Abstract
Introduction
It is predicted that gaining health insurance via the Affordable Care Act will result in increased rates of preventive health services receipt in the U.S, primarily based on self-reported findings from previous health insurance expansion studies. This study examined the long-term (36-month) impact of Oregon’s 2008 randomized Medicaid expansion (“Oregon Experiment”) on receipt of 12 preventive care services in community health centers using electronic health record data.
Methods
Demographic data from adult (aged 19–64 years) Oregon Experiment participants were probabilistically matched to electronic health record data from 49 Oregon community health centers within the OCHIN community health information network (N=10,643). Intent-to-treat analyses compared receipt of preventive services over a 36-month (2008–2011) period among those randomly assigned to apply for Medicaid versus not assigned, and instrumental variable analyses estimated the effect of actually gaining Medicaid coverage on preventive services receipt (data collected in 2012–2014; analysis performed in 2014–2015).
Results
Intent-to-treat analyses revealed statistically significant differences between patients randomly assigned to apply for Medicaid (versus not assigned) for eight of 12 assessed preventive services. In intent-to-treat[MM1] analyses, Medicaid coverage significantly increased the odds of receipt of most preventive services (ORs ranging from 1.04 [95% CI=1.02, 1.06] for smoking assessment to 1.27 [95% CI=1.02, 1.57] for mammography).
Conclusions
Rates of preventive services receipt will likely increase as community health center patients gain insurance through Affordable Care Act expansions. Continued effort is needed to increase health insurance coverage in an effort to decrease health disparities in vulnerable populations.
Introduction
In the U.S., lack of health insurance is associated with decreased access to health care, including lower receipt of recommended preventive services among uninsured patients compared with insured patients.1–8 The 2010 Affordable Care Act (ACA) created new opportunities for millions of uninsured people to obtain health insurance.9,10 It is predicted that ACA coverage opportunities will positively affect rates of receipt of preventive services as uninsured patients become insured.11–13 These predictions are largely based on data that could be influenced by unmeasured external factors. For instance, increased rates of preventive services receipt among people who gain insurance coverage as a result of a significant life event (e.g., getting a new job) could confound how change in insurance status affects preventive care receipt. To estimate the causal effect of gaining health insurance on receipt of preventive services, researchers examined “natural experiments” in which individuals gained coverage owing to a policy change such as Massachusetts’ 2006 health insurance expansion. Most of these studies were observational or quasi-experimental and relied on self-reported data, which could explain why their findings were inconsistent.14–18
Randomizing patients to receive an intervention provides the strongest design to assess causal relationships; however, it is nearly impossible to conduct a study that randomizes insurance coverage. The “Oregon Experiment,” a randomized natural experiment, provided a unique opportunity to isolate the effect of health insurance on preventive services receipt.19–22 In 2008, Oregon expanded Medicaid coverage to a limited number of “non-categorically eligible” individuals (i.e., those not federally mandated to receive Medicaid). It was anticipated that the number of people that signed up for coverage would exceed the expansion budget; thus, to most fairly allocate limited resources, interested adults were added to a list and were randomly selected to apply for Medicaid coverage. From a “reservation list” of >100,000 entries, approximately 30,000 people were randomly selected to apply, and approximately 10,000 gained coverage.23 Detailed information about Oregon’s Medicaid program in 200823,24 and the Oregon Experiment is available elsewhere.19,21,23,25 This study utilized this randomized natural experiment to assess the impact of gaining Medicaid coverage on receipt of preventive services among community health center (CHC) patients. The authors hypothesized that those who were selected to apply and gained Medicaid would receive more preventive services than those who did not gain Medicaid coverage.
An ideal setting for isolating the effect of insurance, CHCs provide care for millions of patients, regardless of insurance coverage status or ability to pay.26 CHCs also care for a high percentage of racial/ethnic minority patients and others likely to have low rates of preventive services and to experience healthcare disparities.27 Thus, CHC patients would likely be among those most affected by a policy change to expand Medicaid coverage.
To limit bias inherent in self-reported measures, this study utilized electronic health record (EHR) data from 49 CHCs. It assessed participants’ receipt of preventive services, as documented in the EHR, in the 36 months after the Oregon Experiment. This is the first study to focus on the impact of the Oregon Experiment on receipt of preventive care services in CHCs utilizing EHR data.
Methods
Data Sources
This study used EHR data from the OCHIN community health information network, a 501(c)(3) network of health systems that supports >300 CHC clinic sites by providing a centrally hosted EpicCare EHR with an enterprise-wide master patient index (each patient has a single medical record available across the network). Originally called the Oregon Community Health Information Network, its official name became “OCHIN, Inc.” as membership expanded beyond Oregon. Detailed information about OCHIN and the suitability of OCHIN’s EHR database for research purposes is available elsewhere.28–30 The authors identified all Oregon CHC sites in the OCHIN network that were live on EHR as of March 11, 2008 (N=49), which was the earliest date a patient could have received Medicaid via the Oregon Experiment. State administrative data, including the Oregon Experiment reservation list (names, addresses, and other contact details provided to sign up for the chance to gain Medicaid) and Oregon’s Medicaid enrollment data were also used to assess periods of Medicaid coverage during the study period.
Study Population
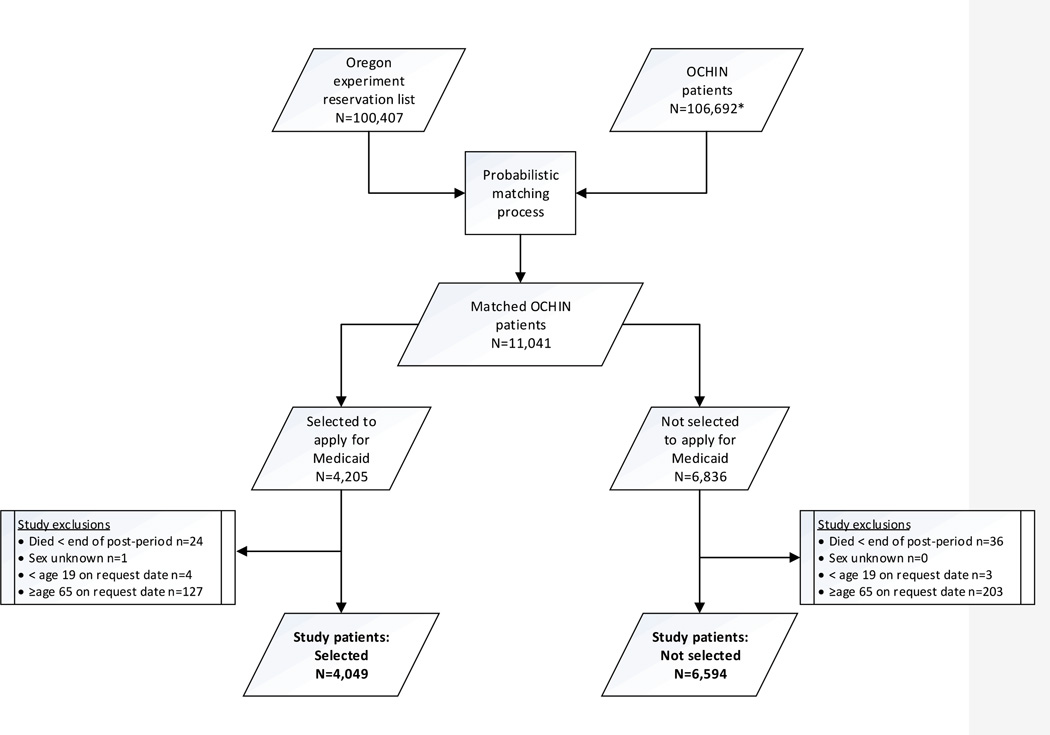
Individuals on the Oregon Experiment “reservation list” (N=100,407) were probabilistically matched to individual OCHIN patients (N=106,692), using Link Plus software31 and demographic variables common to both data sets. Two researchers independently performed a case-by-case review of uncertain matches using additional demographic variables. Appendix Table 1 provides more details. The authors identified 11,041 matched individuals, 4,205 of whom were selected to apply for coverage, and 6,836 who were not selected. To preserve randomization, minimal exclusions were applied: patients aged <19 years (n=8) and >64 years (n=337), patients not alive at the end of the post-period (n=60), and those with unknown sex (n=1). This led to an exclusion of 156 (3.7%) from the selected group and 242 (3.5%) from the non-selected group. The final study population consisted of 10,643 patients: 4,049 selected to apply for coverage and 6,594 not selected.
Measures
Random selection to apply for Medicaid coverage occurred through eight monthly drawings held between March and October 2008. Among selected individuals, coverage start dates were retroactively assigned as the date of selection notification (the “selection date”). For analyses, a 2008 selection date was randomly assigned to individuals not selected to apply based on the distribution of observed selection dates among people selected to apply. Outcomes were assessed in the 36 months after the selection date (post-period).
