Abstract
Ischiofemoral impingement (IFI) is an uncommon source of hip pain characterized by abnormal proximity of the lesser trochanter (LT) and the anterior border of ischium. The condition can be treated non-operatively but in severe cases, LT excision can provide beneficial results. Most previous descriptions for IFI operation use an open surgical approach but with the advancement of arthroscopic surgery, the LT can be approached less invasively. This study describes a simple endoscopic method to decompress the LT. Due to the posteromedial location of LT, this method requires careful positioning of the leg, and the use of curved type instruments is recommended. Also, it is helpful to assess the amount of resection with a properly oriented fluoroscopic view.
INTRODUCTION
Ischiofemoral impingement (IFI) is an uncommon cause of hip pain derived from direct impingement between the lesser trochanter (LT) and the ischium or from entrapment of quadratus femoris muscle between the two structures [1]. The condition can often improve with non-operative treatment but in cases with recalcitrant symptoms, operation maybe required. There are only few documented descriptions on operative technique for IFI which mostly recommend excision of LT with an open approach. However, with the improvement in arthroscopic techniques and devices, the entire LT can be accessed endoscopically. In this article, we introduce a novel technique for LT resection using endoscopy for treatment of IFI.
BRIEF CASE DESCRIPTION
A 17-year-old female college student was referred to our clinic complaining of a 3-year history of soreness and clunking in the left hip, initially after swimming. There was no preceding history of trauma. The pain was severe enough to prohibit her from participating in any sport activity and to interfere with normal daily life. The physical examination showed pronounced pain provocation when the hip was placed in an adducted and externally rotated position. Clunking was pronounced when the hip was adducted and externally rotated. Magnetic resonance imaging (MRI) revealed oedema and atrophy in the quadratus femoris adjacent to the ischium, but no intra-articular pathology was observed. A plane radiograph showed a prominent anterior inferior iliac spine presumably secondary to an old traction apophysitis. The symptoms did not respond to physiotherapy, cortisone injection and PRP treatment over 1-year period. Psoas tendon lengthening had been performed, and provided no relief of symptoms. Computed tomography-guided injection of local anaesthetic into the quadratus femoris provided marked temporary pain relief. The patient was diagnosed with IFI and the decision was made to perform LT resection using endoscopy.
SURGICAL TECHNIQUE
After general anaesthesia, the patient was placed on the surgical table in the supine position prepared in normal sterile fashion. A pillow was placed under the contralateral buttock to externally rotate the affected hip so that LT is rotated anteriorly, and can then be better visualized with fluoroscopic imaging. This arthroscopic technique requires the use of fluoroscopy, therefore, it is essential to use a radiolucent surgical table and proper radiation protection. Traction is not required during the operation process.
Two portals are used for this method: The proximal portal, which is used for instrumentation, is established at the level of the LT using a 16G spinal needle, and with the aid of fluoroscopy. The needle entry point in the skin is deliberately placed approximately 3 cm anterior to the femur, and the needle is directed posteromedially. Initially, the aim is for the needle tip to contact the lateral side of the femur, and the needle is then directed a little more anteriorly to pass across the anterior surface of the femur. This method of portal creation will result in a slightly oblique path for the instruments across the femur, passing from anterolateral to posteromedial, and help to access the more posterior part of the LT. The distal portal (main viewing portal) is made 5 cm distal to the anterolateral portal so that the instrument and the endoscope can be inserted between the interval of rectus femoris and vastus lateralis and triangulate at the LT (Fig. 1). With the hip in 30° external rotation, the spinal needle is introduced through the distal portal directed toward the anterior border of femur and advanced medially to the level of LT guided with fluoroscopy. The needle was switched with a nitinol guidewire and subsequently replaced with 4.5 mm trocar and 70° endoscope. With direct visualization, a radiofrequency ablation wand (ArthroCare, Austin, TX) is introduced through the proximal portal toward the LT and placed in the iliopsoas bursa. The soft tissue is ablated and the underlying iliopsoas tendon dissected until the anterior aspect of LT can be visualized. A pressure-controlled pump system, set at 60 mmHg provided sufficient pressure to create a working space around the LT. However, if extra working space is needed, a switching stick can be introduced through an additional accessory portal and used as a retractor.
