Abstract
Rationale
Although observational and experimental studies have shown that volunteering is linked with better mental health, physical health, and health behaviors, no studies have examined whether volunteering is associated with patterns of health care use.
Objective
The purpose of this study was to prospectively examine whether volunteering was associated with a greater use of preventive health care services, but fewer doctor visits and nights spent in the hospital.
Methods
Participants (n=7,168) were drawn from the 2006 wave of the Health and Retirement Study, a nationally representative panel study of American adults over the age of 51, and tracked for one wave (2 years). Logistic regression and generalized linear models were used for analyses. Results. In analyses that adjusted for sociodemographic factors and baseline health, volunteers were 30% more likely to receive flu shots (OR=1.30, 95% CI=1.16–1.47), 47% more likely to receive cholesterol tests (OR=1.47, 95% CI=1.24–1.74); female volunteers were 53% more likely to receive mammograms/x-rays (OR=1.53, 95% CI=1.28–1.83) and 21% more likely to receive Pap smears (OR=1.21, 95% CI=1.03–1.41); male volunteers were 59% more likely to receive prostate exams (OR=1.59, 95% CI=1.29–1.95). In a model that adjusted for sociodemographic factors, volunteers spent 38% fewer nights in the hospital (RR=0.62, 95% CI=0.52–0.76), however volunteering was not associated with frequency of doctor visits (RR=0.94, 95% CI=0.87–1.02). The association between volunteering and number of nights spent in the hospital was minimally affected after adjusting for potential confounding (baseline health) and explanatory variables (health behaviors, social integration, stress, positive psychological factors, personality).
Conclusion
This is the first known study to examine the association between volunteering and health care use. If future studies replicate these findings, the results may be used to inform the development of new strategies for increasing preventive health screenings, lowering health care use and costs, and enhancing the health of older adults.
Keywords: volunteering, volunteer, health care use, physician visits, preventive health screening, psychological, aging
Introduction
The United States has a rapidly aging population. People over the age of 65 currently represent 13.7% of the population, and by the year 2050, this is estimated to double (United States Census Bureau; Vincent and Velkoff, 2010). The average annual health expenditure is $3,931 for people under the age of 65 and $10,082 for people over the age of 65 (Kashihara and Carper, 2012). As the number of older adults continuously increases, our aging population will likely put a significant strain on our health care system. Therefore, it is important to identify feasible and low cost interventions to help alleviate this strain.
Among the more expensive health care costs are hospital stays. Older adults (65+) account for 34% of hospital stays and 41% of hospital expenditures (Pfuntner et al., 2013). Each hospital stay for an adult aged 65–84 costs approximately $12,300 (Pfuntner et al., 2013). Physician visits also represent non-trivial expenses, averaging $218 per visit (Davis and Carper, 2012). A related issue is the underuse of preventive health care services among older adults. Less than 30% of adults aged 50–64 and less than 50% of adults over the age of 65 are up-to-date with core preventive services that could help improve health (Center for Disease Control, 2011; Department of Health and Human Services, 2010; Maciosek et al., 2010).
Volunteering and health
Volunteering, or donating time to nonprofit organizations (Wilson, 2000), may be an ideal low-cost strategy to help improve health among older adults. In 2012, 64.5 million volunteers in the US (26.5% of the population) provided 7.9 billion hours of service, worth an estimated $175 billion (Corporation for National & Community Service, n.d.). As summarized in recent reviews, volunteering is associated with better physical health outcomes (Konrath, 2014; Konrath and Brown, 2013). For example, compared to non-volunteers, volunteers report engaging in fewer health risk behaviors (e.g., smoking, drinking, sedentary lifestyles; Harris and Thoresen, 2005; Musick et al., 1999; Shmotkin et al., 2003). Volunteers also have better subjective health (Lum and Lightfoot, 2005; Musick and Wilson, 2003; Piliavin and Siegl, 2007) and randomized trials designed to increase people’s volunteering behavior demonstrate causal effects of volunteering on increased physical activity, fewer functional limitations, and a healthier profile of cardiovascular biomarkers (e.g., inflammatory markers and cholesterol; Fried et al., 2004; Hong and Morrow-Howell, 2010; Schreier et al., 2013; Tan, Xue, Li, Carlson, & Friend, 2006). Ultimately, volunteers have a lower mortality risk in prospective studies, even when controlling for plausible confounds such as prior health status (Harris and Thoresen, 2005; Konrath et al., 2012; Musick et al., 1999; Okun, Yeung, & Brown, 2013). There is much research on volunteering and health, however, we know of no research that has examined how volunteers use health care services, both as preventive measures (health behaviors) and as responses to illnesses (health outcomes). We address these questions in the current study.
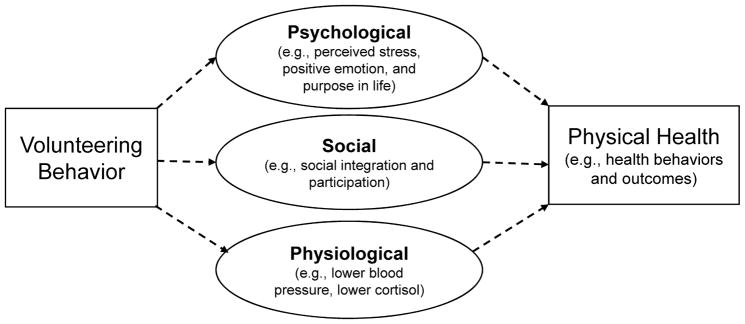
Why might volunteering be associated with healthier lifestyle choices and better physical health? Scholars have a number of theories, ranging from psychological to social to physiological (see Figure 1). There is currently no consensus in the literature about which explanation is best, and of course, each of them likely works together with the others in complex ways to promote healthy choices and better physical health outcomes.
Figure 1.
