Abstract
Black men who have sex with men (MSM) in the United States are disproportionately impacted by HIV. To better understand this public health problem, we reviewed the literature to calculate an estimate of HIV incidence among Black MSM. We used this rate to model HIV prevalence over time within a simulated cohort, which we subsequently compared to prevalence from community-based samples. We searched all databases accessible through PubMed, and Conference on Retroviruses and Opportunistic Infections abstracts for HIV incidence estimates among Black MSM. Summary HIV incidence rates and 95 % confidence intervals (CIs) were calculated using random effects models. Using the average incidence rate, we modeled HIV prevalence within a simulated cohort of Black MSM (who were all HIV-negative at the start) from ages 18 through 40. Based on five incidence rates totaling 2898 Black MSM, the weighted mean incidence was 4.16 % per year (95 % CI 2.76–5.56). Using this annual incidence rate, our model predicted that 39.94 % of Black MSM within the simulated cohort would be HIV-positive by age 30, and 60.73 % by 40. Projections were similar to HIV prevalence found in community-based samples of Black MSM. High HIV prevalence will persist across the life-course among Black MSM, unless effective prevention and treatment efforts are increased to substantially reduce HIV transmission among this underserved and marginalized population.
Keywords: HIV/AIDS, Black MSM, Epidemiology, Prevention, HIV incidence, HIV prevalence
Introduction
Black men who have sex with men (MSM) are estimated to comprise less than 1 % of the United States (US) population, but represent between 20 and 25 % of all new HIV infections nationally [1] Compared to other HIV-positive MSM, HIV-positive Black MSM are more likely to be unaware of their infection, experience lower rates of HIV care linkage and retention after diagnosis, are less likely to adhere to antiretroviral (ART) therapy, and less likely to attain viral suppression [2] In addition to individual clinical benefits, successful movement through the HIV care continuum limits new infections, as ART efficaciously inhibits HIV transmission (i.e., treatment as prevention) [3, 4]. HIV incidence among Black MSM, therefore, is a metric not only for how effective prevention efforts are operating for HIV-negative Black MSM, but also how successful public health and health care systems are serving HIV-positive Black MSM as they navigate the HIV care continuum.
A prior review of HIV incidence rates among MSM of all races and ethnicities living in the US yielded an annualized mean incidence of 2.39 % [5]. The authors calculated that this incidence rate would yield HIV prevalence of approximately 40 % in a cohort of MSM by the age of 40. However, this projection underestimates the burden of HIV infection among Black MSM. The plurality of HIV diagnoses among MSM in 2011 were among Black men (39 %) [1], and new infections continue to rise among young (i.e., aged 13–24 years) Black MSM [6] Forecasting future prevalence from available HIV incidence rates among Black MSM may prove useful in illustrating the HIV epidemic among Black MSM.
Producing samples from which to draw HIV incidence rates representative of Black MSM populations remains challenging. Though several community-based samples exist, their generalizability is limited by study-specific characteristics such as sampling method, location, and time. To mitigate limitations of any one incidence rate, we aim to systematically search the literature for studies that report unique incidence estimates of HIV infection among Black MSM. From this literature we employ meta-analytic methods to calculate an overall estimate of HIV incidence, which we then use to model HIV prevalence over time within a simulated cohort of Black MSM from age 18–40. We compare this projection to current HIV prevalence to examine how well the model describes current epidemio-logic dynamics among Black MSM. Our cohort starts at 18 as it is the youngest age at which we facilitate comparison of HIV prevalence among large samples of Black MSM, and concludes at 40 because the extant HIV incidence literature largely focuses on men until this age. Lastly, recommendations for intervention, research, and policy strategies are provided and placed in the context of the current and possible future of the HIV epidemic among Black MSM in the US.
Methods
To meet the objectives of the current paper, we engaged in the following steps: (1) conducted a systematic review of the available data on HIV incidence among Black MSM; (2) generated the weighted mean HIV incidence; (3) modeled HIV prevalence over time using the weighted mean; and (4) compared modeled HIV prevalence with observed HIV prevalence data among Black MSM.
Systematic Review of HIV Incidence
Three co-authors conducted independent searches and extractions of the peer-reviewed literature that reported HIV incidence among Black MSM in the US. Searches were conducted among all databases accessible through PubMed. We used combinations of the following terms: “Black” OR “African American;” “MSM” OR “men who have sex with men” OR “gay” OR “bisexual;” HIV; “incidence” OR “seroincidence;” “annual” OR “yearly” OR “rate” OR “person year” or “person-year.” We also checked reference lists of manuscripts that provided HIV incidence estimates among Black MSM for additional publications. We contacted authors of manuscripts that reported incidence estimates among Black MSM for any necessary additional information (e.g., number of incident cases) if they were not included in the original publication. We employed the same search strategy for peer-reviewed abstracts from the most recent (2014) Conference on Retroviruses and Opportunistic Infections, recognizing the high likelihood of this research to appear in future peer-reviewed literature. We concluded our search on January 22, 2015.
