Abstract
Primary lymphoma of the urinary bladder is a rare entity. It has a distinctively different presentation than the urothelial carcinoma, which is the most common form of bladder cancer, but might mimic inflammatory lesions such as tubercular cystitis, clinically as well as radiologically. We present a case of primary extranodal marginal zone lymphoma of the bladder, which was a close mimicker of tuberculosis, leading to delay in diagnosis. We highlight the role of biopsy in prompt diagnosis of these cases. We emphasize on the high index of suspicion required to identify such cases at an early stage, which has pronounced prognostic implications.
Keywords: Bladder, bladder cancer, lymphoma, mucosa associated lymphoid tissue type, tuberculosis
INTRODUCTION
Primary lymphoma of the bladder is rare, and it constitutes 5% of the nonurothelial tumor of the urinary tract.[1] They represent 0.2% of all known bladder malignancies and 0.2% of extranodal lymphomas.[2] Primary bladder lymphoma usually occurs in the background of chronic cystitis. We present a case of primary extranodal marginal zone lymphoma of the mucosa-associated lymphoid tissue type (MALT type lymphoma) of the bladder, which mimicked tubercular cystitis leading to delay in diagnosis.
CASE REPORT
A 53-year-old woman with on and off complaints of dysuria, urgency, urge incontinence, and increased frequency of urination presented to the urology department of our institute. There was long-standing history of recurrent cystitis, but no history of hematuria or loin pain.
On examination, there was no organomegaly or lymphadenopathy. Urine examination showed the presence of numerous pus cells, but on culture was sterile, signifying sterile pyuria. Urine cytology for malignant cells was negative. Routine hematological investigation, screening renal and liver function tests were normal except for mildly raised total count at 11,800 cells/cu mm. Peripheral blood smear examination was normal. The patient was hypothyroid. Ultrasound, computerized tomography (CT), and intravenous urography showed diffuse thickening of the bladder wall [Figure 1a and b]. Cystoscopy showed a smooth nonulcerated nodular bulge in the right side of the bladder wall [Figure 2]. Ziehl–Neelsen (ZN) stain of the urine showed the presence of acid-fast Bacilli (AFB). Based on the clinical presentation, imaging, a preliminary AFB positivity report, and due to the exceptionally high incidence of tuberculosis (TB) in this region, the patient was started on antitubercular treatment. Initially, the patient appeared to improve symptomatically. In the meantime, simultaneously sent urine sample for culture and polymerase chain reaction could not confirm the presence of mycobacterium TB. Furthermore, repeat samples of urine examined on microscopy did not reveal the presence of AFB.
Figure 1.
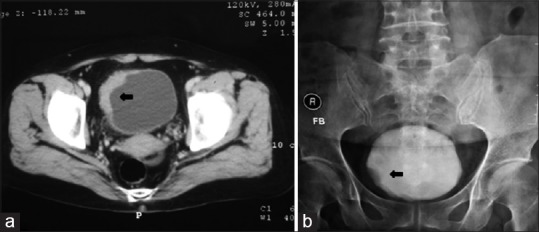
Pretreatment radiological images. (a) Computerized tomography scan and (b) intravenous urography showing thickening of the right lateral aspect of the urinary bladder wall (arrow)
Figure 2.
