Abstract
Objective
Examine the effect of a multi-component office ergonomics intervention on visual symptom reductions.
Methods
Office workers were assigned to either a group receiving a highly adjustable chair with office ergonomics training (CWT), a training-only group (TO) or a control group (C). A work environment and health questionnaire was administered 2 and 1 month(s) pre-intervention and 3, 6, and 12 months post-intervention. Multi-level statistical models tested hypotheses.
Results
The CWT intervention lowered daily visual symptoms (p < 0.01) post-intervention. The TO group did not significantly differ from the control group. The CWT group differed significantly from the TO group (p = 0.01) post-intervention.
Conclusion
Workers who received a highly adjustable chair and office ergonomics training had reduced visual symptoms and the effect was maintained through twelve months post-intervention. The lack of a training-only group effect supports implementing training in conjunction with the highly adjustable chair to reduce visual symptoms.
Keywords: Office ergonomics intervention, Visual symptoms, Multi-level modeling
1. Introduction
Among office workers, visual symptoms of eyestrain, stinging and burning eyes are often found to be prevalent (Collins et al., 1991; Dain et al., 1988; Salibello and Nilsen, 1995; Smith et al., 1981). Despite the relationship between visual symptoms and computer use (Bergqvist et al., 1992; Bergqvist and Knave, 1994; Dainoff et al., 1981; Knave et al., 1985; Mocci et al., 2001; Rocha and Debert-Riberiro, 2004), little intervention research exists demonstrating how best to design and build offices to reduce visual symptoms (Aaras et al., 1998, 2001, 2005; Dainoff et al., 2005a, 2005b; Horgen et al., 2004, 2005; Konarska et al., 2005). The office ergonomic intervention literature contains few well-designed interventions (NRC, 2001; Brewer et al., 2006). Only Aaras et al. (1998, 2001) and Horgen et al. (2004) report on visual symptom changes resulting from both lighting changes and the use of corrective lenses. In a knowledge economy with growing numbers of workers using computers, visual strain can affect performance and overall workforce productivity (Daum et al., 2004).
A large-scale intervention study was implemented in two US work places to examine the health consequences of providing workers with office ergonomics training and/or a new highly adjustable chair (Amick et al., 2003). The chair coupled with training resulted in reduced musculoskeletal symptom growth over the workday (Amick et al., 2003) and increased worker productivity by 17% (DeRango et al., 2003). In Norway work places, Aaras et al. (1998, 2001) and Horgen et al. (2004) documented a relationship between musculoskeletal symptoms, EMG activity and visual symptoms suggesting interventions designed to improve musculoskeletal health may also affect visual health.
We hypothesized receiving a new highly adjustable chair and office ergonomics training reduces worker visual symptoms at the end of the workday compared to workers who only receive training and workers in a control group. Workers who only receive training will have reduced visual symptoms at the end of the workday compared to workers in a control group. Similarly, we hypothesized the intervention reduces visual symptom growth over the workweek.
2. Methods
2.1. Study design
Three groups of workers participated in a 16 month study: a control group (C – which received the office ergonomics training at the end of the study), a training-only group (TO – which received only the office ergonomics training intervention) and a chair-with-training group (CWT – which received both an office ergonomics training and a new highly adjustable chair). Workers completed two pre-intervention work environment and health questionnaires at two months and one month prior to intervention. Following the second measurement period the interventions were implemented. Workers completed follow-up work environment and health questionnaires at three, six and twelve months post-intervention. Visual symptoms data was collected using a symptoms diary administered at the end of each workday for one week as part of a daily musculoskeletal symptom diary that was administered 2 months and 1 month prior to intervention and again 3, 6, and 12 months post-intervention. If less than 80% of the information was present, workers were asked to complete a second week. All data was collected via the Internet. The Liberty Mutual Research Institute for Safety Human Subjects IRB approved the study protocol.
Group assignment was non-random. Geographic separation between groups rather than individual-level randomization was conducted, because of the potential for communication of ergo-nomic knowledge between the intervention group participants and the control group participants.
