Abstract
Health disparities among Native Americans persist despite efforts to translate evidence-based programs from research to practice. Few evidence-based, theory-driven prevention and management interventions have been successfully translated within Native American communities. The use of community-based participatory research (CBPR) has shown promise in this process. This article provides an overview of the use of CBPR with Native American communities and discusses the translation of the Stanford Chronic Disease Self-Management Program, using a CBPR approach, with an urban Native American community. This article highlights not only how the CBPR process facilitates the successful translation of the Stanford program but also how CBPR is used within this community to build community capacity.
Keywords: Native American, American Indian, community-based participatory research, diabetes, diabetes self-management, chronic disease self-management
Native Americans have a higher burden of illness, injury, and premature mortality than non-Hispanic Whites (Dixon & Roubideaux, 2000; Roubideaux, 2002). Diabetes disproportionately affects Native Americans. On average, Native Americans are 2.6 times more likely to be diagnosed with diabetes than non-Hispanic Whites of a similar age (National Institute of Diabetes and Digestive and Kidney Diseases, 2005). Despite these health disparities, implementing evidence-based and theory-driven programs within Native American communities remains a challenge. The history of exploitation by scientific researchers experienced by many Native American communities, including an exclusion from control over the research process or findings, has led to difficulty in gaining access to and conducting research within many Native American communities (Campbell, Wunungmurra, & Nyomba, 2007; Davis & Reid, 1999; Mail, Conner, & Conner, 2006; Tom-Orme, 2006). Furthermore, the predominant TRIP (translation of research into practice) paradigm leaves out the critical element of community engagement in the cocreation and implementation of evidence-based programs (National Institutes of Health, 2007) and continues to be the predominant model in health promotion and disease prevention interventions despite its limited success (Glasgow, Vogt, & Boles, 1999; Green & Glasgow, 2006; Kerner, 2006). Community-based participatory research (CBPR) offers an alternative to traditional research approaches. CBPR can be a powerful conduit for translating research into practice and building capacity for greater community change.
CBPR has been defined as “systematic inquiry, with the participation of those affected by an issue for the purpose of education and action or effecting social change” (Green & Mercer, 2001, p. 1927). CBPR in health has been defined as “a collaborative approach to research that equitably involves all partners in the research process and recognizes the unique strengths that each brings. CBPR begins with a research topic of importance to the community with the aim of combining knowledge and action for social change to improve community health and eliminate health disparities” (Israel, Schulz, Parker, & Becker, 1998, p. 173).
CBPR is a means of community capacity building that uses research as a tool for social change. With its roots in the popular education and social justice movements, CBPR can be used by public health professionals and communities to collaborate in creating community-defined and community-driven public health that can be relevant and meaningful to the lives of those affected most by health disparities (Minkler & Wallerstein, 2003). The essence of the CBPR approach lies in a partnership between the researchers and the community (Minkler & Wallerstein, 2003). Researchers collaborate with the community rather than impose their research protocol on them (Minkler & Wallerstein, 2003). Community members are no longer passive subjects of research but active participants involved in a process of gaining and sharing knowledge and creating change (Minkler & Wallerstein, 2003; see also Green et al., 1995; Israel, Eng, Schulz, & Parker, 2005).
COMMUNITY-BASED PARTICIPATORY RESEARCH WITH NATIVE AMERICAN COMMUNITIES
CBPR has shown promise in translating research into practice within Native American communities. A literature review of CBPR with Native American communities showed that most published efforts to date have focused on substance abuse prevention and treatment (Ellis, 2004; Mohatt et al., 2004; Santiago-Rivera, Skawennio Morse, Hunt, & Lickers, 1998). Examples of CBPR with Native American communities can also be found in the areas of environmental health (Severtson, Baumann, & Will, 2002), breast cancer screening (Lantz et al., 2003), diabetes and obesity prevention (Davis & Reid, 1999; Satterfield et al., 2003), and suicide prevention (Fisher & Ball, 2002, 2003; Jumper-Thurman, Plested, Edwards, Foley, & Burnside, 2004). Some publications discuss specific health outcomes of interventions whereas others focus on describing the processes by which CBPR approaches have been used.
Lantz et al. (2003) describe the efforts of the National Breast and Cervical Cancer Early Detection Program to implement comprehensive cancer screening programs within tribal communities using a program model developed by state health departments. The researchers used participatory research processes, including key informant interviews and focus groups, to make the screening program more successful. Community members identified solutions to reduce barriers, including providing child care, transportation, and allowing community members to bring friends to the screenings for support. CBPR was essential in better understanding the programs and led to improved program planning and the development of more culturally appropriate screenings and interventions.
A participatory approach to exploring environmental health concerns among Lac Courte Oreilles (LCO) Ojibwa Indians in Sawyer County, Wisconsin, was used by Severtson et al. (2002). The project was grounded in a broad ecological conceptualization of environmental health and in principles of CBPR. Community participation was accomplished through a steering committee that consisted of the researchers and community members. The selected assessment methodology was a self-administered survey mailed to LCO members in Sawyer County. Concern for environmental issues was high within this tribal community and the LCO community used the survey results to further inform data needs and program development for the community.