Potential explanations for how volunteering may affect physical health outcomes
a) Psychological
First, there may be internal characteristics of volunteers themselves, or psychological experiences that result from volunteering, that can help to explain why volunteering predicts better health outcomes. For example, people with relatively fewer stressful events in their lives may find it easier to make the time to volunteer in the first place, and those with more stressful events may be so depleted from trying to deal with them that they do not have extra psychological resources to devote to nonprofit organizations. These stressed out people may also have poorer health outcomes.
Another potential psychological explanation is that volunteers experience more positive emotions, psychological well-being, and less depression, when compared to non-volunteers (Meier and Stutzer, 2008; Windsor, Anstey, & Rodgers, 2008; Wheeler et al., 1998). Since positive emotions are associated with stronger immune systems (Dillon, Minchoff, & Baker, 1985), better cardiovascular health (Boehm & Kubzansky, 2012; Fredrickson & Levenson, 1998), and a lower mortality risk (Chida & Steptoe, 2008), positive psychological states could be one potential explanations for the health benefits of volunteering.
In particular, volunteering appears to buffer against a low sense of purpose in life, especially among older adults who lack social positions in society or “role-identities” (Greenfield & Marks, 2004). Higher purpose in life has been linked with an array of health advantages such as increased longevity, decreased risk of heart attacks and strokes, and increased use of preventive health services and less use of illness-based health services (Boyle, Barnes, Buchman, & Bennett, 2009; Kim, Strecher, & Ryff, 2014; Kim, Sun, Park, & Peterson, 2013; Kim, Sun, Park, Kubzansky, & Peterson, 2013). If volunteering increases a person’s purpose in life, this increase in purpose may lead to a higher will to live, which in turn may lead to healthier lifestyle choices and better health.
Finally, people who choose to volunteer have different personalities than those who do not; volunteers score higher on agreeableness and extraversion than non-volunteers (Carlo et al., 2005; Elshaug & Metzer, 2010). In addition, although some studies find null or minimal associations between conscientiousness and volunteering (Carlo et al., 2005; Elshaug & Metzer, 2010), studies of older adults find that the relationship between conscientiousness and volunteering becomes larger during retirement, when conscientious people channel their energies outside of the workplace (Mike, Jackson, & Oltmanns, 2014). It is thus possible that the health effects of volunteering are to some extent, explained by personality differences between volunteers and non-volunteers (King et al., 2014).
Potential social explanations
Volunteering may also affect health by enriching people’s social networks and participation, which have been linked with a variety of salubrious outcomes (Smith & Christakis, 2008; Berkman, Glass, Birssette, and Seeman, 2000). Indeed, one study found that older adult volunteers experienced an increase in both perceived social support and the number of social connections in the months after starting to volunteer, while control group participants declined in both of these (Fried et al., 2004). With larger social networks it is possible that volunteers would be more likely to see or hear about healthy behaviors such as getting preventive health care screenings. More social interactions could also increase the chance of someone making healthy suggestions, giving advice, or actually working together on a healthy lifestyle goal.
Potential physiological explanations
Scholars theorize that volunteering may help people to regulate their stress (Brown & Okun, 2013), but there is currently limited direct physiological evidence for this hypothesis. If volunteering does increase physiological resilience to stress, it may have the added benefit of making volunteers feel more energetic and able to prioritize their time and effort into making healthy lifestyle choices.
The current study
In the current study, we wondered whether volunteering at one time point would be associated with the later use of health care services, both preventively (i.e. as a healthy lifestyle choice), and because of illness (i.e. as a health outcome). Research has clearly shown that volunteering is associated with improved health behaviors, physical health, and longevity, but no study to our knowledge has examined the health care use patterns of volunteers versus non-volunteers. This research gap is important to examine for both practical and theoretical reasons. Practically, examining this gap may provide a potential avenue for increasing preventive health care service use and reducing illness-based health care use. Theoretically, examining this gap may lead to new information about how and why volunteers are healthier and live longer than non-volunteers.
Based on previous research, we hypothesized that volunteering would be associated with more preventive doctor visits (e.g., flu shots, cholesterol tests), but less illness-based health care use (e.g., doctor visits, nights in the hospital). We examined this hypothesis using a nationally representative sample of Americans aged 51+. We examined the association between volunteering and health care use after controlling for a wide range of covariates including: demographic factors, baseline health, health behaviors, and health insurance status. We further considered whether psychological factors (e.g., perceived stress, positive psychological functioning, personality traits) or social factors (e.g., social integration or participation), all of which have previously been linked with both volunteering and health, might account for the relationship between volunteering and health care use. If controlling for these factors significantly reduces this relationship, this would be evidence that they are potential explanatory pathways. Because we did not have real-time physiological measures of how volunteering affects stress regulation in the moment, we could not control for such variables, but we return to this potential explanation in the discussion section.
Method
Study Design and Sample
The Health and Retirement Study (HRS) is an ongoing nationally representative panel study of US adults aged 51 and older that has interviewed Americans every two years since 1992 (Sonnega et al., 2014). The HRS is sponsored by the National Institute on Aging and is conducted by the University of Michigan. Starting in 2006, a random 50% of HRS respondents were assigned to undergo an enhanced face-to-face interview. After the interview, interviewers left behind self-report psychological questionnaires, which respondents returned by mail to the University of Michigan. The response rate for the leave-behind questionnaire was 90% and the final sample consisted of 7,168 respondents.
The average age of respondents at baseline was 69 years (SD = 9.84). Respondents tended to be female (58%) and married (65%). Most had a high school degree (55%) or attended some college (26%). Respondents identified as being European-American (78%), African-American (13%), Hispanic (7%), or “Other” (1%). Table S1 describes the rest of the descriptive statistics.
The HRS website provides thorough documentation about the protocol, instrumentation, and complex sampling strategy (http://hrsonline.isr.umich.edu/). The study used de-identified, publicly available data; therefore, the Institutional Review Board at Harvard University exempted it from review.
