Abstract
Background
The National Children’s Study (NCS) Vanguard Study began enrollment in January 2009 as an initial pilot study for a planned large-scale, longitudinal U.S. cohort study of the effect of environmental influences on child health and development, with biological and environmental sample collection conducted in seven locations from April 2009 to October 2010. We sought to determine rates of consent for, and success of collection of, maternal and paternal biospecimens before and during pregnancy in the NCS Vanguard Study.
Methods
Samples of blood, saliva, vaginal swabs, urine, hair, and nails were collected prior to and during pregnancy. All specimens were sent to a central repository for processing, storage, and quality assessment.
Results
Of 780 pregnant women asked to consent to sample collection, 773 (>99%) agreed, and of 295 non-pregnant women, 292 (99%) agreed. Of 440 fathers asked to consent to sample collection, 435 (99%) agreed. Frequency of successful collection of biospecimens varied depending on sample and visit type. In descending order, the ranges over all visit types of the proportion of expected samples successfully collected from women were: urine, 92.5-95.7%; hair, 89.6-92.5%; vaginal swab, 84.2-88.5%; blood, 74.9-78.5%; two-day saliva, 65.8-81.6%; and nails, 76.4-76.7%. For fathers, rates were highest for urine (94.9%) and lowest for hair (63.0%).
Conclusions
High rates of consent for and collection of a wide variety of biospecimens can be achieved in prospective epidemiologic cohort studies of pregnant women. Ease of sample collection may be a primary factor influencing successful biospecimen collection.
Introduction
Growing recognition that transgenerational,1,2 prenatal,3,4 and early childhood5,6 events or processes are linked to childhood morbidity and to adult disease and mortality has led to the planning and piloting of large-scale, prospective studies of cohorts recruited at or prior to birth that include ongoing collection and storage of biological and environmental samples, with a goal to improve the health and well-being of children and to contribute to understanding the influence on health of various environmental and genetic factors. Birth defects, in particular, arise primarily from the effects of both genetic and environmental factors present during embryonic development. The identification of etiological factors will require the collection of various biospecimens during pregnancy in a longitudinal fashion. The NCS Vanguard was a pilot study designed to test feasibility, acceptability, and cost of candidate methodologies under consideration for inclusion in a larger cohort. Central to the conduct of such epidemiological cohort studies is the ability to obtain biological specimens for biological, environmental, and genetic analyses.7 Future measurement of genetic information and of exogenous and endogenous substances in biological specimens from the mothers, fathers, and children enrolled in the study allows analysis of environmental exposures, gene-environment interactions, and associations with health outcomes to be accomplished efficiently through nested prospective case-control studies. But not all biological specimens are created equally; some are invasive (blood), others difficult to obtain (infant urine), and still others raise concern among study participants about how the results of the tests may be used (e.g., genetic testing).8-16 This paper reports the initial NCS Vanguard experience in obtaining consent for biological and environmental sample collection and successful biological specimen collection. We also examined the acceptability of sample collection through the use of participant evaluation questionnaires.
Methods
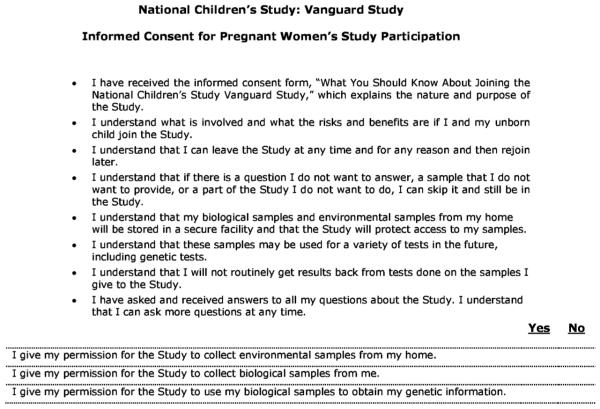
We report on 1,399 women and 440 men who were enrolled into the NCS initial Vanguard Study from seven locations: Queens County, New York; Duplin County, North Carolina; Salt Lake County, Utah; Orange County, California; Montgomery County, Pennsylvania; Waukesha County, Wisconsin; and four adjacent counties in South Dakota and Minnesota, as previously described.17 Written informed consent was obtained from all National Children’s Study (NCS) Vanguard participants or their legally authorized representatives, and the NCS Vanguard Study protocol was approved by an NIH Institutional Review Board (IRB) as well as multiple local IRBs at collaborating institutions. Adult participants were administered a general informed consent for overall participation in the study. A second informed consent, the Biospecimen and Environmental Sample Consent (BEC; Figure 1), was administered prior to the first study visit that required sample collection. The BEC applied to the consent for collection of environmental samples and biological specimens, and for those who consented to collection of biological samples, included permission to conduct genetic analyses. Every aspect of study participation was voluntary, and participants were reminded of this at each Study Visit.
