Abstract
Introduction
People with serious mental illness experience elevated severe obesity rates, yet limited evidence documents whether lifestyle intervention participation can benefit these individuals. This study examined the impact of the In SHAPE lifestyle intervention on weight loss among participants with serious mental illness and severe obesity (BMI ≥40 kg/m2) compared with participants who are overweight (BMI 25 to <30 kg/m2) and have class I (BMI 30 to <35 kg/m2) or have class II (BMI 35 to <40 kg/m2) obesity.
Methods
Data were combined from three trials of the 12-month In SHAPE intervention for individuals with serious mental illness collected between 2007 and 2013 and analyzed in 2014. In SHAPE includes individual weekly meetings with a fitness trainer, a gym membership, and nutrition education. The primary outcome was weight loss. Secondary outcomes were fitness, blood pressure, lipids, and program adherence.
Results
Participants (N=192) were diagnosed with schizophrenia spectrum (53.1%) or mood (46.9%) disorders. At 12 months, the overall sample showed significant weight loss, but differences among BMI groups were not significant (severe obesity, 2.57% [7.98%]; class II, 2.26% [8.69%]; class I, 1.05% [6.86%]; overweight, 0.83% [7.62%]). One third of participants with severe obesity achieved ≥5% weight loss, which was comparable across groups. More participants with severe obesity achieved ≥10% weight loss (20%) than overweight (2.9%, p=0.001) and class I (5.9%, p<0.001), but not class II (17.8%, p=0.974), obesity groups.
Conclusions
People with severe obesity and serious mental illness benefit similarly to those in lower BMI groups from lifestyle intervention participation.
Introduction
People with serious mental illness, including schizophrenia, schizoaffective disorder, major depressive disorder, and bipolar disorder, experience rates of obesity nearly double the observed rates within the general population,1–3 as well as elevated prevalence of severe obesity (BMI ≥40 kg/m2).1 This patient population is also disproportionately affected by comorbid medical conditions, increased cardiovascular risk, and poor health behaviors, which combined with elevated rates of obesity contribute to significantly reduced life expectancy up to 30 years fewer than the general population.4,5 This is further exacerbated by numerous challenges in achieving weight loss among people with serious mental illness, including metabolic effects of psychoactive medications, the impact of symptoms on motivation, poor diet, and poverty.2 Lifestyle interventions targeting fitness and diet may be an effective approach for addressing this serious public health concern.
In the general population, there is some evidence of the effectiveness and long-term benefit of behavioral weight management interventions for individuals with severe obesity.6,7 Similar behavioral interventions may be well suited for people with serious mental illness given recent evidence supporting the use of fitness and diet interventions in this population.8 For example, studies of different lifestyle interventions have demonstrated effectiveness in achieving ≥5% weight loss in upwards of 47% of participants, or reduced cardiovascular risk in as many as half of participants with serious mental illness.9–12 However, potential differential outcomes in different BMI groups are not known and it is not clear whether people with severe obesity and serious mental illness benefit from participation in an intensive lifestyle intervention to the same extent as less obese individuals.
The purpose of this study was to examine the impact of the 12-month In SHAPE lifestyle intervention on weight loss among participants with serious mental illness who had severe obesity (class III) compared with participants who were overweight (BMI 25 to <30 kg/m2) and had class I (BMI 30 to <35 kg/m2) or had class II (BMI 35 to <40 kg/m2) obesity. Secondary outcomes including fitness, blood pressure, lipids, and program adherence were also compared among the different BMI groups. Specifically, the aim of this study was to determine whether participants with severe obesity achieved differential outcomes when compared with lower BMI classes after participation in the In SHAPE lifestyle intervention.
Methods
The analyses in this study used data from participants who received the In SHAPE lifestyle intervention in three separate clinical trials in people with serious mental illness. Two were randomized trials and the third was an implementation study. The first randomized trial (N=133), conducted from April 2007 to November 2011, compared In SHAPE to gym membership at one community mental health center in Concord, New Hampshire.12 The second randomized trial (N=210), conducted from April 2008 to May 2013, compared In SHAPE to gym membership in people receiving services at one of three community mental health centers in Boston, Massachusetts.11 The third evaluation (N=122), conducted between December 2009 and March 2013, compared In SHAPE implemented in two community mental health centers with usual care in two additional centers from rural and urban settings in New Hampshire.
The current analytic sample consisted of data from the 192 participants who completed the 12-month In SHAPE intervention. Forty participants completed baseline assessments but did not complete the 12-month intervention. These dropouts were not included in the analyses, and did not differ from participants who completed the intervention on any baseline characteristics.
Participants across all three studies were aged ≥21 years; had serious mental illness defined by an axis I diagnosis of major depressive disorder, bipolar disorder, schizoaffective disorder, or schizophrenia (based on the Structured Clinical Interview for DSM-IV), and persistent impairment in multiple areas of functioning (e.g., work, school, self-care)13; had BMI >25 kg/m2; and provided informed consent for participation. Participants were on stable pharmacologic treatment defined as receiving the same psychiatric medications over the prior 2 months. Detailed inclusion and exclusion criteria are described elsewhere.11,12 Committees for the Protection of Human Subjects at Dartmouth College and specific to each site approved the study procedures.