Volunteer Measurement
In 2006 HRS asked, “Have you spent any time in the past 12 months doing volunteer work for religious, educational, health-related or other charitable organizations?” The HRS first asked a question about volunteering in 1998, however, we start with the 2006 wave as baseline because it was the first year that HRS included covariates that were crucial to our analyses. We wanted to control for variables that co-occurred with the volunteering variable. Then HRS asked how many hours a respondent volunteered, if applicable, in 50-hour intervals, up to 200 hours. The distribution of time that people in our sample volunteered was: 64.13% (0 hours), 14.52% (1–50 hours), 8.57% (51–100 hours), 6.38% (101–200 hours), and 6.40% (200+ hours). However, like most studies in this area of research, the analyses reported in this study treated volunteering as a binary variable (volunteer or non-volunteer). In the supplemental materials, analyses are reported with volunteering split into the five 50-hour groups.
Preventive Health Care Use Measurement
Use of preventive health care was measured in 2008. Each respondent was asked gender-specific questions regarding use (yes/no) of preventive health care services over the last two years (2006–2008). HRS asked about five preventive measures recommended by either the Centers for Disease Control (CDC) or the United States Preventive Services Task Force (USPSTF). HRS asked respondents: In the last two years, have you had any of the following medical tests or procedures: A flu shot? A blood test for cholesterol? A mammogram or X-ray of the breast to search for cancer? A Pap smear? An examination of your prostate to screen for cancer? The HRS preventive measures were evaluated by benchmarking them against other national surveys and are highly reliable and valid (Jenkins, Ofstedal, and Weir, 2008).
To identify visits that were made in the service of primary prevention, the number of respondents in our analyses changed depending on which preventive service was examined. For example, analyses for the Pap smear used only data from women with no history of cancer. Sensitivity analyses comparing models with and without adjustment for the relevant disease (e.g., including and excluding women with a history of cancer in the Pap smear analyses) found little difference in the estimated effects.
Doctor Visit and Overnight Hospital Visit Measurements
The number of doctor visits between 2006 and 2008 was assessed using data from the 2008 wave of HRS: “Aside from any hospital stays or outpatient surgery, how many times have you seen or talked to a medical doctor about your health, including emergency room or clinic visits in the last two years?” The number of nights spent in the hospital was assessed in the same way except respondents were asked “Have you been a patient in a hospital overnight?” If the respondent answered “no,” the respondent was assigned a value of zero. If the respondent answered “yes,” the respondent was then asked, “How many nights were you a patient in the hospital?” These items have been used to measure the frequency of doctor visits in other studies (Kim et al., 2014; McWilliams et al., 2007). Self-reported health care use shows substantial agreement with both administrative claims and medical records (Cleary and Jette, 1984; Reijneveld and Stronks, 2001; Ritter et al., 2001).
Baseline Covariates
All covariates were collected at baseline in 2006. We controlled for potential demographic and health confounds. Sociodemographic covariates included: age, gender, race/ethnicity (White, Black, Hispanic, other), marital status (married/not married), educational attainment (no degree, GED or high school diploma, college degree or higher), total wealth in U.S. dollars (<25,000; 25,000–124,999; 125,000–299,999; 300,000–649,999; >650,000—based on quintiles of the score distribution), and health insurance status (yes/no).
We also controlled for two measures of baseline health including a 23-item measure of functional status and an index of eight major chronic illnesses. Physical functioning was assessed using items adapted from scales developed by Rosow and Breslau (1966), Nagi (1976), Katz, Ford, Moskowitz, Jackson, and Jaffe (1963), and Lawton and Brody (1969). Physical functioning was conceptualized as a multidimensional construct that assessed general mobility, large-muscle functioning, gross motor skills, fine motor skills, and the ability to execute a variety of activities of daily living and instrumental activities of daily living. Respondents were asked if they experienced difficulty with activities such as running or jogging a mile, climbing stairs, bathing, and getting up from a chair. The present analyses used a count of reported limitations, where higher values indicated more limitations. The chronic illness index was a self-report of a doctor’s diagnosis concerning eight major medical conditions: (1) high blood pressure, (2) diabetes, (3) cancer or malignant tumor of any kind (excluding minor skin cancer), (4) lung disease, (5) heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems, (6) emotional, nervous, or psychiatric problems, (7) arthritis or rheumatism, and (8) stroke.
Health behaviors included smoking status (never, former, current), exercise frequency (never, 1–4 times per month, more than once a week), and alcohol consumption frequency (abstinent, less than 1–2 days per month, 1–2 days per week, and 3+ days per week). Self-reported health measures used in HRS have been rigorously assessed for their validity and reliability (Fisher et al., 2005; Jenkins et al., 2008).
We also controlled for potential psychological or social explanations of the relationship between volunteering and health (Figure 1). Chronic stress was defined as the sum of the presence of 7 enduring events that lasted for more than 12 months and were perceived as stressful (M = 1.50, SD = 0.50, α = 0.66). Example items included “Ongoing physical or emotional problems (in spouse or child),” “Ongoing problems with alcohol or drug use in family member.” Purpose in life was measured using the purpose in life subscale of the Ryff Psychological Well-Being Scales (M = 4.52, SD = 0.93, α = 0.75; Ryff and Keyes, 1995). Positive affect was measured using a six-item scale that was developed for use in nationally representative datasets (M = 3.58, SD = 0.69, α = 0.91). Big Five Personality Traits were measured using the Midlife Development Inventory (MIDI) Personality Scales (Lachman & Weaver, 1997; openness (M = 2.93, SD = 0.55, α = 0.79), conscientiousness (M = 3.34, SD = 0.48, α = 0.67), extraversion (M = 3.20, SD = 0.55, α = 0.76), agreeableness (M = 3.52, SD = 0.47, α = 0.78), neuroticism (M = 2.06, SD = 0.60, α = 0.71).