We considered studies eligible for inclusion if they reported an estimate of HIV incidence among Black MSM between the ages of 18 and 40 in US. Several studies featured separate analyses from the same data source (e.g., HPTN 061), in which case only the parent manuscript presenting incidence for the entire sample was prioritized to the exclusion of others. We utilized manuscript author definition of Black MSM. A majority of studies defined Black as non-Hispanic Black or non-Hispanic African American, though others were inclusive of Caribbean Black or multiethnic Black as well. We allowed the term “MSM” to be inclusive of any same-sex sexual behavior between men regardless of sexual identity. All study publication dates were eligible for inclusion.
We excluded studies that presented incidence rates based on approximations rather than observed data, including surveillance systems. Because the total number of Black MSM at risk for HIV infection is estimated rather than measured in these studies, they could not be appropriately weighted in a summary estimate. This is why organizations such as the Centers for Disease Control and Prevention routinely release HIV incidence rates for demographic groups that can be enumerated with Census data (e.g., sex, race, age) but not transmission category (e.g., MSM, injection drug use) [6]. We note the high HIV prevalence among transgender populations, however, we also exclude any transgender-specific incidence estimates from analysis to yield a consistent definition of Black MSM across studies. Studies that did not contain any data from 1996 onwards (the introduction of highly active antiretroviral therapy) were also excluded. We did not impose exclusion criteria on how new infections were assessed.
Analysis of Weighted Mean HIV Incidence
Summary HIV incidence rates and 95 % confidence intervals (CI) were calculated with Comprehensive Meta-Analysis software (Biostat, Inc., Englewood, NJ). We assigned weights to each rate that represented the inverse of that sample's variance, plus an estimate of the variance between samples. To account for heterogeneity among samples, we calculated I-squared statistics and conducted a random effects computational model that does not assume equality of variance [7]. Because young (≤30 years of age) Black MSM have experienced a marked increase in new infections [6], we also calculated a separate summary incidence rate for this subgroup of Black MSM.
Analysis of Modeled HIV Prevalence
Using the average incidence rate, we projected HIV prevalence over time within a simulated cohort of Black MSM from age 18–40. We defined the cohort with 0 % HIV infection at age 18, whose size does not change over time, but is capable of engaging in sexual behavior with the universe of sexually active persons in the US. We also assumed that incidence was constant until age 40, no disease remission, and that HIV-specific and general mortality was negligible. The formula used to model prevalence then reduces to Pn+1 = Pn + I(1 – Pn), where I is our constant incidence rate, Pn is prevalence at age n, and Pn+1 the prevalence at age n + 1. These assumptions err on the side of presenting a conservative projection over time. For additional information about this modeling strategy see Stall et al. [5].
HIV Prevalence Model Compared with Current HIV Prevalence Among Black MSM
To contextualize model projections, we present existing HIV prevalence data among Black MSM, stratified by age, from two separate large data sources. The first is the 2008 National HIV Behavioral Surveillance System (NHBS). The second is from the first year (2014) of Promoting Our Worth, Equality, and Resilience (POWER), an ongoing study of Black MSM attending Black Pride events.
NHBS Sample
At current, the largest reported age-stratified sample of HIV prevalence among Black MSM is from the second MSM-specific cycle of data collection of the NHBS collected in 2008 [8] MSM were recruited across 21 cities using time–space sampling methods from a randomly selected subset of venues enumerated with formative research. Upon agreeing to participate in the NHBS, MSM complete an anonymous behavioral questionnaire and HIV testing. More detailed methods of the NHBS are published elsewhere [9]. At time of manuscript preparation, the third MSM-specific NHBS cycle for 2011 had been completed, though age-stratified HIV prevalence among Black MSM had not yet been published.
POWER Sample
We also present age-stratified prevalence estimates from POWER, an ongoing multi-site community-based sample of Black MSM collected in 2014 at Black Pride events in Atlanta, GA; Detroit, MI, Houston, TX, Philadelphia, PA, and Washington, DC. Similar to NHBS, this study employed random time-location sampling to maximize representativeness of Black MSM attending Black Pride events, and data were weighted for sampling design [10]. Study participants were offered free and confidential HIV testing, the results of which were linked to an anonymous questionnaire via a unique study identifier. Participants opting out of confidential HIV testing were offered the option to anonymously provide antibody samples assessing their HIV status via OraQuick ADVANCE rapid HIV-1/2 oral fluid antibody testing (OraSure Technologies, Inc., Bethlehem, PA). All HIV testing was incentivized with $10, as was the initial questionnaire. This analysis excludes Black MSM who did not opt for HIV testing, unless they self-identified in the anonymous survey as HIV-positive. This study was approved by the [redacted for blind review] Institutional Review Board.