Fig. 1.
The patient position with pillow under right pelvis (a). The endoscope and the arthroscopic burr are triangulate at the level of lesser trochanter with hip externally rotated (b)
Once the bony surface of LT is clearly visualized (Fig. 2A), a standard 5.5 mm round arthroscopic burr is introduced. The normal hooded sheath on the burr can be replaced with a shorter sheath, so the entire burr is unguarded. The shorter sheath allows better vision of the burr, and also minimizes abutment of the sheath against bone leading to impaired access. The anterior surface of LT is then burred away and this process is continued posteriorly by gradually externally rotating the hip (Fig. 2). As the LT is located on the posteromedial aspect of the femur, access to the posterior surface of LT may require additional hip external rotation a combination of hip flexion, abduction and external rotation can be beneficial. However, when the external rotation is achieved using this method, the muscle around the portal will become tense and it will be difficult to introduce the instruments through the portals. Therefore, it is helpful to first position the endoscope and arthroscopic burr adjacent to the LT and keeps the instruments in place as the assistant slowly manipulates the hip into the desired position. Also use of a curved type burr or ablation wand can be beneficial but care should be taken when manipulating these instruments in the externally rotated position as tensed muscle will create leverage stress on the instruments and may cause breakage. A working portal can be also moved more anteriorly to better access the posterior LT. The portals for camera and burr can be swapped as necessary. The final assessment of LT can be assessed with an oblique view of the hip (Fig. 3). As the Psoas attaches to the LT and also the adjacent bone and periosteum, the Psoas was not seen to detach and retract during trochanter resection. The key surgical tips are listed in Table I.
Fig. 2.
Arthroscopic view of the left hip through the distal portal. The iliopsoas tendon insertion and surrounding soft tissue is first ablated to expose the anterior bony structure (a). The lesser trochanter can be removed by gradual external rotating of the hip (b) until posterior aspect of lesser trochanter is completely removed (c). (Asterisk : lesser trochanter, arrow pointing proximal, double arrow head showing iliopsoas tendon.)
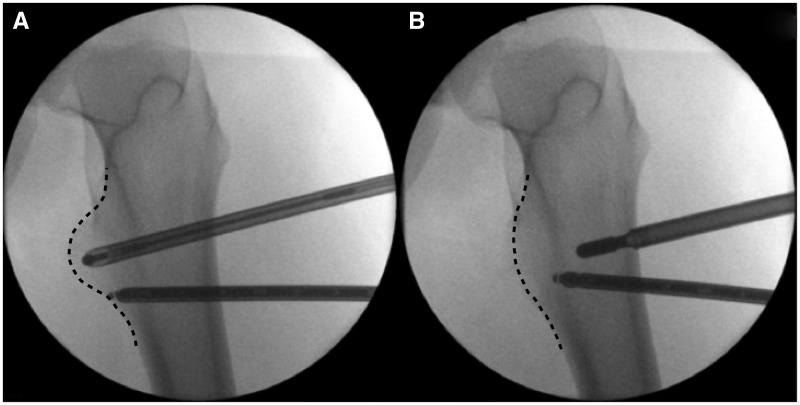
Fig. 3.
Fluoroscopic view of lesser trochanter in external rotation (a) before and (b) after the resection. The resection edge is marked by dotted line.
Table I.
Key surgical tips
|
The patient’s resting pain and provocation pain on adduction and external rotation disappeared within 1 week from the index operation. The symptom relief is maintained at 4 months follow up.