Social participation was measured by summing eight social activities (M = 4.03, SD = 1.71, α = 0.62), and social integration (M = 2.71) was measured using a 1-item measure that asked respondents to answer the following question on a 6-point Likert scale, “Not including attendance at religious services, how often do you attend meetings or programs of groups, clubs, or organizations that you belong to?”
The chronic stress scale and social participation scale have lower than ideal Cronbach alpha’s. However, these scales were created as counts of events and not necessarily constructed to have high internal consistency. Smith et al. (2013) provide further information about how these psychosocial factors were measured and constructed.
Statistical Analyses
We used logistic regression in the analyses that examined preventive health care use. For this set of analyses, all results can be interpreted as the change in odds of obtaining a preventive service when comparing volunteers against non-volunteers. Logits were converted into odds ratios (ORs) for ease of interpretation. In analyses that examined the association between volunteering and preventive health care services, we used a simpler model because we only included factors that have been repeatedly identified in the literature as theoretically justified covariates. Therefore, in preventive health care service analyses, we controlled factors that were from the core sociodemographic model, which included: age, race/ethnicity, marital status, education level, total wealth, and insurance status, along with measures of baseline health (an index of eight major chronic illnesses and a 23-item measure of physical functioning).
For the analyses that examined frequency of doctor visits and numbers of nights spent in the hospital, we used a generalized linear model with a negative binomial distribution and log link rather than an ordinary least squares regression. This statistical method appropriately models count data that have overdispersion and a skewed distribution. Due to the non-linear nature of the model, the estimated β coefficients were not directly interpretable. Therefore, to obtain more easily interpretable results, the coefficients created by the model were exponentiated into rate ratio (RR) estimates using the eform command in Stata. We used HRS sampling weights in this study to account for the complex multistage probability survey design. Stata (version 13) was used in all analyses. We conducted multiple generalized linear models to test whether volunteering was associated with fewer doctor visits and fewer number of nights spent in the hospital. We examined the impact of the risk factors by first creating a minimally adjusted model that controlled only for age (Model 1). Model 2, the core model, adjusted for age, gender, race/ethnicity, marital status, education level, total wealth, and insurance status. Five additional models were created; Model 3–core model + baseline health (index of eight major chronic illnesses and functional status), Model 4–core model + health behaviors (smoking, exercise, and alcohol use); Model 5–core model + social integration (social participation, social integration); Model 6–core model + stress (chronic stressors); Model 7–core model + personality factors (openness, conscientiousness, extraversion, agreeableness, neuroticism), Model 8–core model + positive psychological factors (purpose in life, positive affect); Model 9 included all covariates. This fully adjusted model is likely over-adjusted and underestimates the true association between volunteering and health care use.
Missing Data
The overall item non-response rate was 4.36%, however, data were missing across many variables. Thus, a complete case analysis (i.e. using data only from respondents with complete data on all variables) resulted in a 7.45%–37.89% loss of respondents, depending on which analysis was run (e.g., analyses examining preventive flu shots only had 7.45% of missing data, while nights spent in the hospital had 37.89% missing data). Therefore, to obtain less biased estimates, a multivariate normal multiple imputation was used to impute missing data. The “mi estimate” command in Stata was used to create 10 datasets and results were stable across these imputations. We therefore used the dataset with multiple imputation for all analyses because this technique provides a more accurate estimate of association than other methods of handling missing data (Little and Rubin, 2002).
Results
Volunteering and Use of Preventive Health Care Services
In models that adjusted for age, gender, race/ethnicity, marital status, educational attainment, total wealth, insurance status, chronic illnesses, and functional status (see Table 1), volunteers (compared to non-volunteers) had 30% higher odds of obtaining flu shots (OR=1.30, 95% CI=1.16–1.47), and 47% higher odds of obtaining cholesterol tests (OR=1.47, 95% CI=1.24–1.74). Further, women who volunteered had 53% higher odds of obtaining mammograms/x-rays (OR=1.53, 95% CI=1.28–1.83), and 21% higher odds of obtaining Pap smears (OR=1.21, 95% CI=1.03–1.41), while men who volunteered had a 59% higher odds of obtaining prostate exams (OR=1.59 95% CI=1.29–1.95).
Table 1.
Odds ratios for the association between volunteering and preventive health care services (adjusted for sociodemographic factors and baseline health)a
| Health Service Measure | n | Adjusted OR (95% CI) | P-value | Prevalence |
|---|---|---|---|---|
| Preventive flu shot | 7,168 | 1.30 (1.16–1.47) | <.001 | 64.58% |
| Cholesterol test | 5,160 | 1.47 (1.24–1.74) | <.001 | 80.63% |
| Mammogram / X-ray of breasts | 3,535 | 1.53 (1.28–1.83) | <.001 | 70.52% |
| Pap smear | 3,535 | 1.21 (1.03–1.41) | .018 | 47.53% |
| Prostate exam | 2,534 | 1.59 (1.29–1.95) | <.001 | 68.38% |
All models controlled for the following covariates: age, race/ethnicity, marital status, education level, total wealth, insurance, chronic illnesses, functional status
Volunteering and Frequency of Doctor Visits
The average number of doctor visits over the two-year follow-up period was 10.51 (SD=14.79). Findings from the core model, which adjusted for all sociodemographic factors, indicated that volunteering was not associated with frequency of doctor visits, RR=0.94, 95% CI=0.87–1.02; Table 2, Model 2). The lack of an association between volunteering and doctor visits remained in all of the models (Table 2, Models 3–9).
Table 2.
