 ± 5.9 | 140 ± 7.9 | 0.7/0.107/0.009 |
| LCE | 30.2 ± 5.2 | 27.6 ± 6.6 | 11 ± 5.2 | 0.827/0.001/0.001 |
| AI | 3.3 ± 5.2 | 4.7 ± 4.2 | 16.3 ± 9 | 1.0/0.001/0.001 |
| FEI | 17 ± 7.2 | 19 ± 5.9 | 33.9 ± 12.6 | 1.0/0.001/0.001 |
| Angle alpha (3 o’clock) | 43.5 ± 5.6 | 48.8 ± 8.4 | 48.4 ± 6.8 | 0.064/0.234/1.000 |
| Asphericity angle (1’30 o’clock) | 46.2 ± 6.9 | 54.8 ± 13.1 | 46 ± 8.9 | 0.031/1.000/0.094 |
Fig. 4.
Boxplot of the size of the labrum of the three groups. 1) hypotrophic, 2) normal, 3) hypertrophic.
In group 1 the averaged mean CSA over all clock positions was 12.1 ± 2.9 mm2 (range 6.2–16.1 mm2), in group 2 it measured 25.2 ± 6.2 mm2 (range 17.5–43.2 mm2) and in group 3 it was 41.1 ± 12.3 mm2 (range 24.3–61.6 mm2). The lowest single CSA value measured was 1.4 mm2 in group 1, the highest 94.6 mm2 in group 3. The mean size in mm2 and distribution of the cross sectional area of the labrum around the circumference are presented in Table II and Fig. 5.
Table II.
Size of the labrum in mm2 at the various clock positions. At 6:00 is the transverse ligament, therefore no data was available
| Position | Hypotrophic | Normal | Hypertrophic | P value (1:2/1:3/2:3) |
|---|---|---|---|---|
| 12:00 | 14.4 ± 5 | 23 ± 5.3 | 42.4 ± 7.7 | 0.0001/0.0001/0.0002 |
| 01:00 | 11.5 ± 6.2 | 22.4 ± 9.3 | 36.1 ± 13.7 | 0.0002/0.0001/0.002 |
| 02:00 | 9.6 ± 4.4 | 19.9 ± 10.6 | 24.2 ± 16 | 0.003/0.002/0.035 |
| 03:00 | 15 ± 6 | 19.8 ± 5.8 | 22.7 ± 9.4 | 0.037/0.008/0.078 |
| 04:00 | 13.1 ± 4.9 | 18.4 ± 6.4 | 29.6 ± 1.7 | 0.19/0.045/0.075 |
| 05:00 | 14 ± 4.8 | 17 ± 6.9 | 38.8 ± 2.6 | 0.27/0.0007/0.0012 |
| 06:00 | 0 | 0 | 0 | |
| 07:00 | 8.7 ± 2.8 | 13 ± 1.3 | 22.1 ± 9.4 | 0.028/0.0045/0.05 |
| 08:00 | 10.3 ± 2.1 | 14.1 ± 4.3 | 18.8 ± 5.6 | 0.008/0.0014/0.09 |
| 09:00 | 13 ± 4.4 | 15.8 ± 4.9 | 30.4 ± 12.1 | 0.11/0.003/0.009 |
| 10:00 | 16.1 ± 7.7 | 19.1 ± 6.6 | 32.8 ± 10.5 | 0.35/0.004/0.008 |
| 11:00 | 19.6 ± 5.6 | 22.7 ± 4 | 34.4 ± 17.3 | 0.079/0.0006/0.0016 |
Fig. 5.
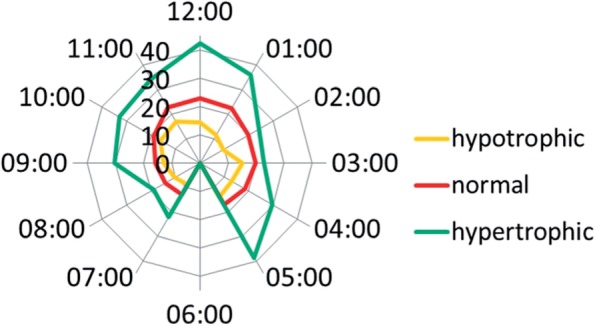
Schematic representation of the size of the labrum for hypotrophic, normal and hypertrophic labra (in mm2).