In SHAPE is a fitness intervention consisting of a gym membership, weekly individual meetings with a certified fitness trainer, and instruction on healthy eating and nutrition.11,12,14 The fitness trainers completed a 1-week In SHAPE training consisting of instruction in motivational interviewing, fitness goal setting, healthy nutrition, tracking eating and exercise, and strategies for health behavior change in people with serious mental illness such as addressing mental health symptoms that interfere with exercise and healthy eating. Prior to enrollment, participants obtained medical clearance from their primary care provider. After conducting lifestyle and fitness evaluations, the fitness trainer developed personalized fitness plans for each participant using shared goal setting. Thereafter, they met with participants individually each week for 45–60 minutes at a local gym (YMCA) and provided fitness coaching, support, and reinforcement for exercise. The nutrition component consisted of individualized instruction emphasizing healthy eating during each session. Throughout the program, the fitness trainers received ongoing supervision from a health psychologist, personal fitness trainer, and registered dietitian.
Measures
Assessments were conducted at baseline and at 12-month follow-up for all study outcome measures. The primary outcome was weight (pounds) reported as the change in body weight over time and as the percentage change in weight. The proportion of participants who achieved ≥5% weight loss was calculated because modest weight loss is associated with improvements in cardiovascular risk factors in overweight and obese individuals in the general population15,16 and with diabetes.17 The proportion of participants who achieved ≥10% weight loss was also calculated because this widely used metric contributes to well-documented clinical benefits.18 These measures are considered clinically significant weight loss. Additional measures of obesity included BMI, calculated as weight (kg)/height (m)2, and waist circumference measured in inches.
The 6-Minute Walk Test (6-MWT) measures the distance in feet that an individual can walk in 6 minutes, and was used to evaluate participants’ fitness. In obese adults in the general population, the 6-MWT is considered a reliable and valid measure of fitness.19,20 Change in this measure was reported both as a change in feet and as a percentage change in feet. Two different measurement criteria for clinically significant improvement in fitness were used. First, an increase in distance >50 meters (about 164 feet) on the 6-MWT is considered clinically meaningful in terms of reduced cardiovascular risk among people with medical conditions including heart failure, chronic obstructive pulmonary disease, and pulmonary arterial hypertension.21 Among obese individuals in the general population, a >80 meter (about 263 feet) increase is considered clinically significant.19 Therefore, the proportion of participants who achieved >80 meter increase on the 6-MWT is reported; however, given the numerous challenges in promoting positive lifestyle change and the disproportionate burden of chronic disease affecting people with serious mental illness, the broader >50 meter criteria was also applied.
Blood pressure was measured after completing the 6-MWT. Serum lipids were measured using the CardioChek PA Analyzer, a portable testing system that produces reliable values for total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides using a multipanel test strip and a small amount of blood acquired with a finger prick.22 The number of visits, out of a maximum of 50 planned visits, with the fitness trainer over the 12-month intervention was measured. Study retention was assessed as completing the 12-month assessment.
Data on participants’ current medication use was collected because different antipsychotic agents are associated with varying degrees of weight gain23,24 and are known to affect ability to lose weight.2 Participants’ antipsychotic medications were classified as high weight gain propensity (e.g., olanzapine and clozapine), medium weight gain propensity (e.g., risperidone), or low weight gain propensity (e.g., ziprasidone) (footnote in Table 1 provides a full list of medications).