Rate ratios for the association between volunteering and doctor visits.
| Model | Covariates | Adjusted RR (95% CI) | P-value |
|---|---|---|---|
| 1 | Age adjusted | 0.94 (0.86–1.01) | 0.107 |
| 2 | Demographic factors (age, gender, race/ethnicity, marital status, education level, total wealth, insurance) | 0.94 (0.87–1.02) | 0.122 |
| 3 | Demographics + baseline health (index of major chronic illnesses, functional status) | 1.03 (0.95–1.11) | 0.515 |
| 4 | Demographics + health behaviors (smoking, exercise, alcohol use) | 0.99 (0.91–1.07) | 0.778 |
| 5 | Demographics + social integration (social integration: social integration, social participation) | 0.93 (0.85–1.02) | 0.117 |
| 6 | Demographics + stress (chronic stressors) | 0.96 (0.89–1.04) | 0.345 |
| 7 | Demographics + positive psych (purpose in life, positive affect) | 0.99 (0.91–1.08) | 0.867 |
| 8 | Demographics + personality factors (openness, conscientiousness, extraversion, agreeableness, neuroticism) | 0.97 (0.90–1.05) | 0.446 |
| 9 | All of the above | 1.00 (0.92–1.10) | 0.886 |
Volunteering and Frequency of Nights Spent in the Hospital
The average number of nights spent in the hospital over the two-year follow-up was 2.38 (SD=8.11). Compared to non-volunteers, people who volunteered spent 38% fewer nights in the hospital (RR=0.62, 95% CI=0.52–0.76; Table 3, Model 2). The association between volunteering and number of nights in the hospital was attenuated but remained significant in all of the subsequent covariate models (Table 3, Models 3–9).
Table 3.
Rate ratios for the association between volunteering and number of nights spent in the hospital.
| Model | Covariates | Adjusted RR (95% CI) | P-value |
|---|---|---|---|
| 1 | Age adjusted | 0.56 (0.45–0.70) | <0.001 |
| 2 | Demographic factors (age, gender, race/ethnicity, marital status, education level, total wealth, insurance) | 0.62 (0.52–0.76) | <0.001 |
| 3 | Demographics + baseline health (index of major chronic illnesses, functional status) | 0.73 (0.62–0.87) | 0.001 |
| 4 | Demographics + health behaviors (smoking, exercise, alcohol use) | 0.73 (0.60–0.89) | 0.002 |
| 5 | Demographics + social integration (social integration: social integration, social participation) | 0.65 (0.52–0.80) | <0.001 |
| 6 | Demographics + stress (chronic stressors) | 0.66 (0.55–0.79) | <0.001 |
| 7 | Demographics + positive psych (purpose in life, positive affect) | 0.70 (0.58–0.85) | <0.001 |
| 8 | Demographics + personality factors (openness, conscientiousness, extraversion, agreeableness, neuroticism) | 0.66 (0.54–0.80) | <0.001 |
| 9 | All of the above | 0.78 (0.64–0.96) | 0.019 |
Discussion
Using a prospective and nationally representative sample of older U.S. adults, the current study found that volunteers (compared to non-volunteers) were more likely to use preventive health care services but spent fewer nights in the hospital. Considering that each hospital stay for an adult aged 65–84 costs approximately $12,300 (Pfuntner et al., 2013), this has important implications. Taken together, these results suggest that volunteers may actively pursue preventive health services, and perhaps as a result they may become healthier, which in turn may lead to fewer number of nights spent in the hospital. However, we did not test this hypothesis directly, so the specific causal path between these variables remains unknown. We also found that volunteering was not associated with physician visits. This may be because doctor visits could include both preventive health screenings and check-ups, and illness-related visits. Although the HRS measure does not distinguish between those different reasons for visiting a doctor, future studies should do so.
This study contributes to a literature that has focused mainly on the associations between volunteering and mental health, physical health, and mortality risk—with no research to our knowledge examining the implications of these outcomes in terms of health care use. Given the rapidly aging population and the rising costs of health care services, it is important to explore low cost methods of reducing health care expenditures while maintaining optimal health.
Based on our theoretical model, we also controlled for plausible psychological and social variables that scholars have suggested may help to explain the link between volunteering and health (Figure 1). Results showed that adjusting for these factors did not meaningfully attenuate our findings. This outcome could be for many reasons. First, the instruments we used to assess the potential mechanisms may not have adequately measured the construct of interest. Future researchers should use more fine-grained instruments.
Second, adjusting for blocks of covariates is not the most ideal method of examining mechanisms. Future researchers should more closely examine potential mechanisms that help to explain the association between volunteering and health care use using more advanced statistical methods. For example, structural equation modeling could be used so that researchers can decompose effects and simultaneously test multiple mediating pathways. However, the examination of mechanisms warrants a more thorough investigation than we can provide within the scope of this study. This study was primarily focused on providing an initial exploration into the associations between volunteering health care use, with a preliminary examination of whether certain psychological or social factors were clearly potential explanations. Future researchers should continue to investigate potential mechanisms.
Third, volunteering may work through other mechanisms that were not measured. For example, one possibility is that volunteers actively use preventive health care services because of other psychological factors that we did not capture in the current study. For example, perhaps people who volunteer are more cognizant of the detrimental effects their poor health would have on others. Prior research, showing that volunteers have more empathic traits than non-volunteers is consistent with this explanation (Penner, 2002; Wilhelm & Bekkers, 2010). It is also possible that volunteers are better at self-regulation than non-volunteers, which in turn is associated with better health behaviors and increased use of preventive health screens (Bandura, 2005). Still, controlling for conscientiousness (or any of the other personality factors) did not meaningfully alter results.
Another possibility is that volunteering experiences affect physiological systems that maximize stress resilience (Brown & Okun, 2013). This seems plausible given research on the intimate link between bonding behavior and stress regulation in humans and other mammals. For example, feeling compassion leads to an increase in the hormone oxytocin (Barazza & Zak, 2009), and oxytocin administration causes lower stress hormone (cortisol) responses and less cardiovascular reactivity to stressful situations (Heinrichs et al., 2010). So far, there has been limited direct evidence that volunteering can minimize the physiological damage from stressors. However, research finds that volunteering psychologically buffers people from work stress (Mojza & Sonnentag, 2010), and makes people feel like they have more time, even though they actually have less (Mogilner et al., 2012). So it is at least plausible that volunteering can help to attenuate the negative physical consequences of stress, thus making people feel more serene and able to focus on longer-term future planning, rather than feeling overwhelmed by immediate stressors.