To examine the effect of providing access to apply for health insurance on the receipt of preventive services, intent-to-treat (ITT) analyses were conducted comparing patients randomly selected to apply for Medicaid coverage (i.e., intervention group) versus those not selected to apply (i.e., control group). However, the ITT approach does not provide a causal estimate of obtaining Medicaid insurance. For example, individuals randomly selected to apply for insurance did not always follow through, and thus remained uninsured. To estimate the effect of gaining Medicaid on receipt of preventive services, bivariate probit instrumental variable (IV) analyses were conducted. To be considered a valid instrument for IV analyses, the variable(s) must be associated with Medicaid coverage, but not associated with the receipt of preventive services in the relevant time period except through the instrument’s effect on Medicaid coverage. Based on these criteria, two instrumental variables that met the standards for valid instruments were used: (1) selection status in the Oregon Experiment (randomly selected to apply, or not)20,32; and (2) Medicaid coverage status in the pre-period (any coverage or no coverage). Both variables were positively and significantly associated with post-period coverage, but neither would be expected to be directly associated with post-period preventive service receipt except through their association with post-period coverage. The treatment variable was having at least 6 months of continuous Medicaid coverage in the post-period starting from their selection date, as participants who received Medicaid were covered for 6 months before they had to reapply to renew coverage. The ITT and IV analyses are presented together in this study to identify the effects of gaining access to apply for health insurance (ITT) and actually gaining Medicaid (IV), which are two different experiences.
The primary outcomes were whether or not the patient received preventive care services in the post-period: screenings for cervical, breast, and colorectal cancer (fecal occult blood testing and colonoscopy); screenings for diabetes (glucose and hemoglobin A1c [HbA1c]), hypertension, obesity, smoking; lipid screening; chlamydia testing; and receipt of influenza vaccination. Codes were used based on EHR Meaningful Use Stage 1 measures.33 These included ICD-9-CM diagnosis and procedure codes, Current Procedural Terminology and Healthcare Common Procedure Coding System codes, Logical Observation Identifiers Names and Codes, and medication codes. The authors also used relevant code groupings and codes specific to the OCHIN EHR, used for Meaningful Use reporting and internal quality improvement initiatives.34 Appendix Table 2 provides detailed technical specifications and patient eligibility criteria for each measure.
For covariates, this study used EHR data to obtain patient age, sex, race/ethnicity, household income, and baseline health status prior to each patient’s selection date. Patients’ household income was estimated as the average of available Federal Poverty Level from all visits. To measure baseline health status, prior diagnosis of five chronic conditions was assessed using standard Meaningful Use criteria33 or Healthcare Effectiveness Data and Information Set35 codes: asthma, coronary artery disease, diabetes, dyslipidemia, and hypertension. If a qualifying diagnosis code appeared on the problem list or in two or more encounters prior to the selection date, the patient was considered to have the condition.
Statistical Analysis
Differences were assessed in the covariates between patients randomly selected to apply for Medicaid versus those not selected to apply, using chi-square tests for categorical characteristics and two-sample t-tests for continuous predictors. This was done for every preventive service outcome separately, and covariates that displayed significant differences between the selection groups were included in adjusted analyses. Next, ITT analyses were conducted for each outcome, comparing preventive service receipt in the 36 month post-period among those randomly selected to apply versus not selected using generalized estimating equation models with a logit link and robust sandwich variance estimator to account for the clustering of patients within CHCs.
A maximum-likelihood bivariate probit IV model36 was used, as it has been shown to be more consistent and less biased for models with binary outcomes and binary endogenous variables compared with the common two-stage least-squares model.37 The bivariate probit model controlled for the same covariates included in the ITT models. A robust variance estimator that account for within-clinic correlation was implemented.38,39 The validity of the instruments was tested using an over-identification test. All statistical tests were two-sided and significance was defined as a p-value <0.05. Statistical analyses were performed using SAS, version 9.3 and Stata, version 12.1 (data collected in 2012–2014; analysis performed in 2014–2015). This study was approved by the IRB at Oregon Health and Science University and was registered as an observational study at clinicaltrials.gov (NCT02355132).
Results
A total of 10,643 participants with an average age of 39.2 years at baseline were followed for 36 months after random selection to apply for coverage (Table 1). About 59% of participants had no chronic conditions documented in the EHR in the pre-period, and 60% were non-Hispanic white. There were no significant differences at baseline between the selected and not selected groups in gender, age, Federal Poverty Level, or race/ethnicity. The groups differed on the number of chronic conditions prior to selection date.
Table 1.
Demographic Characteristics by Selected Versus not Selected to Apply for Medicaid Coverage via Oregon Experiment
| Selected N=4,049 |
Not Selected N=6,594 |
p-valuea | |
|---|---|---|---|
| Total N=10,643 | no. (column %) | no. (column %) | |
| Gender | 0.734 | ||
| Female | 2,231 (55.1) | 3,611 (54.8) | |
| Male | 1,818 (44.9) | 2,983 (45.2) | |
| Age | |||
| Mean (SD)b | 39.2 (11.7) | 39.5 (11.9) | 0.185 |
| Race/Ethnicity | 0.063 | ||
| Hispanic, any race | 548 (13.5) | 867 (13.2) | |
| Non-Hispanic, white | 2,447 (60.4) | 3,949 (59.9) | |
| Non-Hispanic, other | 795 (19.6) | 1,412 (21.4) | |
| Unknown | 259 (6.4) | 366 (5.6) | |
| Average FPLc | 0.827 | ||
| <100% | 2,911 (71.9) | 4,772 (72.4) | |
| ≥100% | 1,101 (27.2) | 1,766 (26.8) | |
| Missing/Unknown | 37 (0.9) | 56 (0.8) | |
| Number of chronic conditions diagnosed prior to selection dated | <0.001 | ||
| 0 | 2,394 (59.1) | 3,936 (59.7) | |
| 1 | 567 (14.0) | 1,083 (16.4) | |
| 2 | 261 (6.5) | 442 (6.7) | |
| 3–5 | 135 (3.3) | 272 (4.1) | |
| No data to assess | 692 (17.1) | 861 (13.1) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Table 2 presents the percentage of participants who received preventive services during the 36-month post-period by selection group and the ORs of receipt of preventive services, comparing those participants selected to apply versus those not selected. Patients selected to apply had significantly higher odds of receiving assessments of BMI (AOR[MM2]=1.12, 95% CI=1.10, 1.14), blood pressure (AOR=1.09, 95% CI=1.07, 1.12), and smoking status (AOR=1.04, 95% CI=1.02, 1.06). Statistically significant increases in the odds of receipt of preventive services were also observed when comparing selected with not selected groups for the following outcomes: 15% increase for Pap test, 27% increase for mammography, 15% increase for fecal occult blood testing, and 24% increase for chlamydia testing. Additionally, participants who were selected to apply had lower odds of receiving HbA1c testing (AOR=0.79, 95% CI=0.71, 0.88), compared with participants not selected.
Table 2.
Preventive Services Receipt by Selection Status to Apply for Medicaid Coverage via the Oregon Experiment
| UNADJUSTED | ADJUSTED | ||||||
|---|---|---|---|---|---|---|---|
|
Screening |
N | % Receipt |
Difference in % |
OR | (OR 95% CI) | OR | (OR 95% CI) |
| BMIb | |||||||
| Selected | 4,049 | 54.3 | +3.6 | 1.14 | (1.12–1.17) | 1.12 | (1.10–1.14) |
| Not selected | 6,594 | 50.7 | Ref | ||||
| Blood pressureb | |||||||
| Selected | 4,049 | 65.6 | +3.0 | 1.10 | (1.07–1.13) | 1.09 | (1.07–1.12) |
| Not selected | 6,594 | 62.6 | Ref | ||||
| Smokingb | |||||||
| Selected | 4,049 | 59.2 | +2.3 | 1.07 | (1.04–1.10) | 1.04 | (1.02–1.06) |
| Not selected | 6,594 | 56.9 | Ref | ||||
| Pap testa,b | |||||||
| Selected | 1,872 | 39.3 | +3.4 | 1.16 | (1.02–1.32) | 1.15 | (1.01–1.30) |
| Not selected | 3,059 | 35.9 | Ref | ||||
| Mammographyc | |||||||
| Selected | 979 | 45.7 | +6.0 | 1.27 | (1.02–1.57) | 1.27 | (1.02–1.57) |
| Not selected | 1,682 | 39.7 | Ref | ||||
| FOBTb | |||||||
| Selected | 951 | 20.0 | +1.5 | 1.17 | (0.98–1.40) | 1.15 | (1.01–1.32) |
| Not selected | 1,580 | 18.5 | Ref | ||||
| Colonoscopyb | |||||||
| Selected | 951 | 10.8 | +1.2 | 1.10 | (0.95–1.27) | 1.04 | (0.90–1.20) |
| Not selected | 1,580 | 9.6 | Ref | ||||
| Chlamydia testb | |||||||
| Selected | 133 | 38.4 | +5.8 | 1.28 | (1.11–1.49) | 1.24 | (1.07–1.44) |
| Not selected | 233 | 32.6 | Ref | ||||
| Lipid screeningb | |||||||
| Selected | 3,958 | 36.1 | +2.0 | 1.10 | (0.92–1.32) | 1.10 | (0.93–1.31) |
| Not selected | 6,449 | 34.1 | Ref | ||||
| Influenza vaccinationb | |||||||
| Selected | 948 | 37.7 | +0.0 | 1.00 | (0.83–1.20) | 1.02 | (0.85–1.21) |
| Not selected | 1,557 | 37.7 | Ref | ||||
| Glucoseb | |||||||
| Selected | 1,506 | 58.6 | +2.4 | 1.08 | (1.00–1.17) | 1.05 | (0.94–1.17) |
| Not selected | 2,576 | 56.2 | Ref | ||||
| HbA1cc | |||||||
| Selected | 248 | 69.0 | −4.8 | 0.79 | (0.71–0.88) | 0.79 | (0.71–0.88) |
| Not selected | 480 | 73.8 | Ref | ||||
Note: Boldface indicates statistical significance (p<0.05). Statistics were estimated from intent-to-treat generalized estimating equation logistic models. Each model controlled for imbalances between selection groups (Appendix Tables 3A–3I show tables comparing patient demographics by selection group for each outcome):
Model adjusted for age
Model adjusted for number of chronic conditions diagnosed prior to selection date
No covariate adjustment made. No differences in covariate distribution between groups.