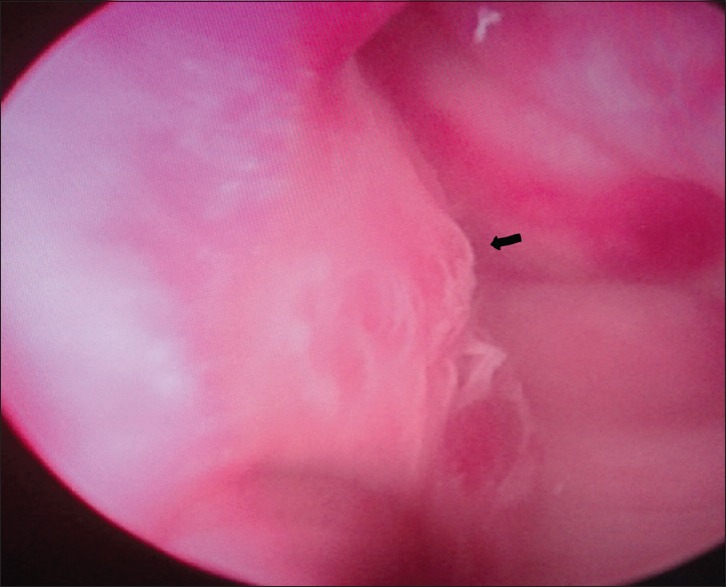
Pretreatment cystoscopy. A nonulcerated nodular bulge is seen on the right lateral wall of the bladder mucosa (arrow)
On recurrence of the symptoms, a repeat cystoscopy was performed, and the findings were similar to the pretreatment cystoscopy with thickening of the bladder mucosa. Hence, a bladder biopsy was planned, and transurethral resection was performed. Tissue was also taken from the deep muscle. Histopathological examination (HPE) showed intact but thinned out bladder epithelium. The subepithelial tissue showed the presence of lymphoid follicles with expanded marginal zone, which totally replaced the sub epithelial bladder tissue. The cells were small to medium sized with dispersed chromatin, inconspicuous nucleoli and abundant cytoplasm showing clearing, imparting monocytoid morphology. No large or transformed cells were seen. No granuloma was identified. On immunohistochemistry (IHC), the cells stained positive for CD45 and CD20 [Figure 3]. Cytokeratin, epithelial membrane antigen (EMA), CD3, CD5, CD10, and Bcl2 were negative. ZN stain was negative for AFB on the HPE sections. Deep muscle biopsy showed presence of lymphoid follicles with reactive germinal center. CT scan failed to reveal any lymphadenopathy or involvement of any other organ. Bone marrow examination was unremarkable.
Figure 3.
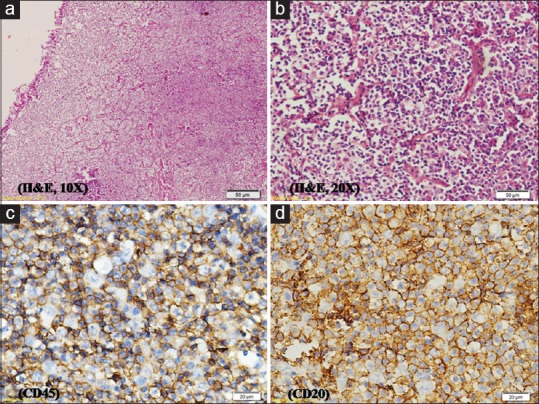
Histopathology images. (a and b) Intact but attenuated urothelium with diffuse replacement of subepithelium by lymphoma cells (H and E, x100 and x200). Lymphoma cells shows (c) CD45 positivity and (d) CD20 positivity on immunohistochemistry (×100)
Based on these findings, a diagnosis of primary MALT lymphoma of the bladder was made, Ann-Arbor stage 1EA. The patient was started on systemic chemotherapy with cyclophosphamide, vincristine, doxorubicin, and prednisolone. Six cycles were given. The patient is under follow-up and 9 months postchemotherapy, the patient is symptomatically normal. Repeat CT scan, cystoscopy, and postchemotherapy showed completely normal bladder [Figure 4].
Figure 4.
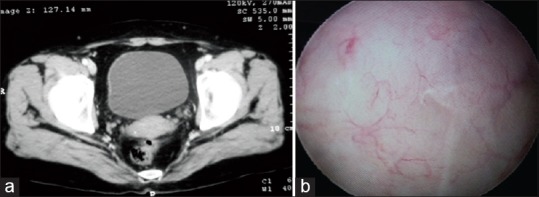
Posttreatment images. (a) Computerized tomography scan and (b) cystoscopy showing completely unremarkable bladder wall and mucosa
DISCUSSION
Bladder cancer is the second most common urogenital malignancy in India, urothelial transitional cell carcinoma being the most common type of bladder malignancy.[3,4] Primary lymphoma of the bladder is rare, it comprises 20% of all lymphomas of the bladder, the rest being secondary involvement of the bladder, which is a more common form of bladder lymphoma.[1] It was first described in 1885 by Eve and has marked female preponderance with a male to female ratio of 1:6.5.[5] MALT type lymphoma is the most common primary lymphoma, which was first described in 1990. Diffuse large B-cell lymphoma is the other known common type.[6]
Typically, primary bladder lymphoma is seen in a female patient, usually after the fifth decade of life. The patient presents with frequency, urgency, dysuria, lower abdominal pain, and most of the patients have a preceding history of chronic cystitis.[7] Genitourinary TB (GUTB) may present with recurrent, resistant urinary tract infection with sterile pyuria and irritative bladder symptoms, which might clinically mimic lymphoma.[8]
On imaging, the most common presentation of lymphoma is a submucosal mass, which may be solitary or multiple. Some cases present with diffuse bladder wall thickening.[9] These findings may mimic early bladder TB, which also shows reduced bladder volume with wall thickening or filling defects due to granulomatous material.[10] Our patient on initial evaluation showed similar findings supported by presence of AFB (probably contaminant on retrospective analysis), leading to a misdiagnosis of GUTB.
