Abstract
Introduction:
Priapism has a devastating consequence on the sexual function of men if not promptly managed. We are presenting our experience of the treatment of priapism and the status of sexual function even following successful detumescence achieved after treatment.
Materials and Methods:
Nineteen patients, who presented with priapism from January 2012 to December 2014, were included in the study. After obtaining a detailed history; color Doppler ultrasonography of penis and blood gas analysis of the initial corporal aspirate were done to ascertain the type of priapism. Standard protocol in our institute for management of priaprism was to start with conservative treatment by corporal aspiration and intracorporeal injection (ICI) of phenylephrine. On the failure of conservative management, distal shunts were performed. Proximal shunts were performed on the failure of distal shunt procedures. Erectile function was evaluated with International Index of Erectile Function-5 questionnaire on admission and during follow-up.
Results:
All the patients had ischemic type priapism. Age of the patients ranged from 22 to 55 years. Duration of priapism varied from 20 to 480 h (mean 96.7). Etiologies attributed were; over-the-counter sildenafil use, chlorpromazine, opium intake and intracorporeal papaverine injection, chronic myeloid leukemia, and idiopathic. Five patients had preserved erectile function during follow-up. Preservation of normal erectile function following aspiration and ICI, proximal and distal shunt procedures were 66.7%, 18.1% and 20%, respectively.
Conclusion:
Patients with late presentation and those patients requiring higher treatment modalities (e.g., proximal shunts) for achieving detumescence will subsequently have a poor erectile function. These patients should be counseled about the early penile prosthesis placement during initial surgical management.
Keywords: Erectile dysfunction, impotence, penile implant, penile prosthesis, priapism
INTRODUCTION
Priapism although uncommon, has a devastating consequence on the sexual function of men if not promptly managed. Although various treatment modalities for ischemic priapism achieves the reversal of ischemic episode and complete detumescence of penis, with longer duration of priapism (>24 h), causes irreversible damage in the ultrastructure of the erectile tissue and later poor erectile function.[1] Many studies reported the results of various treatment modalities in priapism. However, most were retrospective in nature and having small number of patients. In those studies, the management protocol was also not clearly defined. We are presenting our experience on the treatment of priapism and the status of sexual function even following successful detumescence achieved after treatment.
MATERIALS AND METHODS
It was a prospective, observational study conducted in a tertiary care center. After the institute had obtained the ethical board clearance, we included all the patients who were presented with priapism to our department from January 2012 to December 2014. A total of nineteen patients were studied. On admission, detailed history of duration of the priapism, presence of penile pain, previous similar episodes or any treatment for priapism, drug intake, local or perineal trauma, blood dyscrasia, neurologic conditions, and erectile dysfunction (ED) were taken. In all the patients, color Doppler ultrasonography (CDU) of penis and blood gas analysis of the initial corporal aspirate were performed after the admission to differentiate the type of priapism (high flow or ischemic). For ischemic priapism, our protocol was to start immediate local treatment to resolve the ischemic environment. Initial corporal aspiration and irrigation were followed by intracorporeal injection (ICI) of phenylephrine (100 µg/ml) as per the requirement, up to a maximum dose of 1000 µg. If penis failed to detumescent after giving 1-h of conservative management, we proceeded for percutaneous distal shunt under local anesthesia (Winter shunt). We checked for penile detumescence following Winter shunt. If penile detumescence was not achieved within 30 min of Winter shunt, we performed open distal shunt under general anesthesia as soon as possible. Initially, we planned for Al-Ghorab shunt by glans incision and distal corporotomy. If all clots inside the corpora could not be evacuated by squeezing and saline irrigation, we performed “corporal snake” maneuver by introducing dilators through distal corporotomy. If erection persists following distal shunts, we repeated blood gas analysis of the corporal aspirate and CDU of the penis to check the resolution of the ischemic event. If it showed a failure of the distal shunt, we performed proximal shunt as soon as possible. In the postoperative period, frequent check for penile detumescence was performed. If failed, we repeated the CDU and did magnetic resonance imaging (MRI) of the penis. For patients who showed extensive corporal fibrosis on MRI, we advised for early penile prosthesis insertion. Follow-up was done at outpatient service. Erectile function was evaluated with the International Index of Erectile Function-5 (IIEF-5) questionnaire. Baseline erectile function score was recorded on admission and further scores were recorded at 6-month intervals during follow-up.
