Abstract
Context:
Thulium LASER is fast emerging as a safe and effective modality for benign prostatic hyperplasia (BPH). Still, compared to holmium laser transurethral enucleation of the prostate (HoLEP) the number of institutes all over the world using Thulium LASER are limited. This is our effort to bring the statistical facts about the safety and effectivity of Thulium LASER.
Aims:
To study the efficacy of thulium laser enucleation of the prostate (ThuLEP).
Settings and Design:
All patients in the stipulated period were documented for all parameters and were evaluated. The results were tabulated.
Subjects and Materials:
(1) Two hundred and thirty-six patients with symptomatic BPH were treated with ThuLEP between March 2010 and September 2014 at our institute by a single surgeon. (2) The inclusion criteria were maximum urinary flow rate (Qmax) <15 ml/s, International Prostate Symptoms Score (IPSS) >15 or acute retention of urine with the failure of catheter trial or Acute retention of urine with prior history of severe bladder outlet obstruction. (3) Patients evaluated by: Digital rectal examination, uroflowmetry, IPSS, prostate-specific antigen (PSA), blood and urine routine tests, abdominal usage with trains rectal ultrasonography (TRUS), TRUS guided biopsies.
Statistical Analysis Used:
Not used.
Results:
(1) ThuLEP was a highly effective procedure as compared to all other procedures like HOLEP, TURP in terms of catheterization time, hospital stay, and drop in hemoglobin (Hb). (2) Catheterization time: 25.22 h (224 patients within 24 h and 12 patients within 48 h). (3) Hospital stay: 24–36 h 218 patients (92.3%), 36–48 h 18 patients (7.6%). (4) Drop in Hb: 0.8 ± 0.42 g/dl. (5) Average operative time: 56.91 min.
Conclusions:
Thulium LASER is a safe and highly effective LASER in terms of blood loss, speed of tissue resection, drop in serum PSA, and versatility of prostatic resection.
Keywords: Benign prostatic hyperplasia, enucleation, morbidity, morcellation, mortality, thulium laser
INTRODUCTION
Urologists all over the world are in constant search for the “gold standard” treatment for benign prostatic hyperplasia (BPH). Recently, there has been a surge in a newer technique such as various LASERS and bipolar TURP and its various modifications. LASERs have come up a long way in their developments from evaporation till enucleation techniques and various combinations. Urologists themselves have stretched themselves for acquiring new skills to do prostatectomy in a total reverse way by LASER enucleation compared to TURP. Morcellation machines and their accessories have helped us to achieve enucleation in larger glands too. We study the outcome of 236 patients operated for thulium laser enucleation of the prostate (ThuLEP).
SUBJECTS AND METHODS
In this prospective study, 236 patients with symptomatic BPH were treated with ThuLEP between March 2010 and September 2014 at a single institute.
The inclusion criteria
Were maximum urinary flow rate (Qmax) <15 ml/s, International Prostate Symptoms Score (IPSS) >15 or acute retention of urine with the failure of catheter trial or acute retention of urine with prior history of severe bladder outlet obstruction.
Exclusion criteria
Were neurogenic bladder, associated strictures, associated bladder stones, and operations by other surgeons, malfunction of LASER converted to TURP.
Preoperative assessment with IPSS, digital rectal examination, uroflowmetry prostate specific antigen (PSA), and routine pathological evaluation including PSA was done. Abdominal use with trains rectal ultrasonography (TRUS) was performed. TRUS guided biopsies were done whenever indicated.
A total of 236 ThuLEP procedures was performed by a single surgeon. One hundred and twenty Watt Quanta (Italy) systems, LASER machine with 600 µ fiber with the standard resectoscope with the Kuntz working element (Richard–Wolf) were used along with Richard–Wolf Piranha morcellator with morsoscope.
Three lobar enucleation technique was used when the median lobes were large. Two lobar technique used when median lobe was not significant. We started at 5 and 7 o’clock, incision deepened till capsule and from the bladder neck till verumontanum and then joining them together delineating the capsule all along. Mechanical lifting the lobe away from the capsule was used, but lobes were not dissected by mechanical force. Twelve o’clock incision was taken, the lateral lobes were dissected from 12 o’clock to 3 o’clock by dissecting lateral lobes away from capsule using laser energy, once 5 o’clock and 3 o’clock gutter were dissected well, they were joined in convex manner and lobe was separated. The same procedure was repeated 9 o’clock till 7 o’clock. Then, the lobes were morcellated. In prostates with insignificant median lobes, instead of 5 and 7 o’clock, 6 o’clock incisions were taken, and the same procedure was followed.
