Abstract
Introduction
The preschool years provide a unique window of opportunity to intervene on obesity-related lifestyle risk factors during the formative years of a child’s life. The purpose of this study was to assess the impact of a preschool-based obesity prevention effectiveness trial at 1-year follow-up.
Design
RCT.
Settings/participants
Primarily African American children (aged 3–5 years, N=618) attending Head Start preschool programs administered by Chicago Public Schools.
Methods
Eighteen preschools were randomly assigned in 2007–2008 to receive either: (1) a 14-week teacher-delivered intervention focused on healthy lifestyle behaviors; or (2) a 14-week teacher-delivered general health curriculum (control group).
Main outcome measures
The primary outcome, BMI, was measured at baseline, post-intervention, and 1-year follow-up. Diet and screen time behaviors were also assessed at these time points. Multilevel mixed effects models were used to test for between-group differences. Data were analyzed in 2014.
Results
Significant between-group differences were observed in diet, but not in BMI z-score or screen time at 1-year follow-up. Diet differences favored the intervention arm over controls in overall diet quality (p=0.02) and in subcomponents of diet quality, as measured by the Healthy Eating Index-2005, and in fruit intake (servings/day, excludes juice) (p=0.02). Diet quality worsened more among controls than the intervention group at 1-year follow-up.
Conclusions
The adaptation of Hip-Hop to Health Jr. produced modest benefits in diet quality, but did not significantly impact weight gain trajectory. Not unlike other effectiveness trials, this real-world version delivered by Head Start teachers produced fewer benefits than the more rigorous efficacy trial. It is important to understand and build upon the lessons learned from these types of trials so that we can design, implement, and disseminate successful evidence-based programs more widely and effectively.
Introduction
Childhood obesity disproportionately affects African American children.1 National data reflect racial/ethnic disparities in children aged as young as 2–5 years and these trends persist through adolescence.1 Healthy People 2020 includes objectives to reduce the proportion of children and adolescents who are obese.2 Therefore, identifying prevention efforts that could curb this trend should remain a priority.
The Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial was a 14-week classroom teacher-delivered intervention modeled after the Hip-Hop to Health Jr. efficacy trial.3,4 In the original efficacy trial, early childhood educators from the research team delivered the intervention.5 The efficacy trial demonstrated significantly smaller increases in BMI z-score among African American preschool children in the intervention group compared with controls at the 1- and 2-year follow-up periods.6 In order to more broadly disseminate the intervention, the authors adapted and tested the intervention for a more “real-world” application using teachers in existing Head Start classrooms to deliver the intervention. In the initial findings, assessed immediately after the intervention (post-intervention), significant between-group differences were found favoring the intervention arm in physical activity and screen time, but not in BMI or diet.5 This article examines the study’s primary outcome, which was to compare BMI z-score changes between intervention and control groups at 1-year follow-up (i.e., 1 year after post-intervention period). Diet and screen time were assessed as secondary outcomes.
Methods
Study Design, Setting, and Participants
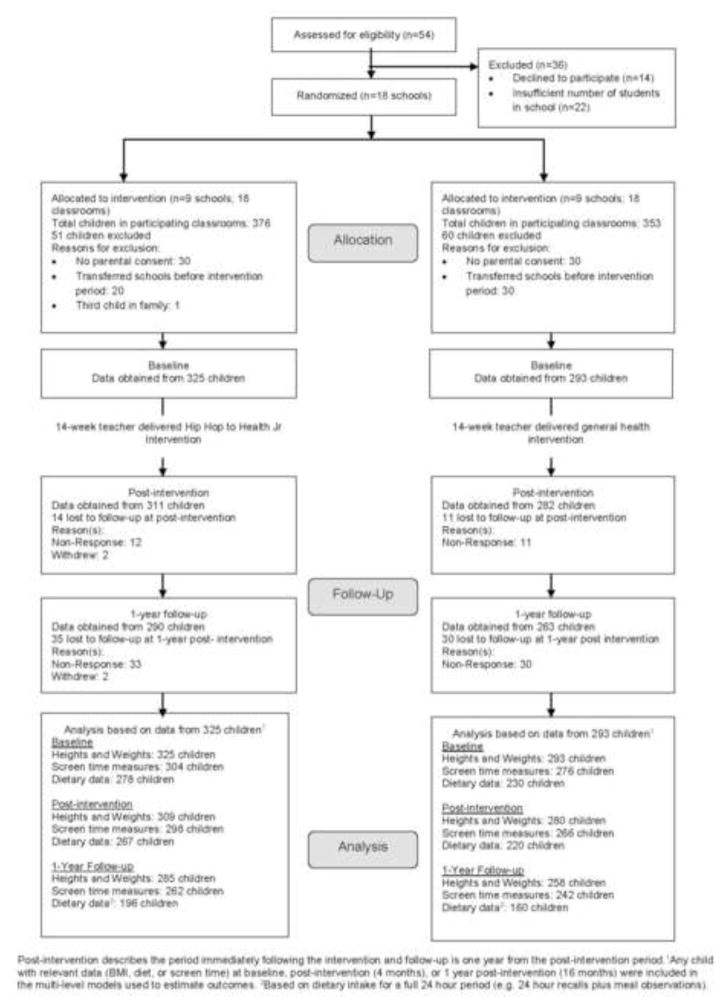
The Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial was an RCT targeting African American children aged 3–5 years from low-income households participating in Head Start. Randomization was carried out at the school level rather than at the classroom or student level in order to minimize the possibility that teachers, children, and parents in the control group would be influenced by intervention group participants. Initially, 54 Chicago Public School–administered Head Start programs in primarily African American communities were contacted. Eighteen schools agreed to participate and the remaining schools either declined to participate (n=14) or had insufficient student enrollment in the school (n=22) (Figure 1). The study design through 1-year follow-up is shown in Figure 1. The IRBs at the University of Illinois at Chicago and the Chicago Public Schools approved this study.