RESULTS
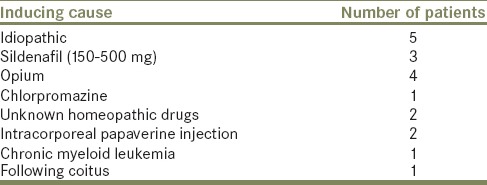
Age of the patients ranged from 22 to 56 years (mean 33.9). Duration of priapism varied from 20 to 480 h (mean 96.7). Etiologies attributed were; over-the-counter sildenafil use, chlorpromazine, opium intake and intracorporeal papaverine injection, and chronic myeloid leukemia [Table 1]. One newly married young patient reported priapism following coitus. He had no previous history of ED or priapism or prolonged erection episodes. Two patients had diabetes as well as hypertension as additional comorbidities. Rest of the patients had no medical comorbidities.
Table 1.
Etiologies of priapism
All patients had ischemic priapism, confirmed by CDU and blood gas analysis of the initial corporal aspirate. With initial intracorporeal aspiration and ICI of phenylephrine (total dose range: 600–1000 µg) penile detumescence was achieved in three patients. In two hypertensive patients, only intracorporeal aspiration was performed and phenylephrine injection was omitted. Fourteen patients had residual tumescence after bilateral Winter shunt procedure [Figure 1a], in those patients open distal shunts were performed. In six patients, Al-Ghorab shunt was performed. In eight patients “corporal snake” maneuver was performed [Figure 1b]. Al-Ghorab shunt was successful in four out of six patients and “corporal snake” maneuver was successful in five out of eight patients in achieving detumescence and reversing ischemic priapism. Five patients had persistent tumescence following distal shunt procedure on the next day. Proximal shunts (Quackles shunt) were performed in those patients. In all the patients, ischemic priapism event was reversed and successfully confirmed by CDU. Out of which three patients achieved complete detumescence, one patient had partial detumescence, and another had persistent priapism. In the case of persistent priapism, on further evaluation with the blood gas analysis of corporal aspirate and color Doppler ultrasound, showed conversion to high flow priapism due to the proximal shunt. In the other case of partial detumescence, the cause was due to fibrosis of the corpora as a result of prolonged duration of priapism (480 h) confirmed by MRI of the penis. MRI showed diffuse heterogenous low signal intensities on T2-weighted images in the corpora and after gadolinium injection there was no enhancement in the fibrotic regions in T1-weighted postcontrast images. Success rate observed in various treatment modalities depicted in Table 2.
Figure 1.
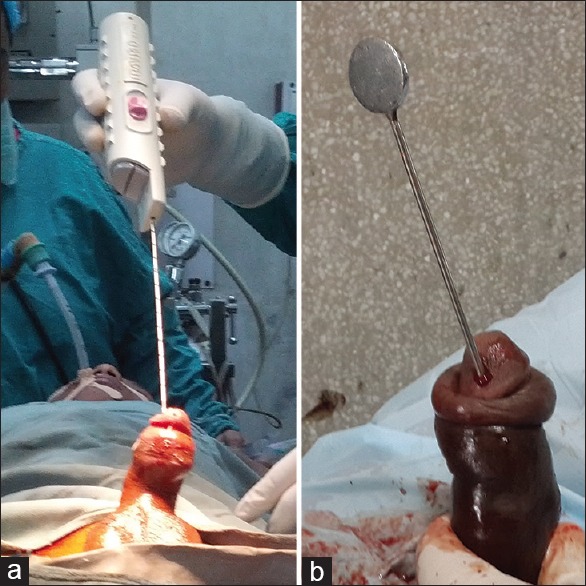
(a) Winter shunt. (b) Corporal snake maneuver with dilator passed into the corpora through glans incision
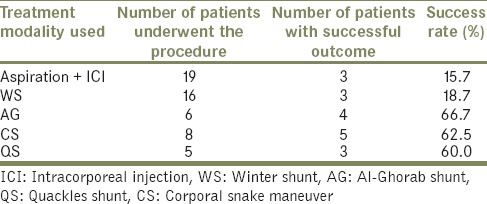
Table 2.