2.2. Intervention
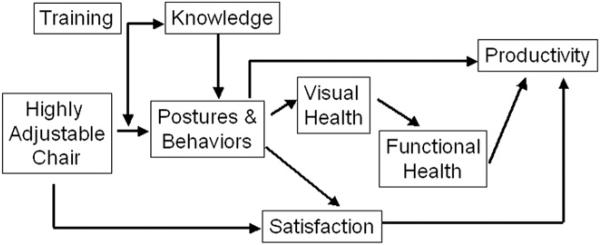
Fig. 1 displays the a priori theory of change guiding the research (Amick et al., 2003). The office ergonomics training was expected to increase knowledge and with the new highly adjustable chair (see Fig. 2) reduce postural risks and encourage healthy computing behaviors (e.g., taking frequent rest breaks, adjusting monitor height). Furthermore, it was hypothesized the new chair coupled with training would more significantly reduce postural risk and behaviors (e.g., dynamic movement in the chair while working, making adjustments to optimize gaze height) than training alone (Robertson et al., 2009). Moreover, these behavioral and postural changes should increase productivity directly and indirectly through health improvement.
Fig. 1.
Theory of change.
Fig. 2.
Highly adjustable chair.
The office ergonomics training was designed following instructional systems design principles and based on adult learning theories (Robertson et al., 2002, 2009). The training was developed specifically for use in the organization where the intervention was implemented. The 90-min training workshop included PowerPoint presentations, an office ergonomics video, problem solving exercises and hands on training for chair (all workers brought their own chairs) and workstation adjustment. Twenty-two training workshops (with attendance varying from 1 to 24) were conducted by two trained facilitators. All supervisors participated in the training.
The highly adjustable chair used in this study was designed to improve worker fit to his or her office workspace (Bush and Hubbard, 1999; Faiks and Allie, 1999). Key design features include arm rests that have height, lateral location and pivot adjustability, a full dynamic back support with both upper and lower back adjustability, adjustable seat depth, and a dynamic gliding mechanism allowing the user to recline in the seat without significantly pulling away from his or her working position. That is, the seated worker's hands should not have to move away from the keyboard and the worker is able to maintain his or her line of sight with the screen. This would minimize any changes in the worker's viewing angle.
2.3. Study sample
Participants had Internet access and worked in sedentary, computer-intensive office jobs, requiring at least 4 h per day of computing time and at least 6 h per day of sitting in an office chair. Subjects were excluded if they had filed a workers’ compensation claim within the past six months. All workers were public sector workers in a single department whose jobs involved collecting tax revenues.
2.4. Outcome measures
Participants were asked whether any of 11 visual symptoms (stinging, itching, feeling gritty, becoming red, tearing, feeling dry, burning, aching, feeling sensitive to light, blurry vision, difficulty focusing) were present (Kuorinka and Forcier, 1995; NIOSH, 1981). The visual symptoms scale was a count of all symptoms experienced and ranged from 0 (no symptoms at all) to 11 (all 11 symptoms present). If information was missing on any one question the scale was set to missing. The visual symptoms scale had an average Cronbach's alpha of 0.98 across the five survey rounds (range, 0.96–0.99).
2.5. Covariate selection
Data collected on thirty-four potential covariates were categorized as physical demands, psychosocial work environment, workstation factors, health factors, and demographics. Potential confounders were included in the model if, (1) they demonstrated an association with the outcome variable pre-intervention, (2) they were not highly correlated with other confounders pre-intervention, (3) they were not evenly distributed between the study groups either pre-intervention or post-intervention, and (4) the observed differences between the groups were substantively meaningful pre-intervention or post-intervention. The first two conditions were assessed by identifying significant associations with the outcome (Pearson's correlation, p ≤ 0.05) and absence of a strong correlation with other confounders (r > 0.65). When high correlations existed, the confounder with the higher correlation with the outcome variable was chosen. Between-study group heterogeneity (condition three) was assessed for each time-varying continuous variable by using a two-level variance components model with the confounder as the outcome and study groups, intervention and study group by intervention interactions as predictors. A joint chi-square statistic was used to determine if there was a significant difference (at p ≤ 0.10) between the study groups pre- or post-intervention. Study group heterogeneity for time-invariant continuous variables was assessed by one-way ANOVA. Heterogeneity between study groups for dichotomous variables was determined by cross-sectional time series logistic regression modeling. All confounders meeting inclusion criteria 1–3 were placed into a multi-level model and a stepwise backwards selection procedure was followed. Those not significantly decreasing the model log likelihood (p > 0.20) were removed.