Figure 1.
Study flow diagram.
Post-intervention describes the period immediately following the intervention and follow-up is one year from the post-intervention period. 1 Any child with relevant data (BMI, diet, screen time) at baseline, post-intervention (4 months), or 1 year post-intervention (16 months) were included in the multi-level models used to estimate outcomes. 2 Based on dietary intake for a full 24 hour period (e.g. 24 hour recalls plus meal observations).
Seven schools were recruited during winter and spring of 2006 and were randomized in September 2006. In the following year, eleven schools were recruited over a similar time period and were randomized in September 2007. In total, eighteen schools were randomized to one of two conditions: (1) a teacher-delivered intervention curriculum; or (2) a teacher-delivered general health curriculum. There were two participating classrooms per school (n=36 classrooms) with approximately 17 children per classroom enrolled in the study at baseline (N=618 children). This sample size was determined because nine schools per randomization arm and two classrooms per school with 17 students per classroom could achieve at least 80% power to detect a small to medium effect size7 of 0.35 in BMI z-score change at the 5% significance level. Based on estimates from our efficacy trial, a between-classroom variance component of ≤ 2.5% and a between-school variance component of ≤ 2.0% were assumed. Randomization was stratified by cohort, with participating schools randomized together at the start of the school year using an allocation sequence generated in SAS, version 9.2. The data analyst who randomized the schools had no contact with school personnel or study participants.
The intervention and general health curriculum were delivered as part of classroom activities during regular classroom hours. Thus, children in intervention schools received the intervention curriculum, whereas children in the control schools received the general health curriculum. Only students whose parent or guardian provided informed consent were eligible to enroll in the study. Being enrolled in the study meant that a parent gave permission to the study to obtain study measures (e.g., BMI, diet, screen time) on his or her child (Figure 1).
The intervention curriculum aimed to improve both diet and physical activity, and decrease TV viewing.5 The intervention materials were culturally specific to the target population and considered the practices and beliefs of this audience.5 Teachers delivered this curriculum two times/week for 14 weeks. Weekly sessions were theme-based and included: (1) a 20-minute lesson on healthy eating or physical activity; and (2) a 20-minute interactive physical activity component. The names of the weekly themes were previously reported.5 Study staff supplied teachers with colorful puppets representing food groups and a CD containing two fully scripted exercise routines to aid them in curriculum delivery. In many of the food-themed lessons, children prepared simple classroom recipes and participated in food tastings. The Hip-Hop to Health Jr. intervention curriculum used in this effectiveness trial was similar to the curriculum delivered in the efficacy trial; however, modifications were made to how often the lessons were offered. To allow teachers to administer the curriculum two times/week instead of three times/week, an optional third lesson was offered to accommodate this change. The third lesson reinforced content, but did not introduce new concepts. Therefore, teachers could implement this third lesson, if time allowed. Additionally, the interactive 20-minute physical activity component was intended to be led by teachers through live demonstration. However, the level of comfort that teachers had with the physical activity component was variable, so a CD was developed, enhancing the ability of the teachers to deliver the physical activity component of the curriculum with sufficient structure and dose. Intervention materials can be accessed at www.hiphoptohealth.com.
Parents were encouraged to participate through weekly homework assignments that mirrored the intervention classroom curriculum. Parents received $5 for each completed homework submission. They were also given a copy of the physical activity CD and a weekly newsletter highlighting the weekly theme.
The general health curriculum, developed by the research investigators, focused only on general health topics and excluded all mention of diet, physical activity, and screen time. Topics included car safety, emergency procedures, dental hygiene, and immunizations. Teachers in control classrooms delivered this curriculum once/week for 14 weeks. Parents also received weekly newsletters highlighting the general health topic, but were not asked to complete homework assignments.
Participating teachers and teacher’s aides attended an initial 3-hour training session conducted by the research team. Intervention teachers and aides received three additional in-school trainings on curriculum implementation whereas control teachers and aides received one additional in-school training. Throughout the 14-week intervention period, the study coordinator met individually with intervention teachers weekly and met with control teachers monthly.
Measures
Study staff measured children’s heights and weights at each time point (i.e., baseline, post-intervention, 1-year follow-up) using a Tanita BWB-800 portable stadiometer (Tanita Corp., Arlington Heights, IL) for height and a SECA 214 digital scale (SECA, Hanover, MD) for weight. The children were weighed without shoes and in light clothing. Height (nearest 0.1 cm) and weight (nearest 0.1 kg) were measured twice and averaged for analyses. BMI percentiles for age and sex and BMI z-scores, based on the 2000 CDC Growth Charts, were calculated using a SAS program developed by CDC.8
Staff dietitians collected one 24-hour recall per parent report at each time point for each enrolled child. Twenty four–hour recalls reported by parents have been validated previously in preschool populations.9–11 To aid in recalls with staff dietitians, parents were asked to record all meals and snacks consumed by their child outside of school on a food record form provided to them. A portion size guide was given to parents to assist them in estimating portion sizes. The 24-hour recalls provided by parents captured the foods consumed by children away from school. The Nutrition Data System for Research 2007 (Nutrition Coordinating Center, University of Minnesota) was used to process all dietary data for this study.