The energy used varied from 35 w to 80 w, normal saline was used as irrigation 29 patients were on ecosprin and six patients were on ecosprin + clopidogrel. The ASA grade III + were seen in 59 patients. All patients who were on ecosprin in whom it could be stopped safely according to cardiologist's opinion were stopped at least 5 days prior. Those with severe ischemic heart disease (IHD) or vascular insufficiencies requiring ecosprin were continued on ecosprin with or without clopidogrel.
20 F Foley's catheter was inserted postoperative. Traction on Foley's catheter was not given in any patients except for two patients with significant hematuria in the immediate postoperative period. The catheter was removed within 24 h postoperative in 224 patients and within 48 h in 12 patients. Six patients had not cleared urine totally without irrigation fluids (hematuria not stopped totally). Hence, catheter removal was delayed until 48 h and for six patients in ecosprin + clopidogrel it was done as a precautionary measure.
Preoperative hemoglobin (Hb) and Hb after 24 h after surgery were compared to document the blood loss. Histopathology reporting was done in all patients.
All patients were watched for 6–8 h for retention/urinary flow rate/hematuria/incontinence.
IPSS score was compared along with other symptoms were documented at 4–6 weeks postoperative. All the associated events in intraoperative, immediate postoperative and till 6 weeks postoperative period was documented such as – hematuria, clot retention, postoperative pain, urgency, frequency, dysuria, incontinence, stress urinary incontinence, retention, retrograde ejaculation, and urinary tract infection.
Serum PSA was compared preoperative and 4–6 weeks postoperative.
All patients were followed for a period of minimum 11 months. Following parameters were documented: Age, IPSS score, duration of surgery, retention, PSA, prostate size, Qmax, average flow rates, ASA score, associated co-morbidities, hypertension, IHD, DM, CRF, pacemakers, antiplatelet drugs, clot retention, readmission, postoperative symptoms of <1 month period, and late (>1 month) complications.
The minimum age was 57 years and maximum 94 years (mean - 68 years).
RESULTS
Out of 236 patients in our study five were below 60 years of age, 161 were between 6 and 70 years of age, 59 were between 71 and 80 years of age, 14 patients from 81 to 90 years of age and two patients were between 91 and 95 years of age.
Eighty-one patients out of 236 presented with retention of urine. IPSS score was documented in 155 patients. IPSS score improved from 21 in the preoperative stage to 4.2 in the postoperative stage. Preoperatively Qmax was in the range of 9–13.5 and it improved to 18–24 in the postoperative period.
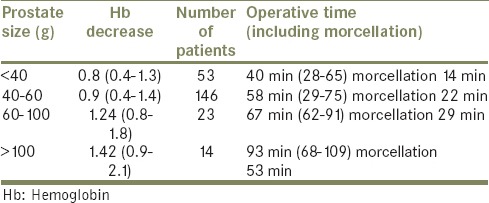
Fifty-nine patients had a postvoid residue <100 ml. Sixty-eight patients had a residue between 100 ml and 200 ml and 28 patients had a residue of >200 ml. Co-relation of prostatic size with the operative time [Table 1].
Table 1.
Co-relation of prostatic size with the operative time
In two patients, the procedure had to be done in two stages, one due to left ventricular failure and another due to the transient ischemic attack. Second stage morcellation was done in four patients due to lack of vision, oversized prostatic lobe and inadequate anesthesia.
The drop in Hb was observed in the range of 0.8–1.42 g/dl.
The PSA value dropped from 3.8 ng/dl in preoperative period to 1.2 ng/dl in the postoperative period, that is, drop of 68% after 4–6 weeks.
In 224 patients (94%) catheter was removed within 24 h postoperative. In six patients with ecosprin and clopidogrel catheter was removed after 48 h as a precautionary measure. In six patients hematuria did not subside totally after 24 h (without irrigation) and hence catheter was removed after 24 h. Re-catheterization was required in only three patients (1.2%).
Twenty-one patients (92.3%) were discharged between 24 h and 6 h and 18 patients (7.6%) were discharged between 36 h and 48 h.
Only two patients (0.84%) required catheter wash (bedside) for clot retention. Superficial bladder injury due to morcellation was seen in 18 patients (7.62%).
None of the patients required a blood transfusion.
Stricture urethra was seen in nine patients (3.82%) requiring a second procedure. Bladder neck contracture was seen in three patients (1.27%).
DISCUSSION
Thulium LASER is proclaimed to be the safest and most effective LASER in term of blood loss, the speed of tissue resection and versatility of prostatic resection.
In our study, the improvement of obstructive symptoms, PVR, Qmax were better compared to other studies involving holmium laser transurethral enucleation of the prostate (HOLEP), TURP thereby proving that ThuLEP is equally effective.