Table 1.
Baseline Characteristics of In SHAPE Participants Overall and by BMI Groupa
| Characteristic | Overall | Overweight (BMI 25 to <30) |
Class I (BMI 30 to <35) |
Class II (BMI 35 to <40) |
Class III (BMI ≥40) |
p-value |
|---|---|---|---|---|---|---|
| N | 192 | 34 | 53 | 48 | 57 | |
| Demographics | ||||||
| Age (yr) | 44.0 (11.1) | 47.9 (11.6) | 43.5 (10.5) | 42.1 (11.9) | 44.1 (10.2) | 0.117 |
| Sex | 0.507 | |||||
| Male | 92 (47.9%) | 15 (44.1%) | 26 (49.1%) | 27 (56.3%) | 24 (42.1%) | |
| Female | 100 (52.1%) | 19 (55.9%) | 27 (50.9%) | 21 (43.8%) | 33 (57.9%) | |
| Race | 0.289 | |||||
| Black | 33 (17.2%) | 3 (8.8%) | 11 (20.8%) | 10 (20.8%) | 9 (15.8%) | |
| Hispanic | 17 (8.9%) | 3 (8.8%) | 2 (3.8%) | 6 (12.5%) | 6 (10.5%) | |
| Non-Hispanic white | 131 (68.2%) | 26 (76.5%) | 34 (64.2%) | 32 (66.7%) | 39 (68.4%) | |
| Other | 14 (7.3%) | 2 (5.9%) | 6 (11.3%) | 0 (0%) | 3 (5.3%) | |
| Completed high school | 160 (83.3%) | 28 (82.4%) | 45 (84.9%) | 42 (87.5%) | 45 (78.9%) | 0.681 |
| Current smoker | 69 (36.1%) | 12 (35.3%) | 19 (35.8%) | 19 (39.6%) | 19 (33.9%) | 0.945 |
| Living situation | 0.190 | |||||
| Living independent | 132 (68.8%) | 24 (70.6%) | 39 (73.6%) | 27 (56.3%) | 42 (73.7%) | |
| Supervised/supported housing | 60 (31.3%) | 10 (29.4%) | 14 (26.4%) | 21 (43.8%) | 15 (26.3%) | |
| Married | 0.064 | |||||
| Never married | 125 (65.1%) | 20 (58.8%) | 40 (75.5%) | 35 (72.9%) | 30 (52.6%) | |
| Currently married | 13 (6.8%) | 2 (5.9%) | 1 (1.9%) | 2 (4.2%) | 8 (14.0%) | |
| Previously married | 54 (28.1%) | 12 (35.3%) | 12 (22.6%) | 11 (22.9%) | 19 (33.3%) | |
| Diagnosis | 0.394 | |||||
| Schizophrenia spectrum Disorder | 102 (53.1%) | 16 (47.1%) | 25 (47.2%) | 30 (62.5%) | 31 (54.4%) | |
| Mood disorder | 90 (46.9%) | 18 (52.9%) | 28 (52.8%) | 18 (37.5%) | 26 (45.6%) | |
| Obesity measures | ||||||
| BMI | 37.1 (8.0) | 27.8 (1.7) | 32.3 (1.6) | 37.3 (1.5) | 47.0 (6.4) | <0.001 |
| Weight (lbs) | 235.2 (56.0) | 179.2 (28.1) | 206.5 (25.8) | 237.5 (27.8) | 293.4 (53.1) | <0.001 |
| Waist circumference (inches) | 47.0 (6.9) | 39.5 (4.6) | 43.9 (3.1) | 47.8 (3.8) | 53.8 (6.3) | <0.001 |
| Fitness | ||||||
| Fitness (6-MWT in feet)b | 1,388.3 (313.0) | 1,529.5 (283.5) | 1,485.5 (227.1) | 1,366.6 (273.4) | 1,233.3 (359.5) | <0.001 |
| Blood pressure and serum lipids | ||||||
| Systolic blood pressure (mmHg) | 126.4 (18.5) | 119.5 (16.7) | 124.2 (17.5) | 126.5 (19.5) | 132.6 (18.3) | 0.008 |
| Diastolic blood pressure (mmHg) | 81.9 (12.3) | 77.6 (10.0) | 80.9 (12.2) | 81.7 (11.5) | 85.5 (13.5) | 0.027 |
| Total cholesterol (mg/dL) | 182.4 (44.7) | 177.1 (45.2) | 183.5 (44.8) | 184.9 (47.9) | 182.5 (42.4) | 0.901 |
| LDL (mg/dL) | 109.6 (37.3) | 112.3 (40.7) | 104.7 (37.5) | 118.8 (39.3) | 106.1 (33.7) | 0.364 |
| HDL (mg/dL) | 41.9 (15.6) | 41.9 (14.3) | 45.0 (20.3) | 36.1 (10.6) | 43.9 (13.6) | 0.033 |
| Triglycerides (mg/dL) | 178.0 (115.4) | 166.5 (110.2) | 173.7 (94.3) | 186.4 (139.6) | 181.7 (116.7) | 0.889 |
| Elevated risk of hypertensionc medications | 64 (33.9%) | 6 (18.2%) | 16 (30.2%) | 16 (34.0) | 26 (46.4%) | 0.048 |
| Number of psychotropic medications | 2.1 (1.1) | 2.0 (1.2) | 2.0 (1.1) | 2.3 (1.2) | 2.2 (1.0) | 0.635 |
| Weight gain propensity medications | 0.166 | |||||
| Highd | 68 (37.6%) | 9 (30.0%) | 25 (49.0%) | 17 (38.6%) | 17 (30.4%) | |
| Mediume | 71 (39.2%) | 16 (53.3%) | 12 (23.5%) | 16 (36.4%) | 27 (48.2%) | |
| Lowf | 31 (17.1%) | 2 (6.7%) | 11 (21.6%) | 8 (18.2%) | 10 (17.9%) | |
| None | 11 (6.1%) | 3 (10.0%) | 3 (5.9%) | 3 (6.8%) | 2 (3.6%) |
Note: Boldface indicates statistical significance (p<0.05).
Chi-square and ANOVAs to compare proportions and means across different obesity classes.
6-MWT refers to the 6-Minute Walk Test, which is a measure of fitness calculated as the number of feet that an individual can walk in 6 minutes.