Results
Search Results
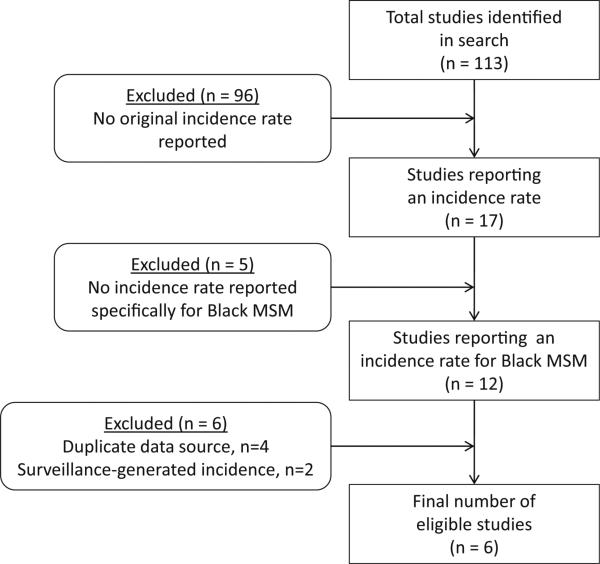
Our search yielded 113 studies. The process of study identification is depicted in Fig. 1. Studies that provided incidence estimates for Black MSM and their relevant characteristics are provided in Table 1. Though they met initial inclusion criteria, we excluded two estimates from our summary incidence calculation. The first was excluded because the sample was drawn exclusively from men attending a sexually transmitted disease clinic and so presents an inflated likelihood of HIV infection due to selection bias [11]. The second was excluded because we were unable to extract information about the number of incident cases or total person-years necessary for weighting the reported 14.7 % annual incidence rate [12]. In the event an incidence rate was inclusive of Black MSM younger than 18 or older than 40 it was included, provided the mean age was still between 18 and 40. We present estimates used to calculate summary incidence by time of data collection (Fig. 2).
Fig. 1.
Identification and selection of studies
Table 1.
Identified studies of HIV incidence among Black MSM
| Source | Study date | Location | Study design | Recruitment and sampling method | Age | N | Incident infection measurement | HIV incidence estimate per 100 PY (95 % CI) |
|---|---|---|---|---|---|---|---|---|
| Balaji et al. [40] | 2008 | Atlanta, GA; Baltimore, MD; Boston, MA; Chicago, IL; Dallas, TX; Denver, CO; Detroit, MI; Houston, TX; Los Angeles, CA; Miami, FL; Nassau, NY; New Orleans, LA; New York, NY; Newark, NJ; Philadelphia, PA; San Diego, CA; San Francisco, CA; San Juan, PR; Saint Louis, MO; Seattle, WA; Washington, DC | Cross-sectional | Random sampling of eligible venues and day-time periods; systematic sampling of MSM at events | 18–24 | 678 | EIA + date of first HIV-positive test | 5.1 (NR) |
| Buchbinder et al. [41] | April 1995–May 1997 | Boston, MA; Chicago, IL; Denver, CO; New York, NY; San Francisco, CA; Seattle, WA | Prospective cohort | Non-random recruitment from STD clinics, bars and clubs, street outreach, advertising, prior cohort studies, and participant referral | ≥18 | 209 | ELISA to establish baseline HIV-negative; EIA + Western blot to establish HIV-positive | 2.1 (0.59–5.52) |
| CDC [1] | 1994–1998 | Baltimore, MD; Dallas, TX; Los Angeles, CA; Miami, FL; New York, NY; San Francisco, CA; Seattle, WA | Cross-sectional | Random sampling of eligible venues and day-time periods | 15–22 | 587 | STARHS | 4.0 (1.3–9.9) |
| CDC [1] | 1998–2000 | Baltimore, MD; Dallas, TX; Los Angeles, CA; Miami, FL; New York, NY; Seattle, WA | Cross-sectional | Random sampling of eligible venues and day-time periods | 23–29 | 497 | STARHS | 14.7 (7.9–27.1) |
| Koblin et al. [16] | July 2009–October 2010 | Atlanta, GA; Boston, MA; Los Angeles, CA; New York, NY; San Francisco, CA; Washington, DC | Prospective cohort | Non-random recruitment directly from community, or referred via sexual networks of index participants | ≥18 | 1164 | Negative rapid test or Western blot to establish baseline HIV-negative; reactive rapid + Western blot to establish HIV-positive | 3.0 (2.0–4.4) |
| 18–30 (subgroup analysis) | 441 | 5.9 (3.6–9.1) | ||||||