CBPR methods have been used in several community-based interventions to prevent or delay the onset of type 2 diabetes in Native American communities (Daniel et al., 1999; Davis & Reid, 1999; Narayan et al., 1998; Satterfield et al., 2003). A total of four published studies were found describing efforts to prevent or delay the onset of type 2 diabetes within Native American communities using CBPR approaches (Daniel et al., 1999; Davis & Reid, 1999; Narayan et al., 1998; Satterfield, 2003). All four interventions engaged the target population in the development, implementation, and promotion of the interventions and incorporated culturally relevant messages, symbols, and strategies, with respect for and inclusion of traditional foods, activities, and knowledge. Narayan et al. (1998) reported a significant increase in sweat-producing physical activity and significant decrease in waist circumference in intervention participants. Daniel et al. (1999) reported that both body mass index and systolic blood pressure were significantly decreased for the intervention community relative to comparison communities. The intervention group showed a significant increase in knowledge of diabetes and increased prevalence of sweat-producing activity relative to comparison communities (Daniel et al., 1999).
The Pathways Study, a youth obesity prevention intervention for Native American schoolchildren, used a CBPR approach in developing the intervention components (Davis & Reid, 1999). This study included forming a collaborative partnership between universities and Native American tribes, schools, and families. The intervention, which was grounded in Social Learning Theory (Bandura, 1986), incorporated Native American customs and practices and sought to intervene at multiple levels.
Two powerful examples of CPBR in the area of substance abuse with Native American communities can be found in McKinley County, New Mexico, and Fremont County, Wyoming. McKinley County, New Mexico, located in the northwest corner of the state, is home to approximately 43,000 Native Americans. McKinley County was known for profiting from its proximity to “dry” reservations by placing few restrictions on the sale and use of alcohol. Gallup, McKinley County’s main border town, became known as “Drunk Town” over the course of several decades (Ellis, 2004). The National Institutes on Alcohol Abuse and Alcoholism reported that McKinley County had the highest composite index of alcohol-related mortality of all the United States for the period 1975 to 1977.
A series of negative media reports demanded the attention of community and tribal leaders and mobilized the entire community to action. A broad-based coalition, which included American Indian community members, policy makers, and public health professionals, implemented extensive policy changes, including an increase in the alcohol sales tax, lowering the driving while intoxicated (DWI) intoxication level, multimillion-dollar funding increases for substance abuse services, mandatory alcohol training for all health care professionals, the replacement of the “drunk tank” at the County jail with a 250-bed substance abuse treatment facility incorporating traditional healing, the closing of troublesome bars, and many other efforts (Ellis, 2004).
A follow-up report funded by the Robert Wood Johnson Foundation found that between 1974 and 1995, McKinley’s mortality rate for motor vehicle accidents declined by 60%, and was matched by similar declines in mortality from homicide (58%), suicide (59%), alcohol-induced causes (30%), and drug-induced causes (50%). Between 1989 and 1995, alcohol-related arrests declined 42% in Gallup, and protective custody detentions had declined by 50%. Finally, between 1982 and 1995, traffic crashes declined by 32% in McKinley County. All declines exceeded improvements in New Mexico and the nation (Ellis, 2004).
Fremont County, Wyoming, home of the Wind River Indian reservation, is located in the north-central portion of Wyoming and has a population of 7,000 Native Americans. Tribal leaders from Fremont Counties solicited the help of tribal leaders from McKinley County, and the two groups met over the course of a year to plan intervention efforts. Fremont County has since implemented both treatment and prevention services for youth and adults, reduced the number of drive-up windows for alcohol sales, created special substance abuse courts to provide treatment in lieu of incarceration, and collaborated with the media to actively promote and support the efforts (Ellis, 2004).
These two communities mobilized their citizenry to address local substance abuse problems through coordinated and community-directed initiatives. They worked closely with researchers in using and leveraging important epidemiological data as well as in the development and implementation of health intervention efforts.
THE SANTA CLARA VALLEY DIABETES COMMUNITY ACTION PROJECT
The Indian Health Center (IHC) of Santa Clara Valley, California, used a participatory approach to work in partnership with the local Native American community of Santa Clara Valley to facilitate the development of a 12-member diabetes community advisory committee, which has since become known as the Diabetes Community Action Project (DCAP). The DCAP consists of Native American community members who mobilized around their concerns about the high rates of diabetes within their community. The DCAP met monthly and its efforts were the guiding principles of the CBPR: research should be participatory, cooperative, empowering, and a colearning process; include systems development and capacity building; and balance research and action (Israel et al., 2005).
The Santa Clara Valley is home to approximately 21,000 Native Americans according to the U.S. Census Bureau (National Council for Urban Indian Health, 2005). San Jose, the largest city in the Valley, was a relocation city designated by the U.S. government as part of the Bureau of Indian Affairs Indian Relocation Termination Period, from 1952 to 1979, in which thousands of Native Americans were relocated to urban cities to be assimilated into mainstream society and culture. The urban Native American community is diverse and home to Native Americans representing more than 100 different tribal groups. There is no one particular area in which Native Americans live within the Santa Clara Valley, and they work and participate in all segments of the community. The lack of a community or cultural center for the population has made the local IHC one of the few places within the Valley that is specific to Native Americans.
The IHC was started by Native American community activists in the 1970s to develop a center for health care for Native Americans living within the area. Today however the Native American patient population of the clinic represents less than 30% of the total IHC patient population and the clinic now sees predominately low-income Hispanics. The reason for this is the clinic’s reliance on MediCal reimbursement to keep the clinic in operation. The lack of funding provided from the Indian Health Service to urban Indian health clinics has necessitated that the urban Indian health clinics be open to all low-income residents of the area. This has created tensions for some Native American community members, who feel the clinic should be used solely for Native Americans.