Elevated risk of hypertension defined as systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg
High weight gain propensity medications include: olanzapine, clozapine
Medium weight gain propensity medications include: haloperidol, risperidone, quetiapine, thioridazine, chlorpromazine, paroxetine, amitriptyline, divalproex, valproate, doxepin, lithium, carbamazepine, imipramine, gabapentin
Low weight gain propensity medications include: ziprasidone, perphenazine, fluphenazine, fluoxetine, buproprion, venlafaxine, molindone, lamotrigine, duloxetine, aripiprazole, fluvoxamine, trazodone, desipramine, loxapine, sertraline, escitalopram, clomipramine, nortriptyline, citalopram, paliperidone, topiramate, mirtazapine, lurasidone
Statistical Analysis
Participants from different BMI groups were compared at baseline on demographic characteristics, obesity measures, fitness, blood pressure, lipids, and use of antipsychotic medications and differing weight-gain propensity psychiatric medications using chi-square tests for categorical variables and one-way ANOVAs for continuous variables. For continuous outcome variables including the primary outcome of weight loss and secondary measures of obesity, fitness, blood pressure, and lipids, linear regression models were used to compare BMI group means at 12 months, controlling for study (Trial 1, 2, or 3), age, gender, race, and program adherence. The proportions of participants in the different BMI groups who achieved ≥5% and ≥10% weight loss, and improved fitness (>50- and >80-meter increase on the 6-MWT) at 12 months were compared via logistic regression models adjusting for study (Trial 1, 2, or 3), age, gender, race, and program adherence. When a significant association was found between BMI group and an outcome (type III test), post hoc pairwise comparisons between BMI groups were performed using contrasts from the model. The purpose of these pairwise comparisons was to assess how participants in the class III obesity group differed compared with each of the other groups. For overall comparisons between BMI groups, a p-value of 0.05 was considered significant. To assess significance of the post hoc pairwise comparisons, a Bonferroni correction was applied to the three pairwise comparisons between each BMI group and the class III obesity group. Therefore, a p-value of 0.017 (0.05/3) or less was considered significant, yielding an overall 0.05 significance level for the group of tests. All statistical analyses were performed in 2014 using SPSS, version 19.
Results
At baseline, marital status, fitness, blood pressure, and high-density lipoprotein cholesterol differed among the weight classes (Table 1). Elevated risk of hypertension, defined as systolic blood pressure >140 mmHg or diastolic blood pressure >90 mmHg differed among weight classes (p=0.048), and was highest among participants with severe obesity (46.4%). Number of antipsychotic medications, use of high weight gain–propensity psychiatric medications, smoking status, and other demographic characteristics were comparable among BMI groups at baseline. BMI in the severe obesity group ranged from 40.2 to 77.3 kg/m2, where 95% had a BMI between 40 and 60 kg/m2.
Table 2 shows the baseline to 12-month changes in the primary outcome of weight, and secondary measures including fitness, blood pressure, and lipids. The table presents raw unadjusted means for BMI class and p-values from the linear regression models. At 12 months, the overall sample showed significant weight loss (4.73 [19.20] pounds, p=0.002), but differences in weight loss among BMI groups were not significant. Improvement in the 6-MWT was observed at 12-months for the overall sample (59.89 [228.98] feet, p=0.001), with no significant differences among BMI groups. There were no significant differences among BMI groups for changes in blood pressure and lipids.
Table 2.
Change in Outcomes From Baseline to 12 Months Among BMI Groups (12 Month – Baseline)
| Variable | n | Overall (N=192) |
Overweight (N=34) |
Class I (N=53) |
Class II (N=48) |
Class III (N=57) |
p-valuea |
|---|---|---|---|---|---|---|---|
| Change in obesity measures | |||||||
| Weight change (lbs) | 185 | −4.73 (19.20) | −1.88 (12.61) | −2.06 (14.01) | −5.51 (21.19) | −7.13 (24.37) | 0.136 |
| Weight change (%) | 185 | −1.76 (7.78) | −0.83 (7.62) | −1.05 (6.86) | −2.26 (8.69) | −2.57 (7.98) | 0.205 |
| BMI (kg/m2) | 185 | −0.72 (3.03) | −0.28 (2.04) | −0.33 (2.22) | −0.83 (3.25) | −1.25 (3.87) | 0.086 |
| Waist circumference (inches) | 185 | −1.42 (3.32) | −1.82 (3.42) | −1.41 (2.52) | −1.64 (3.43) | −1.00 (3.84) | 0.853 |
| Change in fitness | |||||||
| % Change in fitness (6 MWT in feet)b | 165 | 5.57 (18.03) | 4.55 (18.05) | 2.52 (18.48) | 8.22 (14.81) | 6.84 (20.02) | 0.643 |
| Fitness (6 MWT in feet) | 165 | 59.89 (228.98) | 62.12 (267.39) | 26.09 (271.52) | 99.83 (192.44) | 56.04 (183.46) | 0.767 |
| Change in blood pressure and serum lipids | |||||||
| Systolic blood pressure | 173 | 2.32 (18.37) | 3.25 (18.97) | 2.33 (17.76) | 5.45 (15.91) | −0.86 (20.37) | 0.231 |
| Diastolic blood pressure | 173 | −0.21 (12.15) | 0.28 (13.21) | 0.60 (11.95) | −0.95 (11.55) | −0.69 (12.44) | 0.897 |
| Total cholesterol | 149 | −3.08 (40.43) | −4.50 (44.65) | −0.26 (39.22) | −6.50 (47.36) | −2.43 (34.49) | 0.917 |
| LDL | 105 | −3.46 (36.44) | −5.71 (35.33) | −6.47 (34.91) | −3.90 (46.48) | 0.41 (33.56) | 0.966 |
| HDL | 149 | −3.22 (16.51) | 0.36 (14.47) | 5.71 (21.79) | 7.03 (12.88) | 0.11 (13.72) | 0.211 |
| Triglycerides | 149 | −8.42 (114.15) | −18.11 (91.29) | 10.52 (113.49) | −35.69 (126.39) | −1.02 (117.59) | 0.334 |
P-values from linear regression models adjusting for study (Trial 1, 2, or 3), age, gender, race, and program adherence.