| Pathela et al. [11] | January 2008–March 2010 | New York, NY | Retrospective cohort | Census of MSM from STD clinics with diagnosed rectal Chlamydia or gonorrhea infection, and who reported receptive anal intercourse in past 3 months | <20 to ≥40 | 51 | Negative rapid test confirmed with NAAT to establish baseline HIV-negative; match to HIV surveillance registry to establish HIV-positive | 15.34 (8.31–26.08) |
| Pathela et al. [11] | January 2008–March 2010 | New York, NY | Matched retrospective cohort | Cohort matching (see above), but with no diagnosed rectal Chlamydia or gonorrhea infection | <20 to ≥40 | 51 | See above | 6.48 (2.37–14.36) |
| Rosenberg et al. [26] | 2009–2014 | Atlanta, GA | Prospective cohort | Recruitment at sample of enumerated venue-day-time periods, non-random recruitment on Facebook | 18–39 | 260 | Negative rapid test to establish HIV-negative at baseline; Reactive rapid test + confirmatory Western blot to establish HIV-positive | 6.6 (4.3–9.9) |
| 18–24 (subgroup analysis) | 130 | 12.1 (6.9–19.6) |
EIA enzyme immunoassay, ELISA enzyme linked immunosorbent assay, NAAT nucleic acid amplification test, NR not reported, STARHS serologic testing algorithm for recent HIV conversion
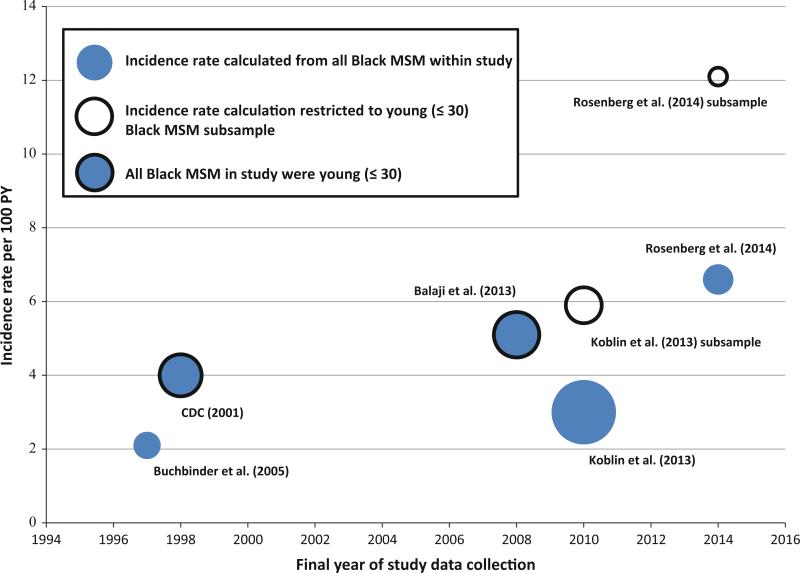
Fig. 2.
Estimates of HIV incidence of Black MSM over time, weighted by sample size
Based on five incidence rates totaling 2898 Black MSM, the weighted mean incidence was calculated to be 4.16 % per year (95 % CI 2.76–5.56). For Black MSM ≤30 years of age, four studies totaling 2045 Black MSM yielded a weighted mean incidence of 6.73 % per year (95 % CI 5.10–8.37).
Estimated Incidence Rates for Black MSM Over Time
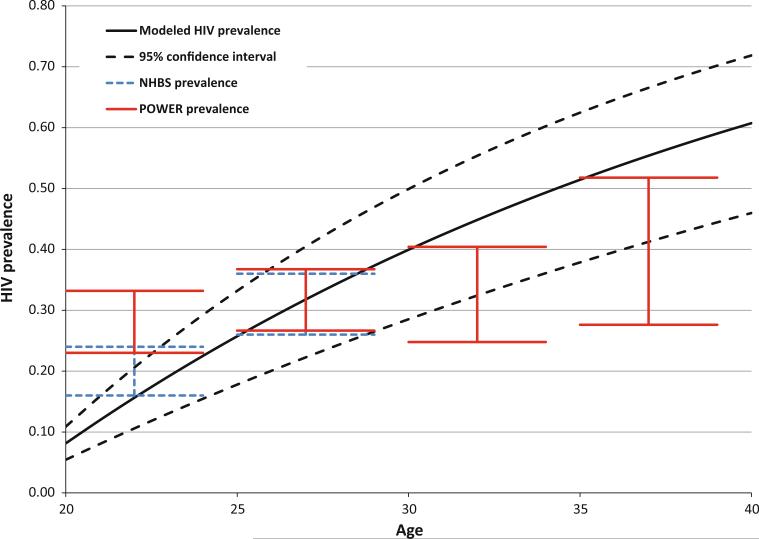
Substituting the average incidence of 4.16 % per year into the model of HIV prevalence over time results in a prediction of 8.15 % (95 % CI 5.44–10.89). of Black MSM within our simulated cohort living with HIV by age 20, 25.72 % (95 % CI 17.79–33.20) by 25, 39.94 % (95 % CI 28.52–49.92) by 30, 51.43 % (95 % CI 37.86–62.46) by 35, and 60.73 % (95 % CI 45.98–71.86) by 40 as shown in Fig. 3.
Fig. 3.
Existing HIV prevalence estimates among Black MSM by age, and projection based on annualized HIV incidence rate of 4.16 %
Comparison of Projected and Observed HIV Prevalence Among Black MSM
The 2008 NHBS data reported HIV prevalence of 8.81 % for 18- and 19-year old Black MSM, with prevalence increasing to 19.71 % among Black MSM 20–24, and 30.35 % among Black MSM 25–29 [8]. POWER contains HIV testing data on 83.7 % of Black MSM respondents; of the 1563 Black MSM respondents, 1303 consented to receive an HIV test and/or reported living with HIV in the questionnaire. This yielded a weighted HIV prevalence of 14.0 % among Black MSM 18–19 years old, with prevalence increasing to 28.7 % for those 20–24 years old, 31.9 % among 25–29 year olds, 33.2 % among 30–34 year olds, 41.3 % among 35–39 year olds, and 51.4 % for Black MSM ≥40. We contrast 2008 NHBS and POWER study sample characteristics in Table 2. Figure 3 illustrates the projected HIV prevalence among the simulated cohort by age, with age-stratified prevalence from the NHBS and POWER samples.
