Abstract
Objectives
To determine the diagnostic performance of transrectal ultrasound in virgin patients with polycystic ovary syndrome (PCOS) by receiver operating characteristic (ROC) curve analysis, compared with conventional transvaginal ultrasound assessment.
Methods
Ultrasound examinations were performed in 963 Korean women, with transvaginal transducers in 677 women and transrectal transducers in 286 women at Ewha Womans University Mokdong Hospital. Transvaginal ultrasound examinations were performed in 494 normal control women and 183 PCOS patients according to National Institutes of Health (NIH) PCOS diagnostic criteria. In virgin patients, transrectal ultrasound examinations were performed in 141 normal control women and 145 PCOS patients. ROC curves were calculated for ovarian volume and follicle number.
Results
By transvaginal ultrasound examination, the ovarian volume showed an area under the ROC curve (AURC) of 0.838. An ovarian volume decision threshold > 7 cm3 had a sensitivity of 73.0% and a specificity of 84.2% for the diagnosis of PCOS. The follicle number showed an AURC of 0.886. A follicle number decision threshold ≥ 9 had a sensitivity of 78.6% and a specificity of 87.2% for the diagnosis of PCOS. By transrectal ultrasound examination, the ovarian volume and the follicle number showed AURCs of 0.815 as same thresholds with a sensitivity of 67.2% and 66.4%, respectively and a specificity of 86.8% each. Ovarian volume and follicle number by transvaginal and transrectal ultrasound assessment had a high diagnostic power for PCOS screening.
Conclusion
Transrectal ultrasound assessment is as effective as conventional transvaginal ultrasound for the detection of PCOS in virgin patients.
Keywords: Polycystic ovary syndrome, Transrectal ultrasonography, Transvaginal ultrasonography
Introduction
Polycystic ovary syndrome (PCOS) is not a specific endocrine disorder, but a syndrome represented by a collection of signs and symptoms, and no one sign, symptom, or test is diagnostic. Establishing the criteria for diagnosis of PCOS has still proven both challenging and controversial. In 1990, the National Institutes of Health (NIH) suggested the criteria for the diagnosis of PCOS, which included hyperandrogenism or hyperandrogenemia and oligo-ovulation regardless of the sonographic finding.1 This definition was criticized due to the exclusion of sonographic findings of polycystic ovaries. In 2003, the Rotterdam Consensus Conference2 defined PCOS when at least 2 of the following 3 clinicopathologic features are present: chronic anovulation, clinical or biochemical hyperandrogenism, and polycystic ovaries on pelvic sonography. More than 12 follicles measuring 2 to 9 mm in diameter or more than 10 mL of ovarian volume is an important sonographic finding for the diagnosis of polycystic ovary.
The ultrasound is very useful diagnostic tool in gynecologic area to investigate pelvic space including uterus, ovaries and other adnexal mass and it can be used to evaluate pelvic masses whether these have malignant risk or not.3 Serum cancer antigen 125 (CA-125) is also used to discriminate ovarian tumor preoperatively.4 The route of pelvic sonography is a transvaginal, transabdominal, or transrectal approach. Transvaginal sonography (TVS) provides clear images of the region of interest, provided the targeted organ is within the focal range of the probe. There are only a few real disadvantages of TVS. Agenesis of the vagina, a virginal introitus and the fear of introducing infection are some of the more common situations in which TVS is not possible or is relatively contraindicated. Especially in Korea, conventional TVS is not acceptable to virgin patients due to fear of hymenal injury.
In such cases, transabdominal sonography (TAS) is preferred. However, in our previous study, we observed that transabdominal ultrasound assessment is not effective for the detection of PCOS in young women of reproductive age.5 Transrectal scanning could be used liberally after proper patient selection and counseling. Introducing a commercially available vaginal probe through the anal sphincter into the rectum, transrectal sonography (TRS), seems to be a reasonable alternative to image the female pelvic structures. The images obtained are superior to TAS and comparable to those obtained by TVS.6
In this study, we determined the diagnostic performance of transrectal ultrasound in virgin patients with PCOS by receiver operating characteristic (ROC) curve analysis, compared with conventional transvaginal ultrasound assessment.
