Abstract
Background
Anesthesiologists routinely perform high-risk procedures that are associated with permanent disability or death. Critical perioperative events require that the anesthesiologist perform procedures that are only used intermittently. Teaching these procedures is complicated by their infrequency and pressure to maximize operating room efficiency; therefore we created an annual 1-day anesthesiology skills lab as an innovative method of residency education.
Methods
Anesthetized pigs served as the educational platform for first-year anesthesiology residents to gain hands-on experience performing regional, thoracic, vascular, and difficult airway techniques. A 20-question test was administered pre- and post-lab to assess the effectiveness of our educational intervention. Participants evaluated the quality of the educational experience (1-poor to 5-excellent).
Results
First-year anesthesiology residents participated (n=70, 2008-2012). Residents’ pre-test scores measured 50.3±2.6% (range 20-80). Following lab participation, their test scores signi ficantly improved to a mean of 84.2±1.9% (range 45-100, p<0.0001). Participants increased their knowledge and skills (mean 4.96±0.02), considered the skills lab to be a worthwhile educational experience (mean 4.99±0.01), and agreed that the lab should be repeated in the future (mean 5.00).
Conclusions
In vivo labs confers educational benefits which are both perceived and self-reported by the participants and objectively demonstrated by marked improvements in their post-test scores. Animal models provide high-fidelity tactile learning, real-time physiological changes, and potential for complications which builds residents’ familiarity and confidence with anesthesiology-related procedures and crisis events that would otherwise involve potential patient risk. Our lab is an enriching and well-received educational tool which promotes our goal of improving patient safety.
Keywords: Anesthesiology, residency, education, in vivo, skills, animal
Introduction
Anesthesiologists routinely perform high-risk procedures that are associated with permanent disability or death. Critical perioperative events which contribute to adverse patient outcomes must be recognized and treated and often require techniques (ex. cricothyrotomy) that the anesthesiologist infrequently employs. Often these techniques cannot be taught to residents in an elective setting.1,2 Additionally, there is increased pressure to maximize efficiency in the operating room (OR).3,4 Despite the critical nature of these procedures and the pressured OR setting, this is the very environment where anesthesiology residents are often learning skills on patients for the first time.4
The field of Anesthesiology currently utilizes varied curricula to improve cognitive and technical skills, accelerate the acquisition of new skills, and increase exposure to crisis situations outside of the clinical arena via the incorporation of mannequins/simulators,1,5 computers and web-based training,6 cadavers,7 ex vivo models,8 and human volunteers.9 In vivo models most closely replicate the human patient in terms of tactile and real-time feedback, anatomy, hemodynamic/respiratory function, physiological responses to pharmacological support, and complications including blood loss, edema, arrhythmias, and death. While the use of an in vivo laboratory in residency training has been shown to improve participants’ procedural speed and competency in other fields,10-12 a recent survey found that only 7.9% of anesthesiology chief residents surveyed practiced airway emergencies in an animal lab.13
In 2008 we developed a single-day in vivo skills laboratory as a way for our first-year anesthesiology residents to learn and practice technical skills each July prior to beginning formal residency training. The educational objectives were for the residents to review and gain hands-on experience performing anesthesia, critical care, cardiovascular, and thoracic procedures under the guidance of attending anesthesiologists in a risk-free environment where mistakes are permissible. They were encouraged to experience the successes, complications, and failures of their attempts, and to utilize teamwork, decision-making skills, and crisis-management skills to build familiarity and confidence with the goal of improving patient safety as they segue into patient care. In this paper we present our course curriculum that we have refined over the past five years, the results of resident participation and follow-up data, and discuss the process for developing an in vivo anesthesiology skills lab.
Materials and Methods
Model
Our anesthesiology skills lab received approval from the Institutional Animal Care and Use Committee (IACUC) and conformed to the Guide for the Care and Use of Laboratory Animals (NRC 2011). Pigs (25-35kg) underwent tiletamine-zolazepam sedation (6.0mg/kg IM) and intubation. Ventilation was maintained at a PaCO2 of 40mmHg under 1.5-2.5% isoflurane anesthesia. Ketamine (1.0mg/kg/hr IV) was additionally administered during the airway procedures. At the end of the course, the animals were euthanized under general anesthesia per the IACUC protocol.