Definition of Outcome Denominators:
BMI: all adults in the study
Blood pressure: all adults in the study
Smoking status: All adults in the study
Pap test: Females age 21–64, no history of hysterectomy
Mammography: Females age ≥40, no history of bilateral mastectomy
Colorectal cancer screen: age ≥50, no history of colorectal cancer or total colectomy
Chlamydia test: Sexually active females age 19–24
Lipid screening: age ≥20
Influenza vaccination: age ≥50, without indication of vaccine allergy/contraindication or declined
Glucose: age ≥45
HbA1c: diagnosis of diabetes (diagnosis requires ICD9 code to appear on problem list OR in 2+ separate encounters prior to request date)
Among the 4,049 patients that were selected to apply, 44% actually gained Medicaid coverage (≥6 months of continuous coverage) in the post-period. Table 3 displays the effects of gaining Medicaid coverage on receipt of preventive services estimated by the IV approach. The bivariate probit model estimates indicated that participants who had Medicaid coverage in the post-period had significantly higher likelihood of receiving BMI (increase of 12.5%, 95% CI=10.6, 14.4), blood pressure (increase of 10.1%, 95% CI=7.0, 13.3), and smoking (increase of 6.2%, 95% CI=5.3, 7.1) screenings, compared with those who did not have Medicaid coverage. Among cancer-related screenings, statistically significant Medicaid coverage effects were observed for Pap testing (10.3% increase, 95% CI=8.8, 11.7) and mammography (14.5% increase, 95% CI= 10.1, 18.8). A positive Medicaid coverage effect was also observed for chlamydia testing (increase of 27.3%, 95% CI=14.1, 40.4) and lipid screening (increase of 8.0%, 95% CI=1.0, 15.0). No significant effect of Medicaid coverage was found on receipt of fecal occult blood testing, colonoscopy, glucose, or HbA1c screenings.
Table 3.
Estimated Treatment Effect of Medicaid Coverage via the Oregon Experiment on Preventive Services Receipt
| Screening outcome | N | Mean value (%) in control group (95% CI) |
Change (%) with Medicaid coverage (95% CI) |
p-value |
|---|---|---|---|---|
| BMI | 10,643 | 49.1 (45.6, 52.6) | 12.5 (10.6, 14.4) | <0.001 |
| Blood pressure | 10,643 | 61.5 (59.1, 63.8) | 10.1 (7.0, 13.3) | <0.001 |
| Smokinga | 10,643 | 56.4 (53.0, 59.7) | 6.2 (5.3, 7.1) | <0.001 |
| Pap test | 4,931 | 34.4 (32.5, 36.3) | 10.3 (8.8, 11.7) | <0.001 |
| Mammography | 2,661 | 38.2 (32.7, 43.7) | 14.5 (10.1, 18.8) | <0.001 |
| FOBT | 2,531 | 19.1 (11.8, 26.4) | −0.2 (−5.1, 4.7) | 0.933 |
| Colonoscopy | 2,531 | 9.4 (7.3, 11.4) | 2.7 (−1.7, 7.1) | 0.235 |
| Chlamydia | 366 | 28.7 (26.5, 31.0) | 27.3 (14.1, 40.4) | <0.001 |
| Lipid screeninga | 10,407 | 32.9 (27.3, 38.4) | 8.0 (1.0, 15.0) | 0.026 |
| Influenza vaccination | 2,505 | 37.8 (31.5, 44.0) | −0.4 (−8.3, 7.5) | 0.922 |
| Glucose | 4,082 | 55.9 (51.5, 60.3) | 4.8 (−3.0, 12.7) | 0.227 |
| HbA1c | 728 | 71.9 (69.5, 74.4) | 0.8 (−4.0, 5.7) | 0.732 |
Note: Boldface indicates statistical significance (p<0.05). Estimated statistics using bivariate probit instrumental variable model. Models adjusted for same covariate set as intent-to-treat models.
Selection status in Oregon Experiment was the only instrument in this model based on test of overidentifying restrictions.
Discussion
Previous studies of the Oregon Experiment examined the impact of a Medicaid expansion on self-reported healthcare utilization and service receipt in the general population.21,22,25,40 This study extends that work to evaluate the effect of a Medicaid expansion on receipt of preventive services in CHCs, a setting likely to be impacted by ACA Medicaid expansions, as most CHC patients are uninsured or Medicaid recipients.41 This study also expands on prior examination of the Oregon Experiment by including a longer follow-up (36 months) and using EHR data from a linked system to objectively measure receipt of preventive services.20,21 EHR data can overcome potential biases that result when asking patients to recall service receipt, particularly over a long period of time.42–44 The randomization component of the Oregon Experiment enabled examination of [MM3]both the effect of being selected to apply for Medicaid coverage on utilization of CHC services, and the isolated effect of actually gaining Medicaid coverage.
The findings strengthen the survey-based evidence from other Oregon Experiment studies regarding the causal link between health insurance and receipt of breast and cervical cancer screening.20,21 Similar to those studies no significant effect of insurance on influenza vaccination was found. Interestingly, Medicaid coverage positively affected screenings for BMI, blood pressure, and smoking (not assessed in previous Oregon Experiment studies), despite the fact that these services are usually performed at most visits and do not generate a separate billing charge. Based on post-hoc analyses (results not shown), one possible explanation for these findings is that insured patients had a higher primary care office visit rate than those who were uninsured, increasing the odds that these routine services would be performed. It should be noted that although the authors did not find statistically significant differences in glucose and HbA1c testing and colorectal cancer screenings by insurance coverage, there was a trend toward Medicaid coverage having a positive effect on these outcomes.
Policy Implications
These findings can help inform what to expect as an increasing number of uninsured patients gain coverage via the ACA insurance expansions.45 CHCs provide critical access to millions of uninsured and underinsured Americans and do an excellent job of providing quality services.27,46–51 However, previous studies show that without insurance coverage, CHC patients cannot always obtain all recommended services; having a primary care medical home and health insurance coverage is optimal.4,52–55 The finding that CHC patients who gained insurance coverage in the Oregon Experiment had increased rates of receipt of many preventive care services suggests that ACA Medicaid expansions could potentially lead to better access to preventive healthcare services for many Americans. Another ACA provision that requires most health plans to cover evidence-based preventive services without cost sharing will further increase this access: About 71 million Americans with private insurance gained access to fully covered preventive services in 2010–2011 with no co-pay.56 Without cost sharing, it is reassuring that discussion of preventive care receipt for insured patients may no longer have to include whether or not a patient can afford the out-of-pocket costs that used to be associated with many of these services. However, it is important to remember that an estimated 30 million Americans might remain uninsured, despite ACA insurance expansions.57 The findings also suggest that these people are much less likely to receive many recommended preventive services, and that continued effort is needed to increase access to insurance and health care in this population.