6-MWT refers to the 6-Minute Walk Test, which is a measure of fitness calculated as the number of feet that an individual can walk in 6 minutes.
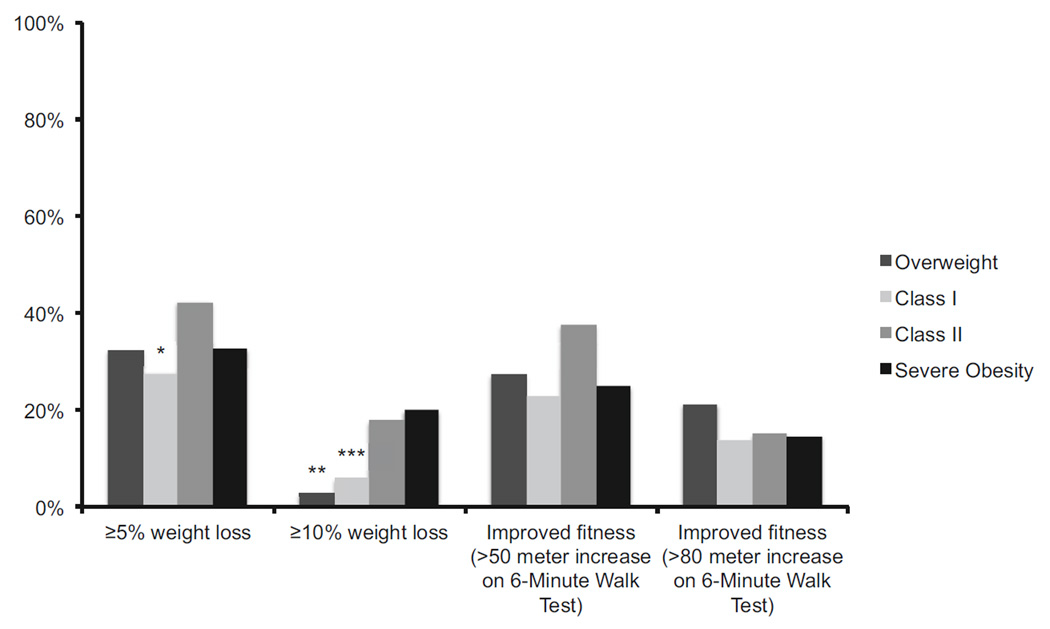
Differences in clinically significant weight loss and improved fitness are illustrated in Figure 1. The proportions of participants who achieved ≥5% weight loss differed among BMI groups (p=0.024). One third (32.7%) of participants with severe obesity achieved ≥5% weight loss, which differed significantly compared only with class I (27.5%; p=0.015), and not overweight (32.4%, p=0.064) or class II (42.2%, p=0.900), participants. The proportion of participants who achieved ≥10% weight loss also differed among BMI groups (p<0.001). More participants with severe obesity (20.0%) achieved ≥10% weight loss compared with overweight (2.9%, p=0.001) and class I (5.9%, p<0.001), but not class II (17.8%, p=0.974), participants.
Figure 1.
Clinically significant changes in weight and fitness compared between BMI groupsa, b
a Overweight: BMI 25 to <30 kg/m2; Class I obesity: BMI 30 to <35 kg/m2; Class II obesity: BMI 35 to <40 kg/m2; and Severe Obesity: BMI ≥ 40 kg/m2
b The proportion of participants who achieved improved fitness determined as >50 meter and >80 meter increase on the 6-Minute Walk Test did not differ significantly between BMI groups.
* Participants with class I obesity were significantly less likely to achieve ≥5% weight loss compared to participants with severe obesity (OR=0.57; 95% CI=0.37–0.90).
** Participants who were overweight were significantly less likely to achieve ≥10% weight loss compared to participants with severe obesity (OR=0.21; 95% CI=0.08–0.52).
*** Participants with class I obesity were significantly less likely to achieve ≥10% weight loss compared to participants with severe obesity (OR=0.26; 95% CI=0.13–0.55).
The proportion of participants who achieved clinically significant improved fitness, based on >50-meter increase on the 6-MWT, did not differ among groups (p=0.073). Similarly, the proportion of participants who achieved >80-meter increase on the 6-MWT did not differ among groups (p=0.080) (Figure 1).