Table 2.
Characteristics of Black MSM in the National HIV Behavioral Surveillance (NHBS) and Promoting Our Worth, Equality, and Resilience (POWER) samples
| NHBS | POWER | |
|---|---|---|
| Study period | June–December 2008 | April–September 2014 |
| Number of Black MSM with HIV status data | 1,895 | 1286 |
| Sample HIV prevalencea | 539/1895 (28.44 %) | 492/1286 (38.26 %) |
| Sampling method | Random time–space sampling | Random time–space sampling |
| Location | Atlanta, GA; Baltimore, MD; Boston, MA; Chicago, IL; Dallas, TX; Denver, CO; Detroit, MI; Houston, TX; Los Angeles, CA; Miami, FL; Nassau, NY; New Orleans, LA; New York, NY; Newark, NJ; Philadelphia, PA; San Diego, CA; San Francisco, CA; San Juan, PR; Saint Louis, MO; Seattle, WA; Washington, DC | Atlanta, GA; Detroit, MI; Houston, TX; Philadelphia, PA; Washington, DC |
Not weighted for sampling design
Discussion
By presenting an estimate of current HIV incidence rates among Black MSM in the US, and its associated implications, we hope to draw renewed attention to an epidemic among a population that has long borne a disproportionate burden of new HIV infections. Stall et al. noted that a 2.39 % incidence rate would lead to an HIV prevalence of 40 % by age 40 among gay men in the US, a situation they characterized as “running in place” [5]. Black MSM have an incidence rate almost twice that, with an even faster pace of new infections occurring among young Black MSM [6]. If Black MSM in the US formed a country today, it would have the highest HIV prevalence on the globe [13, 14]. Characterizing the outcomes of HIV prevention among Black MSM forces us to conclude that if it is going anywhere, it is running backwards. Our model projections are already within the limits of current HIV prevalence estimates; this is not an epidemic that could happen, but rather is happening. This endeavor is meant neither to stigmatize nor dishearten, but rather to serve as a call to action: we will not end the HIV epidemic in this country without a powerful and effective response to the HIV epidemic among Black MSM.
Despite the notable strengths of our approach, our analysis has several limitations. The first being that any summary estimate is only as meaningful as the quality of individual studies that comprise it. The few published incidence rates for Black MSM are primarily from samples of MSM in large cities and metropolitan areas. The omission of areas where Black MSM have relatively lower prevalence but high incidence (e.g., the South) [15] would suggest that published incidence rates—and by extension model projections—may fail to capture important regional variations [16]. Though incidence rates are higher among young Black MSM we assumed a uniform incidence and 0 % prevalence at age 18 to facilitate a conservative model. The model we used to project prevalence was intentionally simplistic and did not take into account variables known to influence infection and transmission rates (e.g., behavioral change after diagnosis [17], treatment as prevention [4], serosorting [18], network characteristics [19]), though to some extent these dynamics are reflected in the incidence estimates themselves. Also, our average incidence estimate only includes those studies we were able to identify in the peer-reviewed literature and as such suffers from the same limitations inherent in all systematic reviews [20]. In acknowledgement of these limitations, we used a random effects model to generate the summary incidence rate. Though resulting in a wider confidence interval it appropriately reflects the uncertainty inherent in using observed incidence rates, which reflect a complex 30 year history of the epidemic, to predict prevalence in a qualitatively different future. We provided two separate sources of age-stratified HIV prevalence among Black MSM that support our model projection, though we acknowledge these prevalence data may underestimate existing infections, as they are from samples that underrepresent Black MSM with high HIV-related morbidity, and exclude those who experienced premature mortality.
The challenge before us lies in developing strategies that render our projections inaccurate. A cornerstone of the National HIV/AIDS Strategy is to proportionately allocate resources to communities according to epidemiologic need [21]. Yet an analysis by The Fenway Institute found that HIV prevention, risk reduction, and research funding for MSM, and Black MSM in particular, is disproportionately low [22]. Addressing the current epidemic requires at the very least a commensurate increase in resources for research and interventions targeting Black MSM. The high rate of new infections among Black MSM requires greater monitoring and faster reporting systems, as data can too quickly become inaccurate to inform timely public health interventions. With respect to intervention and policy, one of the most efficient methods to prevent additional infection is to focus on transmission. There will always be a role for primary prevention—individual behavior remains a proximal determinant of infection, and a recent modeling study has shown how a combination of condom use and pre-exposure prophylaxis (PrEP) could dampen current HIV incidence rates among Black MSM [23]. However, the lack of difference in sexual risk behaviors between Black MSM and other MSM [2], suggest interventions that focus on individual sexual behavior will have a limited impact in reducing disparities. Strategies that focus on navigating HIV-positive Black MSM through the care continuum to achieve viral suppression represent an ideal use of scarce public health resources. In addition to the large potential public health benefit, HIV-positive individuals experience a substantial direct health benefit from early diagnosis and viral suppression [24].