Figure 1.
NCS Biological and Environmental Sample Consent (BEC) for Pregnant Women Signature Page Excerpt
In the course of their human research subject protection reviews, some local IRBs required changes to the NCS general informed consent materials. These changes ranged from inclusion of addenda to modifications in the language or substance of the consent forms. To assess any effects of such modifications on consent rates for genetic analyses, we categorized each of the study locations into three levels based on the degree of local IRB-initiated changes at a given study location. A “Level 3” location was defined as one that imposed significant, substantive changes to the consent forms and consent process, in particular as applied to genetic testing. The Level 3 modified consent form layout resembled the “black box” warnings listed on drug information inserts with one box dedicated to the collection of biospecimens, and required an additional signature specific to those activities. There was one Level 3 location (Queens County, New York). “Level 2” locations made minimal changes to the consent process, typically addition of a one or two-page informational sheet. There were two Level 2 locations (Waukesha County, Wisconsin and Orange County, California). “Level 1” locations did not alter the consent process as approved by the NICHD IRB. There were four Level 1 locations (Montgomery County, Pennsylvania; four adjacent counties in South Dakota and Minnesota; Salt Lake County, Utah; Duplin County, North Carolina).
Several different types of study visits were conducted during the NCS initial Vanguard Study: Pre-pregnancy visit (P1), first trimester visit (T1), third trimester visit among women who had a prior study visit (T3-Prior), third trimester visit among women who did not have a prior study visit (T3-First), and a Father visit, which occurred among identified fathers at any point prior to the birth of the child. The P1 study visit protocol included collection of 6 blood tubes, a saliva sample for genetic analyses if blood was not collected (blood not collected [BNC]-saliva), a 2-day saliva sample, 3 self-collected vaginal swabs, one 120-mL self-collected urine sample, and a hair sample (≥ 20 strands ≥ 1 cm in length). The T1 visit included collection of 7 blood tubes, a saliva sample for genetic analyses if blood was not collected (BNC-saliva), a 2-day saliva sample, 3 self-collected vaginal swabs, and one 120-mL self-collected urine sample. At the T3-Prior and T3-First visits, the protocol included collection of 8 blood tubes, a saliva sample for genetic analyses if blood was not collected (BNC-saliva), a 2-day saliva sample, 3 self-collected vaginal swabs, one 120-mL self-collected urine sample, a hair sample and nails (clippings from 10 toes). The Father visit included collection of 4 blood tubes, a saliva sample for genetic analyses if blood was not collected (BNC-saliva), one 120-mL self-collected urine sample, a hair sample, and nails. After collection, all biospecimens were processed, stored locally, and shipped to the NCS Repository (Fisher Bioservices, Rockville, MD) in accordance with specific NCS standard operating procedures.
Biospecimen quality was assured by use of pre-tested standard operating procedures18, data collector training and certification, and standardized supplies and equipment for all phases of biospecimen collection, transport, short-term storage, shipping, receipt, processing, and long-term storage. Collection supplies were prescreened to assure freedom from contamination by environmental chemicals. Biospecimen condition was evaluated and recorded upon receipt at the central repository. The quality of biospecimens was evaluated by testing a systematic sample for a wide range of clinical chemistry, metabolic, endocrine, immunologic, nutritional, toxicologic, and genetic analytes. Pooled NCS quality control materials were characterized and included as external controls with analytical runs. Analyte stability in short- and long-term storage was evaluated prospectively. Biospecimen quality was assessed further through pilot testing for environmental chemicals by the Division of Laboratory Sciences, National Center for Environmental Health, Centers for Disease Control and Prevention19,20, NCS supported formative research projects21,22, and independent supplemental methodologic studies23,24.
Each study visit also included an interview, which inquired about demographic characteristics, health conditions, medicines, environmental influences, and health-related behaviors; a physical exam (height, weight, blood pressure, etc.); the collection of environmental samples (maternal visits only); and a participant evaluation questionnaire.
Data Analysis
We calculated the proportions of interviewed participants who signed the BEC and who allowed for genetic testing of their biospecimens. Then we stratified those interviewed participants who signed the BEC according to the following demographic characteristics: age (<26, 26-35, >35 years); education (not high school graduate, high school graduate or some college, college graduate or higher); marital status (married, unmarried); survey language (English, Spanish); race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic African American, Asian, other race or multiple races); and family income (<$20,000, $20,000– $49,999, $50,000– $99,999, ≥$100,000).