Participants and evaluations
During anesthesiology residency orientation in July of each year, first-year anesthesiology residents and dental anesthesia residents were invited to participate in our skills lab. Participants first completed a brief questionnaire to assess their prior procedural experiences. Example questions included, “So far in your medical training, how many epidural catheters have you placed?” and “How many chest tubes have you placed?”. Participants next completed a 20-question free-response pre-test the morning of the skills lab. Example questions included, “During bronchoscopy, how do you tell right from left when viewing the carina?” and “Anatomically, what is the last structure traversed before reaching the epidural space?” Following their participation in the skills lab, the participants completed an identical post-test to measure their knowledge gained during the day. All participants completed a course evaluation with criteria rated on a scale of 1 (poor) to 5 (excellent).
Curriculum
We designed our in vivo skills lab curriculum to be presented in multiple modalities to encompass the auditory, visual, and tactile forms of learning. Participants first learned each technical skill during a brief lecture/discussion session. For example, they first watched a brief slide presentation on intercostal nerve blocks, including and overview on the indications, anatomy, and drug dosing, followed by an animation of the procedure itself. They immediately moved on to the animal, where they watched their preceptor perform the skill for them, explaining procedural tips along the way. Finally, the participants performed the technique themselves under the guidance of their preceptor. The single-day course curriculum is shown in Table 1.
Follow-up study
Following institutional review board approval, past in vivo skills lab participants who are current residents in our program provided written informed consent to complete a follow-up survey-based study assessing whether their participation in the skills lab increased their knowledge and confidence in understanding and executing anesthesiology-related procedures.
Statistics
Statistical analyses were performed using GraphPad Prism (GraphPad Software, Inc., San Diego, CA). Where appropriate, data are presented as mean ± SEM and analyzed using a Wilcoxon matched pairs test. p<0.05 was considered significant.
Results
Seventy first-year anesthesiology and dental anesthesia residents have participated in our skills lab (14 per year on average, 2008-2012). While participation was voluntary due to the sensitivity of working with animals, the participation rate was 97.2%. As part of the pre-test assessment prior to the skills lab, participants completed a questionnaire to assess their prior procedural experiences. Only 6 out of 39 participants had placed an epidural catheter prior to attending the skills lab and none had ever performed a retrograde intubation (Figure 1).
Figure 1.
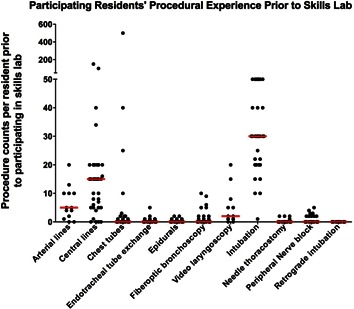
Residents’ mean procedural experience prior to participating in the in vivo skills lab. The data presented shows the participants’ mean self-reported estimation of the number of times they performed a particular procedure prior to participating in the in vivo skills lab (2010-2012 courses). n=39 participants’ responses for all procedures except for arterial line placement (n=13) and video laryngoscopy (GlideScope, n=13). Data is presented as raw procedure count per resident (black dots) and the median procedure count per skill (red line).
To assess their general knowledge of anesthesiology-related topics, participants completed a 20-question pre-test prior to their participation in the skills lab, and then an identical post-test at the conclusion of the course. Prior to their participation in the skills lab, residents’ pre-test scores ranged from 20-80% with a mean score of 50.3 ± 2.6% (Figure 2A). Following their participation in the skills lab, residents’ post-test scores ranged from 45-100%, and the mean score significantly increased to 84.2 ± 1.9%, an overall improvement of 67.5% (p<0.0001). Upon conclusion of the skills lab, all participants complete a course evaluation to provide feedback on the quality of their educational experience. Participants felt that they increased their knowledge and clinical skills from participating in the anesthesiology skills lab (Figure 2B); the significant improvements in their post-test scores are evidence of this. Participants additionally provided written feedback regarding their favorite (Figure 2C) and least-favorite aspect of the skills lab (Figure 2D).