Hall et al. estimate that 38,920 additional HIV-positive Black MSM need to be on treatment just to raise viral suppression to 56 %, the same level experienced by White MSM aware of their infection [25]. Yet even this number is a far cry of what will be required to end the epidemic. For if we were to equalize the HIV care continuum between Black and White MSM today, it would only reduce incidence by 27 %, as excess incident infections would remain simply due to current disparities in HIV prevalence [26]. Ending disparities in new HIV infections is an important step to ending the HIV epidemic, but they cannot be confused as synonymous goals.
An assortment of effective and diverse policy actions that are capable of influence on a wide-scale over the long-term is necessary to lower the number of new HIV infections. Prioritizing access to treatment for all HIV-positive individuals is one immediate first step, as HIV-positive Black MSM are only about half as likely to have health insurance as other HIV-positive MSM [2]. The provision of Emergency Relief Funds, which effectively eliminated AIDS Drug Assistance Program waiting lists across the country in 2013, remains an instructive example of how targeted resource allocation can have a profound impact [27]. Though the Affordable Care Act will reduce disparities in access [28], Black MSM still experience significant barriers to care linkage, retention, and ART adherence [2]. A recent review found low availability of culturally competent services, and limited availability of HIV testing and prevention services in the communities where Black MSM live [29]. Even when services are available, stigma remains a powerful deterrent to their use [30]. Policies can remove structural sources of stigma; the Department of Justice has recently called for states to modify ineffective laws that criminalize HIV non-disclosure, invoking the National HIV/AIDS Strategy and scientific knowledge as an impetus for this change [31]. Finally, improving the health of Black MSM will require not only addressing sociocultural factors that facilitate HIV infection (e.g., homophobia, stigma, racism) [30], but also recognizing that HIV infection is but one of many health outcomes born of structural inequalities that adversely affect the lives of Black men.
Research, intervention, and policy must work in concert to identify and modify contextual factors that pattern HIV infection and lower care utilization. To that end, public health must be mindful to engage, not simply target, communities of Black MSM at every opportunity. Understanding strategies that HIV-negative and HIV-positive Black MSM employ to remain healthy and thrive are poised to inform initiatives that have the greatest chance at making a positive impact because they originate from these communities [32]. PrEP is a contemporary example about the need for this engagement. Despite the potentially large benefit from PrEP use [23], we know incredibly little about the awareness, access, and utilization of PrEP among Black MSM, though preliminary research suggests they are low [33, 34]. Establishing meaningful community relationships is crucial to ensure Black MSM have the ability to weigh their options, decide what is most appropriate, and execute a personalized prevention portfolio. Yet absent changes in public health infrastructure simply launching awareness campaigns will have little effect. Stigma and medical mistrust limit the engagement of Black MSM with health care (including HIV care for Black MSM with diagnosed HIV infection) and will continue to serve as a barrier to not just PrEP use, but more general preventive health care services necessary for Black MSM to remain healthy [35].
Highlighting the specific needs of young Black MSM warrants special attention. Though working with youth requires specific consideration to a variety of factors salient to these populations [36], it remains necessary to better understand and reach these young Black MSM, as many are already diagnosed with HIV before 18 years of age [6, 8]. Though the amount of formally evaluated engagement with young Black MSM remains limited, efforts such as the HRSA-funded Special Projects of National Significance Young MSM of Color Initiative prove not only feasibility of such efforts but their value [37, 38].
Despite the alarming projections found in this paper, we caution against falling prey to a defeatist paradigm. Short of an effective vaccine or cure, there will not be one silver bullet that halts new infections and ensures those living with HIV receive the care they need. But to start running forward in addressing the HIV epidemic among Black MSM, we as a country must summon both the energy and investment to make up for the missed opportunities of the past. We have a greater diversity of prevention and treatment options than at any point during the history of the HIV epidemic, but their potential will not be realized until interventions and policies sufficiently reduce the gap between efficacy in the laboratory and effectiveness in communities.
The US has made an impressive commitment to ending the HIV epidemic around the world, and in several regards has made laudable progress towards that goal [39]. Just as the US has devoted resources beyond our borders, it must similarly act to end an epidemic which exceeds in magnitude that of many countries in the developing world. Invoking that spirit, we challenge the US to rise to the occasion and meet the needs of Black MSM, currently in the throes of a growing epidemic. Creating an AIDS-free generation requires no less than the commitment and urgency owed to current and future generations of Black MSM living in the US.
Acknowledgments
This study was partially supported by the National Institute for Nursing Research (R01NR013865), the National Institute for Mental Health (T32MH094174; R01MH094230), and the National Institute on Drug Abuse (F31DA037647). We thank Dr. Eli Rosenberg for his comments on an earlier version of this draft, the Center for Black Equity for partnering with us to implement POWER, and the hundreds of study participants who volunteered their time to contribute to this research. This article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix
The members of POWER study team are as follows:
Center for Black Equity: Earl D. Fowlkes, Jr., Michael S. Hinson, Jr.
Columbia University: Alexander J. Martos, Patrick A. Wilson
University of Connecticut: Robert Baldwin, Christopher Conway-Washington, Daniel D. Driffin, Lisa A. Eaton, Harlan Smith
University of Pittsburgh: Patrick Buehler, Leigh Bukowski, Amy L. Herrick, Christopher Hoffmann, Derrick D. Matthews, Marcus A. Poindexter, Noah Riley, Ron D. Stall, Orrin Tiberi, Mudia Uzzi
Footnotes
Parts of these data were previously presented at the National AIDS & Education Service for Minorities (NAESM) Annual MSM Leadership Conference on January 16, in Atlanta, GA.