We enumerated each biospecimen type collected by visit. We also categorized the degree of completeness of sample collection for each biospecimen as “complete” (all protocol-required biospecimens collected successfully), “partial” (one or more of the required biospecimen collection containers not collected), or “not collected” (no biospecimens collected). We then calculated the proportions of biospecimen collections that were complete, partial, or not collected.
We examined the genetic testing opt-out rate across the three different levels of local IRB-initiated changes to the consent process to determine if a lengthier or more complicated consent process might have deterred participants from consenting to genetic testing. Finally, we analyzed participant evaluation questionnaires to determine the acceptability of specimen collection.
Results
Participant characteristics by visit are shown in Table 1. The demographic characteristics of participants at initial Vanguard Study site locations represent a relatively diverse sample. Table 2 presents the numbers of participants who were interviewed, participants who signed the BEC, and participants who allowed for genetic testing of their samples. Across all visit types, the percent of participants who signed the BEC was very high (range: 99%–100%), as was the rate of consent for use of biospecimens for genetic testing (range: 91%–98%).
Table 1.
Characteristics of Biospecimen and Environmental Consent (BEC) Signatories
| Participant Characteristics | Pre- pregnancy (P1) n = 292 No. (%) |
First Trimester (T1) n = 610 No. (%) |
Third Trimester Initial (T3- First) n = 163 No. (%) |
Father n = 435 No. (%) |
|---|---|---|---|---|
| Age | ||||
| Under 26 | 81 (28) | 147 (24) | 58 (36) | 68 (16) |
| 26 to 35 | 178 (61) | 395 (65) | 76 (47) | 256 (59) |
| 36 and Over | 33 (11) | 68 (11) | 29 (18) | 111 (26) |
| Education1,2 | ||||
| Less than high school | N/A | 152 (25) | 65 (40) | 129 (30) |
| High school graduate or some college |
N/A | 184 (30) | 50 (31) | 128 (29) |
| College graduate or more | N/A | 271 (44) | 44 (27) | 178 (41) |
| Marital Status2 | ||||
| Married | 174 (60) | 474 (78) | 100 (61) | 366 (84) |
| Unmarried | 100 (34) | 136 (22) | 62 (38) | 69 (16) |
| Survey Language2 | ||||
| English | 252 (86) | 539 (88) | 129 (79) | 395 (91) |
| Spanish | 35 (12) | 66 (11) | 30 (18) | 35 (8) |
| Race and Ethnicity2,3,4 | ||||
| Hispanic | 68 (23) | 107 (18) | 48 (29) | 73 (17) |
| Non-Hispanic White | 112 (38) | 416 (68) | 86 (53) | 297 (68) |
| Non-Hispanic African American | 24 (8) | 31 (5) | 13 (8) | 21 (5) |
| Asian | 16 (5) | 26 (4) | * | 16 (4) |
| Other race/ multiple races | 69 (24) | 30 (5) | * | 28 (6) |
| Family Income1,2 | ||||
| Less than $20,000 | N/A | 73 (12) | 39 (24) | N/A |
| $20,000-$49,999 | N/A | 159 (26) | 31 (19) | N/A |
| $50,000-$99,999 | N/A | 192 (31) | 44 (27) | N/A |
| $100,000 or higher | N/A | 121 (20) | 16 (10) | N/A |
If a characteristic was not surveyed at a particular visit, N/A is entered since that information was not collected.
Some responses to surveys on these topics were unknown or not ascertained; therefore, the sum of the number of responses will not equal the combined N of 1,839.
The number of collections made on American Indians/Alaska Natives and Native Hawaiian/Pacific Islanders is included in the ‘Other race’ category because it was lower than the NCS disclosure risk threshold.
Values <10 are below an NCS defined disclosure risk threshold for protection of participant confidentiality and are represented by an asterix (*).
Table 2.
Biospecimen and Environmental Consent (BEC) and Genetic Consent Rate by Visit Type
| BEC Consent Rate No. (%) |
Genetic Consent Rate No. (%) |
|
|---|---|---|
| P1 n=295 | 292 (99) | 268 (91) |
| T1 n=615 | 610 (99) | 584 (95) |
| T3-First n=398 | 398 (100) | 392 (98) |
| Father n=440 | 435 (99) | 410 (93) |
Abbreviations: BEC= Biospecimen and Environmental Consent, P1 = pre-pregnancy visit, T1= first trimester visit, T3-First = Third trimester visit among women without a prior study visit.