To capture the segment of the day that children were in school, study staff observed each enrolled child during meal times (e.g., breakfast, lunch, and snack) on one school day. This combined approach (i.e., 24-hour recall plus meal observation) allowed assessment of all the foods children consumed in and out of school over a 24-hour period.12,13 Each trained observer watched two to three children during a given meal period and unobtrusively documented the amount of foods and beverages served. Foods or beverages left unconsumed on trays were labeled, measured with utensils, and weighed with a digital ounce/gram scale that was calibrated prior to each use. The amount consumed for each child was estimated by calculating the difference between the amount of food served and the amount of food not consumed.
Based on 24-hour recalls and in-school meal observations, diet quality was measured with the Healthy Eating Index 2005 (HEI-2005), which is considered a valid measure for diet quality.14,15 In addition to the food groups and nutrients that the authors previously assessed (e.g., fruits, vegetables, fiber, fat),5 diet quality was added as a measure because our intervention focused on multiple aspects of diet and aimed overall, to promote a more healthful dietary pattern. This index measures adherence to the 2005 Dietary Guidelines for Americans (DGA),16 which reflects the time period when the intervention took place. The total HEI-score (maximum 100) is derived from the sum of component scores, with higher scores reflecting better conformance to guidelines.16 The HEI-2005 components most relevant to the intervention curriculum were reported in the results. These components included: total fruit (range, 0–5), whole fruit (range, 0–5), total vegetables (range, 0–5), whole grains (range, 0–5), saturated fat (range, 0–10), and calories from solid fat, alcohol, and added sugar (SoFAAS) (range, 0–20).
To assess screen time use, parents were asked to report the amount of time (i.e., minutes/day) their child engaged in various forms of screen time on a usual school day and weekend day17 at each time point. Examples of screen time activities included watching TV or DVDs, using a computer, or playing video games. A weighted average of time spent on school and weekend days was used to estimate total screen time use. This measure has been previously examined for test–retest reliability on older school-age children (r =0.94),17,18 but not in preschool-age samples.
Statistical Analysis
For the main analyses, multilevel mixed effects models were used to properly account for repeated measures on students grouped within classrooms (n=36).19 Specifically, a random intercept and random time trend, varying across students and classrooms, were estimated to test for between-group differences in the outcome measures from baseline to 1-year follow-up. Classrooms were allowed to deviate from the overall mean; likewise, students were allowed to deviate from their classroom mean. Time was treated as a linear continuous variable (baseline, post-intervention, 1-year follow-up), and change from baseline to 1-year follow-up was estimated from these models. Any child with outcome data (i.e., BMI, diet, or screen time) at baseline (i.e., 0 months), post-intervention (i.e., 4-months), or 1-year follow-up (i.e., 16 months) was included in these models. In other words, measures at each time point contributed to fitting the models and in estimating longer-term change at 1-year follow-up. Models were adjusted for baseline age. Cohen’s d was used to estimate the effect size for BMI z-score. All analyses were conducted in 2014 using SAS, version 9.2.
Results
At 1-year follow-up, 553 of 618 children (89%; n=290 intervention, n=263 control) were reached for follow-up; 65 children (n=35 intervention, n=30 control) were unavailable for assessment at this time point (Figure 1). The control and intervention groups were similar on main demographic variables; however, children in the intervention group (50.7 months) were slightly younger than control group children (51.9 months). The majority of children were African American (94%) and 33% of children were at or above the 85th percentile for BMI (Table 1). As reported previously, parents were aged 30.9 years on average and primarily mothers (83%). Most parents had a BMI ≥ 30 kg/m2 (53%) with 18% of parents at a BMI ≥ 40 kg/m2.5
Table 1.
Characteristics of Participating Children at Baseline, Teacher-Delivered Hip-Hop to Health Jr.
| Intervention (N=325) | Control (N=293) | All (N=618) | |
|---|---|---|---|
| Female, no. (%) | 168 (52%) | 161 (55%) | 329 (53%) |
| Race, no. (%) | |||
| Black | 314 (97%) | 266 (91%) | 580 (94%) |
| Latino | 4 (1%) | 14 (5%) | 18 (3%) |
| Multiracial/other | 7 (2%) | 13 (4%) | 20 (3%) |
| Age, months, mean (SD) | 50.7 (6.8) | 51.9 (6.3) | 51.3 (6.6) |
| BMI, kg/m2, mean (SD) | 16.5 (1.6) | 16.6 (2.2) | 16.6 (1.9) |
| BMI Z score, mean (SD) | 0.6 (1.0) | 0.7 (1.1) | 0.6 (1.0) |
| ≥85th BMI percentile, no. (%) | 107 (33%) | 100 (34%) | 207 (33%) |
Note: Significant difference between groups, from t-test or chi-square test. Boldface indicates statistical significance (p<0.05).