In 2003 the IHC was interested in assessing the needs of the Native American community around diabetes and improving the quality of diabetes care to patients. The clinic also hoped to strengthen community relationships and build trust. The newly hired Community Health Service Director and author of this article was asked to facilitate the development of a community advisory board to discuss health needs, diabetes needs in particular, and strengthen relationships with community members. Although the clinic hoped that diabetes would be a priority for the community, no specific issues were predetermined and the development of the group was to be community directed using participatory approaches.
As the new Community Health Services Director at the IHC I had relocated to the area and held the status of outsider, or at best “insider-outsider” as a Native American but not a member of the community. To reach out to the community I knew I would need the guidance and mentoring from an elder community member, but I did not yet know any elders. The Community Health Services Department staff of the clinic, particularly the community health representatives (CHRs), oriented me to the community and identified community members who might be interested in participating on the committee.
A list of names was generated and community members, IHC patients interested in or living with diabetes, community leaders, and elders were identified by the CHRs. Some of the names were repeatedly mentioned by all of the CHRs. One such person was a charismatic local community leader living with diabetes, Karen Medicine Cloud. A well-respected advocate, Karen had vocalized to the clinic in the past that she wanted to start a community diabetes group and was happy that the clinic had devoted a staff person to the development of the group. I called her and we spoke over the phone. I asked her for her help and Karen graciously agreed to mentor me.
First, she insisted, she would have to introduce me to community members in a nonformal way at community events. For 2 months I went to every community event being held and I attended with Karen Medicine Cloud and her family. The community members could feel free to come and talk to me, learn where I was from, hear about my life, and get to know me, and they could do this in an informal setting in which they were surrounded by their friends and fellow community members. This process, though simple, was powerful. I was developing a relationship with the people for whom I was going to advocate and work, and I could not do this unless they knew me and I knew them. After 2 months, Karen suggested we plan a community forum on diabetes.
Flyers were created and disseminated at all local community activities including health fairs, powwows, and community social and cultural gatherings. The flyers invited and encouraged all community members to attend the forum and share their voice in the health needs of the community. Diabetes was not specifically mentioned in the invitation to encourage participation from a broad range of community members and not only people interested in diabetes or living with diabetes. The goal of the forum was to facilitate openended dialogue about community health. The forum was advertised for roughly 2 months, and approximately 60 community members attended.
The format and agenda of the forum were open ended. The meeting was held at the IHC. Healthy food was provided from a local restaurant. Introductions were an important element of the evening, and on finishing the introductions, the floor was open for community members to talk about issues they felt the community was facing with regards to health. Karen Medicine Cloud raised the issue of diabetes and how it had affected her life. Diabetes was identified as being one of the most pressing health issues within the community. After several hours of discussing health in general and diabetes in particular, a consensus vote of the group was taken by an elder that an advisory committee would be formed in partnership with the clinic to focus on the issue of diabetes. The group would meet initially every month. Those who wanted to meet monthly could attend, and others could attend when they had time. At the first monthly meeting approximately 20 people attended. Over the course of the first three meetings, this smaller subgroup was composed of 12 community members who volunteered to meet monthly to work on the projects. This group has met regularly for more than 4 years and as noted above is called the Diabetes Community Action Project.
The first several monthly DCAP meetings were devoted to the facilitation of dialogue and trust building, a critical component of CBPR (Minkler & Wallerstein, 2003). The group began to identify issues related to diabetes and develop goals and priorities. Early project-specific action was also critical for the group in facilitating a sense of collective efficacy among its members (Bandura, 1986). Although the DCAP members needed time to examine this disease and how it was affecting the community, we also wanted to offer the community a service or program while further building our trust in each other and our confidence in ourselves as a group. Setting realistic goals for “early wins” can be an important part of the success of CBPR efforts (Minkler & Wallerstein, 2003).
The DCAP proposed the idea of implementing a kind of diabetes support program to help community members manage diabetes. I knew the importance of implementing theory-driven and evidence-based programs. We discussed the history of a self-management program that had been offered at the clinic several years prior for Native Americans with diabetes, the Stanford Chronic Disease Self-Management Program (CDSMP).
THE STANFORD CHRONIC DISEASE SELF-MANAGEMENT PROGRAM
The Stanford CDSMP is one of the most widely used patient self-management model in the world (Lorig, Sobel, Ritter, Laurent, & Hobbs, 2001). The program is a 6-week, peer-led program taught by two peer leaders to a group of 12 to 15 people and is based on the self-efficacy theory developed by Albert Bandura (1986). Self-efficacy theory specifies the determinants and mechanisms governing the acquisition of competencies and the regulation of motivation, adaptive behavior, and emotional well-being (Bandura, 1986). People’s belief in their personal efficacy is a central mechanism mediating the effects of psychosocial influence (Bandura, 1997). The CDSMP integrates self-efficacy theory through guided mastery experiences, acquisition of skills and enhancement of self-confidence through peer modeling, reinterpretation of physiological symptoms, and social persuasion.
In a randomized controlled trial, participants who took the CDSMP when compared with controls demonstrated improvements at 6 months in weekly exercise, frequency of cognitive symptom management, communication with the physician, self-reported health, health distress, fatigue, disability, and social or role function (Lorig et al., 2001). They also had fewer hospitalizations and 0.8 fewer days in the hospital (p < .05; Lorig et al., 2001).
Although the CDSMP had never been evaluated within the Native American population, it had been implemented in First Nations communities in Canada and several years prior to the formation of the DCAP the program had been implemented at the IHC. The IHC had contracted with a local hospital to offer the CDSMP program for its Native American diabetic patients. Fifteen people attended the first of the 6-week CDSMP. The program was cancelled after the 3rd week owing to lack of attendance. The DCAP members, some of whom had been participants in the original class, discussed reasons why the CDSMP may have failed.