Methods
1. Subjects
Nine hundred sixty-three Korean women aged between 15 and 44 years who were diagnosed with normal menstruation or PCOS were recruited from the Department of Obstetrics and Gynecology at Ewha Womans University Mokdong Hospital from December 2008 through December 2013.
PCOS was diagnosed according to the NIH criteria,1 when the following criteria were met: 1) chronic anovulation, 2) clinical hyperandrogenism or hyperandrogenemia. Chronic anovulation was defined as oligomenorrhea that was less than 10 episodes of menstruation per year, and clinical hyperandrogenism was diagnosed when the modified Ferriman Gallwey (FG) score was more than 8 points. Hyperandrogenemia referred to a situation when the serum testosterone level was more than 95th percentile of the control group that had normal menstrual cycle.
Women with normal menstruation without hyperandrogenism or polycystic ovaries on pelvic sonography were defined as the control group.
The Institutional Review Board of the Ewha Womans University Mokdong Hospital approved the study protocol, and written informed consent was obtained from all of the participants.
2. Pelvic ultrasound
Pelvic ultrasound examinations were performed with 7 MHz transvaginal or transrectal transducer (LOGIQ 500, General Electric Medical Systems, Milwaukee, WI, USA) to evaluate ovarian volume and follicle number. Ultrasound examinations were performed at the early follicular phase within 5 to 10 days of the menstrual cycle or amenorrhea for more than 3 cycles. The virgin women underwent transrectal approach to avoid hymenal injury.
Each ovary was scanned in the longitudinal cross-section from the inner to outer margins in order to count the total number of follicles which measured between 2 and 9 mm in diameter. The ovarian volume was calculated using the formula for a prolate ellipsoid (0.523 × length × width × thickness). Patients with ovarian cysts or a history of ovarian surgery were excluded from this study.
3. Statistics
Statistical analysis between the normal control group and the PCOS group was performed using IBM SPSS Statistics Version 20 (Statistical Package for Social Science Japan, Inc., Tokyo, Japan). Quantitative variables are given as mean ± standard deviation. The P value under 0.05 by Student's t-test was considered statistically significant. Area under the ROC curve (AURC) was used for determining the optimal follicle number and ovarian volume to diagnose PCOS. Using the ROC curve, sensitivity and specificity were determined, and the diagnostic power was calculated.
Results
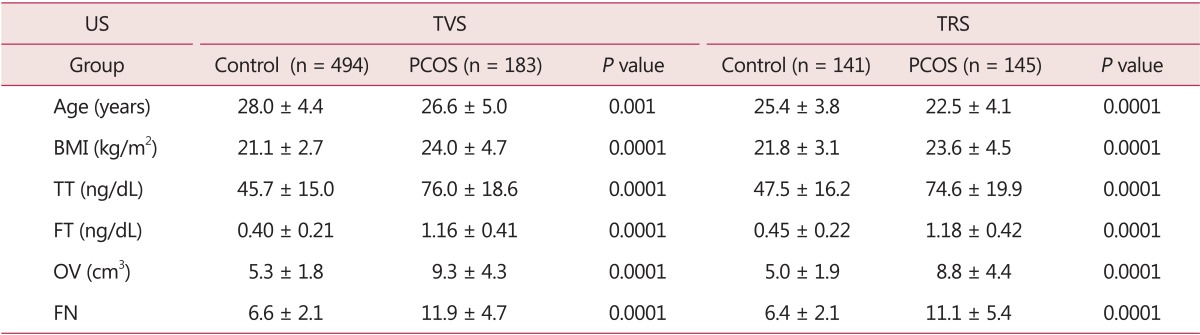
Among the 963 Korean reproductive aged women who received ultrasound examination, 677 women were examined by transvaginal ultrasound and 286 women were examined by transrectal ultrasound. We compared between the normal menstruation group and PCOS patients by NIH using the criteria. Baseline characteristics of the two groups according to the route of ultrasound are shown in Table 1.