Proportions of fully completed biospecimen collections ranged from 40% to 95% across all samples and visit types, with a median of 74% (Table 3). The proportion of fully completed biospecimen collections was 85% or higher in 14 of the 24 biospecimen-visit type combinations (P1 blood or BNC-saliva, P1vaginal swab, P1urine, P1hair; T1 blood or BNC-saliva, T1 2-day saliva, etc.). Urine collection was the most frequently completed biospecimen collection across the different visit types (median 95%). Blood collections were fully completed in 68% to 73% of visits. The lowest proportion of fully completed collections overall was observed for BNC-saliva (median 63%). The proportion of fully completed blood or BNC-saliva collections was 80% or more across all visit types (median 85%). The highest proportion of fully completed collections for all biospecimens at a given visit (“all specimen” in Table 3) was observed at the P1 visit (70%), and the lowest was at the T3-Prior visit (40%).
Table 3.
Biological Sample Collections Completed, Partially Completed, or Not Completed by Participant, Visit, and Sample Type
| Complete | Partial | Not Collected | |||||
|---|---|---|---|---|---|---|---|
| Biospecimen Type (# of collection containers) |
No. BEC Consented |
No. | % | No. | % | No. | % |
| P1 | |||||||
| Blood (6) | 292 | 212 | 73 | 15 | 5 | 65 | 22 |
| BNC Saliva (1) | 65 | 30 | 46 | N/A | N/A | 35 | 54 |
| Blood or BNC Saliva (6 or 1) | 292 | 242 | 83 | 15 | 5 | 35 | 12 |
| Vaginal (3) | 292 | 245 | 84 | * | * | * | * |
| Urine (1) | 292 | 270 | 92 | N/A | N/A | 22 | 8 |
| Hair (1) | 292 | 270 | 92 | N/A | N/A | 22 | 8 |
| All Specimen (11 or 6) | 292 | 205 | 70 | * | * | * | * |
| T1 | |||||||
| Blood (7) | 610 | 414 | 68 | 43 | 7 | 153 | 25 |
| BNC Saliva (1) | 153 | 88 | 58 | N/A | N/A | 65 | 42 |
| Blood or BNC Saliva (7 or 1) | 610 | 502 | 82 | 43 | 7 | 65 | 11 |
| 2-Day Saliva (6) | 610 | 449 | 74 | 49 | 8 | 112 | 18 |
| Vaginal (3) | 610 | 536 | 88 | * | * | * | * |
| Urine (1) | 610 | 580 | 95 | N/A | N/A | 30 | 5 |
| All Specimen (17 or 11) | 610 | 355 | 58 | 241 | 40 | 14 | 2 |
| T3-First | |||||||
| Blood (8) | 163 | 117 | 72 | 11 | 7 | 35 | 21 |
| BNC Saliva (1) | 35 | 22 | 63 | N/A | N/A | 13 | 37 |
| Blood or BNC Saliva (8 or 1) | 163 | 139 | 85 | 11 | 7 | 13 | 8 |
| 2-Day Saliva (6) | 163 | 100 | 61 | 13 | 8 | 50 | 31 |
| Vaginal (3) | 163 | 142 | 87 | 0 | 0.00 | 21 | 13 |
| Urine (1) | 163 | * | * | N/A | N/A | * | * |
| Hair (1) | 163 | 146 | 90 | N/A | N/A | 17 | 10 |
| Nails (1) | 163 | 125 | 77 | N/A | N/A | 38 | 23 |
| All Specimen (20 or 13) | 163 | 66 | 40 | * | * | * | * |
| T3-Prior | |||||||
| Blood (8) | 398 | 279 | 70 | 25 | 6 | 94 | 24 |
| BNC Saliva (1) | 94 | 59 | 63 | N/A | N/A | 35 | 37 |
| Blood or BNC Saliva (8 or 1) | 398 | 338 | 85 | 25 | 6 | 35 | 9 |
| 2-Day Saliva (6) | 398 | 245 | 62 | 17 | 4 | 136 | 34 |
| Vaginal (3) | 398 | 345 | 87 | * | * | * | * |
| Urine (1) | 398 | 379 | 95 | N/A | N/A | 19 | 5 |
| Hair (1) | 398 | 361 | 91 | N/A | N/A | 37 | 9 |
| Nails (1) | 398 | 304 | 76 | N/A | N/A | 94 | 24 |
| All Specimen (20 or 13) | 398 | 158 | 40 | 228 | 57 | 12 | 3 |
| Father | |||||||
| Blood (4) | 435 | 318 | 73 | 12 | 3 | 105 | 24 |
| BNC Saliva (1) | 105 | 75 | 71 | N/A | N/A | 30 | 29 |
| Blood or BNC Saliva (4 or 1) | 435 | 393 | 90 | 12 | 3 | 30 | 7 |
| Urine (1) | 435 | 413 | 95 | N/A | N/A | 22 | 5 |
| Hair (1) | 435 | 274 | 63 | N/A | N/A | 161 | 37 |
| Nails (1) | 435 | 388 | 89 | N/A | N/A | 47 | 11 |
| All Specimen (7 or 4) | 435 | 226 | 52 | * | * | * | * |
Abbreviations: BEC= Biospecimen and Environmental Consent, BNC= Blood not collected, P1 = pre-pregnancy visit, T1= first trimester visit, T3 First = Third trimester visit among women without a prior study visit.