DCAP members attributed the lack of success of the CDSMP to several key issues, all of which were related to the delivery of the program and the cultural acceptance of that delivery. The primary issue was that the curriculum had not been peer-led as it is intended to be implemented. The CDSMP had been led by a non–Native American person from the contracting hospital, who was perceived as an “outsider” by community members. The leader followed the curriculum rigidly, beginning the classes exactly on time even though most of the attendees had not yet arrived. A technique of the curriculum, social persuasion, had also not been implemented in a culturally acceptable manner. The peer leader encouraged everyone to set a goal, as written in the curriculum. When one of the elders refused to set a goal, the peer leader repeatedly asked him to set a goal despite his silence. The class perceived the peer leader as disrespectful. Finally, although the CDSMP had been offered during the evening at dinnertime, no meal had been provided to the participants, all of whom were diabetic. Transportation had also not been provided.
I felt the problem with the translation of the program into effective practice had not been in the design or content of the curriculum; it had been in its introduction to the community and in its delivery. The DCAP members agreed that most of the problems could be alleviated. The DCAP decided to implement the CDSMP, this time with community support and direction of the program. However, DCAP members determined that community capacity building would be the primary goal of implementing the CDSMP, not assessing the efficacy of the CDSMP among Native Americans. The DCAP intended to use the CDSMP as a mechanism for greater community awareness and change around diabetes.
PROGRAM IMPLEMENTATION
The DCAP implemented the CDSMP program in partnership with the Community Health Services Department at the IHC and with the support of Stanford Patient Education Research Center. Three DCAP members attended a local training on how to be a CDSMP peer leader and they worked with the clinic to advertise the program and recruit for the class. Participants were recruited through the IHC community health representatives at office visits, powwows, and local community gatherings, and the peer leaders (DCAP members) teaching the class were instrumental in recruiting via word of mouth.
A total of 18 people enrolled in the course. Three people were put on a waiting list and 15 people were invited to attend the first session. Twelve people arrived to the first class. Three participants from the waiting list joined the class during Week 2, whereas 3 dropped out of the class after Week 1 citing family responsibilities that would prevent them from coming regularly for 6 weeks. In total 12 people (n = 12) attended and graduated from the 6-week CDSMP course. All participants were Native American adults aged 18 years and older with type 2 diabetes.
Minimal changes were made to the program, listed as follows: (a) The teaching for each class began approximately 30 min after everyone arrived to give participants time to arrive, meet people, and start eating. (b) A meal was provided and the first 30 min of each meeting included socializing, eating, and talking. (c) Each class began with a blessing led by one of the peer leaders, and incorporated smudging (a cleansing ceremony practiced by many tribes) at the end of the class. (d) Although the peer leaders taught the curriculum exactly as was written, each class was approximately a half hour longer to accommodate story telling and narrative from the patients. (e) The symptom cycle, which represents all of the topic areas of the program’s curriculum, was presented in the form of a dream catcher, to illustrate self-management as a journey, as the peer leaders described it and the word vicious, which had been in the center of the graph where it read “vicious cycle,” was also removed. The revised symptom cycle can be seen in Figure 1.
FIGURE 1.
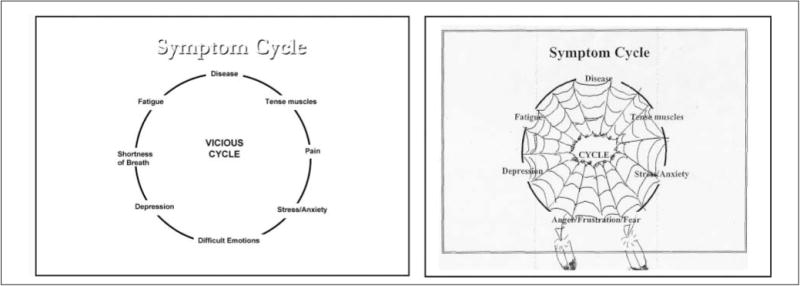
Symptom Cycles
PROGRAM EVALUATION AND OUTCOMES
The DCAP and peer leaders had a discussion about program evaluation; specifically, how they would evaluate or measure the usefulness and value of the CDSMP to the community. Members of the DCAP were reluctant to do any kinds of measurements given the history of research among Native Americans. They said they did not want to be “guinea pigs” or to “fill out a bunch of surveys.” However they did recognize and acknowledge the importance of knowing if the program was beneficial to their community and the need to determine that.
A fundamental goal of CBPR is education and action for effecting social change (Green et al., 1995). Participatory research begins with a research agenda defined by the community. The evaluation efforts of the CDSMP, as defined by the DCAP, cannot be examined outside the larger community context of the wellness movement the DCAP was creating. The CDSMP was only part of this movement, and the DCAP members determined early on in the process of implementing the CDSMP that community capacity building was the primary goal of the process. DCAP used CBPR to define their goals and help measure their successes. Community organizing and activism accompanied the implementation of CDSMP, and the outcomes of both efforts are interwoven.
The group developed a list of goals and ways to measure these goals. Table 1 shows the goals, measures, and outcomes of the CDSMP.
TABLE 1.