The mean NSA was significantly higher (P < 0.009) in group 3 compared with group 2. No significant difference was found between group 1 and 3 (P < 0.107) or 1 and 2 (P < 0.7). The lowest NSA was 121° measured in group 2, and the highest 156° in group 3.
The mean LCE was significantly lower (P < 0.001) in group 3 than in the two other groups. The highest value measured was 40° in group 1, and the lowest −17° in group 3. No significant difference was found between groups 1 and 2 (P = 0.827).
The mean AI was also significantly higher (P < 0.001) in the dysplastic hips group than in group 1 or group 2. Again, group 1 and 2 did not differ significantly. The lowest AI-value measured was −8.8° in group 1, and the highest 30.6° in group 3.
The mean FEI was significantly higher (P < 0.001) in group 3 compared with the other groups. Once more, no significant difference was found between group 1 and 2. Sixty-three percent in group 3 was the highest value measured, 0% in group 1 the lowest.
The radiographic parameters are summarized in Table IV.
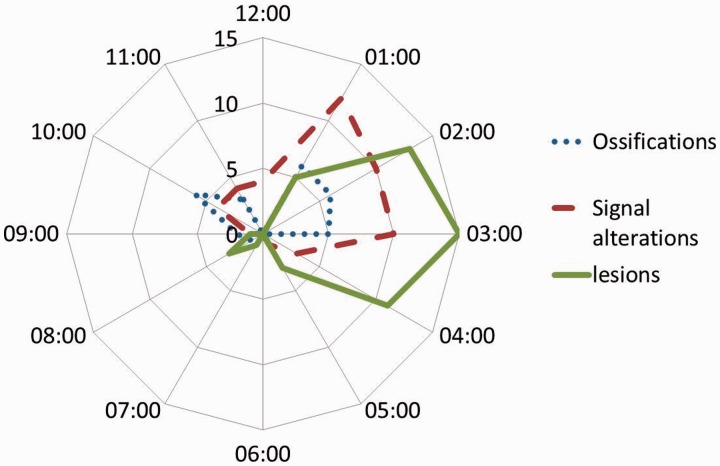
Most labral disorders were found between 1 and 4 o’clock, representing the antero-superior quadrant. Ossifications were found more often in the hypoplastic group (20 slices versus 9 slices versus 1 slice) while signal alterations and lesions were equally distributed. The distribution of labral disorders is shown in Fig. 6.
Fig. 6.
Distribution of labral disorders.
Signs of acetabular retroversion (ARI > 20%) were seen in five hips in group 1 (25%) versus five hips in group 2 (25%) versus two hips in group 3 (20%) (Table III) [51–53].
Table III.
Presence of acetabular retroversion and cam deformity within the three different groups
| Acetabular retroversion | Cam | |
|---|---|---|
| Hypotrophic | 5 (25%) | 0 |
| Normal | 5 (25%) | 11 (55%) |
| Hypertrophic | 3 (30%) | 4 (40%) |
A cam-deformity was found in none of the hips in group 1 (0%), in 11 hips of group 2 (55%) and in 4 hips in group 3 (40%). The absence of a cam deformity at the 01:30 position was statistically significant (P = 0.031). No difference between groups was observed concerning the alpha-angle at 03:00 (Tables III and IV).
Multivariate regression analyses showed a significant correlation between all radiographic parameters (NSA, LCE, AI and FEI) and overall mean labral CSA with a corrected R2 value of 0.278. Simple linear regression analyses showed a significant correlation between LCE value and overall mean labral CSA (P < 0.001) with a corrected R2-value of 0.301.