Program adherence differed significantly among BMI groups (p=0.001), with participants with severe obesity attending fewer sessions (21.53 [15.43]) compared with overweight (27.74 [12.72]), class I (24.49 [14.86]), and class II (29.74 [12.84]) participants. However, post hoc pairwise comparisons revealed that participants with severe obesity did not differ from those in the overweight or class I obesity groups in terms of program adherence, but showed significantly lower program adherence compared only with class II participants (p=0.009). Study retention did not differ among BMI groups.
Discussion
People with severe obesity and serious mental illness appear to have benefited similarly to those in lower BMI groups from participation in a lifestyle intervention targeting fitness and weight loss. Not only was percentage weight loss comparable among BMI groups, but nearly one third (32.7%) of participants with severe obesity achieved ≥5% weight loss, which was higher than class I and comparable to overweight and class II obesity groups. Furthermore, one in five participants with severe obesity achieved ≥10% weight loss, representing a significantly greater proportion when compared with people in the overweight and class I obesity groups, but not those in the class II obesity group.
One quarter of participants with severe obesity achieved improved fitness based on a >50-meter increase on the 6-MWT, while about 15% achieved improved fitness based on a >80-meter increase on the 6-MWT, both of which did not differ significantly among BMI groups. Despite the smaller number of fitness trainer visits among participants with severe obesity, which differed significantly only when compared with participants with class II obesity, retention rates in the In SHAPE intervention were comparable across groups. Retention among participants with severe obesity was 79.2%, which is consistent with retention rates (78%) reported in a weight loss trial of people with severe obesity from the general population.25
Modest (≥5%) weight loss and improved fitness are associated with reduction in cardiovascular risk,16,21 which is meaningful given the elevated burden of health concerns, such as hypertension, diabetes, and metabolic syndrome that disproportionately affect people with severe obesity and serious mental illness.1,2,26,27 These positive findings associated with reduced cardiovascular risk are also consistent with other evaluations of lifestyle interventions targeting people with serious mental illness who are overweight or obese.9,10
To the authors’ knowledge, this is the first evaluation comparing the effectiveness of a lifestyle intervention among people with serious mental illness who have severe obesity, and those who are overweight or have varying levels of obesity. The findings reported here are consistent with behavioral weight management interventions in general patient populations. For example, in the Look AHEAD (Action for Health in Diabetes) trial, people with severe obesity and Type 2 diabetes experienced greater weight loss than people who were overweight, and comparable weight loss to people with class I and class II obesity.6 Further, in a randomized trial of a diet and physical activity intervention targeting adults with class II and class III obesity, people with severe obesity (class III) achieved significantly greater weight loss compared with people with class II obesity, and comparable outcomes to people with lower levels of obesity from prior lifestyle intervention studies.25 Lastly, in a primary care–based weight management program, nearly one third (31%) of people with severe obesity achieved ≥5% weight loss compared with 9% in a usual care control.28 Hence, there is mounting evidence that behavioral weight loss approaches can be effective among individuals who have severe obesity.
Thirty-one percent of participants in this study had severe obesity, representing a high proportion of individuals enrolled in a lifestyle intervention targeting fitness and weight loss (prior trials of lifestyle interventions in general patient populations reported that 22%6 and 17%29 of participants had severe obesity). This suggests that at least a subgroup of people with severe obesity and serious mental illness are interested in fitness and weight loss. This is consistent with prior findings that individuals with serious mental illness who are obese are distressed about their weight and want to lose weight.1,30
Future efforts must capitalize on this interest to lose weight and motivation to enroll in a lifestyle intervention among individuals with severe obesity and serious mental illness. Even though this study showed comparable outcomes across BMI groups, individuals with severe obesity remain at markedly higher risk of cardiovascular disease and other serious health concerns. Smoking is also a significant contributor to elevated rates of cardiovascular disease and increased mortality among people with serious mental illness.31 The In SHAPE intervention did not target smoking, yet 33.9% of participants with severe obesity were smokers, highlighting the need to explore lifestyle interventions targeting weight loss, fitness, and smoking in this at-risk group.32
Limitations
Several limitations warrant consideration. First, all participants across each of the In SHAPE trials were receiving mental health treatment, and therefore these findings cannot generalize to individuals with serious mental illness who are not currently in treatment. Second, 70% of the sample was non-Hispanic white, which limits generalizability across different minority groups. Third, only participants with baseline and 12-month data were included in the analyses, which limits generalizability to individuals who completed the study. Even though completers and dropouts did not differ on any baseline characteristics, completers may have differed owing to unmeasured characteristics. Fourth, the relatively small sample size in each of the BMI groups may have increased the risk of Type 2 error. Lastly, long-term follow-up data are not available to determine whether outcomes persist equally among BMI groups over time. In the Look AHEAD trial, at 4-year follow-up, a significant proportion of participants with severe obesity achieved long-term weight loss comparable to other BMI groups.7 Future research is necessary to determine whether long-term weight loss can be achieved similarly among people with severe obesity and serious mental illness.