Figure 2.
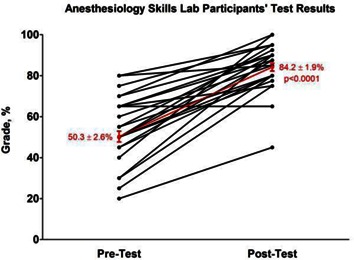

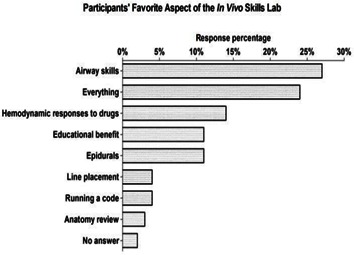
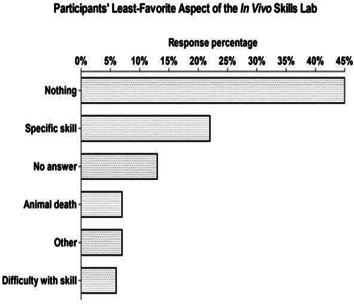
Residents’ test scores and course evaluations. A, data from n=39 residents (2010-2012 courses) demonstrates the improvement in their 20-question assessment tests before and after their participation in the anesthesiology in vivo skills lab. Mean test scores ± SEM is in red. p < 0.0001 via a Wilcoxon matched pairs test. Thirty nine distinct lines are not visible on the graph due to some participants having overlapping pre- and post-test scores; B, the results of course evaluations from n=55-70 participants from 5 skills labs (2008-2012). Criteria were rated on a scale of 1 (poor) to 5 (excellent). Data is presented as the mean ± SEM; C, the results of the participants favorite aspects of the course (n=55 responses); D, the results of the participants least-favorite aspects of the course (n=55 responses).
Past in vivo skills lab participants who are current residents in our program (range PGY-2 through -4) were invited to participate in a follow-up survey-based study assessing whether their participation in the skills lab increased their knowledge and confidence in understanding and executing anesthesiology-related procedures. The mean elapsed time since the respondents (n=22) participated in the animal skills lab was 17.0 ± 2.4 months (range 5-29 months). Respondents reported that the lab was an important part of their residency education, rating the course 4.2 ± 0.2 on a scale from 1 (not important) to 5 (very important). Ninety-one percent would repeat the lab as is and 96% wrote that the lab helped them to gain confidence more quickly with certain procedures. Participants reported that airway techniques and line placement were the most useful techniques to have learned (Figure 3). All of the respondents reported that participating in the in vivo skills lab allowed them to perform procedures that they may never encounter again during residency training. Sixty-eight percent reported that they would be interested in attending a procedure-specific in vivo lab (100% of those respondents specified a surgical airways lab) and 77% would pay to attend an in vivo skills lab course for CME credit during their post-graduate years.
Figure 3.
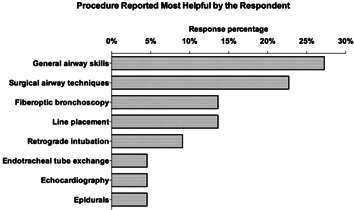
Anesthesiology in vivo skills lab procedures reported most helpful by the respondents. Anesthesiology residents who had participated in past skills labs were invited to complete a follow-up survey on their course experience and were asked to list the procedure they felt was most helpful to for them to have learned during their training. n=22 responses.
Survey respondents provided an estimation of the number of each procedure they had performed to date as a resident (Figure 4A). They self-evaluated their present confidence level (at the time of survey completion) in each procedure on a scale from 1 (little confidence) to 5 (very confident) (Figure 4B) and estimated how much of that confidence is attributed to participating in the skills lab on a scale from 1 (a little) to 5 (a lot) (Figure 4C). PGY-2 residents had an overall lower confidence in their ability to perform procedures compared to the PGY-3 and-4 classes, most likely due to being earlier in their training and less-experienced. Confidence in performing the majority of skills progressively increased from the PGY-2 through -4 classes. Despite reporting very little confidence in advanced airway skills, all 3 residency classes attributed a greater amount of the confidence they had to their participation in the skills lab, presumably since the skills lab provided them with the only opportunity to perform these techniques in an in vivo setting. Interestingly, the PGY-2 class reported a 19% greater confidence in their ability to perform a surgical airway than the PGY-4 class. This finding may be attributed to the PGY-2 class being temporally closer to their participation in the in vivo skills lab and thus maintaining a better retention of surgical airway skills than the PGY-4 class.