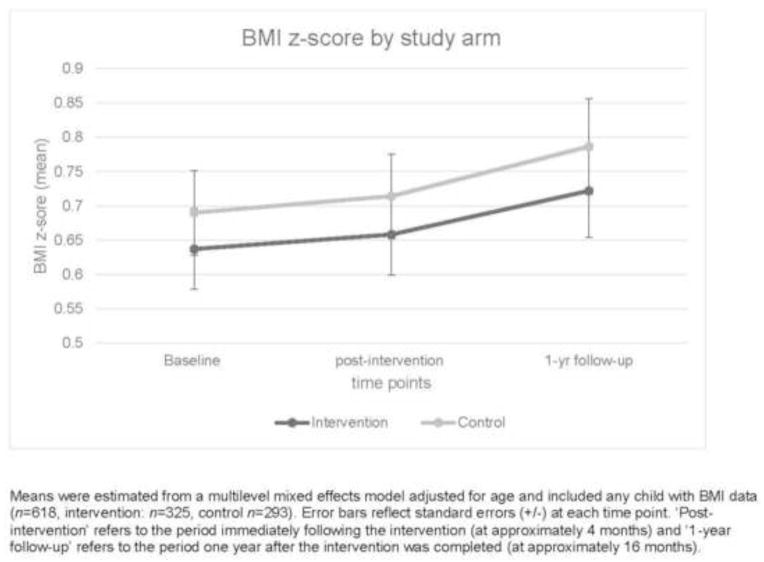
Table 2 presents the adjusted mean changes in BMI z-score from baseline to 1-year follow-up. BMI z-score change in the intervention arm was +0.08 (SE=0.04) and +0.10 (SE=0.04) among controls; however, the between-group difference was not significantly different (−0.01, SE=0.06, p=0.83)(Table 2). Figure 2 presents the adjusted mean BMI z-scores at all three time points. The estimated effect size (Cohen’s d) for BMI z-score was −0.03 (in favor of the intervention arm). As reported in Table 2, the intervention group did not significantly differ from controls in their TV viewing (hours/day) or total screen time change (hours/day) at 1-yr follow-up. Time spent on screen time or watching TV remained relatively unchanged in both groups at 1-year follow-up.
Table 2.
Child BMI, BMI-z Score, Screen Time, and Diet Quality at Baseline and 1-Year Follow-Up
| Intervention | Control | Group Difference in Δ (Int-Cont) mean (SE) |
p-valueb | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline mean (SE) |
1-Yr Follow-up mean (SE) |
Δa mean (SE) |
Baseline mean (SE) |
1-Yr Follow-up mean (SE) |
Δa mean (SE) |
|||
| BMI (kg/m2)c | 16.5 (0.12) | 16.8 (0.14) | 0.30 (0.08) | 16.7 (0.12) | 17.1 (0.14) | 0.43 (0.08) | −0.13 (0.11) | 0.26 |
| BMI z-scorec | 0.64 (0.06) | 0.72 (.07) | 0.08 (0.04) | 0.69 (0.06) | 0.79 (0.07) | 0.10 (0.04) | −0.01 (0.06) | 0.83 |
|
| ||||||||
| TV viewing (hrs/d)d | 2.7 (0.11) | 2.7 (0.13) | −0.03(0.10) | 2.6 (0.11) | 2.4 (0.13) | −0.21 (0.11) | 0.18 (0.15) | 0.23 |
| Total screen time (hrs/d)d | 5.2 (0.19) | 5.4(0.21) | 0.22 (0.16) | 4.8 (0.20) | 4.9 (0.21) | 0.08 (0.16) | 0.14 (0.22) | 0.52 |
|
| ||||||||
| Healthy Eating Indexe (HEI) | ||||||||
| HEI-Total | 56.0 (0.73) | 56.7 (0.99) | 0.63 (1.01) | 56.6 (0.79) | 53.6 (1.08) | −3.0 (1.11) | 3.6 (1.50) | 0.02 |
| HEI-Total fruit | 3.5 (0.10) | 3.3 (0.14) | −0.16 (0.16) | 3.4 (0.11) | 2.5 (0.16) | −0.92 (0.18) | 0.76 (0.24) | 0.003 |
| HEI-Whole fruit | 2.7 (0.14) | 2.6 (0.23) | −0.04 (0.23) | 3.1 (0.16) | 2.2 (0.25) | −0.91 (0.25) | 0.88 (0.34) | 0.02 |
| HEI-Saturated fat | 5.7 (0.26) | 5.8 (0.37) | 0.12 (0.34) | 5.5 (0.28) | 5.5 (0.40) | 0.02 (0.38) | 0.11 (0.51) | 0.84 |
| HEI-Whole Grains | 1.4 (0.11) | 1.6 (0.18) | 0.12 (0.18) | 1.0 (0.12) | 1.8 (0.19) | 0.78 (0.20) | −0.67 (0.27) | 0.02 |
| HEI-Total Vegetables | 2.0 (0.09) | 2.3 (0.14) | 0.28 (0.15) | 2.3 (0.10) | 2.2 (0.15) | −0.09 (0.16) | 0.37 (0.22) | 0.11 |
| HEI-SoFAAS | 12.1 (0.38) | 13.1 (0.47) | 0.93 (0.48) | 12.1 (0.41) | 11.4 (0.52) | −0.75 (0.53) | 1.7 (0.71) | 0.02 |
Multilevel models with a random intercept and random time trend at the student and classroom levels were used to test for differences between groups. All models were adjusted for baseline age.
Any child with relevant data (BMI, diet, or screen time) at baseline, post-intervention (4 months), or 1 year follow-up (16 months) was included in these models.
Note: Boldface indicates statistical significance (p<0.05).
Change from baseline to 1-year follow-up (1 year follow-up - baseline)
p-value indicates whether the between group difference from baseline to 1-yr follow-up was significant.
Height and weight data at baseline n=325 (Intervention), n=293 (Control); 4 months: n=309 (Intervention), n=280 (Control); 16 months: n=285 (Intervention), n=258 (Control)
Screen time data at baseline n=304 (Intervention), n=276 (Control); 4 months: n=298(Intervention), n=266 (Control); 16 months: n=262 (Intervention), n=242(Control)
Diet data at baseline n=278 (Intervention), n= 230 (Control); 4 months: n= 267 (Intervention), n=220 (Control); 16 months: n=196 (Intervention), n=160 (Control)
SoFAAS: Calories from Solid Fat, Alcohol, and Added Sugar; Maximum points for HEI-total =max points: 100, HEI-total fruit = max points: 5, HEI-Saturated fat = max points: 10; HEI-Whole Grains = max points: 5, HEI-Total Vegetables = max points: 5, HEI-SoFAAS max points: 20.