The members of the Promoting Our Worth, Equality, and Resilience (POWER) study team are listed in Appendix.
References
- 1.Centers for Disease Control and Prevention HIV among African American gay and bisexual men. 2014 http://www.cdc.gov/hiv/risk/racialethnic/bmsm/facts/
- 2.Millett GA, Peterson JL, Flores SA, Hart TA, Wilson PA, Rourke SB, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 3.Department of Health and Human Services HIV/AIDS care continuum. 2013 http://aids.gov/federal-resources/policies/care-continuum.
- 4.Rodger A, Bruun T, Cambiano V, Vernazza P, Estrada V, Lunzen JV, et al. HIV Transmission risk through condomless sex if HIV + partner on suppressive ART: PARTNER Study.. Conference on Retroviruses and Opportunistic Infections; Boston. 2014. [Google Scholar]
- 5.Stall R, Duran L, Wisniewski SR, Friedman MS, Marshal MP, McFarland W, et al. Running in place: implications of HIV incidence estimates among urban men who have sex with men in the United States and other industrialized countries. AIDS Behav. 2009;13(4):615–29. doi: 10.1007/s10461-008-9509-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to meta-analysis. Wiley; Chichester: 2011. [Google Scholar]
- 8.Centers for Disease Control and Prevention Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–7. [PubMed] [Google Scholar]
- 9.Finlayson TJ, Le B, Smith A, Bowles K, Cribbin M, Miles I, et al. HIV risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance System, 21 U.S. Cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2011;60(SS14):1–34. [PubMed] [Google Scholar]
- 10.Kalton G. Sampling considerations in research on HIV risk and illness. In: Ostrow D, Kessler R, editors. Methodological issues in AIDS behavioral research. Plenum; New York: 1993. pp. 53–74. [Google Scholar]
- 11.Pathela P, Braunstein SL, Blank S, Schillinger JA. HIV incidence among men with and without sexually transmitted rectal infections: estimates from matching against an HIV case registry. Clin Infect Dis. 2013;57(8):1203–9. doi: 10.1093/cid/cit437. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention HIV incidence among young men who have sex with men–seven US cities, 1994-2000. MMWR Morb Mortal Wkly Rep. 2001;50(21):440–4. [PubMed] [Google Scholar]
- 13.Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J. HIV infection and awareness among men who have sex with men–20 Cities, United States, 2008 and 2011. PLoS ONE. 2013;8(10):e76878. doi: 10.1371/journal.pone.0076878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization Data on the size of the HIV/AIDS epidemic: Prevalence of HIV among adults aged 15 to 49. Data by country. 2013 http://apps.who.int/gho/data/node.main.562?lang=en.
- 15.Hightow LB, MacDonald PD, Pilcher CD, Kaplan AH, Foust E, Nguyen TQ, et al. The unexpected movement of the HIV epidemic in the Southeastern United States: transmission among college students. J Acquir Immune Defic Syndr. 2005;38(5):531–7. doi: 10.1097/01.qai.0000155037.10628.cb. [DOI] [PubMed] [Google Scholar]
- 16.Koblin BA, Mayer KH, Eshleman SH, Wang L, Mannheimer S, del Rio C, et al. Correlates of HIV acquisition in a cohort of Black men who have sex with men in the United States: HIV prevention trials network (HPTN) 061. PLoS ONE. 2013;8(7):e70413. doi: 10.1371/journal.pone.0070413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Defic Syndr. 2005;39(4):446–53. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- 18.Marks G, Millett GA, Bingham T, Lauby J, Murrill CS, Stueve A. Prevalence and protective value of serosorting and strategic positioning among Black and Latino men who have sex with men. Sex Transm Dis. 2010;37(5):325–7. doi: 10.1097/OLQ.0b013e3181c95dac. [DOI] [PubMed] [Google Scholar]
- 19.Mustanski B, Birkett M, Kuhns LM, Latkin CA, Muth SQ. The role of geographic and network factors in racial disparities in HIV among young men who have sex with men: an egocentric network study. AIDS Behav. 2014;19(6):1037–47. doi: 10.1007/s10461-014-0955-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull. 1979;86(3):638–41. [Google Scholar]
- 21.White House Office of National AIDS Policy. National HIV/AIDS strategy for the United States; Washington, D.C.: 2010. [Google Scholar]
- 22.The Fenway Institute. More HIV prevention funding should be shifted to gay men, Fenway says. 2013 http://www.fenway health.org/site/News2?page=NewsArticle&id=8675.