Figure 4.
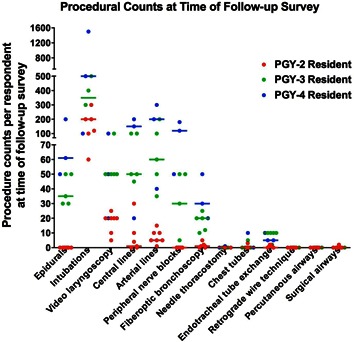
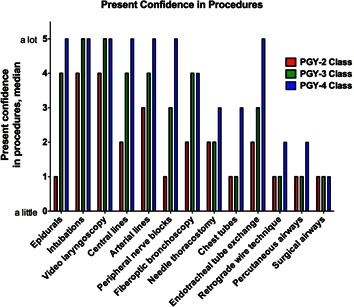
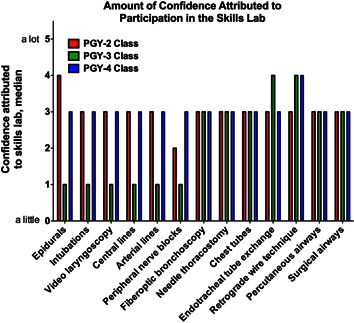
Procedural experience, confidence, and confidence attributed to the in vivo skills lab. A, the results of a follow-up survey showing survey respondents’ estimated total number of procedures performed clinically at the date of the survey; B, self-reported present confidence in performing anesthesiology-related procedures C, the amount of self-reported confidence attributed to participation in the in vivo skills lab. The data is broken down by PGY class: PGY-2 data (red), PGY-3 data (green), and PGY-4 data (blue). n=7 PGY-2, n=5 PGY-3, and n=7 PGY-4 respondents. Data is presented as A, procedure counts per resident (colored dots) and median procedure count per class per skill (colored bar); B and C, median response by PGY class.
Discussion
Anesthesiology residency training currently utilizes varied curricula outside of the clinical arena to improve cognitive and technical skills and accelerate acquisition of new skills. As residency programs adjust to work hour restrictions and training requirements that take residents out of the ORs, innovative methods of training have become critical to residency education. In a single day, an in vivo skills lab experience may provide a new resident with the opportunity to perform a number of high-risk procedures that would otherwise take months or years to encounter in the OR. Modern residency training also emphasizes the need for patient safety. Respectful use of animal models in the education environment allows trainees to make mistakes the first time they do a difficult procedure without exposing a patient to additional morbidity. These concepts have been recognized by the American College of Graduate Medical Education (ACGME) by making simulated patient experiences a yearly requirement for all accredited anesthesiology residency programs. In addition to our skills lab, our residents participate in 4-5 three hour sessions of computer-assisted patient simulation each year, and new PGY-2 residents additionally receive at least 7-10 hours of simulation training during their first month. These experiences also provide an opportunity for teaching and evaluation of the ACGME core competencies.
Airway management is a critical skill and a target of specialized rotations in anesthesiology. Pott et al14 surveyed anesthesiology residency programs in the US and Canada and reported that 49% of the respondents’ programs offered an airway rotation. Hagberg et al15 found that 33% of survey respondents’ programs provided a difficult airway rotation. Holak et al16 reported that 88% of survey respondents’ programs provided surgical airway training. The opportunity for anesthesiology residents to obtain hands-on practice performing difficult airway techniques as early in their careers as possible is invaluable: in a survey of anesthesiology chief residents,13 53% of the respondents participated in 10 or fewer airway emergencies and 92% never performed a surgical airway (median = 0, none had performed more than 2). The results of our participant follow-up survey were comparable: 96% of respondents had never performed a surgical airway clinically (median = 0, one person had performed 2). These data demonstrate that anesthesiology residents have limited opportunities during their training to experience airway emergencies and develop proficiency with difficult airway techniques; thus alternate means of exposure are warranted.