Values <10 are below an NCS defined disclosure risk threshold for protection of participant confidentiality and are represented by an asterix (*).
Consent for genetic testing was obtained in 96.0% of participants in Level 1 sites, with a range across different visit types from 94.2% to 98.8% (Table 4). In Level 2 sites, 91.1% of participants provided consent for genetic testing, with a range from 83.5% to 97.5% across visits. The lowest proportions of participants who provided genetic testing consent in Level 2 locations occurred at the pre-pregnancy (P1) and Father visits (83.5% and 87.5%, respectively). Proportions of participants who gave consent for genetic testing at the maternal T1, T3-First, or T3-Prior visits in Level 2 locations were similar to those observed for other Levels. The proportion of participants who gave consent for genetic testing at the single Level 3 study location was intermediate between those observed for Level 1 and Level 2 locations. The Level 3 rate of consent for genetic testing was 94.6%, with a range across visit types from 89.6% to 100%. Sample size was insufficient to permit statistical comparisons of the effect of variance in the consent process across study locations on the proportion of participants who provided consent for genetic testing.
Table 4.
Consent for Genetic Testing among Interviewed Participants by Visit Type and Institutional Review Board Consent Modification Level
| P1 | Father | T1 | T3-First | T3-Prior | Total | |
|---|---|---|---|---|---|---|
| Level 1* | 154/162 (95.1%) |
256/269 (95.2%) |
380/397 (95.7%) |
97/103 (94.2%) |
250/253 (98.8%) |
1137/1184 (96.0%) |
| Level 2* | 71/85 (83.5%) |
112/128 (87.5%) |
160/170 (94.1%) |
37/42 (88.1%) |
116/119 (97/5%) |
496/544 (91.1%) |
| Level 3* | 43/48 (89.6%) |
42/43 (97.7%) |
44/48 (91.7%) |
20/20 (100%) |
26/26 (100%) |
175/185 (94.6%) |
| Total | 268/295 (90.8%) |
410/440 (93.2%) |
584/615 (95.0%) |
154/165 (93.3%) |
392/398 (98.5%) |
1808/1913 (94.5%) |
Level 1 = no alterations to NICHD IRB-approved consent process; Level 2 = minimal alterations to NICHD IRB-approved consent process; and Llevel 3 = significant, substantive changes to consent process, particularly as applied to genetic testing.
Participant satisfaction
Upon completion of study visits, a participant evaluation questionnaire was administered which included two questions that pertained to the sample collection process. The first question asked about participant perception of study visit duration. Three response choices were presented: (1) “far too long”; (2) “a little too long”; or (3) “about the right length”. Of those completing the first question, 70.8% felt that the study visit was “about the right length”, 25.5% felt it was “a little too long”, and the remaining 3.6% felt it was “far too long”. The second question asked how well the explanation prior to the study visit helped prepare the participant for what actually happened. Possible response options were (1) “not at all”; (2) “a little”; (3) “some”; or (4) “a lot”. Among survey respondents, 89.3% indicated that the explanation provided “a lot” of help, and 8.9% indicated that it provided “some” help. Responses from participants who consented to genetic testing were virtually identical to those who did not (data not shown).
Discussion
Successful collection of biospecimens provides an essential tool to evaluate the relationship between environment, genetics, and health across the lifecourse. Our analysis demonstrates that in the NCS Vanguard, a very high proportion of participants provided consent for biological and environmental sample collection and for genetic testing of biospecimens. The proportions of fully completed biospecimen collections varied by biospecimen type and visit type.