Table 1. Baseline characteristics in controls and polycystic ovary syndrome patients according to the route of ultrasound.
US: ultrasound, TVS: transvaginal sonography, TRS: transrectal sonography, PCOS: polycystic ovary syndrome, BMI: body mass index, TT: total testosterone, FT: free testosterone, OV: ovarian volume, FN: follicle number
Among the cases that received transvaginal ultrasound examination, 494 women who had normal menstrual cycle without hyperandrogenism or polycystic ovarian morphology on sonography were the control group. The mean age of the normal control group was 28.0 ± 4.4 years, and the mean ovarian volume and follicle number were 5.3 ± 1.8 cm3 and 6.6 ± 2.1, respectively. The mean age of 183 PCOS patients who received transvaginal ultrasound was 26.6 ± 5.0 years, and the mean ovarian volume and follicle number were 9.3 ± 4.3 cm3 and 11.9 ± 4.7, erspectively.
Among the cases that received transrectal ultrasound examinations, the mean age of 141 women with normal menstruation was 25.4 ± 3.8 years and the mean ovarian volume and follicle number were 5.0 ± 1.9 cm3 and 6.4 ± 2.1, respectively. The mean age of 145 patients with PCOS was 22.5 ± 4.1 years. The mean ovarian volume and follicle number were 8.8 ± 4.4 cm3 and 11.1 ± 5.4, respectively. There were significant differences in body mass index, total testosterone, free testosterone, ovarian volume, and follicle number between normal controls and PCOS patients.
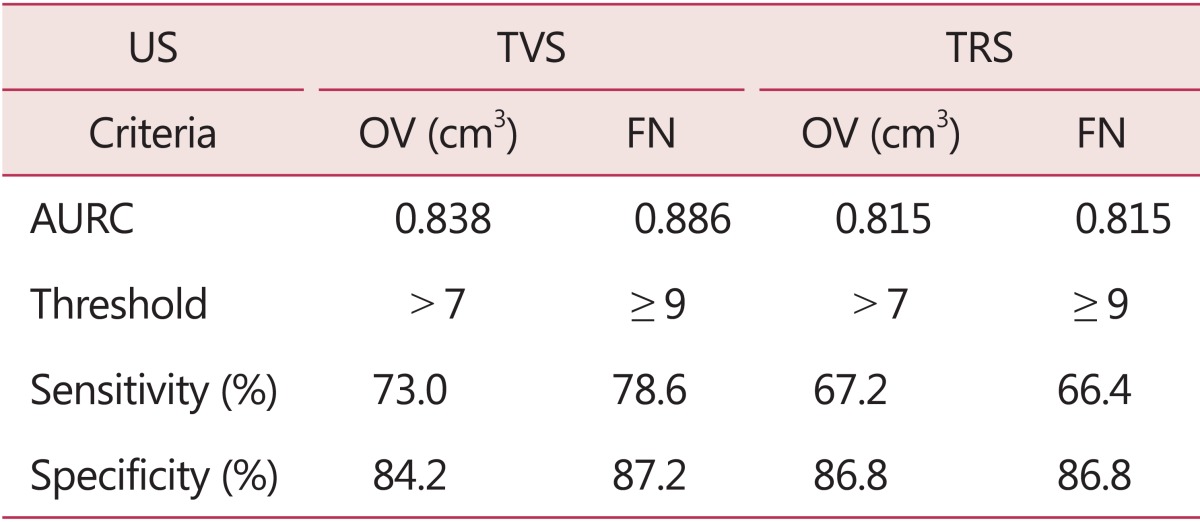
ROC curve data for PCOS detection in the two groups according to the route of ultrasound are shown in Table 2. By transvaginal ultrasound examination, the ovarian volume showed an AURC of 0.838. A ovarian volume decision threshold > 7 cm3 had a sensitivity of 73.0% and a specificity of 84.2% for the diagnosis of PCOS. The follicle number showed an AURC of 0.886. A follicle number decision threshold ≥ 9 had a sensitivity of 78.6% and a specificity of 87.2% for the diagnosis of PCOS.