Developing the course curriculum
Our skills lab curriculum (Table 1) is presented in multiple modalities to encompass the auditory, visual, and tactile forms of learning. The order in which the skills are presented is critical for maximizing educational benefits of the model. Our curriculum begins with the least-invasive procedures and those least-likely to result in serious complications or death, proceeds through skills with the potential for greater complications, and concludes with the highest-risk procedures. Some of the techniques can be performed multiple times by each participant, and since the participants are paired they are able to watch and learn from each other’s attempts. The role of the preceptors is to provide formative assessment and immediate intervention to remediate procedural and knowledge-gap errors. In the event of serious complications, the participants run a code and use their crisis-management skills during resuscitation. At the end of the course after the animals have been euthanized, participants perform a thoracotomy to review thoracic and cardiac anatomy.
Table 1.
Anesthesiology In Vivo Skills Lab Curriculum.
| Introduction: |
| Basics of respiration and ventilation |
| Overview of anesthetic machines and ventilators |
| Refresher on basic anesthetic principles and monitoring |
| Regional Anesthesia Module: |
| Epidural and spinal placement |
| Review anatomy and kit contents |
| Place epidural catheters using kit provided |
| Perform lumbar puncture |
| Place lumbar paravertebral nerve block |
| Peripheral nerve block |
| Review equipment and anatomy |
| Stimulate the sciatic nerve |
| Block response with lidocaine provided |
| Intercostal nerve block |
| Review anatomy and identify ribs |
| Perform intercostal block |
| Thoracic Module: |
| Needle thoracostomy |
| Review anatomy and identify ribs |
| Perform thoracostomy (may create a pneumothorax) |
| Chest tube placement |
| Review pneumothorax and indications |
| Review anatomy and identify ribs |
| Place chest tube and secure with suture |
| Hemodynamics Module: |
| Central line and pulmonary artery (PA) catheter placement |
| Review anatomy and kit components |
| Set up and zero pressure transducer |
| Access femoral vein (percutaneously or via cut-down) |
| Place central venous catheter using kit provided |
| Exchange with an introducer kit over a wire |
| Place PA catheter and review waveforms |
| Arterial line placement |
| Review anatomy and kit components |
| Set up and zero pressure transducer |
| Access femoral artery (percutaneously or via cut-down) |
| Place arterial line using kit provided |
| Review hemodynamics |
| Mystery pharmacology |
| Administer drugs (provided) |
| Assess waveforms and hemodynamic responses |
| Identify drugs and review mechanisms of action |
| Airway Module: |
| Video laryngoscopy |
| Review indications and equipment |
| Perform laryngoscopy |
| Laryngeal mask airway (LMA) |
| Review indications and equipment |
| Place LMA |
| Fiberoptic bronchoscopy |
| Review anatomy and equipment |
| Drive bronchoscope and identify anatomy |
| Perform left bronchial blocker placement |
| Observe alterations in vital signs and perform auscultation |
| Endotracheal tube exchange |
| Review supplies and procedure |
| Exchange endotracheal tube using guide provided |
| Retrograde intubation |
| Review indications and anatomy |
| Review supplies and procedure |
| Perform retrograde intubation |
| Percutaneous airway |
| Review indications and anatomy |
| Review supplies and procedure |
| Extubate and perform percutaneous airway |
| Surgical airway |
| Review indications and anatomy |
| Review supplies and procedure |
| Perform surgical airway and intubate |
| Anatomy Module (following lab completion): |
| Thoracic anatomy |
| Perform left thoracotomy |
| Review anatomy and identify structures |
| Cardiac anatomy |
| Review anatomy and identify structures |
Personnel
Communication between the skills lab director(s), residency program director, and animal staff is critical to the success of the course. Our skills lab is designed and co-directed by two members of the anesthesiology department (authors GM and MG). The course directors work closely with the residency program director (author KM) on resident participation and scheduling. Five to seven attending anesthesiologists volunteer as preceptors and oversee their group of 2-3 residents during the entire course. A veterinarian and several animal technicians perform pre-operative preparations of the animals and assist with intra-operative monitoring and course clean-up.