The research team considered the substantive contribution of each covariate satisfying conditions 1–3 with the goal of developing a robust and readily interpretable model. Each candidate covariate was examined and, if possible, criteria for conceptually meaningful differences were established. When no conceptual difference could be established, a statistical difference of one standard deviation based on the sample distribution was used.
2.6. Statistical analysis
A multi-level linear model was developed to test hypotheses that included terms to describe study group assignment and application of intervention, random terms to account for the study design's hierarchical structure and terms to account for potential confounding (Rasbash et al., 2000).
The multi-level statistical model shown in the following equation was formed by including the covariates as described above, two dummy variables, one for each of the two intervention groups (control group is the referent), a variable indicating study phase (0 = pre-intervention, 1 = post-intervention) and the two two-way interaction terms for these variables. The two levels in this model are occasion of measurement (Level 1) and subject (Level 2). Each subject who responded to symptoms surveys every day for all five time periods (2 pre-intervention and 3 post-intervention) would have 25 occasions of measurement. The resulting model has the form,
where yij = visual symptom score on the ith occasion for the jth subject, β0 = overall mean for the control group, β1 = differential effect of membership in CWT group, β2 = differential effect of membership in TO group, β3 = differential effect of intervention, β4 = effect of receiving the CWT intervention, β5 = effect of receiving the TO intervention, (covariates) denotes terms correcting for selected covariates, uj = deviation due to jth subject, εij = deviation due to ith occasion of measurement within the jth subject and chairij = 1 if jth subject assigned to “chair” on ith occasion, = 0 otherwise, trainingij = 1 if jth subject assigned to “training” on jth occasion, = 0 otherwise, chair*trainingij, chair*interventionij and training*interventionij = interaction terms formed by multiplication.
It was assumed (subject to verification) that the random variables uj and εij are independently normally distributed each with mean 0 and variances and , respectively.
The two-way interaction term chair*intervention describes post-intervention changes in visual symptoms in the CWT group compared to the control group, the two-way interaction training*intervention describes post-intervention changes in visual symptoms in the TO group relative to the control group. The difference between the two two-way interaction terms describes the difference in post-intervention changes in the CWTgroup and the TO group. The Wald Z statistics for the two-way interaction terms are used to test the main hypotheses. A joint chi-square statistic is used to test the difference between the CWT and TO groups.
For each model, levels 1 and 2 residual analyses were performed to determine if distributional assumptions were violated or if systematic variation existed in the residuals. For each model developed, level 1 and level 2 residuals did not demonstrate appreciable deviation form normality and appeared to be free of unwanted patterns. The multi-level models were fitted using MLWIN 1.1 and all other analyses were carried out with STATA 7 (MLwiN, 2001; StataCorp, 2001).
In preliminary analyses, we considered whether visual symptoms grew over the workweek by plotting mean visual symptoms scores by workweek for both pre-intervention periods. There was no noticeable growth over the workweek. Instead, on average, symptoms declined over the week (βdayofweek = −0.27, z = 4.47, p < 0.001). Upon further inspection, there were no discernable patterns across the days of the week. Given the absence of any pre-intervention growth over the workweek in visual symptoms no further hypothesis testing was considered necessary. (All analyses are available from the first author.)
3. Results
Three hundred and sixteen employees were invited to participate. Two hundred and sixteen completed electronic informed consent (69% participation rate). Eleven part-time employees and 21 with incomplete Daily Symptoms Survey data were excluded, leaving 184 participants at baseline. The chair-with-training group was the largest of the three groups, with a high of 78 subjects and a low of 74, the training-only and control group highs were 51 and 48 and lows were 46 and 40, respectively. The number of participants in each group varied over time (Table 1). At 12 months post-intervention, 161 participants completed the questionnaire (88% retention). The mean age was 47, 60% of the participants were female, nearly all (92%) were white or Caucasian, and the average time spent in an office chair computing was 5–6 h per day.