Discovering an explanation for these results is essential in order for the field to advance and in order for researchers to begin outlining practical recommendations. For example, if these results are driven by the empathic personality of volunteers (which was not assessed in this study) rather than the volunteering behavior itself, interventions would focus on teaching people to focus on how their health care choices affect their loved ones. If instead these results are explained by the fact that volunteers have better self-control than non-volunteers, then interventions might use volunteering behavior as a practice grounds for developing and practicing habits of self-control (e.g., waking up early, planning transportation ahead of time, inhibiting negative responses when encountering difficult clients of volunteering, etc.). Of course, there are likely to be multiple explanations that intertwine with each other, but understanding these complex relationships is important.
Limitations and Strengths
This study had some limitations; for example, it is based on self-report, making it possible that respondents misremembered or were otherwise inaccurate in their reports of health care use. However, prior research has found that people are accurate at recalling health care use behaviors (Cleary and Jette, 1984; Reijneveld and Stronks, 2001; Ritter et al., 2001). Despite these limitations, our findings are consistent with a substantial body of research demonstrating that volunteering is linked with enhanced mental and physical health (Konrath, 2014; Konrath and Brown, 2013). This body of evidence helps temper the likelihood that findings from this study are spurious or due to mis-reported health care use, but we recommend using more objective data, such as medical records, in future studies. An additional limitation to the current study is that the Health and Retirement Study did not include information on specific types of volunteering, which could make a difference in terms of explaining some of our results. For example, volunteers who work in health care settings might be more aware of both potential health resources and also potential consequences of failing to engage in preventive health care behaviors. Type of volunteering should thus be examined in future studies of volunteering and health care use. Despite these limitations, this study had several strengths. It is the first known study to examine the association between volunteering and health care use. It also used a large, nationally representative sample, standardized, validated measures, and a prospective design that helped rule out a number of important confounds and recall bias. Future research should seek the mechanisms that help explain the health care use patterns of volunteers.
Conclusion
If future research corroborate our findings, programs designed to encourage volunteering among older adults may be warranted. These programs may offer new ways of increasing preventive health care use and decreasing illness-based health care use, which in turn may help drive down health care costs. More importantly, if these volunteer enhancement programs are optimally designed, they could simultaneously enhance society, along with the health and quality of life among the large segment of people who are moving into older adulthood (Carr, Fried, & Rowe, 2015).
Supplementary Material
Research Highlights.
Past studies show that volunteering is linked with better health and behaviors
We examined the link between volunteering and health care use two years later
Data were from a nationally representative sample of U.S. adults aged 51 and over
Volunteers were more likely to use preventive health care services
Volunteers spent fewer nights in the hospital but did not make fewer doctor visits
Acknowledgments
We thank the anonymous reviewers for their valuable comments and suggestions. We would also like to acknowledge the Health and Retirement Study, which is conducted by the Institute for Social Research at the University of Michigan, with grants from the National Institute on Aging (U01AG09740) and the Social Security Administration.
Support
The first author was supported by a grant from the NIH (T32 HL 098048) while writing this manuscript. The second author was supported by a grant from the John Templeton Foundation (#57942) while writing this manuscript.
Footnotes
Conflict of interest statement
The authors declare that they have no conflict of interest.
Role of the Sponsor
The funding sources had no influence on the design or conduct of the study; collection, management, analysis or interpretation of the data; or preparation, review, or approval of the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barraza JA, Zak PJ. Empathy toward strangers triggers oxytocin release and subsequent generosity. Annals of the New York Academy of Sciences. 2009;1167:182–189. doi: 10.1111/j.1749-6632.2009.04504.x. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Boehm JK, Kubzansky LD. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychological Bulletin. 2012;138:655–691. doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- Brown SL, Okun MA. Using the caregiver system model to explain the resilience-related benefits older adults derive from volunteering. In: Kent M, Davis MC, Reich JW, editors. The resilience handbook: Approaches to stress and trauma. New York: Routledge; 2013. pp. 169–182. [Google Scholar]
- Boyle PA, Barnes LL, Buchman AS, Bennett DA. Purpose in life is associated with mortality among community-dwelling older persons. Psychosomatic Medicine. 2009;71:574–579. doi: 10.1097/PSY.0b013e3181a5a7c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlo G, Okun MA, Knight G, Guzman MRT. The interplay of traits and motives on volunteering: Agreeableness, extraversion and prosocial value motivation. Personality and Individual Differences. 2005;38:1293–1305. [Google Scholar]
- Carr DC, Fried LP, Rowe JW. Productivity & engagement in an aging America: The role of volunteerism. 2015;144:55–67. [Google Scholar]