Limitations
Analyses were limited to the 49 Oregon CHCs that had fully implemented the OCHIN EHR before March 11, 2008 to be able to fully capture documented data on preventive services over the 36-month follow-up. This resulted in small sample sizes and reduced power for some preventive service categories, likely explaining the trend toward Medicaid coverage having a positive effect on colon cancer and glucose screenings but not reaching the level of statistical significance. This study was conducted in Oregon CHCs; patients seeking care outside this state and setting may behave differently. Further, the majority of the sample was already receiving care at the Oregon CHCs prior to the Oregon Experiment; thus, the results may not generalize to other patient populations such as those seeking care for the first time via the ACA, or among patients less engaged in their health care. The observed percentage receipt of most screening outcomes during the 36-month follow-up was slightly lower than other studies,51 likely because the authors did not limit the sample to patients with a primary care visit during the post-period (68% of the selected group and 66% of those not selected had one or more primary care visit in the post-period). The authors also were unable to assess the extent to which patients sought care outside the OCHIN network. If a patient gained insurance and left the OCHIN network, this would diminish the percentage receipt of preventive services for the Medicaid coverage group and thus bias the effects towards the null.28 Additionally, gaining Medicaid was defined as having ≥6 months of continuous Medicaid coverage in the post-period. If subjects in the Medicaid group lost coverage after 6 months, this could adversely affect preventive service receipt later in the study period; thus, the observed treatment effects may be underestimated.
Conclusions
Utilizing the Oregon Experiment, a randomized natural experiment, this study demonstrates a causal relationship between Medicaid coverage and receipt of several preventive services in CHC patients, including receipt of breast and cervical cancer screenings as well as screenings for BMI, blood pressure, and smoking, during a 3-year follow-up.
Figure 1.
CONSORT diagram of the study.
*Subset of 515,575 total OCHIN patients sent for linkage with an encounter at a clinic live on EHR by the earliest study date (March 11, 2008)
Acknowledgments
This study was supported by grants R01HL107647 from the National Heart, Lung, and Blood Institute and K08 HS021522–02 from the Agency for Healthcare Research and Quality. The funding agencies had no involvement in the preparation, review, or approval of the manuscript. We thank Heather Angier and Eve Dexter for their contributions, and gratefully acknowledge the OCHIN community health centers and Practice-Based Research Network.
Appendix Table 1
Demographic Characteristics of Patients on the Medicaid ‘Reservation List’ That Were Probabilistically Matched to OCHIN EHR Data and Included in the Study Sample Versus Those That Were Not
| Study sample N=11,041 |
Not in study sample N=89,366 |
|
|---|---|---|
| no. (column %) | no. (column %) | |
| Gender | ||
| Female | 6,034 (54.7) | 47,080 (52.7) |
| Male | 5,007 (45.3) | 42,286 (47.3) |
| Age | ||
| Mean (SD)a | 39.9 (12.5) | 39.8 (13.3) |
| Language | ||
| English | 9,195 (83.3) | 72,222 (80.8) |
| Spanish | 542 (4.9) | 3,918 (4.4) |
| Other/Unknown | 1,304 (11.8) | 13,226 (14.8) |
| Urban-rural status | ||
| Urban | 10,809 (97.9) | 83,635 (93.6) |
| Rural | 197 (1.8) | 5,441 (6.1) |
| Unknown | 35 (0.3) | 290 (0.3) |
Note: To identify individuals common to both the Medicaid reservation list and the OCHIN patient population, we used LinkPlus software to probabilistically compare demographic variables contained in both datasets. Matching variables included first and last name, date of birth, gender, street address, city, Oregon Medicaid identification number, and preferred language. The software generates a “match score” indicating each pair’s likelihood of being a match. For pairs of uncertain match status based on match score, we conducted double clerical review by independent reviewers. We also completed several rounds of quality assurance analyses to verify the validity of our match results.
Two-sample t-test
Appendix Table 2
Outcome Measure Specifications
| Metric | Denominator | Numerator | Areas of EHR included in search |
|---|---|---|---|
| BMI assessment | All patients | Patients in the denominator with at least one of the following documented in measurement period: MU ICD-9-CM grouper1 Standard Concept Id N_c160 (physical exam finding: BMI percentile); ICD-9-CM diagnosis codes V85.0-V85.4; Height and weight recorded at same encounter. | Encounter vital signs, Encounter diagnoses, Problem list |
| Blood pressure assessment | All patients | Patients in the denominator with systolic and diastolic blood pressure recorded at same encounter(s) in study period. | Encounter vital signs |
| Smoking status assessment | All patients | Patients in the denominator with smoking status recorded at one or more encounters in measurement period. | Social history2 |
| Cervical cancer screening | Female patients ages 21–64. Exclusions: EHR documentation of hysterectomy. Hysterectomy: MU CPT grouper1 Standard Concept Id N_c273 (procedure performed: hysterectomy); MU ICD-9-CM grouper1 Standard Concept Id N_c274 (procedure performed: hysterectomy); hysterectomy noted as reason for no last menstrual period in encounter record. |
Patients in the denominator with at least one of the following documented in measurement period: MU ICD-9-CM grouper1 Standard Concept Id N_c279 (laboratory test result: pap test); MU CPT grouper1 Standard Concept Id N_c277 (laboratory test result: pap test); MU HCPCS grouper1 Standard Concept Id N_c278 (laboratory test result: pap test). |
Hysterectomy: Encounter diagnoses, Problem list, Procedures, Medical history, Surgical history; Screening codes: Encounter diagnoses, Labs, Procedures, Problem list, Health maintenance3 |
| Breast cancer screening | Female patients age ≥40. Exclusions: EHR documentation of bilateral mastectomy. Mastectomy: MU CPT grouper1 Standard Concept Id N_c79 (procedure performed: unilateral mastectomy) |
Patients in the denominator with at least one of the following documented in measurement period: MU CPT grouper1 Standard Concept Id N_c72 (diagnostic study performed: breast cancer screening); MU HCPCS grouper1 Standard Concept Id N_c73 (diagnostic study performed: breast cancer screening); MU ICD-9-CM grouper1 Standard Concept Id N_c74 (diagnostic study performed: breast cancer screening); OCHIN internal use codes for equivalent procedures and referrals. | Bilateral mastectomy: Surgical history; Screening codes: Encounter diagnoses, Procedures, Referrals, Health maintenance3 |
| Colorectal cancer screening | Patients age ≥50. Exclusions: EHR documentation of colorectal cancer history, total colectomy, completed colonoscopy within 10 years, or completed flexible sigmoidoscopy within 5 years. Colorectal cancer history: MU ICD-9-CM grouper1 Standard Concept Id N_c520 (diagnosis active/inactive/resolved: colorectal cancer). Total colectomy: MU CPT grouper1 Standard Concept Id N_c36 (procedure performed: total colectomy). Colonoscopy and flexible sigmoidoscopy: see Numerator column. |