Success rate of treatment modalities
Urethral injury occurred in one patient during Al-Ghorab shunt, which is repaired intraoperatively over a urethral catheter. Another patient following “corporal snake” maneuver developed cavernositis and failure of the shunt, which was managed conservatively. One patient had partial penile skin necrosis.
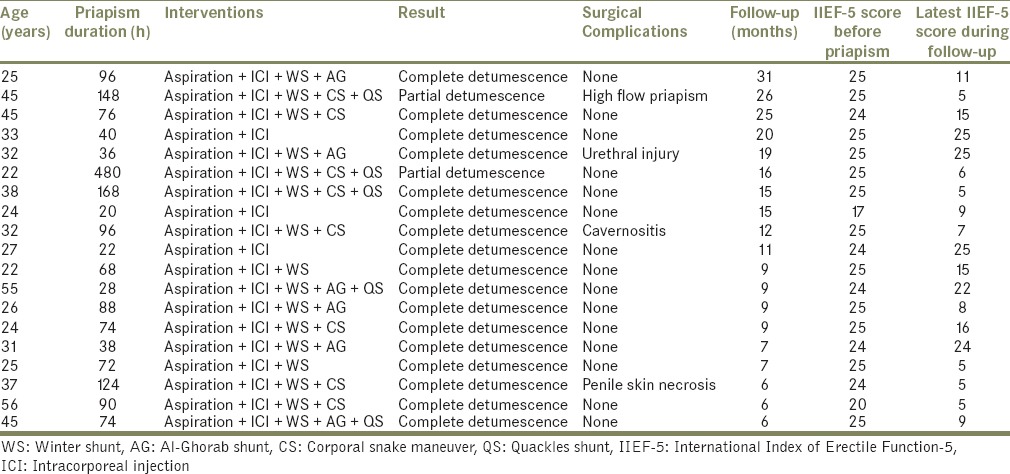
Mean follow-up time was 13.6 months (range: 6–31). Mean IIEF-5 score before the event was 24.0 (range: 25–17). During the follow-up, mean IIEF-5 score was 13.1 (range: 25–5) [Table 3]. Out of nineteen sexually active men, only two patients had mild ED before the priapism episode. Following priapism episode, only five patients preserved normal erectile function. We treated the patients who complained ED during the follow-up with tadalafil (10 to 20 mg as per requirement on demand). With tadalafil treatment, only two patients had improvement in their erectile function. Rest 12 patients had no improvement in erectile function with tadalafil during the follow-up. Mean duration of priapism in patients who preserved the prepriapism erectile function was 32.8 h (range: 22–40), whereas in patients who had declined erectile function was 119.6 h (range: 20–480) (P = 0.005, Mann–Whitney U-test). Two of the three patients (66.7%) treated with aspiration and ICI/aspiration alone had normal erectile function following the treatment. Preservation of normal erectile function following proximal and distal shunt procedures are 18.1% and 20%, respectively.
Table 3.