The drop in Hb in immediate postoperative period is also the least for ThuLEP in our group as compared to HOLEP, TURP, and PVP studies. This is more significant as quite a large number of patients (35) were on ecosprin (29) or along with clopidogrel (6). The peri-operative complication rates - bleeding, TURP syndrome, UTI, mortality and requirement of the second stage (a requirement of the second stage was purely medical reasons - LVF one, TIA one, morcellation related four) were quite low.
There were no cases of TURP syndrome, cases of UTI amounting to the requirement of antibiotics in the postoperative period beyond 5-7 days: 9%
Mortality - 0%.
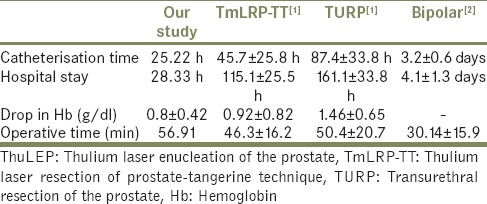
ThuLEP is a better procedure as compared to all other procedures TURP, Bipolar TURP, etc., in terms of catheterization time, hospital stay, and drop in Hb [Table 2].[1,2,3]
Table 2.
Comparison of ThuLEP with TURP and bipolar TURP
If we compare the results of ThuLEP with few studies other of HoLEP, ThuLEP has many advantages as seen in the following studies [Table 3].
Table 3.
Comparison of ThuLEP with other studies
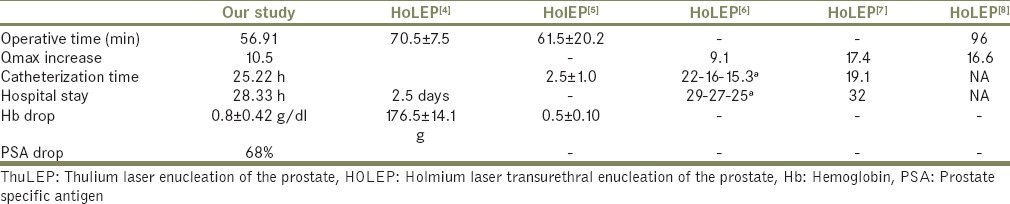
According to Sally Robertson, ThuLEP was superior to HoLEP in terms of blood loss 130 ml versus 166.6 ml but inferior to HoLEP in operative time 72.4 versus 61.5 min.
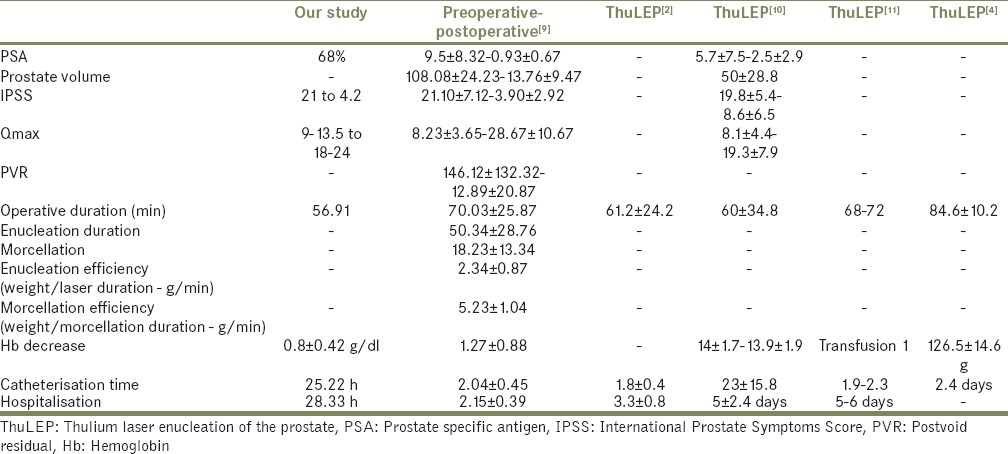
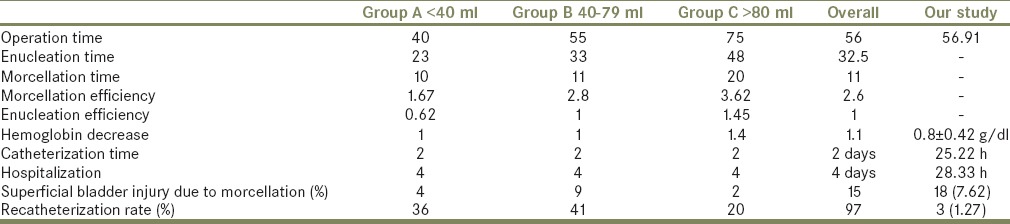
We have observed that the safety and high efficacy of ThuLEP was proven by various other studies. Comparing our study to various other studies of ThuLEP [Table 4].
Table 4.
Comparison of our study to various other studies
There was a gross difference in enucleation time and morcellation time in our study and this study. In our study, the morcellation time was 14–22 min for prostate size <60 g. However, it was 29–53 min for prostate larger than 60 g.