Patients in the denominator with at least one of the following documented in measurement period: MU CPT grouper1 Standard Concept Ids: N_c18 (procedure performed: colonoscopy), N_c29 (procedure performed: flexible sigmoidoscopy), N_c13 (laboratory test performed: FOBT); MU HCPCS grouper1 Standard Concept Ids: N_c32 (procedure performed: colonoscopy), N_c30 (procedure performed: flexible sigmoidoscopy), N_c17 (laboratory test performed: FOBT); HCPCS code G0120; MU ICD-9-CM grouper1 Standard Concept Id N_c15 (laboratory test performed: FOBT); MU LOINC grouper1 Standard Concept Id N_c16 (laboratory test performed: FOBT); OCHIN internal use codes for equivalent labs and referrals. | Colorectal cancer history and total colectomy: Encounter diagnoses, Procedures, Problem list, Medical history, Surgical history; Screening codes: Encounter diagnoses, Labs, Procedures, Problem list, Surgical history, Referrals, Health maintenance3 |
| Colonoscopy | Patients age ≥50. Exclusions: EHR documentation of colorectal cancer history, total colectomy, completed colonoscopy within 10 years, or completed flexible sigmoidoscopy within 5 years. Colorectal cancer history: MU ICD-9-CM grouper1 Standard Concept Id N_c520 (diagnosis active/inactive/resolved: colorectal cancer). Total colectomy: MU CPT grouper1 Standard Concept Id N_c36 (procedure performed: total colectomy). Colonoscopy and flexible sigmoidoscopy: see Numerator column. |
Patients in the denominator with at least one of the following documented in measurement period: MU CPT grouper1 Standard Concept Id N_c18 (procedure performed: colonoscopy); MU HCPCS grouper1 Standard Concept Id N_c32 (procedure performed: colonoscopy); OCHIN internal use codes for equivalent referrals. | Colorectal cancer history and total colectomy: Encounter diagnoses, Procedures, Problem list, Medical history, Surgical history; Screening codes: Procedures, Surgical history, Referrals, Health maintenance3 |
| Fecal occult blood test (FOBT) | Patients age ≥50. Exclusions: EHR documentation of colorectal cancer history, total colectomy, completed colonoscopy within 10 years, or completed flexible sigmoidoscopy within 5 years. Colorectal cancer history: MU ICD-9-CM grouper1 Standard Concept Id N_c520 (diagnosis active/inactive/ resolved: colorectal cancer). Total colectomy: MU CPT grouper1 Standard Concept Id N_c36 (procedure performed: total colectomy). Colonoscopy and flexible sigmoidoscopy: see Numerator column. |
Patients in the denominator with at least one of the following documented in measurement period: MU CPT grouper1 Standard Concept Id N_c13 (laboratory test performed: FOBT); MU HCPCS grouper1 Standard Concept Id N_c17 (laboratory test performed: FOBT); MU ICD-9-CM grouper1 Standard Concept Id N_c15 (laboratory test performed: FOBT); MU LOINC grouper1 Standard Concept Id N_c16 (laboratory test performed: FOBT); OCHIN internal use codes for equivalent labs. | Colorectal cancer history and total colectomy: Encounter diagnoses, Procedures, Problem list, Medical history, Surgical history; Screening codes: Encounter diagnoses, Procedures, Labs, Problem list, Referrals, Health maintenance3 |
| Chlamydia screening | Sexually active female patients ages 19–24. Codes indicative of sexually active woman: MU CPT grouper1 Standard Concept Id N_c207 (procedure performed: procedures indicative of sexually active woman); MU HCPCS grouper1 Standard Concept Id N_c208 (procedure performed: procedures indicative of sexually active woman); MU ICD-9-CM grouper1 Standard Concept Id N_c580 (diagnosis active: sexually active woman); MU LOINC grouper1 Standard Concept Id N_c210 (laboratory test performed: Laboratory tests indicative of sexually active woman); Internal OCHIN grouper “Diagnosis Concept: Sexually Transmitted Disease”; Social History2 sexually active flag. |
Patients in the denominator with at least one of the following documented in measurement period: MU LOINC grouper1 Standard Concept Id N_c219 (laboratory test result: chlamydia screening); Internal OCHIN grouper “Health Maintenance – Chlamydia Satisfying Procedure”. | Sexually active codes: Encounter diagnoses, Labs, Procedures, Problem list, Social history2; Screening codes: Labs, Procedures, Health maintenance3 |
| Cholesterol screening | Patients age ≥20. | Patients in the denominator with at least one of the following documented in measurement period: MU CPT grouper1 Standard Concept Ids: N_c156 (laboratory test performed: LDL), N_c183 (laboratory test performed: HDL), N_c180 (laboratory test performed: Total Cholesterol), N_c186 (laboratory test performed: Triglycerides); MU LOINC grouper1 Standard Concept Ids: N_c157 (laboratory test performed: LDL), N_c184 (laboratory test performed: HDL), N_c181 (laboratory test performed: Total Cholesterol), N_c187 (laboratory test performed: Triglycerides). | Procedures, Labs, Health maintenance3 |
| Influenza vaccine | Patients age ≥50. Exclusions: Documentation of vaccine allergy/contraindication or patient declined. | Patients in the denominator with at least one of the following documented in measurement period: CPT codes 90653, 90654, 90655, 90656, 90657, 90658, 90659, 90660, 90661, 90662, 90663, 90664, 90666, 90667, 90668, 90672, 90685, 90686, 90687, 90688, G0008, Q2038; OCHIN internal use codes for equivalent procedures and immunizations. | Exclusion: Allergies, Immunizations; Vaccine codes: Immunizations, Procedures, Health maintenance3 |
| Pneumococcal vaccine | Patients with a diagnosis of diabetes, asthma, or coronary artery disease by start of measurement period. Exclusions: Documentation of vaccine allergy/contraindication or patient declined. Diabetes: MU ICD-9-CM grouper1 Standard Concept Id N_c47 (diagnosis active: diabetes). Asthma: MU ICD-9-CM grouper1 Standard Concept Id A_c221 (diagnosis active: asthma). CAD: MU ICD-9-CM grouper1 Standard Concept Id A_c122 (diagnosis active: Coronary Artery Disease includes MI); MU CPT grouper1 Standard Concept Id A_c169 (procedure performed: Cardiac Surgery). | Patients in the denominator with at least one of the following documented in measurement period: MU RxNorm grouper1 Standard Concept Id N_c421 (medication administered: pneumococcal vaccination); CPT codes 4040F, 90669, 90670, 90732, G0009, S0195; OCHIN internal use codes for equivalent procedures. | Exclusion: Allergies, Immunizations; Diabetes, asthma, and CAD diagnoses: Encounter diagnoses, Problem list, Surgical history; Vaccine codes: Procedures, Medications, Immunizations, Health maintenance3 |
| Glucose screening | Patients age ≥45. | Patients in the denominator with at least one of the following documented in measurement period: LOINC codes 1492–8, 1494–4, 1496-9, 1499-3, 1501-6, 1502-4, 1504-0, 1507-3, 1508-1, 1514-9, 1515-6, 1518-0, 1530-5, 1531-3, 1533-9, 1554-5, 1557-8, 1558-6, 6749-6, 9375-7, 10450-5, 14753-8, 14754-6, 14756-1, 14757-9, 14759-5, 14764-5, 14765-2, 14771-0, 14995-5, 17865-7, 20436-2, 20437-0, 20438-8, 25666-9, 26554-6, 30251-3, 30265-3, 30267-9, 32320-4, 40285-9, 40286-7, 41024-1, 49134-0, 51597-3, 55351-1, 55381-8, 10449-7, 12610-2, 12646-6, 1521-4, 2345-7, 25428-4, 27353-2, 1527-1, 1469-9, 1539-6, 1542-0, 2348-1, 2349-9, 6760-3; CPT codes 80047, 80048, 80053, 80050, 80069, 82947, 82950, 82951, 82948, 82952; OCHIN internal use codes for equivalent procedures. | Procedures, Labs |
| HbA1c measurement | Patients with a diagnosis of diabetes. Diabetes: MU ICD-9-CM grouper1 Standard Concept Id N_c47 (diagnosis active: diabetes). | Patients in the denominator with at least one of the following documented in measurement period: MU LOINC grouper1 Standard Concept Id N_c87 (laboratory test result: HbA1c test); N groupers: “Health Maintenance – Hemoglobin A1C procedures”; “Health Maintenance – Diabetes HgbA1c satisfying procedures” | Diabetes diagnosis: Encounter diagnoses, Problem list; Screening codes: Procedures, Labs, Health maintenance3 |
CPT, Current Procedural Terminology; EHR, electronic health record; HCPCS, Healthcare Common Procedure Coding System; LOINC, Logical Observation Identifiers Names and Codes; MU, Meaningful Use
Meaningful Use groupers created for OCHIN reporting based on specified Standard Concept identifier from Clinical Quality Measures for Eligible Professionals. www.ushik.ahrq.gov/mdr/portals.