Summary of interventions done and result
DISCUSSION
Priapism is an acute condition, which needs prompt evaluation and appropriate management to maximize erectile function outcomes. It is defined as “full or partial erection that continues more than 4 h beyond sexual stimulation and orgasm or is unrelated to sexual stimulation.”[2] The term priapism was derived from Greek god “Priapus,” who was worshiped as the god of fertility and had giant phallus in sculptures.[3] In a population-based, retrospective cohort study, the incidence of priapism in the general population was reported to be 1.5 per 100,000 person-years.[4] Recent reports of incidence vary widely from 0.13 to 5.34 per 100,000 person-years.[5,6] Pathophysiologically, it is classified into two types; ischemic and nonischemic type. An intermittent variant of ischemic type is called “stuttering” priapism.[7,8] Ischemic priapism is the most common form of priapism (>95%) in all priapism episodes. Although most ischemic priapisms are idiopathic without any precipitating cause, various other etiologies have been attributed for ischemic priapism. Those are drug-induced, hematologic (most common: Sickle cell disease, other hemoglobinopathies), thrombophilia states (protein C and other thrombophilias, lupus), hyperviscosity states (hyperleukocytosis, polycythemia), and central nervous system disorders. Some are idiopathic.[9,10,11,12,13] In our series, all the cases were of ischemic type with varied etiologies. Mean duration of priapism was 96.7 h. Late presentation to medical facilities was due to patient's embarrassment and poor knowledge about the condition attributed to this prolonged duration of priapism at presentation.
Distinction of the type of priapism is paramount as ischemic type needs immediate treatment to preserve good sexual function. Color Doppler Ultrasound and blood gas analysis of corporal aspirate has been advocated initially to differentiate the type of priapism.[2,11,14,15] In our series, CDU accurately diagnosed the ischemic priapism and associated cavernous thrombosis in all cases. In postoperative period, CDU is important for diagnosing the patency of shunt in doubtful cases.[14,16]
In case of ischemic priapism, immediate penile aspiration should be initiated irrespective of the cause without delay.[8] In our study, aspiration with ICI of phenylephrine successfully reversed ischemic priapism in three out of six patients who had presented within 48 h of onset. Overall success rate was 15.7%. Reported success rate of aspiration alone is about 30% and intracavernous injection with or without aspiration ranges from 43% to 81%.[17] In our series, the lower success rate was probably due to delayed presentation to our institution as it was a tertiary center. Winter shunt was successful only in three patients out of sixteen patients in whom the procedure was performed and others (81.3%) required additional shunt procedures. Nixon et al. reported that 86% of their patients treated with a Winter shunt required a second shunt procedure.[18] However, in another report, success rate of Winter shunt was about 66%.[17] Our result and other reports show although Winter shunt is less invasive; the results are poor with this shunt procedure. Open distal shunts such as Al-Ghorab or “corporal snake” maneuver were successful in nine out of fourteen patients to achieve detumescence (64.3% success rate). One patient with “corporal snake” maneuver developed cavernositis and closure of shunt in the 3rd postoperative day and was managed conservatively. Al-Ghorab shunt has a reported success rate of about 74%.[17] In the rest of five patients who had failed distal shunts underwent bilateral Quackles shunt, which was successful in three patients. One developed persistent, partial tumescence due to conversion to high flow type, confirmed by Doppler ultrasound. Another patient who had priapism for about 20 days failed to achieve complete detumescence due to extensive corporal fibrosis.
We used IIEF-5 questionnaire to evaluate ED in the treated patients before the priapism event and during the follow-up at a 6-month interval, which is a validated tool.[19,20] Out of 19 sexually active men, only five patients preserved normal erectile function. This poor result was due to the prolong duration of priapism (without ED mean was 32.8 h, whereas patients having ED mean was 119.6 h). Zheng et al. in their series reported poor erectile function following the treatment of priapism (severe ED present in six out of eight patients) with the mean priapism duration of 96.33 h.[21] Gottsch et al. reported adequate erection in only six of the 35 patients following the treatment of priapism.[22] Tabibi et al. reported normal erectile function in 50%, 33.3%, and 25% of patients following Winter, Al-Ghorab, and Grayhack shunt, respectively. Mean duration of priapism was 51.12 h.[23] Our result also shows poor preservation of erectile function following shunt surgery. In our study, preservation of normal erectile function following proximal and distal shunt procedures were 18.1% and 20%, respectively. Natural history of untreated ischemic priapism or refractory priapism to interventions is severe penile fibrosis, which results in penile deformity, length loss, and ED. Some advocated immediate penile prosthesis insertion in priapism lasting more than 48–72 h due to future inevitable poor ED. The advantages over delay placement of prosthesis described are technically easier implant insertion and preserved penile length.[24,25] However, high complications were associated with immediate prostheses such as 24% revision rate and 6% infection rate.[25] In our settings, due to nonavailability of an immediate prosthesis and financial constraints with the patients, we did not put any penile prosthesis. However, shunt surgery was done irrespective of the duration of priapism as it is reported that failure to maintain complete detumescence leads to increased corporal fibrosis and poor erectile function following priapism.[26]
Limitation of this study is that it has fairly small number of patients.