Table 1.
Number of participants/completed visual symptom surveysa by intervention group and measurement period.
| Measurement Periodb |
|||||
|---|---|---|---|---|---|
| Pre-Intervention |
Post-Intervention |
||||
| Intervention Group | 1 | 2 | 3 | 4 | 5 |
| Chair & Training (n = 79) | 78/325 | 78/315 | 77/329 | 74/294 | 75/301 |
| Training-Only (n = 55) | 51/202 | 51/202 | 50/205 | 49/181 | 46/186 |
| Control n = 50) | 48/188 | 47/170 | 44/158 | 46/170 | 40/164 |
One participant responding every day for every period has 25 completed surveys.
Periods 1 and 2 are pre-intervention and 3–5 are post-intervention.
Only 10 participants (less than 5% of study size) completed no surveys post-intervention. Comparing intervention group means at pre-intervention of four selected confounders (general health, time spent at computer, lighting is comfortable, and chair comfort) revealed no significant differences between participants who participated post-intervention and those who did not. However, there was a greater proportion of those lost to follow-up who did not wear eyeglasses (50%) compared with those who continued in the study (21%).
Data on thirty-four potential covariates were examined for inclusion. Physical demands included hours spent sitting in office chair per week, hours spent working at an office computer per week, total computer use, number of breaks taken per week, repetitive hand and wrist activity, and force used with hands and wrist in office. Workstation factors measured were workstation layout, level of lighting glare, level of noise distraction, workplace privacy satisfaction level, chair comfort and chair satisfaction. Psychosocial work conditions examined were skill use at work, authority at work, decision latitude at work, psychological demands at work, job demands preventing rest breaks and social support. Health factors examined were body mass index, general health, medication taken for pain, medication strength, exercise to relieve pain, and type of eyeglasses lenses worn. Demographic measures included age, job level, education level, job tenure, gender, disability status, marital status, number of persons living in household, and racial/ethnic background.
After satisfying conditions 1–3 of the covariate selection process, seven potential covariates remained, computer use in a typical day, force used with hands/wrists, psychological job demands, lighting produces a lot of glare, satisfaction of privacy of workplace, chair comfort, and eyeglasses lens type. To develop a robust and readily interpretable multivariable model, the four most prominent confounders were retained (condition 4). Two variables (lighting produces a lot of glare and type of lenses worn) were selected because of their direct impact on vision. Hours spent working on the computer in a typical day were also included because of their confounding effect in the same study testing a different health outcome. Finally, chair comfort was included because there were substantively significant differences in mean values across study phases for each group. Three were dropped because observed differences between groups pre- and post-intervention were considered substantively trivial. Table 2 shows the overall mean and means by study phase and group for the four confounders meeting all inclusion criteria.
Table 2.