Morcellation: Morcellation technique available at present has limitations. The morsoscope or nephroscope used have limited vision due to small caliber of scopes and bladder being a large cavity. Even a small amount of bleeding will hamper the vision, thereby delaying the completion of morcellation. It is too dangerous to continue morcellation without good vision. We had to abandon the procedure in four patients, and morcellation had to be completed in the second setting. Smooth ball like prostatic tissue seen (cotton balls) at the end of morcellation is a greater problem as they need to be evacuated with forceps if small or removed by cutting with a laser. We have completed a few cases by drilling holes into them by thulium LASER and then removing them by morcellation.
We compared our data with preoperative data of 1080 patients who underwent thulium vaponucleation of the prostate stratified by prostate size [Table 5].[12]
Table 5.
We compared our data with peri operative data of 1080 patients who underwent thulium vapoenucleation of the prostate stratified by prostate size
According to Zhang et al. Both ThuLEP (70 W) and HoLEP (90 W) relieve lower urinary tract symptoms equally with high efficacy and safety. ThuLEP was statistically superior to HoLEP in blood loss and inferior to HoLEP in operation time, although the differences were clinically negligible.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Xia SJ, Zhuo J, Sun XW, Han BM, Shao Y, Zhang YN. Thulium laser versus standard transurethral resection of the prostate: A randomized prospective trial. Eur Urol. 2008;53:382–89. doi: 10.1016/j.eururo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 2.Peng B, Chun G, Wang C. A comparative study of thulium laser resection of the prostate and bipolar transurethral plasmakinetic prostatectomy for treating benign prostatic hyperplasia. BJU. 2012;III:633–7. doi: 10.1111/j.1464-410X.2012.11610.x. [DOI] [PubMed] [Google Scholar]
- 3.Robertson S. Thulium and holmium lasers equally effective in prostate surgery. Urology. 2012 [Advanced online publication] [Google Scholar]
- 4.Shao Q, Zhang FB, Shang DH, Tian Y. Comparison of holmium and thulium laser in transurethral enucleation of the prostate. Zhonghua Nan Ke Xue. 2009;15:346–9. [PubMed] [Google Scholar]
- 5.Zhang F, Shao Q, Herrmann TR, Tian Y, Zhang Y. Thulium laser versus holmium laser transurethral enucleation of the prostate: 18-month follow-up data of a single center. Urology. 2012;79:869–74. doi: 10.1016/j.urology.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 6.Humphreys MR, Miller NL, Handa SE, Terry C, Munch LC, Lingeman JE. Holmium laser enucleation of the prostate – outcomes independent of prostate size? J Urol. 2008;180:2431–5. doi: 10.1016/j.juro.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 7.Krambeck AE, Handa SE, Lingeman JE. Experience with more than 1,000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol. 2010;183:1105–9. doi: 10.1016/j.juro.2009.11.034. [DOI] [PubMed] [Google Scholar]
- 8.Elmansy HM, Kotb A, Elhilali MM. Holmium laser enucleation of the prostate: Long-term durability of clinical outcomes and complication rates during 10 years of followup. J Urol. 2011;186:1972–6. doi: 10.1016/j.juro.2011.06.065. [DOI] [PubMed] [Google Scholar]
- 9.Iacono F, Prezioso D, Di Lauro G, Romeo G, Ruffo A, Illiano E, et al. Efficacy and safety profile of a novel technique, ThuLEP (Thulium laser enucleation of the prostate) for the treatment of benign prostate hypertrophy. Our experience on 148 patients. BMC Surg. 2012;12(Suppl 1):S21. doi: 10.1186/1471-2482-12-S1-S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Szlauer R, Götschl R, Razmaria A, Paras L, Schmeller NT. Endoscopic vaporesection of the prostate using the continuous-wave 2-microm thulium laser: Outcome and demonstration of the surgical technique. Eur Urol. 2009;55:368–75. doi: 10.1016/j.eururo.2008.10.034. [DOI] [PubMed] [Google Scholar]
- 11.Bach T, Herrmann TR, Haecker A, Michel MS, Gross A. Thulium: Yttrium-aluminium-garnet laser prostatectomy in men with refractory urinary retention. BJU Int. 2009;104:361–4. doi: 10.1111/j.1464-410X.2009.08412.x. [DOI] [PubMed] [Google Scholar]
- 12.Gross AJ, Netsch C, Knipper S, Hölzel J, Bach T. Complications and early postoperative outcome in 1080 patients after thulium vapoenucleation of the prostate: Results at a single institution. Eur Urol. 2013;63:859–67. doi: 10.1016/j.eururo.2012.11.048. [DOI] [PubMed] [Google Scholar]