Figure 2.
BMI z-score by study arm.
Means were estimated from a multilevel mixed effects model adjusted for age and included any child with BMI data (n=618, intervention: n=325, control n=293). Error bars reflect standard errors (+/−) at each time point. ‘Post-intervention’ refers to the period immediately following the intervention (at approximately 4 months) and ‘1-year follow-up’ refers to the period one year after the intervention was completed (at approximately 16 months)
All diet outcomes are based on children’s dietary intake assessed for a full 24-hour period (e.g., 24-hour recall plus meal observations). Total HEI-score14 and HEI-component scores (Table 2) considered most relevant to the intervention were used to estimate change in diet quality from 1-year follow-up compared to baseline. Significant between-group differences were observed in total HEI score change (p=0.02) and in these HEI components: total fruit (p=0.003), whole fruit (p=0.02), whole grain (p=0.02), and SoFAAS (p=0.02). Total HEI score remained relatively stable (mean change, +0.63; SE=1.01) among intervention group children, whereas total HEI score decreased significantly among controls (mean change, −3.0; SE=1.1; p=0.02). Similarly, HEI scores in total fruit (mean change, −0.92; SE=0.18; p=0.001) and whole fruit (mean change, −0.91; SE=0.25; p=0.001) also decreased significantly among controls, whereas no change was observed in the intervention group. Unexpectedly, HEI score in whole grains did not change among intervention group children, but increased among controls (mean change, +0.78; SE=0.20; p<0.001). A marginally significant increase was observed in SoFAAS among the intervention arm (mean change, +0.93; SE=0.48; p=0.06) only. They also improved in their HEI score of dark green/orange vegetables/legumes (mean change, +0.34; SE=0.13; p=0.02); however, this change was not significant compared to controls.
This study also examined between-group differences at 1-year follow-up for other diet variables (i.e., fat, fruit, fruit juice, vegetables, fiber, trans fats) (Appendix Table 3). A significant between-group difference was observed in servings of fruits/day (juice excluded). Specifically, fruit intake remained relatively stable for the intervention group from baseline to 1-year follow-up, whereas the control group’s intake decreased over time. The between-group difference was 0.35 servings/day (SE=0.14, p=0.02).
Appendix Table 3.
Additional dietary variables at baseline and 1-year follow-up
| Intervention | Control | Group Difference in Δ (Int-Cont) mean (se) |
p valueb | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline mean (se) |
1-Yr Follow-up mean (se) |
Δa mean (SE) |
Baseline mean (se) |
1-Yr Follow-up mean (se) |
Δa mean (SE) |
|||
| Fat, % kcal | 33.0 (0.59) | 33.2 (0.86) | 0.22 (0.79) | 32.6 (0.63) | 33.3 (0.93) | 0.62 (0.86) | −0.41 (1.2) | 0.73 |
| Trans fatty acids, % kcal | 2.9 (0.07) | 2.9 (0.15) | −0.04 (0.16) | 2.9 (0.08) | 2.8 (0.08) | −0.25 (0.18) | 0.21 (0.24) | 0.39 |
| Fiber, g/1,000 kcal | 6.9 (0.17) | 7.4 (0.25) | 0.49 (0.26) | 7.3 (0.18) | 7.3 (0.27) | −0.02 (0.28) | 0.51 (0.38) | 0.19 |
| Fruitc servings/day | 0.93 (0.06) | 0.96 (0.08) | 0.03 (0.09) | 1.0 (0.06) | 0.72 (0.09) | −0.32 (0.10) | 0.35 (0.14) | 0.02 |
| 100% fruit juice, servings/day | 1.5 (0.10) | 1.3 (0.14) | −0.12 (0.14) | 1.2 (0.11) | 0.90 (0.15) | −0.26 (0.16) | 0.14 (0.21) | 0.52 |
| Vegetablesd servings/day | 1.2 (0.07) | 1.3 (0.12) | 0.12 (0.13) | 1.2 (0.07) | 1.2 (0.13) | 0.06 (0.14) | 0.06 (0.19) | 0.76 |
Multilevel models with a random intercept and random time trend at the student and classroom levels were used to test for differences between groups. All models were adjusted for baseline age.
Change from baseline to 1-yr follow-up (1 yr follow-up - baseline). Follow-up is one year from the post-intervention period; note: boldface indicates statistical significance (p<0.05).
p value indicates whether the between group difference from baseline to 1-yr follow-up was significant.
excludes juices, avocado, fried fruits, and fruit-based savory snacks,
excludes fried potatoes, other fried vegetables, and vegetable juice
Diet data at baseline n=278 (Intervention), n= 230 (Control); 4 months: n= 267 (Intervention), n=220 (Control); 16 months: n=196 (Intervention), n=160 (Control)
The number of lessons completed by teachers and homework assignments completed by parents have been previously reported.5 Briefly, there were a total of 28 nutrition lessons and 28 exercise sessions, administered twice/week for 14 weeks. Teachers reported completing a mean of 26.6 (SD=1.9) nutrition lessons and 27.1 (SD=1.7) exercise lessons. Parents completed a mean of 5.0 (SD=4.5) of 13 homework assignments.