Urine was the biospecimen most successfully collected, in over 90% of scheduled collections for both mothers and fathers, regardless of the timing of collection during pregnancy. This is consistent with other large health surveys such as the Longitudinal Investigation of Fertility and the Environment (LIFE) Study that demonstrated rates of blood25 and urine26 collection in research participants approaching 100%, and successful serial urine sample collection. Other highly successful biospecimen collections from NCS women included vaginal swabs, possibly because they were self-collected, as well as hair. The proportion of successfully completed hair sample collections was lower in fathers. The 2-day saliva collections in mothers were more frequently successful in first trimester than in third trimester visits, possibly related to changes in relative salivary excretion rates during pregnancy,27 practical considerations associated with sample collection, or both. The proportion of successful blood collections was similar for mothers and fathers regardless of when during pregnancy samples were collected. The proportion of completed BNC-saliva collections was lower in mothers than in fathers. However, when we examined the proportion of fully completed collections for blood or BNC-saliva, it ranged from 82.3% to 85.3% in mothers at all study visit time points. Therefore, providing an alternative to blood draw using saliva, for purposes of analyses that are equally possible with either sample type, is a feasible way to ensure high rates of sample collection from a prenatal cohort.
One of the limitations of the study pertains to sociodemographic differences noted in those participants who enrolled in the study. We noted that study enrollment rates for women aged 35 years or older at the time of recruitment (OR [95% CI] 0.40-0.85 among women who were pregnant at the time of recruitment and 0.38-0.96 among women who were not pregnant) and among Asian women (OR [95% CI] 0.36-0.77). The results of this study should be interpreted within the context of the populations who were willing to consent into the study and provide samples. It should also be noted that this report focuses on sample collection in the field. The NCS Vanguard protocol design also included collection of intrapartum and/or postpartum samples from the delivery hospitalization. A separate analysis and manuscript to address consent for sample collection during delivery hospitalization is currently under review for publication elsewhere.
When we examined the proportion of participants who consented for study participation, sample collection, and genetic testing by level of burden and complexity of the consent process, we found that variation in the consent process did not appear to affect success of consent. However, because there were other differences in populations across the Vanguard sites that could have influenced willingness to consent, and the initial NCS Vanguard sample included only one study location where local IRB-required procedures substantially increased the burden and complexity of the consent process, we cannot draw any generalizable conclusions.
Preparation of study participants for the nature of the study visit appeared to be well received by participants, although it is not clear whether the high rate of consented participants is the result of such preparation. Nevertheless, in a long-term longitudinal cohort, building rapport with participants is essential to retain families over the course of the study. Participant burden is also an important consideration in prospective cohort studies, and if any substantial proportion of participants report that they find study visit length too great, that is an indication to adjust visit length. While we did not analyze recruitment rates to the overall study by location, the various modifications required by local IRBs to the consent process did not seem to affect the consent rate for genetic testing. This suggests that participants are capable of processing similar information in various forms with the same result.
In summary, we observed that initial NCS Vanguard biological sample collection was highly feasible and acceptable, with high proportions of participants consenting both for biospecimen collection and for genetic analysis. Overall sample collection success, fully complete or partial, was quite high across all visits. Very few participants provided no samples. A primary challenge in conducting successful sample collections is presented by the extent of specimen collection and the associated time required for collection. Acknowledging that investigators and participants are equal partners in the research enterprise, providing adequate preparation of participants, identifying optional methods of sample collection, considering samples that have general ease of collection such as urine and saliva, and allowing participants flexibility in contributing certain samples may help to assure success of epidemiologic cohort studies.28
Acknowledgements:
The authors gratefully acknowledge their indebtedness to the many communities, families, and health care providers whose participation made this study possible.
Support:
This analysis was conducted as part of the National Children’s Study, supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), and funded, through its appropriation, by the Office of the Director of the National Institutes of Health, with support through NICHD Contracts HHSN275200503414C, HHSN275200503411C, HHSN275200603416C, HHSN275200503415C, HHSN275200503413C, HHSN275200503410C, HHSN275200503396C, HHSN275200503395C, and HHSN275201000126U. The manuscript was developed by a Writing Team identified by the National Children’s Study Publications Committee for the purpose of timely sharing of centrally collected NCS data. We acknowledge the contributions of the following Vanguard Centers and Principal Investigators: Children's Hospital of Philadelphia, Jennifer Culhane; Mt. Sinai Medical School, Philip Landrigan; South Dakota State University, Bonny Specker; University of California at Irvine, James Swanson and Dean Baker; University of North Carolina at Chapel Hill, Barbara Entwisle and Nancy Dole; University of Utah School of Medicine, Ed Clark; University of Wisconsin, Maureen Durkin.