DISCUSSION
Our study aimed to investigate if hips with hypotrophic labra have deeper hips with more bony acetabular coverage, so that the small size could be explained as a consequence of increased coverage and thus decreased forces acting at the labro-acetabular-interface, possibly thereby disincentivizing the labrum to further hypertrophy during its development. According to our data, this hypothesis could not be confirmed in means of statistical significant differences in bony morphology between groups 1 and 2. Statistical regression analyses showed a weak but significant correlation between LCE and mean labral CSA. Interestingly, the group with the hypotrophic labra did not reveal any cam-deformities, speaking in favor of an isolated pincer-FAI. Acetabular retroversion did not have an influence on labrum size and was equally distributed among all groups.
A study by Cobb et al. [54] showed a difference in bony acetabular morphology between Pincer- and Cam-type hips. They found Cam-type hips to be shallower than normal hips, which in turn were again shallower than Pincer-type hips [54]. In how far this circumstance has an influence on labral morphology was not reported.
A study by Corten et al. [29] showed that in ‘deep’ hips, an existing pincer impingement leads to a bony apposition at the acetabular rim, which displaces the labrum, mimicking a small or absent labrum on MR imaging [29]. The study population though was older than ours (mean 41.9 years for tissue sample group), and patients with ossifications were significantly older than those without (43 years versus 33 years). In our study, we could not identify any labral or acetabular rim ossifications on the AP radiographs, whereas scrutinizing the MRI’s revealed some ossifications as described by Corten et al. [29] but there were also hypotrophic labra without any signs of acetabular rim changes or signal alterations. In addition, also dysplastic hips and hips with normal acetabular labrum showed these ossifications.
As the labrum is thought to have several biomechanical functions, the capability to accomplish these is likely to depend on its integrity and also on its size.
It is questionable in how far the hypotrophic labra are able to perform the assigned biomechanical function of a seal. Patients with hypotrophic labra do not show a vacuum effect while performing a surgical dislocation of the hip, suggesting an insufficient or at least remarkably diminished sealing effect.
Assumed that a hypotrophic labrum is not able to maintain the synovial liquid in the central compartment at loadbearing, higher forces distributed across the cartilage would be the consequence, thus enhancing cartilage and joint degeneration. This would mean that in hips with a hypotrophic labrum osteoarthritis would develop earlier, however, up to date, there is no data confirming a correlation between labral absence and earlier onset of osteoarthritis or FAI.
Most studies mentioning the normal thickness of a labrum being 2–3 mm refer to an article by Barham S. who does not outline the source of this statement [55]. The indicated sources, to our knowledge, do not contain information about the labrum thickness [13, 56]. Aydingöz and Oztürk examined the labra of 180 asymptomatic volunteers in five age groups on MR-scans [25]. They found above mentioned labrum shapes and a size difference of over 25% between left and right hips in the same patients in one-fourth of volunteers. Average labrum area was mentioned to range between 7.8 and 13.5 mm2, but the labra were indirectly measured only on midcoronal slices at the largest appearance using different formulas to determine the area according to its shape. Another effort to evaluate labral size was made by Kantarci et al. [57], measuring the cross sectional area of labra by ultrasound visualization. Again, the CSA was measured only on one single ultrasound image considered to display best the largest area of the labrum. Few cadaver studies mentioned the height of the labrum at certain points ranging from 1 to 33.6 mm (mean 5.9 mm) [14, 58]. Won et al. [58] also distinguished four types of shapes of labra and attachments to the acetabulum in their cadaveric study. They described small labra mainly in the posterior and inferior parts of the acetabulum with an incidence of 6.9%.
The small labra in our study showed a more or less circumferentially hypotrophic appearance, especially in the superior parts. In order to gain complete information about the acetabular shapes and corresponding labral CSA or volumes, combined 3D computed tomography and radial—MRI would be favorable.
Radial MR-arthrography has been described as the best method to detect labral pathology, and, in addition, is capable of showing the labrum circumferentially in its cross section [59–65].