Discussion
The Hip-Hop to Health Obesity Prevention Effectiveness Trial was designed to test a teacher-delivered version of the original efficacy trial.6 The original efficacy trial was successful in halting excessive weight gain (i.e., BMI z-score) among preschool children in intervention schools versus controls.6 In this current effectiveness trial, higher levels of moderate to vigorous physical activity (as measured by accelerometers) and less screen time were initially found (i.e., post-intervention) among intervention children compared with controls. No initial BMI or diet differences were observed.5 At 1-year follow-up, resource constraints prevented the collection of physical activity measurements; however, changes in BMI z-score, diet, and screen time were assessed. One-year follow-up results did not demonstrate between-group differences in BMI z-score or screen time; however, significant between-group differences were observed in diet.
Although the findings of this effectiveness trial were less robust than in the original efficacy trial,6 diet changes favoring the intervention group compared with controls were observed. Specifically, fruit intake remained stable for the intervention group from baseline to 1-year follow-up, whereas fruit intake decreased over time among controls, resulting in a between-group difference of a third of a serving/day. Similarly, overall diet quality worsened among controls but remained unchanged in the intervention group. This trend was emerging at post-intervention (data not shown); however, significant between-group differences were not observed until 1-year follow-up. The worsening of HEI-2005 scores in the control group suggests that early intervention may help prevent diet quality from eroding over time. There is some evidence, based on data from the 1999–2004 National Nutrition and Health Examination Survey (NHANES), to suggest that overall diet quality, as measured by the HEI-2005 and the Revised Children’s Dietary Index, worsens with increasing age.20–22 The cross-sectional comparison of NHANES data conducted by O’Neil et al.22 reported higher scores among preschoolers compared with school age children and adolescents, respectively (age 2–5 years, 53.0; age 6–12 years, 49.3; age 13–18 years, 47.7). The regression analysis presented by Kranz and colleagues23 found a 2.38-lower diet quality score by 1-year increase in age. Similarly, this present study observed a decrease in diet quality score (change, 3.01) over 16 months among controls, whereas no significant change was found among intervention children. Cole et al.,20 representing a large sample of low-income children, also found similar trends. Although this present study assessed diet quality with the HEI-2005 consistent with the 2005 DGA,16 these findings should also apply to updated guidelines (e.g., 2010 DGA)24 because the simple messages and concepts presented in the intervention to the target population (i.e., preschoolers) promote adherence to an overall healthful dietary pattern (e.g., diet high in fruits, vegetables, whole grains, low-fat dairy, and less added sugars), which is foundational to the DGA.16,24
The lack of a significant finding related to BMI z-score in this effectiveness trial may be due to intervention dose. In contrast to the efficacy trial, the amount of time devoted to the intervention curriculum decreased from three times/week to twice weekly to alleviate some of the burden on teachers because they were fully responsible for delivering the curriculum in this version of the intervention. Additionally, it was apparent from the classroom observations that the activity portion of the intervention was not delivered with the same level of intensity by the classroom teachers as it was by the research team in the efficacy trial. Specifically, the 20-minute aerobic portion of the curriculum was a challenge for teachers given that many of the teachers were not physically active themselves. This is a concern and speaks to the need for creating cultures in schools, neighborhoods, and communities where being active is normative. In Chicago Public Schools, there is no specific training provided for preschool teachers to enhance their own fitness or that of the children. Formal physical education instruction could have enhanced the results, but this is not currently part of preschool programming. Based on teacher feedback, many teachers were more comfortable with the nutrition portion of the curriculum and expressed interest in using the materials again. Therefore, it is plausible that the nutrition sessions continued beyond the intervention period and may have contributed to between-group differences in diet quality at 1-year follow-up. It should be noted, however, that the authors did not formally evaluate how many Head Start teachers continued to incorporate, some or all, of the curriculum in their daily lesson plans. Doing so would have allowed for better assessment of the sustainability of the curriculum in that setting. The authors have however, disseminated this curriculum more broadly. Through funding from the U.S. Department of Agriculture,, these materials have been adapted for audiences served by the Expanded Food and Nutrition Education Program and the Supplemental Nutritional Assistance Program Education (M Fitzgibbon, personal communication, 2015). Evaluation efforts for these projects are forthcoming.
At post-intervention, screen time was lower in the intervention group compared with controls, but this effect was not sustained at 1-year follow-up. The intervention group’s use of screen time returned to their baseline levels at 1-year follow-up. No improvements in screen time or TV viewing were observed in the original efficacy trial during the 1- or 2-year follow-up period either.6 Of note, the measure used to capture screen time has not, to the authors’ knowledge, been validated for use among preschoolers. Therefore, the ability to capture screen time use might have been impaired. Despite the limitations of this tool, these findings are not necessarily surprising. For instance, only one lesson out of 14 focused on watching less TV. Periodic booster sessions could have reinforced this message and addressing other screen time activities would be warranted for today’s audience. Additionally, a number of systematic reviews examining screen time interventions in children highlight the importance of parental involvement.25–27 Parents play an important role in establishing routines that provide a model for healthy eating, screen time habits, and activity levels, particularly for young children.28 Finding innovative and feasible ways to involve parents should be considered in future early childhood school-based interventions.