Social history is the area of the EHR used to record sexuality and substance use
Health maintenance is the EHR’s preventive health tool that is used to remind patients and providers when appropriate preventive services are due
Appendix Table 3A
Demographic Characteristics for BMI, Blood Pressure, and Smoking Screening Subpopulation Study Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=10,643)
| Selected N=4,049 |
Not selected N=6,594 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | 0.734 | ||
| Female | 2,231 (55.1) | 3,611 (54.8) | |
| Male | 1,818 (44.9) | 2,983 (45.2) | |
| Age | |||
| Mean (SD)b | 39.2 (11.7) | 39.5 (11.9) | 0.185 |
| Race/Ethnicity | 0.263 | ||
| Hispanic, any race | 548 (13.5) | 867 (13.2) | |
| Non-Hispanic, white | 2,447 (60.4) | 3,949 (59.9) | |
| Non-Hispanic, other | 795 (19.6) | 1,412 (21.4) | |
| Unknown | 259 (6.4) | 366 (5.6) | |
| Average FPLc | 0.827 | ||
| <100% | 2,911 (71.9) | 4,772 (72.4) | |
| ≥100% | 1,101 (27.2) | 1,766 (26.8) | |
| Missing/Unknown | 37 (0.9) | 56 (0.9) | |
| Number of chronic conditions diagnosed prior to selection dated | <0.001 | ||
| 0 | 2,394 (59.1) | 3,936 (59.7) | |
| 1 | 567 (14) | 1,083 (16.4) | |
| 2 | 261 (6.5) | 442 (6.7) | |
| 3–5 | 135 (3.3) | 272 (4.1) | |
| No data to assess | 692 (17.1) | 861 (13.1) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3B
Demographic Characteristics for Pap Screening Subpopulation Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=4,931)
| Selected N=1,872 |
Not selected N=3,059 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | NA | ||
| Female | 1,872 (100.0) | 3,059 (100.0) | |
| Male | 0 (0.0) | 0 (0.0) | |
| Age | |||
| Mean (SD)b | 37.9 (10.9) | 38.6 (11.4) | 0.032 |
| Race/Ethnicity | 0.263 | ||
| Hispanic, any race | 338 (18.1) | 516 (16.87) | |
| Non-Hispanic, white | 1,061 (56.7) | 1,710 (55.9) | |
| Non-Hispanic, other | 364 (19.4) | 663 (21.7) | |
| Unknown | 109 (5.8) | 170 (5.6) | |
| Average FPLc | 0.970 | ||
| <100% | 1,325 (70.8) | 2,167 (70.8) | |
| ≥100% | 531 (28.4) | 868 (28.4) | |
| Missing/Unknown | 16 (0.9) | 24 (0.8) | |
| Number of chronic conditions diagnosedprior to selection dated | 0.008 | ||
| 0 | 1,197 (63.9) | 1,934 (63.2) | |
| 1 | 237 (12.7) | 467 (15.3) | |
| 2 | 110 (5.9) | 183 (6.0) | |
| 3–5 | 52 (2.8) | 106 (3.5) | |
| No data to assess | 276 (14.7) | 369 (12.1) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3C
Demographic Characteristics for Mammography Screening Subpopulation Study Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=3,661)
| Selected N=979 |
Not selected N=1,682 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | NA | ||
| Female | 979 (100.0) | 1,682 (100.0) | |
| Male | 0 (0.0) | 0 (0.0) | |
| Age | |||
| Mean (SD)b | 49.0 (5.8) | 49.4 (6.0) | 0.128 |
| Race/Ethnicity | 0.340 | ||
| Hispanic, any race | 105 (10.7) | 161 (9.6) | |
| Non-Hispanic, white | 633 (64.7) | 1,065 (63.3) | |
| Non-Hispanic, other | 186 (19) | 366 (21.8) | |
| Unknown | 55 (5.6) | 90 (5.4) | |
| Average FPLc | 0.652 | ||
| <100% | 692 (70.7) | 1,206 (71.7) | |
| ≥100% | 278 (28.4) | 465 (27.7) | |
| Missing/Unknown | 9 (0.9) | 11 (0.7) | |
| Number of chronic conditions diagnosed prior to selection dated | 0.126 | ||
| 0 | 442 (45.2) | 788 (46.9) | |
| 1 | 192 (19.6) | 337 (20.0) | |
| 2 | 106 (10.8) | 191 (11.4) | |
| 3–5 | 59 (6.03) | 120 (7.1) | |
| No data to assess | 180 (18.4) | 246 (14.6) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3D
Demographic Characteristics for FOBT and Colonoscopy Screening Subpopulation Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=2,531)
| Selected N=951 |
Not selected N=1,580 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | 0.060 | ||
| Female | 445 (46.8) | 790 (50.0) | |
| Male | 506 (53.2) | 790 (50.0) | |
| Age | |||
| Mean (SD)b | 54.4(3.2) | 54.6(3.4) | 0.141 |
| Race/Ethnicity | 0.060 | ||
| Hispanic, any race | 56 (5.9) | 129 (8.2) | |
| Non-Hispanic, white | 651 (68.5) | 1,012 (64.1) | |
| Non-Hispanic, other | 192 (20.2) | 355 (22.5) | |
| Unknown | 52 (5.5) | 84 (5.3) | |
| Average FPLc | 0.963 | ||
| <100% | 686 (72.1) | 1,145 (72.5) | |
| ≥100% | 256 (26.9) | 421 (26.7) | |
| Missing/Unknown | 9 (1.0) | 14 (0.90) | |
| Number of chronic conditions diagnosed prior to selection dated | <0.001 | ||
| 0 | 359 (37.8) | 601 (38.0) | |
| 1 | 188 (19.8) | 374 (23.7) | |
| 2 | 125 (13.1) | 223 (14.1) | |
| 3–5 | 71 (7.5) | 157 (9.9) | |
| No data to assess | 208 (21.9) | 225 (14.2) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL=federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3E
Demographic Characteristics for Chlamydia Screening Subpopulation Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=366)
| Selected N=133 |
Not selected N=233 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | NA | ||
| Female | 133 (100.0) | 233 (100.0) | |
| Male | 0 (0.0) | 0 (0.0) | |
| Age | |||
| Mean (SD)b | 20.1 (0.8) | 20.1 (0.8) | 0.972 |
| Race/Ethnicity | 0.859 | ||
| Hispanic, any race | 26 (19.6) | 38 (16.3) | |
| Non-Hispanic, white | 67 (50.4) | 124 (53.2) | |
| Non-Hispanic, other | 34 (25.6) | 62 (26.6) | |
| Unknown | 6 (4.5) | 9 (3.9) | |
| Average FPLc | 0.223 | ||
| <100% | 102 (76.7) | 164 (70.4) | |
| ≥100% | 31 (23.3) | 69 (29.6) | |
| Missing/Unknown | 0 (0.0) | 0 (0.0) | |
| Number of chronic conditions diagnosed prior to selection dated | 0.051 | ||
| 0 | 117 (88.0) | 203 (87.1) | |
| 1 | 13 (9.8) | 30 (12.9) | |
| 2 | 3 (2.3) | 0 (0) | |
| 3–5 | 0 (0) | 0 (0) | |
| No data to assess | |||
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3F
Demographic Characteristics for Lipid Screening Subpopulation Study Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=10,407)
| Selected N=3,958 |
Not selected N=6,449 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | 0.732 | ||
| Female | 2,174 (54.9) | 3,520 (54.6) | |
| Male | 1,784 (45.1) | 2,929 (45.4) | |
| Age | |||
| Mean (SD)b | 39.6 (11.4) | 39.9 (11.6) | 0.184 |
| Race/Ethnicity | 0.070 | ||
| Hispanic, any race | 538 (13.6) | 848 (13.2) | |
| Non-Hispanic, white | 2,399 (60.6) | 3,868 (60.0) | |
| Non-Hispanic, other | 769 (19.4) | 1,372 (21.3) | |
| Unknown | 252 (6.4) | 361 (5.6) | |
| Average FPLc | 0.702 | ||
| <100% | 2,843 (71.8) | 4,673 (72.5) | |
| ≥100% | 1,078 (27.2) | 1,722 (26.7) | |
| Missing/Unknown | 37 (0.9) | 54 (0.8) | |
| Number of chronic conditions diagnosed prior to selection dated | <0.001 | ||
| 0 | 2,310 (58.4) | 3,814 (59.1) | |
| 1 | 562 (14.2) | 1,071 (16.6) | |
| 2 | 261 (6.6) | 442 (6.9) | |
| 3–5 | 135 (3.4) | 272 (4.2) | |
| No data to assess | 690 (17.4) | 850 (13.2) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3G
Demographic Characteristics for Flu Vaccine Subpopulation Study Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=2,505)
| Selected N=948 |
Not selected N=1,557 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | 0.156 | ||
| Female | 446 (47.1) | 778 (50.0) | |
| Male | 502 (53.0) | 779 (50.0) | |
| Age | |||
| Mean (SD)b | 54.4(3.2) | 54.6(3.4) | 0.151 |
| Race/Ethnicity | 0.061 | ||
| Hispanic, any race | 57 (6.0) | 126 (8.1) | |
| Non-Hispanic, white | 652 (68.8) | 998 (64.1) | |
| Non-Hispanic, other | 188 (19.8) | 350 (22.5) | |
| Unknown | 51 (5.4) | 83 (5.3) | |
| Average FPLc | 0.994 | ||
| <100% | 687 (72.5) | 1,127 (72.4) | |
| ≥100% | 252 (26.6) | 416 (26.7) | |
| Missing/Unknown | 9 (1.0) | 14 (0.9) | |
| Number of chronic conditions diagnosed prior to selection dated | <0.001 | ||
| 0 | 358 (37.8) | 599 (38.5) | |
| 1 | 185 (19.5) | 359 (23.1) | |
| 2 | 124 (13.1) | 223 (14.3) | |
| 3–5 | 73 (7.7) | 151 (9.7) | |
| No data to assess | 208 (21.9) | 225 (14.5) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3H
Demographic Characteristics for Glucose Screening Subpopulation Study Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=4,082)
| Selected N=1,506 |
Not selected N=2,576 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | 0.352 | ||
| Female | 718 (47.7) | 1,267 (49.2) | |
| Male | 788 (52.3) | 1,309 (50.8) | |
| Age | |||
| Mean (SD)b | 51.7(4.5) | 51.7(4.7) | 0.838 |
| Race/Ethnicity | 0.385 | ||
| Hispanic, any race | 109 (7.2) | 209 (8.1) | |
| Non-Hispanic, white | 1,008 (66.9) | 1,660 (64.4) | |
| Non-Hispanic, other | 305 (20.3) | 564 (21.9) | |
| Unknown | 84 (5.6) | 143 (5.6) | |
| Average FPLc | 0.709 | ||
| <100% | 1,096 (72.8) | 1,894 (73.5) | |
| ≥100% | 396 (26.3) | 663 (25.7) | |
| Missing/Unknown | 14 (0.9) | 19 (0.7) | |
| Number of chronic conditions diagnosed prior to selection dated | <0.001 | ||
| 0 | 615 (40.8) | 1,123 (43.6) | |
| 1 | 303 (20.1) | 554 (21.5) | |
| 2 | 174 (11.6) | 305 (11.8) | |
| 3–5 | 98 (6.5) | 215 (8.4) | |
| No data to assess | 316 (21.0) | 379 (14.7) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
Appendix Table 3I
Demographic Characteristics for HbA1c Screening Subpopulation Study Sample by Oregon OCHIN Patients Selected to Apply for Health Insurance Coverage via Oregon Experiment vs. Not Selected to Apply (N=728)
| Selected N=248 |
Not selected N=480 |
p-valuea | |
|---|---|---|---|
| no. (column %) | no. (column %) | ||
| Gender | 0.717 | ||
| Female | 121 (48.8) | 241 (50.2) | |
| Male | 127 (51.2) | 239 (49.8) | |
| Age | |||
| Mean (SD)b | 47.4 (8.9) | 46.8792 (9.8) | 0.445 |
| Race/Ethnicity | 0.371 | ||
| Hispanic, any race | 47 (19.0) | 94 (19.6) | |
| Non-Hispanic, white | 142 (57.3) | 245 (51.0) | |
| Non-Hispanic, other | 52 (21.0) | 126 (26.3) | |
| Unknown | 7 (2.8) | 15 (3.1) | |
| Average FPLc | 0.856 | ||
| <100% | 186 (75) | 363 (75.6) | |
| ≥100% | 62 (25) | 117 (24.4) | |
| Missing/Unknown | 0 (0.0) | 0 (0.0) | |
| Number of chronic conditions diagnosed prior to selection dated | 0.909 | ||
| 0 | 0 (0.0) | 0 (0.0) | |
| 1 | 58 (23.4) | 108 (22.5) | |
| 2 | 81 (32.7) | 151 (31.5) | |
| 3–5 | 108 (43.6) | 220 (45.8) | |
| No data to assess | 1 (0.4) | 1 (0.2) | |
Note: Boldface indicates statistical significance (p<0.05).