Table 2. Receiver operating characteristic curve data for polycystic ovary syndrome detection by transvaginal sonography and transrectal sonography.
US: ultrasound, TVS: transvaginal sonography, TRS: transrectal sonography, OV: ovarian volume, FN: follicle number, AURC: area under the receiver operating characteristic curve
By transrectal ultrasound examination, the ovarian volume and the follicle number showed AURC of 0.815. A ovarian volume decision threshold > 7 cm3 had a sensitivity of 67.2% and a specificity of 86.8% for the diagnosis of PCOS. A follicle number decision threshold ≥ 9 had a sensitivity of 66.4% and a specificity of 86.8% for the diagnosis of PCOS. Follicle number and ovarian volume by transvaginal and transrectal ultrasound assessment had a high diagnostic power for PCOS screening.
Discussion
PCOS is one of the most common endocrine disorders in women of reproductive age, and the most frequent cause of hyperandrogenism and oligo-anovulation.7 Because PCOS patients show higher risk for cardiovascular diseases, as linked by metabolic dysfunction marked by dyslipidemia, hyperandrogenism, inflammatory state and insulin resistance,8 it is important to diagnose PCOS correctly.
Polycystic ovarian morphology on sonography is one of the diagnostic criteria, and several studies have performed this evaluation. Pache et al.9 reported that the greatest power of discrimination between normal and polycystic ovaries was obtained with combined measurement of follicular size and ovarian volume (sensitivity, 92% [48 of 52 patients]; specificity, 97% [28 of 29 control subjects]). Lujan et al.10 presented that follicular number has better diagnostic potential to distinguish between controls and women with PCOS compared with counts in a single cross section or ovarian volume. An average value of 26 or more follicles per ovary is a reliable threshold for detecting polycystic ovaries in women with frank manifestation of PCOS. Variable approaches were attempted to detect polycystic ovaries by sonography. Fulghesu et al.11 suggested that the ovarian stroma/total area ratio can differentiate between PCOS and control or multifollicular women with both a sensitivity and a specificity of 100%. Three-dimensional (3D) transrectal ultrasonography is also one of the modalities as diagnostic tools for PCOS. In the study with 75 amenorrheic, oligomenorrheic, or asymptomatic virgin patients and 25 healthy controls, 3D-TRS was shown to be convenient, accurate, specific, sensitive, and more reliable than transabdominal ultrasonography. Also, there were significant differences in ovarian stromal area and stromal area/total ovarian area ratio (S/A) ratio between patients with PCOS and controls.12
Although sonographic findings in PCOS are important, previous studies are still inadequate and have some limitations in establishing the precise diagnostic criteria. Additionally, in Asian countries, especially in Korea, TVS in not possible due to the fear of hymenal injuries in the patients who have no history of coitus. In such cases, transabdominal or TRS was performed to determine the gynecologic status. In our previous study, we observed that transabdominal ultrasound assessment is not effective for the detection of PCOS in young women of reproductive age.5 According to another study in 42 cases, transrectal scanning should be used liberally after proper patient selection and counseling and the images obtained are superior to TAS and comparable to those obtained by TVS.6
TRS is a useful method in many cases. Some investigators use TRS to guide the drainage of inflammatory pelvic abscess.13,14,15 Also, it can be used during transvaginal operation to guide procedures.16 TRS can provide effective, real-time assistance to the gynecological surgeon. As one of the diagnostic tools, TRS is also useful in gynecologic field. Kushnir et al.17 and Anguenot et al.18 diagnosed hematocolpometra and hematocolpos using TRS. Fedele et al.19 used TRS in nine patients, six with suspected Rokitansky-Küster syndrome and three with transverse vaginal septum. They compared TAS, TRS, and magnetic resonance imaging (MRI) with surgical findings. TRS provided images that corresponded perfectly with the real anatomical situation, while TAS provided inadequate images in six of the nine patients. The MRI was mistaken in one patient with suspected vaginal septum. The authors concluded that TRS can be considered as the diagnostic method of choice in the assessment of canalization defects of the vagina.