Program Evaluation Goals, Measures, and Outcomes Identified by the DCAP
| Goals | Measures | Outcomes |
|---|---|---|
| Participants show up and participate | Class sign-in sheets | Highest retention rate of any class offered at the Indian Health Center |
| Participants tell us they like the program | Individual interviews | Participants self-reported enjoying the class, learning a great deal |
| Participants start living healthier lives | Usage rates of the wellness and fitness center | Increase in fitness center usage by 34%; new assistant hired to handle increased usage |
| Participants get more involved in the community | Sign-in sheets for the three community events | Increase in participation at community events (sign-ins) |
| Participants encourage the clinic to offer the class again | Community participation to organize next classes | Course members initiated support group, meets monthly; |
| Three new community members were trained as peer leaders; | ||
| Stanford worked in collaboration with DCAP members to offer the program nationally for Native Americans over the Internet |
NOTE: DCAP = Diabetes Community Action Project.
DCAP defined a successful CDSMP as “people showing up and participating.” We agreed that we could determine this in a way that would not make people feel “researched,” by looking at the class sign-in sheets. The CDSMP had the highest retention rate of any health class that had been offered before at the IHC within the past 5 years. The IHC data for retention rates on health education programs only dated back to 5 years. Twelve people started the program, and 3 left at the first class as they were unable to commit to the 6-week length of the program. Three new people from the waiting list joined the class during Week 2 for a total of 12 participants, and all 12 participants completed the full 6-week CDSMP course. Sign-in sheets from all health education classes offered at the IHC for the previous 5 years showed class retention rates, on average, of 50% or lower after the first class. The CDSMP was able to maintain all 12 of their participants throughout the 5 weeks. This completion rate was higher than the usual completion rates for Stanford programs (Lorig, 2001).
One of the program goals was to know how participants felt about the class. To assess this, the peer leaders conducted informal individual interviews. This was the first time any of the peer leaders had ever conducted an interview. Peer leaders spoke over the phone with all 12 of the individuals within the 1st week after the class had ended and asked them about their perceptions of the class and how they felt. The peer leaders took notes and presented some of the quotes from CDSMP participants at the DCAP monthly meeting following the implementation of the CDSMP.
The peer leaders asked questions such as “Did you feel you learned a lot?” and “What changes did you feel like you have made over the last several weeks?” Although each of the participants reported different aspects of the course that they liked the most, all of the participants reported that they felt they were now able to make goals and set them, which is a primary focus of the CDSMP. Everyone also reported feeling like they had benefited from the course. One participant said, “I never felt like I could do anything about my diabetes. I also felt so alone. Now I know that there are others who feel like this. In this class we’ve helped each other find ways to overcome this. This class changed my life.”
A goal of the DCAP was to know if “participants started leading healthier lives.” A way to look at this was to monitor use of the fitness center. We hypothesized that the participants in the CDSMP class would use the fitness center more because of the emphasis on exercise in the CDSMP. The fitness center usage was low at the start of the CDSMP. On average, the sign-in sheets for the fitness center showed about 40 visits monthly to the center, mostly from the same handful of people. The fitness center is a relatively small room that houses five treadmills, some weight lifting equipment, a stretching area, and a conference room that is housed right next to the exercise room.
A review of the sign-in sheets from the fitness center revealed 85 visits within the 1st month of the start of CDSMP, creating an increase of 34%. This increase was maintained at 6 and 12 months after the implementation of the class and actually continued to rise. A fitness center assistant was hired part-time to handle the increased usage, and today that assistant works full-time.
Although the increase in the fitness center usage was general usage and cannot be attributed solely to the course, the 12 members of the community participating in the CDMSP were regularly using the fitness center and bringing with them friends and family members. In addition, the DCAP was building a wave of community support that led members of DCAP to attribute the increase in fitness center usage to the center’s having been “Indianized.” It was a space that had previously not been used, except by a handful of community members. Members of the CDSMP began having coffee at the adjoining room near the fitness center. This became an informal area to socialize outside of the CDSMP. Groups from the class would meet and exercise and then have coffee afterwards in the conference room. The fitness center, like a powwow or community event, became a social gathering point for this urban Native American community. As one class participant said, “People started to go over there and see who was there that day. After a while, I started going by there, doing my walking on the treadmill over there. There was always somebody over there to visit with.”
What the DCAP hoped for as a result of the CDSMP and accompanying DCAP action was that “participants get more involved in the community.” We therefore not only looked at the fitness center sign-in sheets but also the sign-in sheets of the three biggest community events held each year, the Gathering, the Christmas Party, and the Thanksgiving Party. We took sign-in sheets from the previous three years and compared them with the sign-in sheets during the year the CDSMP was implemented and the DCAP was organized. All three events, which averaged between 250 and 300 people in attendance at each event, had approximately 400 people attending the year of the CDSMP and DCAP.
Although we recognize that these methods are limited and the increased community participation cannot be attributed to the DCAP or CDSMP, the broad-based support the DCAP had initiated with its “wellness movement” was accompanied by an increase in community participation not seen in this community since the inception of the IHC and activism of the 1970s. The sign-in sheets were the measures the DCAP members were comfortable with using to determine what they wanted to know, that is, “did participants get more involved in the community.” The participants of the CDSMP attended these community events, as seen by the sign-in sheets, and they brought their friends and relatives with them.
The last measure that the DCAP identified for the CDSMP was that “participants encourage the clinic to offer the class again.” The CDSMP did continue to be offered at the IHC, though not regularly. The reasons for this are discussed in more detail in the Discussion section.