Conclusions
Severe obesity is a major public health concern, and it disproportionately affects people with serious mental illness. Lifestyle interventions targeting diet and exercise offer valuable opportunities for promoting weight loss and reducing cardiovascular risk in this vulnerable group, and the current study offers additional strong evidence for implementing these programs as part of core services delivered within community mental health settings. Targeting people with severe obesity and serious mental illness, a group that is at elevated risk of cardiovascular disease, could help advance ongoing efforts aimed at reducing the dramatic life expectancy disparity impacting people with serious mental illness. These findings provide strong support for the inclusion of individuals with severe obesity in lifestyle interventions targeting fitness and weight loss in people with serious mental illness.
Acknowledgments
This study was supported by grants from CDC (CDC U48DP001935-0) and the National Institute of Mental Health (R01 MH078052 and R01 MH089811-01). Additional support was received from the CDC Health Promotion and Disease Prevention Research Center at Dartmouth (Cooperative Agreement Number U48DP005018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Dickerson FB, Brown CH, Kreyenbuhl JA, et al. Obesity among individuals with serious mental illness. Acta Psychiatrica Scandinavica. 2006;113(4):306–313. doi: 10.1111/j.1600-0447.2005.00637.x. http://dx.doi.org/10.1111/j.1600-0447.2005.00637.x. [DOI] [PubMed] [Google Scholar]
- 2.Allison DB, Newcomer JW, Dunn AL, et al. Obesity among those with mental disorders: a National Institute of Mental Health meeting report. Am J Prev Med. 2009;36(4):341–350. doi: 10.1016/j.amepre.2008.11.020. http://dx.doi.org/10.1016/j.amepre.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 3.Daumit GL, Clark JM, Steinwachs DM, Graham CM, Lehman A, Ford DE. Prevalence and correlates of obesity in a community sample of individuals with severe and persistent mental illness. J Nerv Ment Dis. 2003;191(12):799–805. doi: 10.1097/01.nmd.0000100923.20188.2d. http://dx.doi.org/10.1097/01.nmd.0000100923.20188.2d. [DOI] [PubMed] [Google Scholar]
- 4.Druss BG, Zhao L, Von Esenwein S, Morrato EH, Marcus SC. Understanding excess mortality in persons with mental illness: 17-year follow up of a nationally representative U.S. survey. Med Care. 2011;49(6):599–604. doi: 10.1097/MLR.0b013e31820bf86e. http://dx.doi.org/10.1097/MLR.0b013e31820bf86e. [DOI] [PubMed] [Google Scholar]
- 5.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- 6.Unick JL, Beavers D, Jakicic JM, et al. Effectiveness of Lifestyle Interventions for Individuals With Severe Obesity and Type 2 Diabetes Results from the Look AHEAD trial. Diabetes care. 2011;34(10):2152–2157. doi: 10.2337/dc11-0874. http://dx.doi.org/10.2337/dc11-0874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unick JL, Beavers D, Bond DS, et al. The long-term effectiveness of a lifestyle intervention in severely obese individuals. Am J Med. 2013;126(3):236–242. doi: 10.1016/j.amjmed.2012.10.010. http://dx.doi.org/10.1016/j.amjmed.2012.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cabassa L, Ezell J, Lewis-Fernandez R. Lifestyle interventions for adults with serious mental illness: a systematic literature review. Psychiatr Serv. 2010;61(8):774–782. doi: 10.1176/appi.ps.61.8.774. http://dx.doi.org/10.1176/ps.2010.61.8.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daumit GL, Dickerson FB, Wang N-Y, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. 2013;368(17):1594–1602. doi: 10.1056/NEJMoa1214530. http://dx.doi.org/10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green CA, Yarborough BJH, Leo MC, et al. The STRIDE weight loss and lifestyle intervention for individals taking antipsychotic medications: a randomized trial. Am J Psychiatry. 2015;172(1):71–81. doi: 10.1176/appi.ajp.2014.14020173. http://dx.doi.org/10.1176/appi.ajp.2014.14020173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartels SJ, Pratt SI, Aschbrenner KA, et al. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. Am J Psychiatry. 2015;172(4):344–352. doi: 10.1176/appi.ajp.2014.14030357. http://dx.doi.org/10.1176/appi.ajp.2014.14030357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bartels SJ, Pratt SI, Aschbrenner KA, et al. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatr Serv. 2013;64(8):729–736. doi: 10.1176/appi.ps.003622012. http://dx.doi.org/10.1176/appi.ps.003622012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P, Version 2.0) New York: Biometric Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- 14.Van Citters AD, Pratt SI, Jue K, et al. A pilot evaluation of the In SHAPE individualized health promotion intervention for adults with mental illness. Community Ment Health J. 2010;46(6):540–552. doi: 10.1007/s10597-009-9272-x. http://dx.doi.org/10.1007/s10597-009-9272-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Gaal L, Wauters M, De Leeuw I. The beneficial effects of modest weight loss on cardiovascular risk factors. Int J Obes Metab Disord. 1997;21(Suppl 1):S5–9S. [PubMed] [Google Scholar]