The radiological parameters were chosen because of their reliability to show the degree of acetabular coverage of the femoral head, respectively, the acetabular depth. NSA were gained to determine if coxa valga had also influence on the labrum size, as this pathology leads to additionally increased loading forces on the superoanterior rim in dysplastic hips [39, 40, 43–46, 50].
The difficulty to recruit convenient MRI is the main reason for the small number of patients included in our study. Most patients who undergo arthro-MRI for the hip show labral changes such as signal alterations, ganglia, tears, cysts etc. even at young ages. As labrum MRI signals and labrum forms change during aging, only young patients with almost no symptoms are likely to have an intact labrum, which can be measured circumferentially [24–28]. The prevalence of labral pathology on MRI among 45 asymptomatic young participants was reported to be as high as 69%, underlining above mentioned problem [66]. Furthermore, finding intact hypotrophic and/or hypertrophic labra is an even harder challenge.
Another limitation of our study is selection bias, as our study population was recruited from symptomatic young patients attending our clinic and not from asymptomatic volunteers. In addition, our study population is not representative for the general public due to the selection process (estimated height:length-ratio). In order to determine the normal distribution of labrum sizes for categorization of small, normal or hypertrophic labra, either prospective or cross-sectional studies would be necessary with representative study populations.
CONCLUSION
Labral CSA correlates with the LCE. No statistically significant difference between hips with normal labra and hypotrophic labra concerning the radiological parameters reflecting the amount of acetabular coverage could be identified. However, the absence of a cam deformity leads to the conclusion, that hypotrophic labra are predominantly found in pure pincer FAI. Nevertheless, the group with the hypotrophic labra had the highest mean coverage of all groups, the dysplastic group the lowest. Probably a higher number of patients is necessary to yield a significant difference between groups 1 and 2.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Tan V, Seldes RM, Katz MA, et al. Contribution of acetabular labrum to articulating surface area and femoral head coverage in adult hip joints: an anatomic study in cadavera. Am J Orthop 2001; 30: 809–12. [PubMed] [Google Scholar]
- 2.Takechi H, Nagashima H, Ito S. Intra-articular pressure of the hip joint outside and inside the limbus. Nippon Seikeigeka Gakkai Zasshi 1982; 56: 529–36. [PubMed] [Google Scholar]
- 3.Terayama K, Takei T, Nakada K. Joint space of the human knee and hip joint under a static load. Eng Med 1980; 9: 67–74. [Google Scholar]
- 4.Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res 2007; 465:16–22. [DOI] [PubMed] [Google Scholar]
- 5.Song Y, Safran M, Ito H, et al. Articular cartilage friction increases in hip joints after partial and total removal of the acetabular labrum . J Biomech 2012; 45: 524–30. [DOI] [PubMed] [Google Scholar]
- 6.Ferguson SJ, Bryant JT, Ganz R, et al. The acetabular labrum seal: a poroelastic finite element model. Clin Biomech 2000; 15: 463–8. [DOI] [PubMed] [Google Scholar]
- 7.Field RE, Rajakulendran K. The labro-acetabular complex. J Bone Joint Surg Am 2011; 93(Suppl 2): 22–7. [DOI] [PubMed] [Google Scholar]