However, there was criticism on TRS that would probably be directed toward the question of trauma to the rectum. Ludwig et al.20 stated that rectal lesions during rectoscopy are rare. Anderson et al.21 found that in 10,486 colonoscopies over a 10-year period, 0.19% perforations were noted, most of them resulted from the use of cautery. Therefore, TRS performed by introducing a probe through the anal sphincter into the rectum does not seem to cause injuries.
In our study, ultrasound examinations were performed in 963 Korean women with transvaginal transducers in 677 women and transrectal transducers in 286 women. A total of 328 PCOS patients were enrolled in our study. To determine the diagnostic performance of transrectal ultrasound in virgin patients with PCOS compared with conventional transvaginal ultrasound assessment, ROC curve analysis was used. As per the results, by transvaginal ultrasound examination, the ovarian volume showed an AURC of 0.838. An ovarian volume decision threshold > 7 cm3 had a sensitivity of 73.0% and a specificity of 84.2% for the diagnosis of PCOS. The follicle number showed an AURC of 0.886. A follicle number decision threshold ≥ 9 had a sensitivity of 78.6% and a specificity of 87.2% for the diagnosis of PCOS. By transrectal ultrasound examination, the ovarian volume and the follicle number showed AURCs of 0.815. Follicle number and ovarian volume by transvaginal and transrectal ultrasound assessment had a high diagnostic power for PCOS screening. Base on this result, transrectal ultrasound assessment is as effective as conventional transvaginal ultrasound for the detection of PCOS in virgin patients.
To the best of our knowledge, there is no report on the diagnosis of PCOS by TRS. This study shows effective detection and diagnosis of PCOS by TRS in virgin Korean women.
Footnotes
Conflict of Interests: No potential conflict of interest relevant to this article was reported.
References
- 1.Zawadzki JK, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In: Dunaif A, Givens JR, Haseltine FP, Merriam GR, editors. Polycystic ovary syndrome. Boston, MA: Blackwell Scientific Publications; 1992. pp. 377–384. [Google Scholar]
- 2.Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Park JW, Hwang SO, Park JH, Lee BI, Lee JH, Kim KW, et al. Discrimination between benign and malignant pelvic masses using the risk of malignancy index 1. J Korean Soc Menopause. 2013;19:18–25. [Google Scholar]
- 4.Kim CR, Ku CH, Jeon IS, Son DW, Lee JS. The clinicopathologic features and significance of preoperative CA 125 in patients who had an operation for ovarian tumors. J Korean Soc Menopause. 2013;19:26–35. [Google Scholar]
- 5.Jeong KA, Lee WJ, Chung HW. Transabdominal ultrasound assessment of the polycystic ovary syndrome. Korean J Reprod Med. 2009;36:255–263. [Google Scholar]
- 6.Timor-Tritsch IE, Monteagudo A, Rebarber A, Goldstein SR, Tsymbal T. Transrectal scanning: an alternative when transvaginal scanning is not feasible. Ultrasound Obstet Gynecol. 2003;21:473–479. doi: 10.1002/uog.110. [DOI] [PubMed] [Google Scholar]
- 7.Norman RJ, Dewailly D, Legro RS, Hickey TE. Polycystic ovary syndrome. Lancet. 2007;370:685–697. doi: 10.1016/S0140-6736(07)61345-2. [DOI] [PubMed] [Google Scholar]