Distribution of covariates and outcome by intervention period and intervention group.f
| Intervention Period |
|||||
|---|---|---|---|---|---|
| Pre |
Post |
||||
| 1 | 2 | 3 | 4 | 5 | |
| Daily hours worked at office computera (mean & SD) | |||||
| CWT | 3.27 (0.69) | 3.16 (0.78) | 3.02 (0.84) | 3.21 (0.76) | 3.21 (0.70) |
| TO | 3.08 (0.73) | 2.98 (0.84) | 2.89 (0.84) | 2.82 (0.72) | 2.85 (0.76) |
| Control | 3.20 (0.80) | 3.27 (0.71) | 3.26 (0.68) | 3.25 (0.82) | 3.44 (0.72) |
| Chair comfortb (mean & SD) | |||||
| CWT | 2.52 (0.55) | 2.44 (0.45) | 3.13 (0.42) | 3.17 (0.47) | 3.12 (0.39) |
| TO | 2.63 (0.72) | 2.63 (0.70) | 2.90 (0.49) | 2.94 (0.41) | 2.89 (0.52) |
| Control | 2.58 (0.42) | 2.50 (0.53) | 2.69 (0.52) | 2.75 (0.46) | 2.77 (0.46) |
| Type of lenses wornc (%) | |||||
| None | |||||
| CWT | 18 | 16 | 13 | 20 | 20 |
| TO | 22 | 21 | 16 | 14 | 19 |
| Control | 30 | 24 | 35 | 36 | 32 |
| Single | |||||
| CWT | 39 | 40 | 40 | 37 | 30 |
| TO | 41 | 35 | 37 | 45 | 34 |
| Control | 39 | 38 | 38 | 38 | 35 |
| Bi- or trifocal | |||||
| CWT | 42 | 44 | 47 | 43 | 49 |
| TO | 37 | 43 | 48 | 41 | 47 |
| Control | 31 | 38 | 27 | 26 | 33 |
| Lighting produces glared (mean & SD) | |||||
| CWT | 2.61 (0.66) | 2.65 (0.67) | 2.80 (0.62) | 2.71 (0.64) | 2.71 (0.68) |
| TO | 2.32 (0.80) | 2.44 (0.76) | 2.54 (0.72) | 2.66 (0.56) | 2.70 (0.49) |
| Control | 2.61 (0.53) | 2.59 (0.64) | 2.69 (0.51) | 2.55 (0.69) | 2.43 (0.72) |
| Visual symptoms scoree (mean & SD) | |||||
| CWT | 2.05 (2.33) | 2.03 (2.49) | 1.38 (2.13) | 1.37 (2.21) | 1.24 (2.36) |
| TO | 2.01 (2.16) | 1.32 (1.78) | 1.48 (1.79) | 1.39 (2.04) | 1.14 (1.66) |
| Control | 2.71 (2.56) | 2.48 (2.64) | 2.37 (2.73) | 2.35 (2.83) | 2.65 (3.25) |
Number of hours worked at office computer in a typical day ranges from 0 (0 h) to 5 (>9 h).
Chair is comfortable ranges from 1 indicating strongly disagree to 4 indicating strongly agree.
Type of lenses worn is defined by none, single-vision, or bi/trifocal lenses.
Lighting produces glare varies from 1 indicating strongly agree to 4 indicating strongly disagree.
Visual symptoms range from 0 representing no visual symptoms to 11 representing having all visual symptoms listed. Visual symptoms are averaged over the week(s) for each reporting period.
CWT refers to the chair-with-training group and TO refers to the training-only group.
Visual symptoms are higher in the control group pre-intervention but remain relatively stable over time. In both CWT and TO groups the level of visual symptoms dropped after intervention.
Table 3 shows the multi-level model results. Model 2 differs from Model 1 including the two two-way interaction terms for hypothesis testing. The difference in log likelihoods between Models 2 & (, p = 0.001) suggests the two hypothesized effects improve model fit. Model 2 shows the CWT group experienced a statistically significant reduction in visual symptoms post-intervention compared with the control group (βchair*intervention = −0.49, z = 3.3, p < 0.001). The TO group did not experience a significant reduction in visual symptoms post-intervention compared with the control group (βtraining*intervention = −0.13, z = 0.77, p = 0.44). The CWT differs significantly from the TO group (, p = 0.01).
Table 3.
Multi-level model including and excluding main effect parameters.
| Variable | Model 1 (Std. Error) | Model 2 (Std. Error) |
|---|---|---|
| Time spent in office chair | 0.26 (0.06)* | 0.25 (0.06)* |
| Lighting produces glare on screen | –0.40 (0.07)* | –0.39 (0.08)* |
| Chair comfort | –0.63 (0.08)* | –0.55 (0.08)* |
| Type of glasses, single-vision | –0.48 (0.18)* | –0.52 (0.18)* |
| Type of glasses, bi/trifocals | –0.66 (0.20)* | –0.66 (0.20)* |
| β1, Chair-and-training group | –0.67 (0.30)* | –0.39 (0.31)ns |
| β2, Training-only group | –0.88 (0.33)* | –0.82 (0.34)* |
| β3, Intervention phase | –0.06 (0.07)ns | 0.18 (0.12)ns |
| β4, Chair*intervention | – | –0.49 (0.15)* |
| β5, Training*intervention | – | –0.13 (0.17)ns |
| β0, Intercept term | 1.71 (0.44) | 1.77 (0.45) |
| εij, Level 1 variance | 2.48 (0.07) | 2.47 (0.07) |
| uj, Level 2 variance | 2.56 (0.29) | 2.58 (0.29) |
| Model –2 ln (likelihood) | 12068.01 | 12055.61 |
| Difference in –2 ln (likelihoods) = 12.40* | ||
p < 0.05
p > 0.05.