Footnotes
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Children’s Study, the National Institutes of Health, or the U.S. Department of Health and Human Services.
References
- Adams V, Miller S, Craig S, Sonam, Nyima, Droyoung, Le PV, Varner M. Informed consent in cross-cultural perspective: Clinical research in the Tibetan Autonomous Region, PRC. Cultural Medicine and Psychiatry. 2007;31:445–472. doi: 10.1007/s11013-007-9070-2. [DOI] [PubMed] [Google Scholar]
- Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatrics. 2014;168(11):1063–1069. doi: 10.1001/jamapediatrics.2014.1539. [DOI] [PubMed] [Google Scholar]
- Baker D, Park C, Sweeney C, McCormack L, Durkin M, Brenner R, Dabelea D, Entwisle B. Recruitment of Women in the National Children's Study Initial Vanguard Study. American Journal of Epidemiology. 2014;179(11):1366–1374. doi: 10.1093/aje/kwu062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakulski KM, Lee H, Feinberg JI, Wells EM, Brown S, Herbstman JB, Fallin MD. Prenatal mercury concentration is associated with changes in DNA methylation at TCEANC2 in newborns. Int J Epidemiol. 2015 2015 Apr 22;:pii. doi: 10.1093/ije/dyv032. dyv032. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJ, Eriksson JG, Forsén T, Osmond C. Fetal origins of adult disease: strength of effects and biological basis. International Journal of Epidemiology. 2002;(6):1235–1239. doi: 10.1093/ije/31.6.1235. [DOI] [PubMed] [Google Scholar]
- Birmingham K, Doyle A. Ethics and governance of a longitudinal birth cohort. Paediatric and Perinatal Epidemiology. 2008;23:39–50. doi: 10.1111/j.1365-3016.2008.00995.x. [DOI] [PubMed] [Google Scholar]
- Buck Louis GM, Schisterman EF, Sweeney AM, Wilcosky TC, Gore-Langton RE, Lynch CD, Boyd Barr D, Schrader SM, Kim S, Chen Z, Sundaram R. Designing prospective cohort studies for assessing reproductive and developmental toxicity during sensitive windows of human reproduction and development--the LIFE Study. Paediatric Perinatology and Epidemiology. 2011;25(5):413–424. doi: 10.1111/j.1365-3016.2011.01205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck Louis GM, Sundaram R, Sweeney AM, Schisterman EF, Maisog J, Kannan K. Urinary bisphenol A, phthalates, and couple fecundity: the Longitudinal Investigation of Fertility and the Environment (LIFE) Study. Fertility and Sterility. 2014;101(5):1359–1366. doi: 10.1016/j.fertnstert.2014.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunnik EM, Schermer MHN, Janssens ACJW. Personal genome testing: Test characteristics to clarify the discourse on ethical, legal and societal issues. BMC Medical Ethics. 2011;12:11. doi: 10.1186/1472-6939-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell KL, Pan Y, Mortensen ME, Makhmudov A, Merrill L, Moye J. Iodine Status in Pregnant Women in the National Children's Study and in U.S. Women (15-44 years), National Health and Nutrition Examination Survey 2005-2010. Thyroid. 2013 Aug;23(8):927–937. doi: 10.1089/thy.2013.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl K, Kesmodel U, Hvidman L, Olesen F. Informed consent: providing information about prenatal examinations. Acta Obstetricia et Gynecologica. 2006;85:1420–1425. doi: 10.1080/00016340600985198. [DOI] [PubMed] [Google Scholar]
- Dunbar NM, Szczepiorkowski ZM. Between the trash can and the freezer: donor education and the fate of cord blood. Transfusion. 2011;51:23423–6. doi: 10.1111/j.1537-2995.2010.03018.x. [DOI] [PubMed] [Google Scholar]
- Fisher CB. Privacy and Ethics in Pediatric Environmental Health Research – Part I: Genetic and Prenatal Testing. Environmental Health Perspectives. 2006;114:1617–1621. doi: 10.1289/ehp.9003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghantous A, Saffery R, Cros MP, Ponsonby AL, Hirschfeld S, Kasten C, Dwyer T, Herceg Z, Hernandez-Vargas H. Optimized DNA extraction from neonatal dried blood spots: application in methylome profiling. BMC Biotechnol. 2014 Jul 1;14:60. doi: 10.1186/1472-6750-14-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gronowski AM, Moye J, Jr., Wendler DS, Caplan AL, Christman M. The use of human tissues in research: what do we owe the research subjects? Clinical Chemistry. 2011;57(4):540–544. doi: 10.1373/clinchem.2010.154989. [DOI] [PubMed] [Google Scholar]