- 16.Blackburn G. Effect of degree of weight loss on health benefits. Obes Res. 1995;3(S2):211s–216s. doi: 10.1002/j.1550-8528.1995.tb00466.x. http://dx.doi.org/10.1002/j.1550-8528.1995.tb00466.x. [DOI] [PubMed] [Google Scholar]
- 17.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34(7):1481–1486. doi: 10.2337/dc10-2415. http://dx.doi.org/10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeffery RW, Epstein LH, Wilson GT, Drewnowski A, Stunkard AJ, Wing RR. Long-term maintenance of weight loss: current status. Health Psychol. 2000;19(Suppl 1):5–16. doi: 10.1037/0278-6133.19.suppl1.5. http://dx.doi.org/10.1037/0278-6133.19.Suppl1.5. [DOI] [PubMed] [Google Scholar]
- 19.Larsson UE, Reynisdottir S. The six-minute walk test in outpatients with obesity: reproducibility and known group validity. Physiotherapy Res Int. 2008;13(2):84–93. doi: 10.1002/pri.398. http://dx.doi.org/10.1002/pri.398. [DOI] [PubMed] [Google Scholar]
- 20.Beriault K, Carpentier AC, Gagnon C, et al. Reproducibility of the 6-minute walk test in obese adults. Int J Sports Med. 2009;30(10):725–727. doi: 10.1055/s-0029-1231043. http://dx.doi.org/10.1055/s-0029-1231043. [DOI] [PubMed] [Google Scholar]
- 21.Rasekaba T, Lee AL, Naughton MT, Williams TJ, Holland AE. The six-minute walk test: a useful metric for the cardiopulmonary patient. Intern Med J. 2009;39(8):495–501. doi: 10.1111/j.1445-5994.2008.01880.x. http://dx.doi.org/10.1111/j.1445-5994.2008.01880.x. [DOI] [PubMed] [Google Scholar]
- 22.Springer L, Murphy R, Enright M, LaDuca F. CardioChek PA technical bulletin: clinical performance verification of the CardioChek PA test system. Indianapolis, IN: Polymer Technology Systems, Inc; 2010. [Google Scholar]
- 23.Allison DB, Mentore JL, Heo M, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry. 1999;156(11):1686–1696. doi: 10.1176/ajp.156.11.1686. [DOI] [PubMed] [Google Scholar]
- 24.Taylor D, McAskill R. Atypical antipsychotics and weightgain—a systematic review. Acta Psychiatrica Scandinavica. 2000;101(6):416–432. doi: 10.1034/j.1600-0447.2000.101006416.x. http://dx.doi.org/10.1034/j.1600-0447.2000.101006416.x. [DOI] [PubMed] [Google Scholar]
- 25.Goodpaster BH, DeLany JP, Otto AD, et al. Effects of diet and physical activity interventions on weight loss and cardiometabolic risk factors in severely obese adults: a randomized trial. JAMA. 2010;304(16):1795–1802. doi: 10.1001/jama.2010.1505. http://dx.doi.org/10.1001/jama.2010.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8(9):605–619. doi: 10.1038/oby.2000.79. http://dx.doi.org/10.1038/oby.2000.79. [DOI] [PubMed] [Google Scholar]
- 27.Park Y-W, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2003;163(4):427–436. doi: 10.1001/archinte.163.4.427. http://dx.doi.org/10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ryan DH, Johnson WD, Myers VH, et al. Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana Obese Subjects Study. Arch Intern Med. 2010;170(2):146–154. doi: 10.1001/archinternmed.2009.508. http://dx.doi.org/10.1001/archinternmed.2009.508. [DOI] [PubMed] [Google Scholar]
- 29.Diabetes Prevention Program Research Group. The Diabetes Prevention Program: baseline characteristics of the randomized cohort. Diabetes Care. 2000;23(11):1619–1629. doi: 10.2337/diacare.23.11.1619. http://dx.doi.org/10.2337/diacare.23.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strassnig M, Brar JS, Ganguli R. Self-reported body weight perception and dieting practices in community-dwelling patients with schizophrenia. Schizophr Res. 2005;75(2):425–432. doi: 10.1016/j.schres.2004.04.007. http://dx.doi.org/10.1016/j.schres.2004.04.007. [DOI] [PubMed] [Google Scholar]
- 31.McClave AK, McKnight-Eily LR, Davis SP, Dube SR. Smoking characteristics of adults with selected lifetime mental illnesses: results from the 2007 National Health Interview Survey. Am J Public Health. 2010;100(12):2464–2472. doi: 10.2105/AJPH.2009.188136. http://dx.doi.org/10.2105/AJPH.2009.188136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aschbrenner KA, Brunette MF, McElvery R, et al. Cigarette smoking and interest in quitting among overweight and obese adults with serious mental illness enrolled in a fitness intervention. J Nerv Ment Dis. 2015;203(6):1–4. doi: 10.1097/NMD.0000000000000309. http://dx.doi.org/10.1097/NMD.0000000000000309. [DOI] [PMC free article] [PubMed] [Google Scholar]