Limitations
There are strengths and limitations to consider when interpreting the present findings. The retention rate at 1-year follow-up was strong, at 89%. The dietary data collected for this study can be regarded as both a strength and limitation. Dietary data was based on a full day’s intake captured with a 24-hour recall plus meal observation, which is a strength. However, 1-year follow-up diet data could only be collected on 356 children, compared with 508 at baseline. Most children with missing diet data at 1-year follow-up were older than children with diet data. This mainly occurred because older children left for kindergarten. Because this reason is unrelated to the outcome (i.e., diet), the missing diet data meet the assumption of “missing at random” and can be addressed by including age to the mixed effects model as demonstrated in the analysis.19 This intervention was delivered in an urban environment and participants were low-income, mainly African American children, so the authors cannot speculate how this intervention would be received in other settings with other racial/ethnic groups. Furthermore, the intervention did not include any environmental or policy strategies that have been recommended to support positive changes in weight control behaviors.29 Effectively intervening on the physical, economic, and legislative environments could have a significant impact on childhood obesity. However, they require ongoing partnerships with the organizations and agencies that oversee food pricing and availability, urban planning, and the food industry.30,31
Conclusions
These results suggest that a classroom teacher–delivered obesity prevention intervention for preschool children is feasible, acceptable, and can prevent erosion of dietary quality over time. Translating the efficacy trial into an effectiveness trial took continued attention to engaging stakeholders (e.g., teachers, teacher’s aides, principals) throughout the planning, implementation, and adaptation process to help enhance the fit between the intervention and school culture. In retrospect, more attention could have been paid to the evolving changes in individual schools (e.g., staff turnover) as well as the larger school system (e.g., teacher’s strike) that could have impacted sustainability. The final stage of innovation requires integration of the new practice so that it is part of ongoing practice;32 therefore, the team could have offered teachers and administrators greater guidance on how these materials might be integrated into their curriculum moving forward. If obesity is to be effectively addressed, particularly among underserved youth who are disproportionately affected, early childhood prevention interventions cannot exist in isolation. Reinforcement from ongoing efforts is required. For instance, if this type of intervention was embedded within the educational system as part of standard curriculum and was delivered in a developmentally appropriate format from preschool onward, there is great potential for health-related behaviors and positive weight gain trajectories to be observed more broadly. Furthermore, lifestyle changes among high-risk youth that are made in individually delivered interventions, such as Hip-Hop to Health Jr., are often undermined by immersion in an obesogenic environment that does not currently provide sufficient economic incentives to purchase healthy foods or activity space for consistent and safe physical activity. Therefore, greater consideration for creating societal and environmental supports for sustaining healthful lifestyle changes is also required.
Acknowledgments
This study was funded in part by the National Heart, Lung, and Blood Institute (R01HL081645) and National Cancer Institute (R25CA057699). We would also like to thank the Chicago Public Schools Early Childhood Education Program, the families and teachers who participated in the project, the principals who supported the project, and all research staff for time and dedication to this project. Finally, we would like to thank Stephen Onufrak from CDC for developing the SAS program used for calculating the Healthy Eating Index.
Footnotes
Trial Registration: www.clinicaltrials.gov Identifier NCT00241878.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the united states, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. http://dx.doi.org/10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. DHHS, Office of Disease Prevention and Health Promotion. [Accessed January 26, 2015];Healthy People 2020. www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status/objectives.
- 3.Fitzgibbon ML, Stolley MR, Dyer AR, VanHorn L, KauferChristoffel K. A Community-Based Obesity Prevention Program for Minority Children: Rationale and Study Design for Hip-Hop to Health Jr. Prev Med. 2002;34(2):289–297. doi: 10.1006/pmed.2001.0977. http://dx.doi.org/10.1006/pmed.2001.0977. [DOI] [PubMed] [Google Scholar]
- 4.Stolley MR, Fitzgibbon ML, Dyer A, Horn LV, KauferChristoffel K, Schiffer L. Hip-Hop to Health Jr., an obesity prevention program for minority preschool children: baseline characteristics of participants. Prev Med. 2003;36(3):320–329. doi: 10.1016/s0091-7435(02)00068-3. http://dx.doi.org/10.1016/S0091-7435(02)00068-3. [DOI] [PubMed] [Google Scholar]
- 5.Fitzgibbon ML, Stolley MR, Schiffer LA, et al. Hip-Hop to Health Jr. Obesity Prevention Effectiveness Trial: Postintervention Results. Obesity. 2011;19(5):994–1003. doi: 10.1038/oby.2010.314. http://dx.doi.org/10.1038/oby.2010.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Two-year follow-up results for Hip-Hop to Health Jr.: A randomized controlled trial for overweight prevention in preschool minority children. J Pediatr. 2005;146(5):618–625. doi: 10.1016/j.jpeds.2004.12.019. http://dx.doi.org/10.1016/j.jpeds.2004.12.019. [DOI] [PubMed] [Google Scholar]
- 7.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 8.CDC. [Accessed April 14, 2014];A SAS Program for the 2000 CDC Growth Charts (ages 0 to <20 years) www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm.