CONCLUSION
Patients with late presentation and those patients requiring higher treatment modalities (e.g. proximal shunts) for achieving detumescence will subsequently have poor erectile function irrespective of the successful outcome in achieving complete detumescence of the penis. These patients should be counseled about the early penile prosthesis placement during initial surgical management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Spycher MA, Hauri D. The ultrastructure of the erectile tissue in priapism. J Urol. 1986;135:142–7. doi: 10.1016/s0022-5347(17)45549-2. [DOI] [PubMed] [Google Scholar]
- 2.Broderick GA, Kadioglu A, Bivalacqua TJ, Ghanem H, Nehra A, Shamloul R. Priapism: Pathogenesis, epidemiology, and management. J Sex Med. 2010;7(1 Pt 2):476–500. doi: 10.1111/j.1743-6109.2009.01625.x. [DOI] [PubMed] [Google Scholar]
- 3.Papadopoulos I, Kelâmi A. Priapus and priapism. From mythology to medicine. Urology. 1988;32:385–6. doi: 10.1016/0090-4295(88)90252-x. [DOI] [PubMed] [Google Scholar]
- 4.Eland IA, van der Lei J, Stricker BH, Sturkenboom MJ. Incidence of priapism in the general population. Urology. 2001;57:970–2. doi: 10.1016/s0090-4295(01)00941-4. [DOI] [PubMed] [Google Scholar]
- 5.Sugihara T, Yasunaga H, Horiguchi H, Nishimatsu H, Matsuda S, Homma Y. Incidence and clinical features of priapism in Japan: 46 cases from the Japanese diagnosis procedure combination database 2006-2008. Int J Impot Res. 2011;23:76–80. doi: 10.1038/ijir.2011.7. [DOI] [PubMed] [Google Scholar]
- 6.Roghmann F, Becker A, Sammon JD, Ouerghi M, Sun M, Sukumar S, et al. Incidence of priapism in emergency departments in the United States. J Urol. 2013;190:1275–80. doi: 10.1016/j.juro.2013.03.118. [DOI] [PubMed] [Google Scholar]
- 7.Shrewsberry A, Weiss A, Ritenour CW. Recent advances in the medical and surgical treatment of priapism. Curr Urol Rep. 2010;11:405–13. doi: 10.1007/s11934-010-0142-4. [DOI] [PubMed] [Google Scholar]
- 8.Huang YC, Harraz AM, Shindel AW, Lue TF. Evaluation and management of priapism: 2009 update. Nat Rev Urol. 2009;6:262–71. doi: 10.1038/nrurol.2009.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadeghi-Nejad H, Seftel AD. The etiology, diagnosis, and treatment of priapism: Review of the American Foundation for Urologic Disease Consensus Panel Report. Curr Urol Rep. 2002;3:492–8. doi: 10.1007/s11934-002-0103-7. [DOI] [PubMed] [Google Scholar]
- 10.Cherian J, Rao AR, Thwaini A, Kapasi F, Shergill IS, Samman R. Medical and surgical management of priapism. Postgrad Med J. 2006;82:89–94. doi: 10.1136/pgmj.2005.037291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burnett AL, Sharlip ID. Standard operating procedures for priapism. J Sex Med. 2013;10:180–94. doi: 10.1111/j.1743-6109.2012.02707.x. [DOI] [PubMed] [Google Scholar]