p-values for chi-square test unless otherwise noted
Two-sample t-test
FPL, federal poverty level; values ≥1,000% FPL were set to missing (affected less than 1% of observations). Fisher’s exact test due to low cell counts in missing/unknown category.
Chronic conditions assessed: asthma, coronary artery disease, diabetes, dyslipidemia, hypertension
References
- 1.Bailey SR, O’Malley JP, Gold R, Heintzman J, Likumahuwa S, DeVoe JE. Diabetes care quality is highly correlated with patient panel characteristics. J Am Board Fam Med. 2013;26(6):669–679. doi: 10.3122/jabfm.2013.06.130018. http://dx.doi.org/10.3122/jabfm.2013.06.130018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freeman JD, Kadiyala S, Bell JF, Martin DP. The causal effect of health insurance on utilization, outcomes in adults: a systematic review of U.S studies. Med Care. 2008;46(10):1023–1032. doi: 10.1097/MLR.0b013e318185c913. http://dx.doi.org/10.1097/MLR.0b013e318185c913. [DOI] [PubMed] [Google Scholar]
- 3.Buchmueller TC, Grumbach K, Kronick R, Kahn JG. The effect of health insurance on medical care utilization and implications for insurance expansion: A review of the literature. Med Care Res Rev. 2005;62(1):3–30. doi: 10.1177/1077558704271718. http://dx.doi.org/10.1177/1077558704271718. [DOI] [PubMed] [Google Scholar]
- 4.DeVoe J, Fryer G, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93:786–791. doi: 10.2105/ajph.93.5.786. http://dx.doi.org/10.2105/AJPH.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duru OK, Vargas RB, Kermah D, Pan D, Norris KC. Health insurance status and hypertension monitoring and control in the United States. Am J Hypertens. 2007;20(4):348–353. doi: 10.1016/j.amjhyper.2006.11.007. http://dx.doi.org/10.1016/j.amjhyper.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 6.McMorrow S, Kenney GM, Goin D. Determinants of Receipt of Recommended Preventive Services: Implications for the Affordable Care Act. Am J Public Health. 2014;104(12):2392–2399. doi: 10.2105/AJPH.2013.301569. http://dx.doi.org/10.2105/AJPH.2013.301569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cowburn S, Carlson M, Lapidus J, Heintzman J, Bailey S, DeVoe J. Insurance continuity and human papillomavirus vaccine uptake in Oregon and California federally qualified health centers. Am J Public Health. 2014;104(9):e71–79. doi: 10.2105/AJPH.2014.302007. http://dx.doi.org/10.2105/AJPH.2014.302007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holden CD, Chen J, Dagher RK. Preventive care utilization among the uninsured by race/ethnicity and income. Am J Prev Med. 2015;48(1):13–21. doi: 10.1016/j.amepre.2014.08.029. http://dx.doi.org/10.1016/j.amepre.2014.08.029. [DOI] [PubMed] [Google Scholar]
- 9.Kaiser Family Foundation. [Accessed June 10, 2015];The Medicaid program at a glance. Publication 7235-05; 2012. www.kff.org/medicaid/7235.cfm.
- 10.Kaiser Family Foundation. [Accessed June 10, 2015];How is the ACA Impacting Medicaid Enrollment? 2014 http://kff.org/medicaid/issue-brief/how-is-the-aca-impacting-medicaid-enrollment/.
- 11.Abraham JM. How might the Affordable Care Act’s coverage expansion provisions influence demand for medical care? Milbank Q. 2014;92(1):63–87. doi: 10.1111/1468-0009.12041. http://dx.doi.org/10.1111/1468-0009.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ku L, Jones K, Shin P, Bruen B, Hayes K. The states’ next challenge--securing primary care for expanded Medicaid populations. N Engl J Med. 2011;364(6):493–495. doi: 10.1056/NEJMp1011623. http://dx.doi.org/10.1056/NEJMp1011623. [DOI] [PubMed] [Google Scholar]
- 13.Schoen C, Hayes SL, Radley DC, Collins SR. Access to Primary and Preventive Health Care Across States Prior to the Coverage Expansions of the Affordable Care Act. Commonwealth Fund. 2014;17 (Issue Brief) [PubMed] [Google Scholar]
- 14.Clark CR, Soukup J, Riden H, et al. Preventive care for low-income women in Massachusetts post-health reform. J Womens Health (Larchmt) 2014;23(6):493–498. doi: 10.1089/jwh.2013.4612. http://dx.doi.org/10.1089/jwh.2013.4612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okoro CA, Dhingra SS, Coates RJ, Zack M, Simoes EJ. Effects of Massachusetts Health Reform on the Use of Clinical Preventive Services. J Gen Intern Med. 2014;29(9):1287–1295. doi: 10.1007/s11606-014-2865-2. http://dx.doi.org/10.1007/s11606-014-2865-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keating NL, Kouri EM, He Y, West DW, Winer EP. Effect of Massachusetts health insurance reform on mammography use and breast cancer stage at diagnosis. Cancer. 2013;119(2):250–258. doi: 10.1002/cncr.27757. http://dx.doi.org/10.1002/cncr.27757. [DOI] [PubMed] [Google Scholar]
- 17.Kolstad J, Kowalkski AE. The impact of health care reform on hospital and preventive care: Evidence from Massachusetts. J Public Econ. 2012;96:909–929. doi: 10.1016/j.jpubeco.2012.07.003. http://dx.doi.org/10.1016/j.jpubeco.2012.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Der Wees PJ, Zaslavsky AM, Ayanian JZ. Improvements in health status after Massachusetts health care reform. Milbank Q. 2013;91(4):663–689. doi: 10.1111/1468-0009.12029. http://dx.doi.org/10.1111/1468-0009.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Allen H, Baicker K, Finkelstein A, Taubman S, Wright BJ, Group OHS. What the Oregon health study can tell us about expanding Medicaid. Health Aff (Millwood) 2010;29(8):1498–1506. doi: 10.1377/hlthaff.2010.0191. http://dx.doi.org/10.1377/hlthaff.2010.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. http://dx.doi.org/10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finkelstein A, Taubman S, Wright B, et al. The Oregon Health Insurance Experiment: Evidence from the First Year. Q J Econ. 2012;127(3):1057–1106. doi: 10.1093/qje/qjs020. http://dx.doi.org/10.1093/qje/qjs020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taubman SL, Allen HL, Wright BJ, Baicker K, Finkelstein AN. Medicaid Increases Emergency-Department Use: Evidence from Oregon’s Health Insurance Experiment. Science. 2014;343(6168):263–268. doi: 10.1126/science.1246183. http://dx.doi.org/10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oregon Division of Medical Assistance Programs. [Accessed June 10, 2015];OHP Standard Reservation List Final Report. 2008 www.oregon.gov/oha/healthplan/DataReportsDocs/OHP%20Standard%20Reservation%20List%20Final%20Report.pdf.