Participants from the original pilot CDSMP initiated the formation of a support group following the conclusion of the class. All of the members from the original class joined the support group, and about half of the class comes to the group regularly. This support group continues to meet on a monthly basis. Members from later classes have joined the group as well as members of the Diabetes Prevention Program offered at the clinic. The support group provides food (potluck dinners) and all meals are “diabetic-friendly,” with most of the meals being traditional Native American recipes. The support group has been in existence for more than 4 years to date. The members of this group also participate in a monthly nature walk offered by the clinic and as part of the Diabetes Prevention Program.
SUSTAINED COMMUNITY-BASED PARTICIPATORY RESEARCH EFFORTS
Accompanying the implementation of the CDSMP, the DCAP began holding an annual diabetes awareness health fair, which continues to date. The fair is entirely community-coordinated and implemented by DCAP members and with volunteer assistance from members who attended the original CDSMP class. The Diabetes Awareness Fairs have a community walk; free glucose, cholesterol, and blood pressure screenings; a healthy lunch buffet; and a community speakers panel that includes voices from community members living with diabetes or who are making positive changes to prevent developing diabetes.
The DCAP also launched a “Brown Is Better Campaign” during the 2nd year of our work, which is a campaign that gives away free healthy, whole-grain (brown grain) foods grown locally by the community garden that the DCAP started. The free foods are given away in brown bags with the DCAP logo on them, and the bags include a personal note from a DCAP member with a healthy eating tip or recipe or favorite inspirational quote.
The DCAP members wanted to find ways to sustain our community-organizing and capacity-building efforts and focus on diabetes prevention as well as the social and environmental factors contributing to diabetes. In October 2004, the IHC was one of only a few urban Indian health clinics in the country to receive funding from the national Indian Health Service to replicate the development and work of the DCAP in two additional urban communities. The DCAP members who had helped design the program and develop the grant were the guiding body of the project and secured funding for the next 7 years to continue our community work with a focus on diabetes prevention in our Santa Clara Valley community as well as within two other urban Native American communities.
As part of the diabetes prevention work, the DCAP continues to use participatory approaches to engage fellow community members. One recent example is a community diabetes needs assessment conducted at our annual fair in 2006. The assessment was conducted in the form of a raffle. Community members signed in at the front entrance of the fair and were given two blank sheets of paper. Each community member was asked to write down a question he or she had about diabetes, ask a fellow community member that question, and then write the answer the community member provided on the second sheet of paper. The sheets of paper were then returned to the front desk in exchange for the raffle ticket. The sheets of paper were stapled together and put in the raffle box. The questions were read aloud along with the matching raffle tickets, and the medical doctor member of the DCAP answered and discussed each question and then distributed the raffle prizes.
To help community members connect the social and environmental factors contributing to the epidemic of diabetes among Native Americans, the DCAP embarked on a Photovoice project. Photovoice is a grassroots approach to photography and social action (Herbert, 1996). It provides cameras to people to enable them to act as recorders and potential catalysts for social action and change in their own communities. The activity promotes dialogue about important issues through group discussion and photographs. It uses the power of the visual image and accompanying stories to create a participatory means of sharing expertise to create policy.
The DCAP engaged in a Photovoice project capturing images within our environments related to health. The photographs were vivid and powerful and connected the broad and multilevel environmental, social, and cultural determinants of health. One picture for example showed an empty playground with fast-food wrappers strewn across the basketball court and a broken fence next to a four-lane highway. The picture captured the lack of resources put into the youths’ playground as well as the dangers of playing in this particular neighborhood because of the highway traffic. The DCAP had a gallery showing of the photographs, and community members spoke about the photographs and their significance. The local television station did a film piece about the work for the community spotlight program. The photos were used to raise awareness about the social environment in which we live that contributes to obesity and diabetes and have been used as part of the Diabetes Prevention Program being implemented at the IHC and guided by the DCAP.
In 2007 the DCAP members were honored as recipients of the Indian Health Service Healthy Native Communities Fellowship Award. This program recognizes the community-based efforts of unique grassroots organizing in Indian Country and funds representatives of these efforts to take part in four trainings per year to strengthen skills in CBPR and community organizing.
The DCAP went on to partner with the Indian Health Service Health Promotion and Disease Prevention (HP/DP) Program in California and served as consultants for health promotion efforts with tribal communities in the state of California. The DCAP also worked in partnership with Stanford, the Indian Health Service, and the Healthy Native Communities Fellowship groups, to publish a revised book on community-based participatory research and organizing titled Restoring Balance.
DCAP members have traveled to urban, rural, and reservation communities to discuss diabetes and other health issues, strategies for community organizing, and cross-community capacity building. The DCAP members served as the guiding body for the planning of a national conference on youth obesity sponsored by the CA Indian Health Services HP/DP Program and the University of California, Davis. The DCAP has partnered with the Stanford University Patient Education Research Center and been recognized for its work by the University of California, Berkeley, Senior Leaders Program.
DISCUSSION
This article describes the experience of one urban Native American community in its efforts to make a difference in its community around the issue of diabetes. The evidence-based Stanford Chronic Disease Self-Management Program (CDSMP) was used by the DCAP with community-based participatory research (CBPR) approaches to facilitate a transformational experience for the members of the DCAP and their community.
There are several limitations to this study and the CBPR approach the DCAP undertook. The DCAP and the Indian Health Center (IHC) did not collect long-term data to document the impact of the success of the translation of the CDSMP. CBPR is an approach to research that should include quantitative and qualitative data collection, as appropriate, like any other research process. Long-term data on the effectiveness of the CDSMP would have informed the DCAP of the efficacy of the program and helped the DCAP in the area of sustainability and in securing future funding.