DISCUSSION
IFI has only recently gained attention as a source of hip pain and there is very limited literature describing its characteristics and treatment. The condition was first described by Johnson in 1977 as a medial inguinal pain with a characteristic of reduced distance between LT and ischial ramus in two patients following arthroplasty procedures and one following a proximal femoral osteotomy [2]. The pain resolved with LT resection in these patients thus verifying his theory that the symptoms were caused by the impingement of these two structures. More recent studies reported cases with congenital and acquired deformities (e.g. Perthes diseases) and in active individuals without any history of previous intervention in the hip [3, 4]. Although only a small number of cases have been reported, the condition has been reported predominantly in females with 25–40% being bilateral [4–6].
The diagnosis of IFI can be made with the combination of physical examination and radiologic imaging. A patient typically complains of deep inguinal or gluteal pain which is exacerbated when the hip is in the extension, adduction and external rotation position. The chronic inflammation of the entrapped qudratus femoris as a result of impingement can also affect the hamstrings or iliopsoas tendon; therefore, careful approach should be made to differentiate other tendinopathy conditions. MRI is recognized as the gold standard for diagnosis. Torriani et al. compared the patients group diagnosed with IFI with the control subjects and reported narrowing of the quadrilateral space (7 ± 3 versus 12 ± 4 mm) and ischiofemoral space (13 ± 5 versus 23 ± 8 mm). An abnormal signal intensity in quadratus femoris muscle in axial or coronal view of MRI is also a common presentation [1, 6]. Nevertheless, the diagnosis should be made very carefully as the presenting symptoms could be caused by, or accompanied by other pathologies.
LT excision has been recommended if conservative treatment fails but the operation method has not been standardized. A recent systematic review of extra-articular hip impingement reported operation methods for IFI from 2 case reports and 1 case series which were all treated with open procedures [7]. The pathologic lesion was accessed using either an anterior approach or lateral approach with trochanteric flip or through splitting of the iliotibial band [3, 4, 8]. Although no complication related to the open approach was reported, these invasive approaches can potentially endanger the vascular structures around the LT and some delay in rehabilitation can be expected. Of note, in all of the open approach described, the psoas tendon was reattached to the proximal femur. A very recent case report describes arthroscopic resection of the LT but the detail of the operation is lacking [9].
To safely approach the LT, the neurovascular structures around the hip need to be understood. The potential structures in particular danger are the medial and lateral femoral circumflex vessels. A cadaver dissection study described the medial circumflex artery to be located an average of 18 mm from the LT [10]. Therefore, careful approach is mandatory when approaching posterior and superior portion of LT. Also, as the LT is located posteromedial of the proximal femur, acquiring sufficient external rotation of the hip for visualization and access to the LT can be challenging. The use of curved instruments can be helpful, but if these are not available, an additional portal can be made anterior to the working portal described previously. Also, it is important to understand the best position of the hip to visualize the LT and to obtain the optimal fluoroscopic image for assessing the amount of bone resected. If the resection is done with not enough external rotation, the beveling will only occur in anterior surface leaving posterior LT remaining untouched (Fig. 4). From our experience, at least 60° of external rotation is recommended to accurately assess the posterior surface of LT. Therefore, oblique fluoroscopy image in different viewing angles maybe necessary. It should be noted that the operation involves repeatedly rotating the hip for resecting the LT and confirming amount of resection with fluoroscopy. We found it more efficient to start the operation with pelvis externally rotated on the affected side as this operation can be done on the conventional surgical table and the image can be blocked by metal rail when obliquely tilting the fluoroscopy. However, if the operation is performed on a radiolucent fracture table which allows flexion and external rotation freely, the operation could be performed without pillow after adjusting the angle of fluoroscopy. In addition, tilting the pelvis this way increases the passive external rotation of the hip and brings the LT forward and into view.
Fig. 4.
Drawing of lesser trochanter resection (dotted line) viewed from posterior and corresponding axial view at hip in neutral version (a), 30 external rotation (b), and 60° external rotation (c).