- 12.Salonia A, Eardley I, Giuliano F, Hatzichristou D, Moncada I, Vardi Y, et al. European Association of Urology guidelines on priapism. Eur Urol. 2014;65:480–9. doi: 10.1016/j.eururo.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 13.Vorobets D, Banyra O, Stroy A, Shulyak A. Our experience in the treatment of priapism. Cent European J Urol. 2011;64:80–3. doi: 10.5173/ceju.2011.02.art6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halls JE, Patel DV, Walkden M, Patel U. Priapism: Pathophysiology and the role of the radiologist. Br J Radiol. 2012;85:S79–85. doi: 10.1259/bjr/62360925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Levey HR, Segal RL, Bivalacqua TJ. Management of priapism: An update for clinicians. Ther Adv Urol. 2014;6:230–44. doi: 10.1177/1756287214542096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chiou RK, Aggarwal H, Chiou CR, Broughton F, Liu S. Colour Doppler ultrasound hemodynamic characteristics of patients with priapism before and after therapeutic interventions. Can Urol Assoc J. 2009;3:304–11. doi: 10.5489/cuaj.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Montague DK, Jarow J, Broderick GA, Dmochowski RR, Heaton JP, Lue TF, et al. American Urological Association guideline on the management of priapism. J Urol. 2003;170(4 Pt 1):1318–24. doi: 10.1097/01.ju.0000087608.07371.ca. [DOI] [PubMed] [Google Scholar]
- 18.Nixon RG, O’Connor JL, Milam DF. Efficacy of shunt surgery for refractory low flow priapism: A report on the incidence of failed detumescence and erectile dysfunction. J Urol. 2003;170:883–6. doi: 10.1097/01.ju.0000081291.37860.a5. [DOI] [PubMed] [Google Scholar]
- 19.Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26. doi: 10.1038/sj.ijir.3900472. [DOI] [PubMed] [Google Scholar]
- 20.Rhoden EL, Telöken C, Sogari PR, Vargas Souto CA. The use of the simplified International Index of Erectile Function (IIEF-5) as a diagnostic tool to study the prevalence of erectile dysfunction. Int J Impot Res. 2002;14:245–50. doi: 10.1038/sj.ijir.3900859. [DOI] [PubMed] [Google Scholar]
- 21.Zheng DC, Yao HJ, Zhang K, Xu MX, Chen Q, Chen YB, et al. Unsatisfactory outcomes of prolonged ischemic priapism without early surgical shunts: Our clinical experience and a review of the literature. Asian J Androl. 2013;15:75–8. doi: 10.1038/aja.2012.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gottsch HP, Berger RE, Yang CC. Priapism: Comorbid factors and treatment outcomes in a contemporary series. Adv Urol 2012. 2012:672624. doi: 10.1155/2012/672624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tabibi A, Abdi H, Mahmoudnejad N. Erectile function and dysfunction following low flow priapism: A comparison of distal and proximal shunts. Urol J. 2010;7:174–7. [PubMed] [Google Scholar]
- 24.Rees RW, Kalsi J, Minhas S, Peters J, Kell P, Ralph DJ. The management of low-flow priapism with the immediate insertion of a penile prosthesis. BJU Int. 2002;90:893–7. doi: 10.1046/j.1464-410x.2002.03058.x. [DOI] [PubMed] [Google Scholar]
- 25.Ralph DJ, Garaffa G, Muneer A, Freeman A, Rees R, Christopher AN, et al. The immediate insertion of a penile prosthesis for acute ischaemic priapism. Eur Urol. 2009;56:1033–8. doi: 10.1016/j.eururo.2008.09.044. [DOI] [PubMed] [Google Scholar]
- 26.El-Bahnasawy MS, Dawood A, Farouk A. Low-flow priapism: Risk factors for erectile dysfunction. BJU Int. 2002;89:285–90. doi: 10.1046/j.1464-4096.2001.01510.x. [DOI] [PubMed] [Google Scholar]