Resources
An in vivo skills laboratory must be held in an appropriate facility accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International (AAALAC). The animal protocol must conform to the statutes of the Animal Welfare Act and the guidelines of the Public Health Service as issued in the Guide for the Care and Use of Laboratory Animals (NIH Publication No. 85-23, revised 1996) and receive institutional approval by the Institutional Animal Care and Use Committee (IACUC). Pigs are optimal for our curriculum in terms of their anatomic and hemodynamic similarities to humans.10,17 Their large size is more conducive to the performance of multiple procedures and allows the use of human-sized supplies, and they are relatively low cost.
Limitations
The use of anesthetized animals in residency education is a sensitive topic and warrants thorough analysis of need and consideration of alternative training methods to accomplish curriculum goals.18 The presence of an appropriate facility to support the course is another potential limitation to in vivo training. Finally, the costs associated with holding a skills lab must be evaluated. While surgery residency programs are required by the ACGME to provide a skills laboratory,19 skills laboratories in anesthesiology are at the discretion of the department: only 7.9% of anesthesiology chief residents surveyed used an animal lab for practicing airway emergencies.13 Obtaining education grants and partnering with private industry helps to offset the costs of supplies and specialized equipment.
In summary, an anesthesiology in vivo skills lab is an effective and well-received educational opportunity for anesthesiology residents. It provides them with the opportunity to gain hands-on experience performing anesthesiology-related procedures under the guidance of attending anesthesiologists in a low-pressure environment where mistakes are permissible and result in immediate feedback. As a complement to procedural skills, cognitive challenges encompassing teamwork, decision-making skills, and crisis-management skills during complications collectively enrich resident confidence. This innovative educational experience can assist residency programs to adequately train residents, fulfill ACGME requirements, and assess core competencies with the goal of improving patient safety as residents segue into patient care.
Acknowledgements, Disclaimers
Acknowledgements: The authors would like to thank the staff of University Laboratory Animal Resources at The Ohio State University for their assistance during the skills laboratories and Thomas J. Papadimos, MD for his helpful suggestions.
Sources of funding: This study was supported by the Department of Anesthesiology at The Ohio State University Wexner Medical Center. The in vivo skills labs were supported in part by the Department of Anesthesiology at The Ohio State University Wexner Medical Center, B. Braun Medical Inc., Cook Medical Inc., Covidien, Olympus America Inc., Teleflex Medical, Verathon Inc., and through education grants from Teleflex Medical.
Financial disclosures and potential conflicts of interest: None.
Financial support: This study was supported by the Department of Anesthesiology at The Ohio State University Wexner Medical Center. The in vivo skills labs were supported in part by the Department of Anesthesiology at The Ohio State University Wexner Medical Center, B. Braun Medical Inc., Cook Medical Inc., Covidien, Olympus America Inc., Teleflex Medical, Verathon Inc., and through education grants from Teleflex Medical.