- 8.Lee DE, Park SY, Park SY, Lee SR, Chung HW, Jeong K. Clinical and Biochemical Profiles according to Homeostasis Model Assessment-insulin Resistance (HOMA-IR) in Korean Women with Polycystic Ovary Syndrome. J Menopausal Med. 2014;20:104–110. doi: 10.6118/jmm.2014.20.3.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pache TD, Wladimiroff JW, Hop WC, Fauser BC. How to discriminate between normal and polycystic ovaries: transvaginal US study. Radiology. 1992;183:421–423. doi: 10.1148/radiology.183.2.1561343. [DOI] [PubMed] [Google Scholar]
- 10.Lujan ME, Jarrett BY, Brooks ED, Reines JK, Peppin AK, Muhn N, et al. Updated ultrasound criteria for polycystic ovary syndrome: reliable thresholds for elevated follicle population and ovarian volume. Hum Reprod. 2013;28:1361–1368. doi: 10.1093/humrep/det062. [DOI] [PubMed] [Google Scholar]
- 11.Fulghesu AM, Ciampelli M, Belosi C, Apa R, Pavone V, Lanzone A. A new ultrasound criterion for the diagnosis of polycystic ovary syndrome: the ovarian stroma/total area ratio. Fertil Steril. 2001;76:326–331. doi: 10.1016/s0015-0282(01)01919-7. [DOI] [PubMed] [Google Scholar]
- 12.Sun L, Fu Q. Three-dimensional transrectal ultrasonography in adolescent patients with polycystic ovarian syndrome. Int J Gynaecol Obstet. 2007;98:34–38. doi: 10.1016/j.ijgo.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 13.Chung T, Hoffer FA, Lund DP. Transrectal drainage of deep pelvic abscesses in children using a combined transrectal sonographic and fluoroscopic guidance. Pediatr Radiol. 1996;26:874–878. doi: 10.1007/BF03178041. [DOI] [PubMed] [Google Scholar]
- 14.Pereira JK, Chait PG, Miller SF. Deep pelvic abscesses in children: transrectal drainage under radiologic guidance. Radiology. 1996;198:393–396. doi: 10.1148/radiology.198.2.8596838. [DOI] [PubMed] [Google Scholar]
- 15.Nelson AL, Sinow RM, Oliak D. Transrectal ultrasonographically guided drainage of gynecologic pelvic abscesses. Am J Obstet Gynecol. 2000;182:1382–1388. doi: 10.1067/mob.2000.106177. [DOI] [PubMed] [Google Scholar]
- 16.Bar-Hava I, Rabinerson D, Kaplan B, Orvieto R, Levy T, Shalev Y, et al. Real-time intraoperative ultrasound guidance: the transrectal approach. Ultrasound Obstet Gynecol. 2001;17:150–152. doi: 10.1046/j.1469-0705.2001.00258.x. [DOI] [PubMed] [Google Scholar]
- 17.Kushnir O, Garde K, Blankstein J. Rectal sonography for diagnosing hematocolpometra. A case report. J Reprod Med. 1997;42:519–520. [PubMed] [Google Scholar]
- 18.Anguenot JL, Ibecheole V, Salvat J, Campana A. Hematocolpos secondary to imperforate hymen, contribution of transrectal echography. Acta Obstet Gynecol Scand. 2000;79:614–615. [PubMed] [Google Scholar]
- 19.Fedele L, Portuese A, Bianchi S, Zanconato G, Raffaelli R. Transrectal ultrasonography in the assessment of congenital vaginal canalization defects. Hum Reprod. 1999;14:359–362. doi: 10.1093/humrep/14.2.359. [DOI] [PubMed] [Google Scholar]
- 20.Ludwig K, Schuster R, Diettrich H. Intestinal injuries in rectosigmoidoscopy in expert opinion. Zentralbl Chir. 1984;109:1268–1272. [PubMed] [Google Scholar]
- 21.Anderson ML, Pasha TM, Leighton JA. Endoscopic perforation of the colon: lessons from a 10-year study. Am J Gastroenterol. 2000;95:3418–3422. doi: 10.1111/j.1572-0241.2000.03356.x. [DOI] [PubMed] [Google Scholar]