- 24.Oregon Department of Human Services, Programs DoMA. [Accessed June 2, 2015];Oregon Health Plan Annual Report: Medicaid and State Children’s Health Insurance Program Section 1115(a) Medicaid demonstration extension. 2008 www.oregon.gov/oha/healthplan/DataReportsDocs/FFY%202008%20Annual%20Report.pdf.
- 25.Baicker K, Taubman SL, Allen HL, et al. The Oregon experiment--effects of Medicaid on clinical outcomes. N Engl J Med. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. http://dx.doi.org/10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Association of Community Health Centers. [Accessed June 10, 2015];United States Health Center Fact Sheet. 2012 Available from: www.nachc.org/client//US12.pdf.
- 27.The White House. The Obama Administration and Community Health Centers. Washington, D.C: 2012. [Accessed June 10, 2015]. www.whitehouse.gov/sites/default/files/05-01-12_community_health_center_report.pdf. [Google Scholar]
- 28.Devoe JE, Gold R, McIntire P, Puro J, Chauvie S, Gallia CA. Electronic health records vs Medicaid claims: completeness of diabetes preventive care data in community health centers. Ann Fam Med. 2011;9(4):351–358. doi: 10.1370/afm.1279. http://dx.doi.org/10.1370/afm.1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Devoe JE, Gold R, Spofford M, et al. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice-based Research Network (SNW-PBRN) J Am Board Fam Med. 2011;24(5):597–604. doi: 10.3122/jabfm.2011.05.110052. http://dx.doi.org/10.3122/jabfm.2011.05.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Devoe JE, Sears A. The OCHIN community information network: bringing together community health centers, information technology, and data to support a patient-centered medical village. J Am Board Fam Med. 2013;26(3):271–278. doi: 10.3122/jabfm.2013.03.120234. http://dx.doi.org/10.3122/jabfm.2013.03.120234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. DHHS, CDC, National Center for Chronic Disease Prevention and Health Promotion. [Accessed June 10, 2015];Registry Plus, a suite of publicly available software programs for collecting and processing cancer registry data. 2010 www.cdc.gov/cancer/npcr/.
- 32.Sussman JB, Hayward RA. An IV for the RCT: using instrumental variables to adjust for treatment contamination in randomised controlled trials. BMJ. 2010;340:c2073. doi: 10.1136/bmj.c2073. http://dx.doi.org/10.1136/bmj.c2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Center for Medicaid and Medicare Services. [Accessed June 10, 2015];2011-2012 Eligible Professional Clinical Quality Measures (CQMs) 2012 http://ushik.ahrq.gov/MeaningfulUseMeasures?system=mu&enableAsynchronousLoading=true.
- 34.Heintzman J, Bailey SR, Hoopes MJ, et al. Agreement of Medicaid claims and electronic health records for assessing preventive care quality among adults. J Am Med Inform Assoc. 2014;21(4):720–724. doi: 10.1136/amiajnl-2013-002333. http://dx.doi.org/10.1136/amiajnl-2013-002333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.National Committee for Quality Assurance (NCQA) HEDIS 2013: Technical Specifications for Physician Measurement. Washington, DC: 2013. [Google Scholar]
- 36.Heckman J. Dummy Endogenous Variables in a Simultaneous Equation System. Econometrica. 1978;46(6):931–959. http://dx.doi.org/10.2307/1909757. [Google Scholar]
- 37.Greene W. Econometric analysis. 5th ed. Upper Saddle River, NJ: Prentice Hall; 2003. [Google Scholar]
- 38.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. http://dx.doi.org/10.1111/j.0006-341X.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- 39.Rogers W. Regression standard errors in clustered samples. Stata Technical Bulletin. 1994;3(13):19–23. [Google Scholar]
- 40.Baicker K, Finkelstein A. The effects of Medicaid coverage--learning from the Oregon experiment. N Engl J Med. 2011;365(8):683–685. doi: 10.1056/NEJMp1108222. http://dx.doi.org/10.1056/NEJMp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kaiser Commission on Medicaid and the Uninsured, Kaiser Family Foundation. [Accessed June 10, 2015];Community Health Centers: A 2012 Profile and Spotlight on Implications of State Medicaid Expansion Decisions. 2014 Sep; http://kaiserfamilyfoundation.files.wordpress.com/2014/09/8624-community-health-centers-a-2012-profile-and-implications-of-state-medicaid-expansion-decisions.pdf.
- 42.Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf) 2005;27(3):281–291. doi: 10.1093/pubmed/fdi031. http://dx.doi.org/10.1093/pubmed/fdi031. [DOI] [PubMed] [Google Scholar]
- 43.Choi BC, Pak AW. A catalog of b iases in questionnaires. Prev Chronic Dis. 2005;2(1):A13. [PMC free article] [PubMed] [Google Scholar]
- 44.Tisnado DM, Adams JL, Liu H, et al. What is the concordance between the medical record and patient self-report as data sources for ambulatory care? Med Care. 2006;44(2):132–140. doi: 10.1097/01.mlr.0000196952.15921.bf. http://dx.doi.org/10.1097/01.mlr.0000196952.15921.bf. [DOI] [PubMed] [Google Scholar]
- 45.Decker SL. In 2011 nearly one-third of physicians said they would not accept new Medicaid patients, but rising fees may help. Health Aff (Millwood) 2012;31(8):1673–1679. doi: 10.1377/hlthaff.2012.0294. http://dx.doi.org/10.1377/hlthaff.2012.0294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shi L, Stevens GD. The role of community health centers in delivering primary care to the underserved: experiences of the uninsured and Medicaid insured. J Ambul Care Manage. 2007;30(2):159–170. doi: 10.1097/01.JAC.0000264606.50123.6d. http://dx.doi.org/10.1097/01.JAC.0000264606.50123.6d. [DOI] [PubMed] [Google Scholar]
- 47.Bruen BK, Ku L, Lu X, Shin P. No evidence that primary care physicians offer less care to Medicaid, community health center, or uninsured patients. Health Aff (Millwood) 2013;32(9):1624–1630. doi: 10.1377/hlthaff.2012.1300. http://dx.doi.org/10.1377/hlthaff.2012.1300. [DOI] [PubMed] [Google Scholar]
- 48.Goldman LE, Chu PW, Tran H, Romano MJ, Stafford RS. Federally qualified health centers and private practice performance on ambulatory care measures. Am J Prev Med. 2012;43(2):142–149. doi: 10.1016/j.amepre.2012.02.033. http://dx.doi.org/10.1016/j.amepre.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Angier H, Hoopes M, Gold R, et al. An early look at rates of uninsured safety net clinic visits after the affordable care act. Ann Fam Med. 2015;13(1):10–16. doi: 10.1370/afm.1741. http://dx.doi.org/10.1370/afm.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.National Association of Community Health Centers. A sketch of community health centers. [Accessed June 10, 2015];Chart book. 2014 www.nachc.com/client//Chartbook_2014.pdf.
- 51.Heintzman J, Marino M, Hoopes M, et al. Using electronic health record data to evaluate preventive service utilization among uninsured safety net patients. Prev Med. 2014;67:306–310. doi: 10.1016/j.ypmed.2014.08.006. http://dx.doi.org/10.1016/j.ypmed.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gold R, DeVoe J, Shah A, Chauvie S. Insurance continuity and receipt of diabetes preventive care in a network of federally qualified health centers. Med Care. 2009;47(4):431–439. doi: 10.1097/mlr.0b013e318190ccac. http://dx.doi.org/10.1097/MLR.0b013e318190ccac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.DeVoe JE, Tillotson CJ, Lesko SE, Wallace LS, Angier H. The case for synergy between a usual source of care and health insurance coverage. J Gen Intern Med. 2011;26:1059–1066. doi: 10.1007/s11606-011-1666-0. http://dx.doi.org/10.1007/s11606-011-1666-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gold R, DeVoe JE, McIntire PJ, Puro JE, Chauvie SL, Shah AR. Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage. J Am Board Fam Med. 2012;25(1):42–49. doi: 10.3122/jabfm.2012.01.110142. http://dx.doi.org/10.3122/jabfm.2012.01.110142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bailey SR, O’Malley JP, Gold R, Heintzman J, Marino M, DeVoe JE. Receipt of diabetes preventive services differs by insurance status at visit. Am J Prev Med. 2015;48(2):229–233. doi: 10.1016/j.amepre.2014.08.035. http://dx.doi.org/10.1016/j.amepre.2014.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.U.S. DHHS. Affordable Care Act Rules on Expanding Access to Preventive Services for Women. [Accessed June 10, 2015];HHS.gov/HealthCare. 2013 www.hhs.gov/healthcare/facts/factsheets/2011/08/womensprevention08012011a.html.
- 57.Kaiser Family Foundation. [Accessed June 10, 2015];Adults who remained uninsured at the end of 2014. 2015 Jan 29; http://kff.org/report-section/adults-who-remained-uninsured-at-the-end-of-2014-issue-brief/