References
- 1.Murray DJ. Current trends in simulation training in anesthesia: a review. Minerva Anestesiol. 2011;77:528–33. [PubMed] [Google Scholar]
- 2.Hatton KW, Price S, Craig L, Grider JS. Educating anesthesiology residents to perform percutaneous cricothyrotomy, retrograde intubation, and fiberoptic bronchoscopy using preserved cadavers. Anesth Analg. 2006;103:1205–8. doi: 10.1213/01.ane.0000237328.94837.62. [DOI] [PubMed] [Google Scholar]
- 3.Urman RD, Sarin P, Mitani A, et al. Presence of anesthesia resident trainees in day surgery unit has mixed effects on operating room efficiency measures. Ochsner J. 2012;12:25–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Naik VN, Matsumoto ED, Houston PL, et al. Fiberoptic orotracheal intubation on anesthetized patients: do manipulation skills learned on a simple model transfer into the operating room? Anesthesiology. 2001;95:343–48. doi: 10.1097/00000542-200108000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Nyssen AS, Larbuisson R, Janssens M, et al. A comparison of the training value of two types of anesthesia simulators: computer screen-based and mannequin-based simulators. Anesth Analg. 2002;94:1560–65. doi: 10.1097/00000539-200206000-00035. [DOI] [PubMed] [Google Scholar]
- 6.Lampotang S. Computer and web-enabled simulations for anesthesiology training and credentialing. J Crit Care. 2008;23:173–78. doi: 10.1016/j.jcrc.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Barrington MJ, Wong DM, Slater B, et al. Ultrasound-guided regional anesthesia: how much practice do novices require before achieving competency in ultrasound needle visualization using a cadaver model. Reg Anesth Pain Med. 2012;37:334–39. doi: 10.1097/AAP.0b013e3182475fba. [DOI] [PubMed] [Google Scholar]
- 8.Cummings AJ, Valentini J, Getz MA. Use of a novel animal prototype to teach advanced airway management skills. Teach Learn Med. 2005;17:63–8. doi: 10.1207/s15328015tlm1701_11. [DOI] [PubMed] [Google Scholar]
- 9.Woodall NM, Harwood RJ, Barker GL. Complications of awake fibreoptic intubation without sedation in 200 healthy anaesthetists attending a training course. J Anaesth. 2008;100:850–55. doi: 10.1093/bja/aen076. [DOI] [PubMed] [Google Scholar]
- 10.Custalow CB, Kline JA, Marx JA, Baylor MR. Emergency department resuscitative procedures: animal laboratory training improves procedural competency and speed. Acad Emerg Med. 2002;9:575–86. doi: 10.1111/j.1553-2712.2002.tb02294.x. [DOI] [PubMed] [Google Scholar]
- 11.Traxer O, Gettman MT, Napper CA, et al. The impact of intense laparoscopic skills training on the operative performance of urology residents. J Urol. 2001;166:1658–61. [PubMed] [Google Scholar]
- 12.La Torre M, Caruso C. Resident training in laparoscopic colorectal surgery: role of the porcine model. World J Surg. 2012;36:2015–20. doi: 10.1007/s00268-012-1675-0. [DOI] [PubMed] [Google Scholar]
- 13.Andrews JD, Nocon CC, Small SM, et al. Emergency airway management: Training and experience of chief residents in otolaryngology and anesthesiology. Head Neck. 2012;34:1720–26. doi: 10.1002/hed.21998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pott LM, Randel GI, Straker T, et al. A survey of airway training among U.S. and Canadian anesthesiology residency programs. J Clin Anesth. 2011;23:15–26. doi: 10.1016/j.jclinane.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 15.Hagberg CA, Greger J, Chelly JE, Saad-Eddin HE. Instruction of airway management skills during anesthesiology residency training. J Clin Anesth. 2003;15:149–53. doi: 10.1016/s0952-8180(02)00503-2. [DOI] [PubMed] [Google Scholar]
- 16.Holak EJ, Kaslow O, Pagel PS. Who teaches surgical airway management and how do they teach it? A survey of United States anesthesiology training programs. J Clin Anesth. 2011;23:275–79. doi: 10.1016/j.jclinane.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Forbes RB, Murray DJ, Albanese MA. Evaluation of an animal model for teaching fibreoptic tracheal intubation. Can J Anaesth. 1989;36:141–44. doi: 10.1007/BF03011436. [DOI] [PubMed] [Google Scholar]
- 18.Cheong J. The use of animals in medical education: a question of necessity vs. desirability. Theor Med. 1989;10:53–57. doi: 10.1007/BF00625759. [DOI] [PubMed] [Google Scholar]
- 19.Berg DA, Milner RE, Fisher CA, et al. A cost-effective approach to establishing a surgical skills laboratory. Surgery. 2007;142:712–21. doi: 10.1016/j.surg.2007.05.011. [DOI] [PubMed] [Google Scholar]