- 8.Cadet ER, Chan AK, Vorys GC, et al. Investigation of the preservation of the fluid seal effect in the repaired, partially resected, and reconstructed acetabular labrum in a cadaveric hip Model. Am J Sports Med 2012; 40: 2218–23. [DOI] [PubMed] [Google Scholar]
- 9.Ferguson SJ, Bryant JT, Ganz R, et al. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech 2000; 33: 953–60. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson SJ, Bryant JT, Ganz R, et al. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech 2003; 36: 171–8, [DOI] [PubMed] [Google Scholar]
- 11.Kalhor M, Horowitz K, Beck M, et al. Vascular supply to the acetabular labrum. J Bone Joint Surg Am 2010; 92: 2570–5. [DOI] [PubMed] [Google Scholar]
- 12.Audenaert EA, Dhollander AAM, Forsyth RG, et al. Histologic assessment of acetabular labrum healing. J Arthrosc Relat Surg 2012; 28: 1784–9. [DOI] [PubMed] [Google Scholar]
- 13.Kim YT, Azuma H. The nerve endings of the acetabular labrum. Clin Orthop 1995;310:60–8. [PubMed] [Google Scholar]
- 14.Putz R, Schrank C. Anatomie des labrokapsulären komplexes. Der Orthopäde 1998; 10: 675–80. [DOI] [PubMed] [Google Scholar]
- 15.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. J Bone Joint Surg Br 1991; 73-B: 423–9. [DOI] [PubMed] [Google Scholar]
- 16.Ross JR, Zaltz I, Nepple JJ, et al. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med 2011; (39 Suppl): 72S–8S. [DOI] [PubMed] [Google Scholar]
- 17.Leunig M, Podeszwa D, Beck M, et al. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004; 418: 74–80 [DOI] [PubMed] [Google Scholar]
- 18.Horii M, Kubo T, Inoue S, et al. Coverage of the femoral head by the acetabular labrum in dysplastic hips: quantitative analysis with radial MR imaging. Acta Orthop Scand 2003; 74: 287–92. [DOI] [PubMed] [Google Scholar]
- 19.Kubo T, Horii M, Yamaguchi J, et al. Acetabular labrum in hip dysplasia evaluated by radial magnetic resonance imaging. J Rheumatol 2000; 27: 1955–60. [PubMed] [Google Scholar]
- 20.Büchler L, Beck M, Gollwitzer H, et al. Gelenkerhaltende Hüftchirurgie im Erwachsenenalter. Orthopäde 2012; 41:925–36. [DOI] [PubMed] [Google Scholar]
- 21.Henak CR, Ellis BJ, Harris MD, et al. Role of the acetabular labrum in load support across the hip joint. J Biomech 2011; 44: 2201–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rath E, Gortzak Y, Schwarzkopf R, Benkovich V, Cohen E, Atar D. The Diagnostic Value of the Vacuum Phenomenon during Hip Arthroscopy. ISRN Orthopedics. Volume 2011. Doi:10.5402/2011/852390. [DOI] [PMC free article] [PubMed]
- 23.Prietzel T, Drummer N, Pilz D, et al. Webers experiments regarding the stabilising effect of atmospheric pressure on the hip joint—a historical and experimental retrospect. Z Orthop Unfall 2008; 146:644–50. [DOI] [PubMed] [Google Scholar]
- 24.Chang CY, Huang AJ. MR imaging of normal hip anatomy. Magn Reson Imaging Clin N Am 2013; 21: 1–19. [DOI] [PubMed] [Google Scholar]
- 25.Aydingöz U, Oztürk MH. MR imaging of the acetabular labrum: a comparative study of both hips in 180 asymptomatic volunteers. Eur Radiol 2001; 11: 567–74. [DOI] [PubMed] [Google Scholar]
- 26.Lecouvet FE, Vande Berg BC, Malghem J, et al. MR imaging of the acetabular labrum: variations in 200 asymptomatic hips. AJR Am J Roentgenol 1996; 167:1025–8. [DOI] [PubMed] [Google Scholar]
- 27.Abe I, Harada Y, Oinuma K, et al. Acetabular labrum: abnormal findings at MR imaging in asymptomatic hips. Radiology 2000; 216:576–81. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen MS, Kheyfits V, Giordano BD, et al. Hip anatomic variants that may mimic abnormalities at MRI: labral variants. AJR Am J Roentgenol 2013; 201: W394–400. [DOI] [PubMed] [Google Scholar]