- 9.Klesges RC, Klesges LM, Brown G, Frank GC. Validation of the 24-hour dietary recall in preschool children. J Am Diet Assoc. 1987;87(10):1383–1385. [PubMed] [Google Scholar]
- 10.Baranowski T, Sprague D, Baranowski JH, Harrison JA. Accuracy of maternal dietary recall for preschool children. J Am Diet Assoc. 1991;91(6):669–674. [PubMed] [Google Scholar]
- 11.Johnson RK, Driscoll P, Goran MI. Comparison of Multiple-Pass 24-Hour Recall Estimates of Energy Intake With Total Energy Expenditure Determined By the Doubly Labeled Water Method in Young Children. J Am Diet Assoc. 1996;96(11):1140–1144. doi: 10.1016/S0002-8223(96)00293-3. http://dx.doi.org/10.1016/S0002-8223(96)00293-3. [DOI] [PubMed] [Google Scholar]
- 12.Bollella MC, Boccia LA, Nicklas TA, et al. Assessing dietary intake in preschool children: The healthy start project - New York. Nutr Res. 1999;19(1):37–48. http://dx.doi.org/10.1016/S0271-5317(98)00174-2. [Google Scholar]
- 13.Simons-Morton BG, Baranowski T. Observation in assessment of children’s dietary practices. J Sch Health. 1991;61(5):204–207. doi: 10.1111/j.1746-1561.1991.tb06012.x. http://dx.doi.org/10.1111/j.1746-1561.1991.tb06012.x. [DOI] [PubMed] [Google Scholar]
- 14.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1896–1901. doi: 10.1016/j.jada.2008.08.016. http://dx.doi.org/10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 15.Guenther PM, Reedy J, Krebs-Smith SM, Reeve BB. Evaluation of the Healthy Eating Index-2005. J Am Diet Assoc. 2008;108(11):1854–1864. doi: 10.1016/j.jada.2008.08.011. http://dx.doi.org/10.1016/j.jada.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 16.U.S. DHHS, U.S. Department of Agriculture. [Accessed April 25, 2015];Dietary Guidelines for Americans. 2005 www.health.gov/dietaryguidelines/dga2005/document/
- 17.Borzekowski DLG, Robinson TN. The Remote, the Mouse, and the No. 2 Pencil: The Household Media Environment and Academic Achievement Among Third Grade Students. Arch Pediatr Adolesc Med. 2005;159(7):607–613. doi: 10.1001/archpedi.159.7.607. http://dx.doi.org/10.1001/archpedi.159.7.607. [DOI] [PubMed] [Google Scholar]
- 18.Robinson TN, Killen JD. Ethnic and Gender Differences in the Relationships between Television Viewing and Obesity, Physical Activity, and Dietary Fat Intake. J Health Educ. 1995;26(sup2):S91–S98. [Google Scholar]
- 19.Hedeker DR, Gibbons RD. Longitudinal data analysis. Hoboken, N.J: Wiley-Interscience; 2006. [Google Scholar]
- 20.Cole N, Fox MK. [Accessed April 28, 2015];Diet quality of American young children by WIC participation status: Data from the National Health and Nutrition Examination Survey, 1999–2004. www.fns.usda.gov/sites/default/files/NHANES-WIC.pdf.
- 21.Kranz S, Hartman T, Siega-Riz AM, Herring AH. A Diet Quality Index for American Preschoolers Based on Current Dietary Intake Recommendations and an Indicator of Energy Balance. J Am Diet Assoc. 2006;106(10):1594–1604. doi: 10.1016/j.jada.2006.07.005. http://dx.doi.org/10.1016/j.jada.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 22.O’Neil CE, Nicklas TA, Zanovec M, Cho SS, Kleinman R. Consumption of whole grains is associated with improved diet quality and nutrient intake in children and adolescents: the National Health and Nutrition Examination Survey 1999–2004. Public Health Nutr. 2010;14(2):347–355. doi: 10.1017/S1368980010002466. http://dx.doi.org/10.1017/S1368980010002466. [DOI] [PubMed] [Google Scholar]
- 23.Kranz S, Findeis JL, Shrestha SS. Use of the Revised Children’s Diet Quality Index to assess preschooler’s diet quality, its sociodemographic predictors, and its association with body weight status. J Pediatr (Rio J) 2008;84(1):26–34. doi: 10.2223/JPED.1745. http://dx.doi.org/10.2223/JPED.1745. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Agriculture, U.S. DHHS. [Accessed April 25, 2015];Dietary Guidelines for Americans. 2010 www.health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf.
- 25.Wahi G, Parkin PC, Beyene J, Uleryk EM, Birken CS. Effectiveness of interventions aimed at reducing screen time in children: A systematic review and meta-analysis of randomized controlled trials. Arch Pediatr Adolesc Med. 2011;165(11):979–986. doi: 10.1001/archpediatrics.2011.122. http://dx.doi.org/10.1001/archpediatrics.2011.122. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt ME, Haines J, O’Brien A, et al. Systematic Review of Effective Strategies for Reducing Screen Time Among Young Children. Obesity. 2012;20(7):1338–1354. doi: 10.1038/oby.2011.348. http://dx.doi.org/10.1038/oby.2011.348. [DOI] [PubMed] [Google Scholar]
- 27.Marsh S, Foley LS, Wilks DC, Maddison R. Family-based interventions for reducing sedentary time in youth: a systematic review of randomized controlled trials. Obes Rev. 2014;15(2):117–133. doi: 10.1111/obr.12105. http://dx.doi.org/10.1111/obr.12105. [DOI] [PubMed] [Google Scholar]
- 28.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert committee recommendations. Pediatrics. 1998;102(3):E29. doi: 10.1542/peds.102.3.e29. http://dx.doi.org/10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 29.Khan LK, Sobush K, Keener D, et al. Recommended community strategies and measurements to prevent obesity in the United States. MMWR Recomm Rep. 2009;58(RR-7):1–26. [PubMed] [Google Scholar]
- 30.Huang TT, Drewnosksi A, Kumanyika S, Glass TA. A systems-oriented multilevel framework for addressing obesity in the 21st century. Prev Chronic Dis. 2009;6(3):A82. [PMC free article] [PubMed] [Google Scholar]
- 31.Summerbell CD, Moore HJ, Vögele C, et al. Evidence-based recommendations for the development of obesity prevention programs targeted at preschool children. Obes Rev. 2012;13:129–132. doi: 10.1111/j.1467-789X.2011.00940.x. http://dx.doi.org/10.1111/j.1467-789X.2011.00940.x. [DOI] [PubMed] [Google Scholar]
- 32.Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117–17. doi: 10.1186/1748-5908-8-117. http://dx.doi.org/10.1186/1748-5908-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]