Biopsy supplemented by IHC is imperative in making the right diagnosis in such cases. On HPE, most lymphoma cases show small to medium sized cells, which usually do not involve the muscle fascicles. These cells reveal B-cell immunophenotype as was seen in our case. Some of these low-grade lymphoma cases are known to transform into higher grade DLBCL, implying that an early diagnosis of the MALT lymphoma is important for improved prognosis.[2]
Differential diagnosis of lymphoma on HPE includes undifferentiated urothelial carcinomas and lymphoepithelioma -like carcinoma.[9] Our case failed to reveal the presence of epithelial cells and was negative for cytokeratin and EMA on IHC, ruling out the above differentials.
MALT lymphomas are low-grade lymphomas. They follow an indolent course and are amenable to radiotherapy and chemotherapy.[9] Our case showed excellent response to chemotherapy with complete disappearance of the tumor following 6 cycles.
CONCLUSION
Primary bladder lymphoma of the MALT might be a diagnostic challenge and might mimic TB, clinically and on imaging. Biopsy plays an indispensable role in diagnosis. Suspicious cases should be biopsied as early diagnosis implies excellent prognosis and increased patient survival. A high index of suspicion is necessary to arrive at the correct diagnosis, especially in the developing countries where incidence of TB is high.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Marx A. World Health Organization Classification of Tumors. Pathology and Genetics of Tumors of the Urinary System and Male Genital Organs. In: Eble JN, Sauter G, Epstein IJ, Sesterhen IA, editors. World Health Organization Classification of Tumors. Lyon: IARC Press; 2004. p. 147. [Google Scholar]
- 2.Bacalja J, Ulamec M, Rako D, Boškovic L, Trnski D, Vrdoljak E, et al. Persistence of primary MALT lymphoma of the urinary bladder after rituximab with CHOP chemotherapy and radiotherapy. In Vivo. 2013;27:545–9. [PubMed] [Google Scholar]
- 3.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 4.Lopez-Beltran A, Sauter G, Gasser T, Hartmann A, Schmitz-Drager BJ, Helpap B, et al. Infiltrating urothelial carcinoma. In: Eble JN, Sauter G, Epstein IJ, Sesterhen IA, editors. World Health Organization Classification of Tumors. Pathology and Genetics of Tumors of the Urinary System and Male Genital Organs. Lyon: IARC Press; 2004. pp. 93–109. [Google Scholar]
- 5.Ohsawa M, Aozasa K, Horiuchi K, Kanamaru A. Malignant lymphoma of bladder. Report of three cases and review of the literature. Cancer. 1993;72:1969–74. doi: 10.1002/1097-0142(19930915)72:6<1969::aid-cncr2820720630>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 6.Kempton CL, Kurtin PJ, Inwards DJ, Wollan P, Bostwick DG. Malignant lymphoma of the bladder: Evidence from 36 cases that low-grade lymphoma of the MALT-type is the most common primary bladder lymphoma. Am J Surg Pathol. 1997;21:1324–33. doi: 10.1097/00000478-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Power RE, Kay EW, O’Connell F, Jaber AA, Donovan MG, Hickey DP, et al. Primary lymphoma of the bladder: A report of three cases. Ir J Med Sci. 2001;170:196–7. doi: 10.1007/BF03173891. [DOI] [PubMed] [Google Scholar]
- 8.Wise GJ, Marella VK. Genitourinary manifestations of tuberculosis. Urol Clin North Am. 2003;30:111–21. doi: 10.1016/s0094-0143(02)00123-4. [DOI] [PubMed] [Google Scholar]
- 9.Venyo AK. Lymphoma of the urinary bladder. Adv Urol 2014. 2014:327917. doi: 10.1155/2014/327917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burrill J, Williams CJ, Bain G, Conder G, Hine AL, Misra RR. Tuberculosis: A radiologic review. Radiographics. 2007;27:1255–73. doi: 10.1148/rg.275065176. [DOI] [PubMed] [Google Scholar]