- 29.Corten K, Ganz R, Chosa E, et al. Bone apposition of the acetabular rim in deep hips—a distinct finding of global pincer impingement. J Bone Joint Surg Am 2011; 93(Suppl 2):10–6. [DOI] [PubMed] [Google Scholar]
- 30.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic inclination on determination of acetabular retroversion: a study on cadaver pelves. Clin Orthop Relat Res 2003; 407:241–8. [DOI] [PubMed] [Google Scholar]
- 31.Carsen S, Moroz PJ, Rakhra K, et al. The Otto Aufranc Award. On the etiology of the cam deformity: a cross-sectional pediatric MRI study. Clin Orthop Relat Res 2014; 472: 430–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Czerny C, Hofmann S, Neuhold A, et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology 1996; 200: 225–30. [DOI] [PubMed] [Google Scholar]
- 33.Nötzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002; 84-B: 556–60. [DOI] [PubMed] [Google Scholar]
- 34.Rakhra K, Sheikh AM, Allen DJ, et al. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res 2009; 467: 660–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pfirrmann CW, Mengiardi B, Dora C, et al. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology 2006; 240: 778–85. [DOI] [PubMed] [Google Scholar]
- 36.Chakraverty JK, Sullivan C, Gan C, et al. Cam and pincer femoroacetabular impingement: CT findings of features resembling femoroacetabular impingement in a young population without symptoms. AJR Am J Roentgenol 2013; 200: 389–95. [DOI] [PubMed] [Google Scholar]
- 37.Nepple JJ, Prather H, Trousdale RT, et al. Diagnostic imaging of femoroacetabular impingement. J Am Acad Orthop Surg 2013; 21(Suppl 1): S20–6. [DOI] [PubMed] [Google Scholar]
- 38.Henle P, Tannast M, Siebenrock KA. Bildgebende diagnostik der hüftdysplasie. Der Orthopäde 2008; 37: 525–31. [DOI] [PubMed] [Google Scholar]
- 39.Nelitz G, Puhl G. Reliability of radiological measurements in the assessment of hip dysplasia in adults. Br J Radiol 1999; 72(856): 331–4. [DOI] [PubMed] [Google Scholar]
- 40.Upasani VV, Bomar JD, Parikh G, et al. Reliability of plain radiographic parameters for developmental dysplasia of the hip in children; J Child Orthop 2012; 6: 173–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tönnis D. Die angeborene Hüftdysplasie und Hüftluxation im Kindes- und Erwachsenenalter. Berlin: Springer, 1984/1987. [Google Scholar]
- 42.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complications of osteoarthritis. Acta Chir Scan 1939; 58(Suppl): 7–38. [Google Scholar]
- 43.Mast NH, Impellizzeri F, Keller S, et al. Reliability and agreement of measures used in radiographic evaluation of the adult hip. Clin Orthop Relat Res 2011; 469: 188–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carlisle JC, Zebala LP, Shia DS, et al. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J 2011; 31: 52–8. [PMC free article] [PubMed] [Google Scholar]
- 45.Tschauner C. Die biomechanische Koxarthrose des jungen Erwachsenen. Z Orthop Unfallchir 2007; 145: 369–90. [DOI] [PubMed] [Google Scholar]
- 46.Wilson JD, Eardley W, Odak S, et al. To what degree is digital imaging reliable? Validation of femoral neck shaft angle measurement in the era of picture archiving and communication systems. Br J Radiol 2011; 84: 375–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lequesne M. Coxometry measurement of the basic angles of the adult radiographic hip by a combined protractor. Rev Rhum Mal Osteoartic 1963; 30: 479–85. [PubMed] [Google Scholar]