- Centers for Disease Control and Prevention. Healthy aging: Helping people to live long and productive lives and enjoy a good quality of life. Atlanta, GA: Center for Disease Control; 2011. Retrieved from http://stacks.cdc.gov/view/cdc/6114. [Google Scholar]
- Chida Y, Steptoe A. Positive psychological well-being and mortality: A quantitative review of prospective observational studies. Psychosomatic Medicine. 2008;70:741–756. doi: 10.1097/PSY.0b013e31818105ba. [DOI] [PubMed] [Google Scholar]
- Cleary PD, Jette AM. The validity of self-reported physician utilization measures. Medical Care. 1984;22:796–803. doi: 10.1097/00005650-198409000-00003. [DOI] [PubMed] [Google Scholar]
- Corporation for National & Community Service. Volunteering and civic engagement in the United States. New York, NY: Corporation for National & Community Service; n.d. Retrieved from: http://www.volunteeringinamerica.gov/national. [Google Scholar]
- Davis K, Carper K. Use and expenses for office-based physician visits by specialty, 2009: Estimates for the U.S. civilian noninstitutionalized population. Washington D.C: Agency for Healthcare Research and Quality; 2012. Retrieved from: http://meps.ahrq.gov/data_files/publications/st381/stat381.pdf. [Google Scholar]
- Dillon K, Minchoff B, Baker KH. Positive emotional states and enhancement of the immune system. International Journal of Psychiatry in Medicine. 1985;15:13–18. doi: 10.2190/r7fd-urn9-pq7f-a6j7. [DOI] [PubMed] [Google Scholar]
- Elshaug C, Metzer J. Personality attributes of volunteers and paid workers engaged in similar occupational tasks. The Journal of Social Psychology. 2001;141:752–763. doi: 10.1080/00224540109600586. [DOI] [PubMed] [Google Scholar]
- Fisher GG, Faul JD, Weir DR, Wallace RB. Documentation of chronic disease measures in the Heath and Retirement Study (HRS/AHEAD) Survey Research Center, Institute for Social Research; 2005. Retrieved from: http://hrsonline.isr.umich.edu/ [Google Scholar]
- Fredrickson B, Levenson RW. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cognition & Emotion. 1998;12:191–220. doi: 10.1080/026999398379718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried LP, Carlson MC, Freedman MM, Frick KD, Glass TA, Hill J, Zeger SA. A social model for health promotion for an aging population: Initial evidence on the Experience Corps model. Journal of Urban Health. 2004;81:64–78. doi: 10.1093/jurban/jth094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA, Marks NF. Formal volunteering as a protective factor for older Adults’ psychological well-being. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2004;59:S258–S264. doi: 10.1093/geronb/59.5.s258. [DOI] [PubMed] [Google Scholar]
- Harris AHS, Thoresen CE. Volunteering is associated with delayed mortality in older people: Analysis of the Longitudinal Study of Aging. Journal of Health Psychology. 2005;10:739–752. doi: 10.1177/1359105305057310. [DOI] [PubMed] [Google Scholar]
- Heinrichs M, Baumgartner T, Kirschbaum C, Ehlert U. Social support and oxytocin interact to suppress cortisol and subjective responses to psychosocial stress. Biological Psychiatry. 2003;54:1389–1398. doi: 10.1016/s0006-3223(03)00465-7. [DOI] [PubMed] [Google Scholar]
- Hong SI, Morrow-Howell N. Health outcomes of Experience Corps®: A high- commitment volunteer program. Social Science and Medicine. 2010;71:414–420. doi: 10.1016/j.socscimed.2010.04.009. [DOI] [PubMed] [Google Scholar]
- Jenkins KR, Ofstedal MB, Weir D. Documentation of health behaviors and risk factors measured in the Health and Retirement Study (HRS/AHEAD) Ann Arbor, MI: Survey Research Center, University of Michigan; 2008. Retrieved from: http://hrsonline.isr.umich.edu/sitedocs/userg/dr-010.pdf. [Google Scholar]
- Kashihara D, Carper K. National health care expenses in the U.S. civilian noninstitutionalized population, 2009. Washington D.C: Agency for Healthcare Research and Quality; 2012. Retrieved from: http://meps.ahrq.gov/mepsweb/data_files/publications/st355/stat355.pdf. [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kim ES, Sun JK, Park N, Smith J, Peterson C. Life satisfaction and frequency of doctor visits. Psychosomatic Medicine. 2014;76:86–93. doi: 10.1097/PSY.0000000000000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Strecher VJ, Ryff CD. Purpose in life and use of preventive health care services. Proceedings of the National Academy of Sciences. 2014;111:16331–16336. doi: 10.1073/pnas.1414826111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Sun JK, Park N, Peterson C. Purpose in life and reduced incidence of stroke in older adults: The Health and Retirement Study. Journal of Psychosomatic Research. 2013;74:427–432. doi: 10.1016/j.jpsychores.2013.01.013. [DOI] [PubMed] [Google Scholar]
- Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C. Purpose in life and reduced risk of myocardial infarction among older U.S. adults with coronary heart disease: A two-year follow-up. Journal of Behavioral Medicine. 2013;36:124–133. doi: 10.1007/s10865-012-9406-4. [DOI] [PubMed] [Google Scholar]
- King HR, Jackson JJ, Morrow-Howell N, Oltmanns TF. Personality accounts for the connection between volunteering and health. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2015;70:691–697. doi: 10.1093/geronb/gbu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrath S. The power of philanthropy and volunteering. In: Huppert F, Cooper CL, editors. Wellbeing: A Complete Reference Guide. Interventions and Policies to Enhance Wellbeing. West Sussex, UK: John Wiley & Sons; 2014. pp. 387–426. [Google Scholar]
- Konrath S, Brown SL. The effects of giving on givers. In: Roberts N, Newman M, editors. Handbook of Health and Social Relationships: The good, the bad, and the complicated. Washington DC, US: American Psychological Association; 2013. pp. 39–64. [Google Scholar]
- Konrath S, Fuhrel-Forbis A, Lou A, Brown S. Motives for volunteering are associated with mortality risk in older adults. Health Psychology. 2012;31:87–96. doi: 10.1037/a0025226. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The Midlife Development Inventory (MIDI) Personality Scales: Scale construction and scoring. 1997 Retrieved from http://www.brandeis.edu/departments/psych/lachman/pdfs/midi-personality-scales.pdf.
- Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Lum TY, Lightfoot E. The effects of volunteering on the physical and mental health of older people. Research on Aging. 2005;27:31–55. [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- Maciosek MV, Coffield AB, Flottemesch TJ, Edwards NM, Solberg LI. Greater use of preventive services in US health care could save lives at little or no cost. Health Affairs. 2010;29:1656–1660. doi: 10.1377/hlthaff.2008.0701. [DOI] [PubMed] [Google Scholar]
- McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Health of previously uninsured adults after acquiring Medicare coverage. Journal of the American Medical Association. 2007;298:2886–2894. doi: 10.1001/jama.298.24.2886. [DOI] [PubMed] [Google Scholar]
- Meier S, Stutzer A. Is volunteering rewarding in itself? Economica. 2008;75:39–59. [Google Scholar]
- Mike A, Jackson JJ, Oltmanns TF. The conscientious retiree: The relationship between conscientiousness, retirement, and volunteering. Journal of Research in Personality. 2014;52:68–77. doi: 10.1016/j.jrp.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogilner C, Change Z, Norton MI. Giving time gives you time. Psychological Science. 2012;23:1233–1238. doi: 10.1177/0956797612442551. [DOI] [PubMed] [Google Scholar]
- Mojza EJ, Sonnentag S. Does volunteer work during leisure time buffer negative effects of job stressors? A diary study. European Journal of Work and Organizational Psychology. 2010;19:231–252. [Google Scholar]
- Musick MA, Herzog AR, House JS. Volunteering and mortality among older adults: Findings from a national sample. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1999;54:S173–S180. doi: 10.1093/geronb/54b.3.s173. [DOI] [PubMed] [Google Scholar]
- Musick MA, Wilson J. Volunteering and depression: The role of psychological and social resources in different age groups. Social Science and Medicine. 2003;56:259–269. doi: 10.1016/s0277-9536(02)00025-4. [DOI] [PubMed] [Google Scholar]
- Nagi SZ. An epidemiology of disability among adults in the United States. The Milbank Memorial Fund Quarterly. Health and Society. 1976:439–467. [PubMed] [Google Scholar]
- Okun MA, Yeung EW, Brown S. Volunteering by older adults and risk of mortality: A meta-analysis. Psychology and Aging. 2013;28:564–577. doi: 10.1037/a0031519. [DOI] [PubMed] [Google Scholar]
- Penner L. Dispositional and organizational influences on sustained volunteerism: An interactionist perspective. Journal of Social Issues. 2002;58(3):447–467. [Google Scholar]
- Piliavin JA, Siegl E. Health benefits of volunteering in the Wisconsin Longitudinal Study. Journal of Health and Social Behavior. 2007;48:450–464. doi: 10.1177/002214650704800408. [DOI] [PubMed] [Google Scholar]
- Pfuntner A, Wier LM, Elixhauser A. Costs for hospital stays in the United States, 2010. Rockville, MD: Agency for Health Care Policy and Research; 2013. Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK179196/ [PubMed] [Google Scholar]
- Ritter PL, Stewart AL, Kaymaz H, Sobel DS, Block DA, Lorig KR. Self- reports of health care utilization compared to provider records. Journal of Clinical Epidemiology. 2001;54:136–141. doi: 10.1016/s0895-4356(00)00261-4. [DOI] [PubMed] [Google Scholar]
- Reijneveld SA, Stronks K. The validity of self-reported use of health care across socioeconomic strata: A comparison of survey and registration data. International Journal of Epidemiology. 2001;30:1407–1414. doi: 10.1093/ije/30.6.1407. [DOI] [PubMed] [Google Scholar]
- Rosow I, Breslau N. A Guttman health scale for the aged. Journal of Gerontology. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- Ryff CD, Keyes CLM. The structure of psychological well-being revisited. Journal of Personality and Social Psychology. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Schreier HM, Schonert-Reichl KA, Chen E. Effect of volunteering on risk factors for cardiovascular disease in adolescents: A randomized controlled trial. Journal of the American Medical Association Pediatrics. 2013;167:327–332. doi: 10.1001/jamapediatrics.2013.1100. [DOI] [PubMed] [Google Scholar]
- Shmotkin D, Blumstein T, Modan B. Beyond keeping active: Concomitants of being a volunteer in old-old age. Psychology and Aging. 2003;18:602. doi: 10.1037/0882-7974.18.3.602. [DOI] [PubMed] [Google Scholar]
- Smith KP, Chistakis NA. Social networks and health. Annual Reivew of Sociology. 2008;34:405–429. [Google Scholar]
- Smith J, Fisher G, Ryan L, Clarke P, House J, Weir J. Psychosocial and lifestyle questionnaire 2006–2010. Ann Arbor, MI: Survey Research Center, University of Michigan; 2013. Retrieved from: http://hrsonline.isr.umich.edu/sitedocs/userg/HRS2006-2010SAQdoc.pdf. [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, Weir DR. Cohort profile: The Health and Retirement Study (HRS) International Journal of Epidemiology. 2014;43:576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy people 2020 topics and objectives: Older adults. Washington D.C: US Department of Health and Human Services; 2010. Retrieved from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=31. [Google Scholar]
- United States Census Bureau. State & County Quick Facts. Washington D.C: US Census Burea; Retrieved from: http://quickfacts.census.gov/qfd/states/00000.html. [Google Scholar]
- Vincent G, Velkoff V. The next four decades: The older population in the United States 2010 to 2050. Washington D.C: US Census Bureau; 2010. Retrieved from: https://www.census.gov/prod/2010pubs/p25-1138.pdf. [Google Scholar]
- Wilhelm MO, Bekkers R. Helping behavior, dispositional empathic concern, and the principle of care. Social Psychology Quarterly. 2010;73:11–32. [Google Scholar]
- Wilson J. Volunteering. Annual Review of Sociology. 2000;26:215–240. [Google Scholar]
- Windsor TD, Anstey KJ, Rodgers B. Volunteering and psychological well-being among young-old-adults: How much is too much? Gerontologist. 2008;48:59–70. doi: 10.1093/geront/48.1.59. [DOI] [PubMed] [Google Scholar]
- Wheeler JA, Gorey KM, Greenblatt B. The beneficial effects of volunteering for older volunteers and the people they serve: A meta-analysis. International Journal of Aging and Human Development. 1998;47:69–79. doi: 10.2190/VUMP-XCMF-FQYU-V0JH. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.