We chose to approach the LT from anteriorly for several reasons. First, this is the approach we regularly use to perform Psoas tendon lengthening when we perform that operation at a level immediately proximal to the LT. As a result of performing that operation on many occasions, we know that visualization of the tendon and LT can be readily obtained. Second, an anterior approach avoids the need to partially divide the quadratus femoris muscle. And third, an anterior approach minimizes the risk of damage to the sciatic nerve, and circumflex femoral vessels which are an important part of the blood supply to the femoral head.
Due to the location of the LT, the arthroscopic procedure can also be approached from posterior. A recent study by Hatem et al. [11] described the posterior approach and reported favourable outcome without any complication. However, at the level of the LT, the sciatic nerve is located 4 mm (±7.7) from the femoral boarder, and thus is in danger of injury unless very carefully approached [12]. Also, flexion of the hip enables anterior muscles to be relaxed and allows the manipulation of the instruments inserted anteriorly. We found sufficient bone could be resected without difficulty with proper patient and fluoroscopy positioning.
The number of indications for hip arthroscopy has been growing and arthroscopic techniques can now be applied in number of conditions that were once thought to be extremely difficult. LT decompression using endoscopy is a simple and safe intervention that can be used efficiently to treat IFI. However, the longer-term outcome of this treatment remains uncertain.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Tosun O, Algin O, Yalcin N, et al. Ischiofemoral impingement: evaluation with new MRI parameters and assessment of their reliability. Skeletal Radiol 2012; 41: 575–87. [DOI] [PubMed] [Google Scholar]
- 2.Johnson KA. Impingement of the lesser trochanter on the ischial ramus after total hip arthroplasty. Report of three cases. J Bone Jt Surg 1977; 59: 268–9. [PubMed] [Google Scholar]
- 3.Ganz R, Slongo T, Turchetto L, et al. The lesser trochanter as a cause of hip impingement: pathophysiology and treatment options. Hip Int 2013; Suppl 9: S35–41. [DOI] [PubMed] [Google Scholar]
- 4.Ali AM, Whitwell D, Ostlere SJ. Case report: imaging and surgical treatment of a snapping hip due to ischiofemoral impingement. Skeletal Radiol 2011; 40: 653–6. [DOI] [PubMed] [Google Scholar]
- 5.Stafford GH, Villar RN. Ischiofemoral impingement. Bone Jt J 2011; 93: 1300–2. [DOI] [PubMed] [Google Scholar]
- 6.Torriani M, Souto S, Thomas BJ. Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. Am J Roentgenol 2009; 193: 196–90. [DOI] [PubMed] [Google Scholar]
- 7.de Sa D, Alradwan H, Cargnelli S, et al. Extra-articular hip impingement: a systematic review examining operative treatment of psoas, subspine, ischiofemoral, and greater trochanteric/pelvic impingement. Arthroscopy J Arthrosc Related Surg 2014; 30: 1026–41. [DOI] [PubMed] [Google Scholar]
- 8.Viala P, Vanel D, Larbi A, et al. Bilateral ischiofemoral impingement in a patient with hereditary multiple exostoses. Skeletal Radiol 2012; 41: 1637–40. [DOI] [PubMed] [Google Scholar]
- 9.Safran M, Ryu J. Ischiofemoral impingement of the hip: a novel approach to treatment. Knee Surg Sports Traumatol Arthrosc 2014; 22: 781–5. [DOI] [PubMed] [Google Scholar]
- 10.Gautier E, Ganz K, Krugel N, et al. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br 2000; 82: 679–83. [DOI] [PubMed] [Google Scholar]
- 11.Hatem MA, Palmer IJ, Martin HD. Diagnosis and 2-year outcomes of endoscopic treatment for ischiofemoral impingement. Arthroscopy 2015; 31: 239–46. [DOI] [PubMed] [Google Scholar]
- 12.Ericksen ML, Swenson JD, Pace NL. The anatomic relationship of the sciatic nerve to the lesser trochanter: implications for anterior sciatic nerve block. Anesth Analg 2002; 95: 1071–4, table of contents. [DOI] [PubMed] [Google Scholar]