The IHC does not regularly conduct research so the use of CBPR at the clinic setting was a new approach for both the community and the clinic staff, and the research conducted was truly community directed. The IHC and the DCAP would have benefited from greater use of CBPR methods that were culturally appropriate and acceptable to measure more outcomes. The DCAP has since partnered with the Stanford Prevention Research Center to implement the program using the Internet, and CBPR approaches were used along with the collection of baseline and 6- and 12-month data. Results of that program will be discussed in another study and will reveal more information on the efficacy of the CDSMP with Native Americans and participatory approaches used.
Another limitation of this article is the sustainability of the CDSMP. The DCAP modeled a successful implementation of the CDSMP; however, the efforts to sustain the program were not in place at the IHC. The word-of-mouth recruitment within the community and the trusted Native American peer leaders that originally led the course were what made the program so successful. These variables had distanced the program from the clinic and made the CDSMP a community program.
The IHC made the effort to continue to offer the CDSMP, but assigned non–Native American community health educators employed by the clinic to be the leaders for the program. This was ultimately because the clinic must be concerned with meeting the daily demands of its patients and did not have the capacity to engage in long-term CBPR efforts, specifically identifying and training community peer leaders and recruiting for the program. It was more feasible for the clinic to incorporate the CDSMP into the existing job responsibilities of the health educators at the clinic.
The program has been offered at the clinic twice since it was peer led by the DCAP members and has not achieved the same participation or enthusiasm as it had in the first pilot implementation of the program. The clinic and the program also lost credibility among community members again by not offering the program as a peer-led program. The clinic gained back the reputation of not putting Native American needs as a top priority.
An additional limitation of the study is in how CBPR affected the community. The Diabetes Fair, the Brown Is Better campaign, and the other important events the DCAP spearheaded did serve to raise awareness about diabetes. The work also secured the Diabetes Prevention Program at the IHC that continues to create change in the community. However, the DCAP did not identify a way to measure how their work truly had an impact in the community beyond community participation. The Photovoice project brought greater awareness to the DCAP members who engaged in the work and to the community members about the structural nature of racism and poverty and their contributions to disease, but the DCAP did not have the capacity to advocate for policy change at a city or state level. It is hoped that participation in the Indian Health Service National Healthy Native Communities Fellowship will help build that capacity and leverage the collective power of the Native American population.
The strengths of the CBPR approach highlighted in this article are in the transformational effect that being involved in the DCAP had on its own members. Coming together to identify and support a common goal was not a new concept for community members. However, implementing the CDSMP using a CBPR process provided a structure within which community members could learn about themselves and their communities to create change. That was a new process and it helped the members of this urban Native community overcome prejudices and fears of research and also empowered and inspired these community members to engage in further, even more creative, research efforts, including the use of photography, and now film, to document their stories and reflectively engage with their surroundings. The experience helped us to reflect on our environments, our culture, and our community, and we grew closer through that process.
The work of the DCAP continues to date. The partnership with the Indian Health Service programs has connected the DCAP with grassroots health organizing movements happening across Indian country to strengthen our collective work. Our Diabetes Prevention Program continues. We are still meeting actively and have applied for additional new funding to support our film on diabetes and our community. Karen Medicine Cloud, the founder of our group and my mentor, passed away from diabetes complications 2 months after our DCAP group was formed. We continue to do our work for Karen and all people living with diabetes.
CONCLUSIONS
Though developed separately, CBPR methods in many ways mirror the guidelines developed and implemented by many Native American tribal governments for conducting research within their communities (American Indian Law Center, 1999). These guidelines include respect, equity, and empowerment (Santiago-Rivera et al., 1998; also see Fisher & Ball, 2003; Jumper-Thurman, 2004). The DCAP used the principles of CBPR to incorporate community engagement in the translation of research into practice with the Stanford CDSMP, previously not successful within the community. CBPR was a powerful conduit for translating research into practice and building community capacity. The success of the work was the truly peer-led participatory nature of the approach, which was maintained through all phases of the implementation of the CDSMP, and the empowerment of those who participated in the process.
Acknowledgments
The author would like to acknowledge Meredith Minkler, DrPH, for her guidance and mentorship of this work.
References
- American Indian Law Center. Model tribal research code, 2004. 1999 Retrieved May 9, 2007, from http://www.ihs.gov/medicalprograms/research/pdf_files/mdl-code.pdf.