- 23.Smith DK, Herbst JH, Rose CE. Estimating HIV protective effects of method adherence with combinations of preexposure prophylaxis and condom use among African American men who have sex with men. Sex Transm Dis. 2015;42(2):88–92. doi: 10.1097/OLQ.0000000000000238. [DOI] [PubMed] [Google Scholar]
- 24.May MT, Gompels M, Delpech V, Porter K, Orkin C, Kegg S, et al. Impact on life expectancy of HIV-1 positive individuals of CD4 ? cell count and viral load response to antiretroviral therapy. AIDS. 2014;28(8):1193–202. doi: 10.1097/QAD.0000000000000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall HI, Holtgrave DR, Tang T, Rhodes P. HIV transmission in the United States: considerations of viral load, risk behavior, and health disparities. AIDS Behav. 2013;17(5):1632–6. doi: 10.1007/s10461-013-0426-z. [DOI] [PubMed] [Google Scholar]
- 26.Rosenberg E, Millett G, Sullivan P, Del Rio C, Curran J. Understanding the HIV disparities between black and white men who have sex with men in the USA using the HIV care continuum: a modelling study. Lancet HIV. 2014;1(3):e112–8. doi: 10.1016/S2352-3018(14)00011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Alliance of State & Territorial AIDS Directors . ADAP alert: after five years, adap waiting lists have been eliminated; unmet need and funding uncertainties require continued commitment. Washington, DC.: 2013. http://nastad.org/docs/adap_watch/ADAP-Alert-11-25-13.html. [Google Scholar]
- 28.Gallup U.S., uninsured rate lowest since 2008: uninsured rate declines most among blacks and lower-income Americans. 2014 http://www.gallup.com/poll/168248/uninsured-rate-lowest-2008.aspx.
- 29.Levy ME, Wilton L, Phillips GII, Glick SN, Kuo I, Brewer RA, et al. Understanding structural barriers to accessing HIV testing and prevention services among black men who have sex with men (BMSM) in the United States. AIDS Behav. 2014;18(5):972–96. doi: 10.1007/s10461-014-0719-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arnold EA, Rebchook GM, Kegeles SM. ‘Triply cursed’: racism, homophobia and HIV-related stigma are barriers to regular HIV testing, treatment adherence and disclosure among young Black gay men. Cult Health Sex. 2014;16(6):710–22. doi: 10.1080/13691058.2014.905706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Department of Justice . Best practices guide to reform hiv-specific criminal laws to align with scientifically-supported factors. Washington, D.C.: 2014. [Google Scholar]
- 32.Herrick AL, Lim SH, Wei C, Smith H, Guadamuz T, Friedman MS, et al. Resilience as an untapped resource in behavioral intervention design for gay men. AIDS Behav. 2011;15(Suppl 1):S25–9. doi: 10.1007/s10461-011-9895-0. [DOI] [PubMed] [Google Scholar]
- 33.Smith DK, Toledo L, Smith DJ, Adams MA, Rothenberg R. Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PrEP). AIDS Educ Prev. 2012;24(5):408–21. doi: 10.1521/aeap.2012.24.5.408. [DOI] [PubMed] [Google Scholar]
- 34.Cohen S, Vittinghoff E, Anderson P, Doblecki-Lewis S, Bacon O, Chege W, et al., editors. Implementation of PrEPin STD and community health clinics in the US: high uptake and drug concentrations among MSM in the demo project.. 9th international conference on HIV treatment and prevention; Miami. 2014. [Google Scholar]
- 35.Eaton LA, Driffin DD, Kegler C, Smith H, Conway-Washington C, White D, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health. 2015;105(2):e75–82. doi: 10.2105/AJPH.2014.302322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harper GW. Sex isn't that simple: culture and context in HIV prevention interventions for gay and bisexual male adolescents. Am Psychol. 2007;62(8):806–19. doi: 10.1037/0003-066X.62.8.806. [DOI] [PubMed] [Google Scholar]
- 37.Hightow-Weidman LB, Jones K, Wohl AR, Futterman D, Outlaw A, Phillips G, et al. Early linkage and retention in care: findings from the outreach, linkage, and retention in care initiative among young men of color who have sex with men. AIDS Patient Care STDS. 2011;25(S1):S31–8. doi: 10.1089/apc.2011.9878. [DOI] [PubMed] [Google Scholar]
- 38.Magnus M, Jones K, Phillips G, Binson D, Hightow-Weidman LB, Richards-Clarke C, et al. Characteristics associated with retention among African American and Latino adolescent HIV-positive men: results from the outreach, care, and prevention to engage HIV-seropositive young MSM of color special project of national significance initiative. J Acquir Immune Defic Syndr. 2010;53(4):529–36. doi: 10.1097/QAI.0b013e3181b56404. [DOI] [PubMed] [Google Scholar]
- 39.Department of State . PEPFAR Blueprint: Creating an AIDS-free Generation. Washington, D.C.: 2012. [Google Scholar]
- 40.Balaji AB, Bowles KE, Le BC, Paz-Bailey G, Oster AM, Group NS. High HIV incidence and prevalence and associated factors among young MSM, 2008. AIDS. 2013;27(2):269–78. doi: 10.1097/QAD.0b013e32835ad489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Buchbinder SP, Vittinghoff E, Heagerty PJ, et al. Sexual risk, nitrite inhalant use, and lack of circumcision associated with HIV seroconversion in men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2005;39(1):82–9. doi: 10.1097/01.qai.0000134740.41585.f4. [DOI] [PubMed] [Google Scholar]