Whether the intervention effect was time dependent was examined by considering each time period separately. At three months post-intervention, both the CWT group and the TO group did not differ from the control group (βchair*intervention = −0.35, z = 1.59, p = 0.11; βtraining*intervention = 0.08, z = 0.35, p = 0.72). However, the CWT group did differ from the TO group (, p = 0.03). At 6 months post-intervention, both the CWT and TO groups were not statistically different from the control group (βchair*intervention = −0.20, z = 1.00, p = 0.32; βtraining*intervention = 0.13, z = 0.56, p = 0.57) nor were they different from each other (, p = 0.10). At 12 months post-intervention, the CWT group different from the control group (βchair*intervention = −0.67, z = 3.19, p = 0.001), while the TO group did not (βtraining*intervention = −0.30, z = 1.28, p = 0.20). Furthermore, the CWT group differed from the TO group (, p = 0.02). At all three post-intervention time points the CWT effect was in the hypothesized direction (negative), while only at 12 months was the TO group effect in the hypothesized direction.
Finally, we inspected each visual symptom independently to determine whether one or two symptoms were responsible for the overall effect. Considering average pre- and post-symptom values, the largest differences were for eyes ‘becoming red’, ‘burning’, ‘aching’, and ‘feeling sensitive to light’. ‘Blurry vision’ and ‘feeling gritty’ were the two visual symptoms least responsive to the interventions as shown in Table 4.
Table 4.
Distribution of each visual symptom by intervention period.a
| Intervention Period |
|||||
|---|---|---|---|---|---|
| Pre |
Post |
||||
| 1 | 2 | 3 | 4 | 5 | |
| Stinging | 0.16 (0.37) | 0.12 (0.33) | 0.12 (0.33) | 0.12 (0.32) | 0.11 (0.32) |
| Itching | 0.18 (0.39) | 0.19 (0.39) | 0.15 (0.36) | 0.14 (0.35) | 0.17 (0.37) |
| Feeling gritty | 0.18 (0.38) | 0.17 (0.37) | 0.16 (0.37) | 0.14 (0.35) | 0.16 (0.37) |
| Aching | 0.27 (0.45) | 0.22 (0.42) | 0.17 (0.37) | 0.20 (0.40) | 0.17 (0.37) |
| Feeling sensitive to light | 0.32 (0.47) | 0.25 (0.44) | 0.21 (0.41) | 0.22 (0.42) | 0.21 (0.40) |
| Becoming red | 0.14 (0.35) | 0.11 (0.32) | 0.09 (0.28) | 0.11 (0.31) | 0.07 (0.26) |
| Tearing | 0.08 (0.28) | 0.07 (0.26) | 0.06 (0.24) | 0.05 (0.23) | 0.06 (0.24) |
| Feeling dry | 0.35 (0.48) | 0.33 (0.47) | 0.26 (0.44) | 0.26 (0.44) | 0.25 (0.43) |
| Burning | 0.21 (0.41) | 0.19 (0.39) | 0.15 (0.35) | 0.15 (0.36) | 0.13 (0.34) |
| Blurry vision | 0.16 (0.37) | 0.14 (0.34) | 0.15 (0.36) | 0.14 (0.35) | 0.14 (0.35) |
| Difficulty focusing | 0.21 (0.41) | 0.17 (0.37) | 0.16 (0.36) | 0.15 (0.36) | 0.14 (0.35) |
Mean (standard deviation).