- Bandura A. Social foundations of thought and action: A social cognitive theory approach. Upper Saddle River, NJ: Prentice Hall; 1986. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- Campbell D, Wunungmurra P, Nyomba H. Starting where the people are: Lessons on community development from a remote Aboriginal Australian setting. Community Development Journal. 2007;42(2):151–166. [Google Scholar]
- Daniel M, Green LW, Marion SA, Gamble D, Herbert CP, Hertzman C, et al. Effectiveness of community-directed diabetes prevention and control in a rural Aboriginal population in British Columbia, Canada. Social Science & Medicine. 1999;48:815–832. doi: 10.1016/s0277-9536(98)00403-1. [DOI] [PubMed] [Google Scholar]
- Davis SM, Reid R. Practicing participatory research in American Indian communities. American Journal of Clinical Nutrition. 1999;69(4):755S–759. doi: 10.1093/ajcn/69.4.755S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon M, Roubideaux Y, editors. Promises to keep: Public health policy for American Indians and Alaska Natives in the 21st century. Washington, DC: American Public Health Association; 2000. [Google Scholar]
- Ellis B. Mobilizing communities to reduce substance abuse in Indian country. In: Nebelkopf E, Phillips M, editors. Healing and mental health for Native Americans: Speaking in red. New York: Altamira; 2004. pp. 87–98. [Google Scholar]
- Fisher PA, Ball T. The Indian Family Wellness Project: An application of the tribal participatory research model. Prevention Science. 2002;3(3):235–240. doi: 10.1023/a:1019950818048. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Ball T. Tribal participatory research: Mechanisms of a collaborative model. American Journal of Community Psychology. 2003;32(3):207–216. doi: 10.1023/b:ajcp.0000004742.39858.c5. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health. 1999;89(9):1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green L, George MA, Daniel M, Frankish CJ, Herbert CP, Bowie WR, et al. Study of participatory research in health promotion: Review and recommendations for the development of participatory research in health promotion in Canada. Vancouver, British Columbia: Royal Society of Canada; 1995. [Google Scholar]
- Green LW, Glasgow RE. Evaluating the relevance, generalization, and applicability of research: Issues in external validation and translation methodology. Evaluation & the Health Professions. 2006;29(1):126–153. doi: 10.1177/0163278705284445. [DOI] [PubMed] [Google Scholar]
- Green LW, Mercer SL. Participatory research: Can public health agencies reconcile the push from funding bodies and the pull from communities? American Journal of Public Health. 2001;91:1926–1929. doi: 10.2105/ajph.91.12.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert CP. Community-based research as a tool for empowerment: The Haida Gwaii Diabetes Project example. Canadian Journal of Public Health. 1996;87(2):109–112. [PubMed] [Google Scholar]
- Israel B, Eng E, Schulz A, Parker E. Methods in community-based participatory research for health. San Francisco: Jossey-Bass; 2005. [Google Scholar]
- Israel BA, Schulz AJ, Parker E, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Jumper-Thurman P, Plested B, Edwards R, Foley R, Burnside M. Community readiness: The journey to community healing. In: Nebelkopf E, Phillips M, editors. Healing and mental health for Native Americans: Speaking in red. New York: Altamira; 2004. pp. 77–85. [Google Scholar]
- Kerner J. Knowledge translation versus knowledge integration: A funder’s perspective. Journal of Continuing Education in the Health Professions. 2006;26(1):72–80. doi: 10.1002/chp.53. [DOI] [PubMed] [Google Scholar]
- Lantz P, Orians C, Liebow E, Joe J, Burhansstipanov L, Erb J, et al. Implementing women’s cancer screening programs in American Indian and Alaska Native populations. Health Care for Women International. 2003;24(8):674–696. doi: 10.1080/07399330390227481. [DOI] [PubMed] [Google Scholar]
- Lorig K, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Effective Clinical Practice. 2001;4:256–262. [PubMed] [Google Scholar]
- Mail PD, Conner J, Conner CN. Commentary: New collaborations with Native Americans in the conduct of community research. Health Education & Behavior. 2006;33(2):148–153. doi: 10.1177/1090198104272054. [DOI] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N. Community based participatory research for health. San Francisco: Jossey-Bass; 2003. [Google Scholar]
- Mohatt G, Hazel K, Allen J, Stachelrodt M, Hensel C, Fath R. Unheard Alaska: Culturally anchored participatory action research on sobriety with Alaska natives. American Journal of Community Psychology. 2004;33(3):263–273. doi: 10.1023/b:ajcp.0000027011.12346.70. [DOI] [PubMed] [Google Scholar]
- Narayan KMV, Hoskin M, Kozak D, Kriska AM, Hanson RL, Pettitt DJ, et al. Randomized clinical trial of lifestyle interventions in Pima Indians: A pilot study. Diabetic Medicine. 1998;15:66–72. doi: 10.1002/(SICI)1096-9136(199801)15:1<66::AID-DIA515>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- National Council for Urban Indian Health. 2005 Retrieved January 2005 from http://www.ncuih.org/about/index.html.
- National Institute of Diabetes and Digestive and Kidney Diseases. American Indians, Alaska Natives, and diabetes. 2005 Retrieved April 2007 from http://diabetes.niddk.nih.gov/dm/pubs/americanindian/index.htm.
- National Institutes of Health. Native American research centers for health. 2007 Retrieved April 2007 from http://grants.nih.gov/grants/guide/rfa-files/RFA-GM-00-007.html.
- Roubideaux Y. Perspectives on American Indian health. American Journal of Public Health. 2002;92(9):1401–1403. doi: 10.2105/ajph.92.9.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santiago-Rivera A, Skawennio Morse G, Hunt A, Lickers H. Building a community-based research partnership: Lessons from the Mohawk Nation of Akwesasne. Journal of Community Psychology. 1998;26(2):163–174. [Google Scholar]
- Satterfield D, Volansky M, Caspersen CJ, Engelgau MM, Bowman BA, Gregg EW, et al. Community-based lifestyle interventions to prevent type 2 diabetes. Diabetes Care. 2003;26(9):2643–2652. doi: 10.2337/diacare.26.9.2643. [DOI] [PubMed] [Google Scholar]
- Severtson DJ, Baumann LC, Will JA. A participatory assessment of environmental health concerns in an Ojibwa community. Public Health Nursing. 2002;19(1):47–58. doi: 10.1046/j.1525-1446.2002.19007.x. [DOI] [PubMed] [Google Scholar]
- Tom-Orme L. Research and American Indian/Alaska Native health: A nursing perspective. Journal of Transcultural Nursing. 2006;17(3):261–265. doi: 10.1177/1043659606288379. [DOI] [PubMed] [Google Scholar]