- 48.Delaunay S, Dussault RG, Kaplan PA, et al. Radiographic measurements of dysplastic adult hips. Skeletal Radiol 1997; 26: 75–81. [DOI] [PubMed] [Google Scholar]
- 49.Heyman CH, Herndon CH. Legg-Perthes disease; a method for the measurement of the roentgenographic result. J Bone Joint Surg Am 1950; 32: 767–78. [PubMed] [Google Scholar]
- 50.Bouttier R, Morvan J, Mazieres B, et al. Reproducibility of radiographic hip measurements in adults. Joint Bone Spine 2013; 80: 52–6. [DOI] [PubMed] [Google Scholar]
- 51.Werner CM, Copeland CE, Ruckstuhl T, et al. Radiographic markers of acetabular retroversion: correlation of the cross-over sign, ischial spine sign and posterior wall sign. Acta Orthop Belg 2010; 76: 166–73. [PubMed] [Google Scholar]
- 52.Diaz-Ledezma C, Novack T, Marin-Peña O, et al. The relevance of the radiological signs of acetabular retroversion among patients with femoroacetabular impingement. Bone Joint J 2013;95-B: 893–9. [DOI] [PubMed] [Google Scholar]
- 53.Nehmea A, Trousdaleb R, Tannousa Z, et al. Developmental dysplasia of the hip: Is acetabular retroversion a crucial factor? Orthop Traumatol Surg Res 2009; 95: 511–9. [DOI] [PubMed] [Google Scholar]
- 54.Cobb J, Logishetty K, Davda K, et al. Cams and pincer impingement are distinct, not mixed: the acetabular pathomorphology of femoroacetabular impingement. Clin Orthop Relat Res 2010; 468: 2143–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barham S. Labral tears, extra-articular injuries, and hip arthroscopy in the athlete. Clin Sports Med 2006; 25: 279–92. [DOI] [PubMed] [Google Scholar]
- 56.Wasielewski RC. The hip. In: Callaghan JJ, Rosenberg AG, Rubash HE. (eds.). The Adult Hip. Philadelphia: Lippincott-Raven, 1998. p. 57–73. [Google Scholar]
- 57.Kantarci F, Ozpeynirci Y, Unlu M, et al. Cross-sectional area of the labrum: role in the diagnosis of anterior acetabular labral tears. Eur Radiol 2012; 22: 1350–6. [DOI] [PubMed] [Google Scholar]
- 58.Won YY, Chung IH, Chung NS, et al. Morphological study on the acetabular labrum . Yonsei Med J 2003; 30;44: 855–62. [DOI] [PubMed] [Google Scholar]
- 59.Kubo T, Horii M, Yamaguchi J, et al. Radial magnetic resonance imaging and pathological findings of acetabular labrum in dysplastic hips. Pathophysiology 2000; 7: 171–5. [DOI] [PubMed] [Google Scholar]
- 60.Horii M, Kubo T, Hirasawa Y. Radial MRI of the hip with moderate osteoarthritis . J Bone Joint Surg Br 2000; 82: 364–8. [DOI] [PubMed] [Google Scholar]
- 61.Plotz GM, Brossmann J, von Knoch M, et al. Magnetic resonance arthrography of the acetabular labrum: value of radial reconstructions. Arch Orthop Trauma Surg 2001; 121: 450–7. [DOI] [PubMed] [Google Scholar]
- 62.Kubo T, Horii M, Harada Y, et al. Radial-sequence magnetic resonance imaging in evaluation of acetabular labrum. J Orthop Sci 1999; 4: 328–32. [DOI] [PubMed] [Google Scholar]
- 63.Blankenbaker DG, Tuite MJ. Acetabular labrum. Magn Reson Imaging Clin N Am 2013; 21: 21–33. [DOI] [PubMed] [Google Scholar]
- 64.Thomas JD, Li Z, Agur AM, et al. Imaging of the acetabular labrum. Semin Musculoskelet Radiol 2013; 17: 248–57. [DOI] [PubMed] [Google Scholar]
- 65.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis—what the radiologist should know. AJR Am J Roentgenol 2007; 188:1540–52. [DOI] [PubMed] [Google Scholar]
- 66.Register B, Pennock AT, Ho CP, et al. Prevalence of abnormal hip findings in asymptomatic participants: a prospective, blinded study. Am J Sports Med 2012; 40: 2720–4. [DOI] [PubMed] [Google Scholar]