- Hoover RN, Hyer M, Pfeiffer RM, Adam E, Bond B, Cheville AL, Colton T, Hartge P, Hatch EE, Herbst AL, Karlan BY, Kaufman R, Noller KL, Palmer JR, Robboy SJ, Saal RC, Strohsnitter W, Titus-Ernstoff L, Troisi R. Adverse health outcomes in women exposed in utero to diethylstilbestrol. New England Journal of Medicine. 2011;365(14):1304–1314. doi: 10.1056/NEJMoa1013961. [DOI] [PubMed] [Google Scholar]
- Hugoson A. Salivary secretion in pregnancy: a longitudinal study of flow rate, total protein, sodium, potassium, and calcium concentration in parotid saliva from pregnant women. Acta Odontologica Scandinavica. 1972;30:49–66. doi: 10.3109/00016357209004592. [DOI] [PubMed] [Google Scholar]
- Landrigan PJ, Miodovnick A. Children’s Health and the Environment: An Overview. Mount Sinai Journal of Medicine. 2011;78:1–10. doi: 10.1002/msj.20236. [DOI] [PubMed] [Google Scholar]
- Mechanic L, Mendez A, Merrill L, Rogers J, Layton M, Todd D, Varanasi A, O'Brien B, Meyer WA, III, Zhang M, Schleicher RL, Moye J. Planned Variation in Preanalytical Conditions to Evaluate Biospecimen Stability in the National Children's Study (NCS) Clin Chemical Lab Med. 2013 Dec;51(12):2287–94. doi: 10.1515/cclm-2013-0454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miracle VA. Vulnerable populations in research. Dimensions of Critical Care Nursing. 2010;29(5):242–245. doi: 10.1097/DCC.0b013e3181e6d13e. [DOI] [PubMed] [Google Scholar]
- Moreno J, Caplan AL, Wolpe PR. Human Research Ethics Group. Updating protections for human subjects involved in research. Journal of the American Medical Assocation. 1998;280(22):1951–1958. doi: 10.1001/jama.280.22.1951. [DOI] [PubMed] [Google Scholar]
- Mortensen ME, Calafat AM, Ye X, Wong LY, Wright DJ, Pirkle JL, Merrill LS, Moye J. Urinary Concentrations of Environmental Phenols in Pregnant Women in a Pilot Study of the National Children's Study. Environ Res. 2014 Feb;129:32–8. doi: 10.1016/j.envres.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanes JA, Xia Y, Dassanayake PS, Jones RM, Li A, Stodgell CJ, Walker C, Szabo S, Leuthner S, Durkin M, Moye J, Miller RK. Selected Persistent Organic Pollutants in Human Placental Tissue from the United States. Chemosphere. 2014;106:20–27. doi: 10.1016/j.chemosphere.2013.12.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt CW. Uncertain inheritance: Transgenerational effects of environmental exposures. Environmental Health Perspectives. 2013;121(10):A298–303. doi: 10.1289/ehp.121-A298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith EN, Jepsen K, Angelo DA, Shepard PJ, Chambers CD, Frazer KA. Genetic Ancestry of Participants in the National Children’s Study. Genome Biology. 2014 Feb 3;15(2):R22. doi: 10.1186/gb-2014-15-2-r22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ten Have HAMJ. Global bioethics and communitarianism. Theoretical Medicine and Bioethics. 2011;32(5):315–326. doi: 10.1007/s11017-011-9190-0. [DOI] [PubMed] [Google Scholar]
- Titus-Ernstoff L, Troisi R, Hatch EE, Hyer M, Wise LA, Palmer JR, Kaufman R, Adam E, Noller K, Herbst AL, Strohsnitter W, Cole BF, Hartge P, Hoover RN. Offspring of women exposed in utero to diethylstilbestrol (DES): a preliminary report of benign and malignant pathology in the third generation. Epidemiology. 2008;(2):251–257. doi: 10.1097/EDE.0b013e318163152a. [DOI] [PubMed] [Google Scholar]
- Vickers MH. Early life nutrition, epigenetics and programming of later life disease. Nutrients. 2014;6(6):2165–2178. doi: 10.3390/nu6062165. [DOI] [PMC free article] [PubMed] [Google Scholar]