4. Discussion
Visual symptoms have been recognized as a computer-related health problem since the late 1970's (Dainoff et al., 1981; Ostberg, 1975). The US National Academy of Sciences, in Video Displays, Work and Vision, recommended carefully designed research on the visual performance and comfort effects of VDT work (NAS, 1983). Since then, studies have documented a prospective dose–eresponse relationship between computer use and visual symptoms (Bergqvist et al., 1992). Recently Daum showed in a series of experiments that visual discomfort was associated with lost productivity (Daum et al., 2004). Surprisingly, visual symptoms as an outcome in field-based office ergonomic interventions have received little attention (Brewer et al., 2006).
In this office ergonomics intervention study, workers who received a new chair and office ergonomics training reported significant reductions in visual symptoms when compared to either a group that received only the office ergonomics training or a control group. These effects persisted 12 months after the interventions. In economic analyses, the CWT group experienced a 17% productivity increase (DeRango et al., 2003). Previous analyses have shown an improvement in musculoskeletal health for the CWT group (Amick et al., 2003). Workers who received only office ergonomics training did not report reduced visual symptoms, even though our research has shown employees engage in making adjustments to their workspace following training (Robertson et al., 2009). Two other interventions also found no effect on visual symptoms with workstation adjustments without any new technology such as a highly adjustable chair (Psihogios et al., 2001; Ketola et al., 2002). The current visual symptom results support the importance of providing office workers with highly adjustable chairs and appropriate office ergonomics training to improve both musculoskeletal and ocular health and knowledge worker productivity.
The Norwegian office work interventions conducted by Aaras and Horgen showed the importance of improved lighting conditions and optometric corrections in reducing computer-related visual symptoms (Aaras et al., 1998, 2001; Horgen et al., 2004). In contrast with the Norwegian studies, a reduction in musculoskeletal symptoms was our outcome of interest, the reduction in visual symptoms was of secondary analytic importance. Visual symptoms were expected to decrease with both ergonomic training alone and the chair-with-training intervention.
Factors affecting increased visual symptoms among VDT users include VDT displays (e.g., contrast, flicker, character size, resolution, etc.), working practices (breaks, hours keyboarding per day, task, etc.), environment (lighting, air conditioning, noise, etc.) and workstation design (viewing angle, viewing distance, glare etc.) (Thomson, 1998). Chair design has the potential to influence viewing angle and distance. Recommended optimum viewing ranges vary from 50 to 100 cm (Taptagaporn and Saito, 1993; Taptagaporn et al., 1995; Jaschinski et al., 1998). Recent studies suggest the optimum distance is linked to the user's vision system and is best chosen by the worker (Jainta and Jaschinski, 2002). Viewing angle is achieved through a mixture of changing neck posture, trunk inclination and moving the eyes within the head (Burgess-Limerick et al., 2000). As such, an optimum angle is a balance between musculoskeletal concerns and eye comfort and typically is found to be slightly below the horizontal (Sommerich et al., 2001). A highly adjustable office chair coupled with office ergonomics training can address all of these factors affecting visual symptoms of VDT users.
The highly adjustable chair used in the intervention was designed to allow the user to minimize changes in head location during dynamic use by having the seat slide forward when leaning backward in the chair (Reinicke et al., 1986). This supports the user's maintaining his or her hands on the keyboard (Bush and Hubbard, 1999). The ease of supported back movement may allow the worker to individually adjust their viewing distance without having to move the monitor. It may also allow comfortably minimizing glare by improving the opportunity to readjust eye location with respect to the monitor. Improved height adjustability with the chair may also allow the user to find a comfortable viewing angle without changing monitor height.
The Norwegian interventions identified sensitivity to light as the visual symptom most responsive to change in lighting conditions, whereas the optometric corrections resulted in reductions in eye tiredness, stinging or itching and sensitivity to light (Aaras et al., 1998, 2001). In our work, sensitivity to light, feeling dry and aching eyes were the visual symptoms most responsive to the intervention. The early ergonomic literature suggested two ergonomic-related pathways for visual symptoms, the dry eye pathway (identified by burning, irritation, tearing and dryness symptoms) and the eyestrain pathway (identified by ache, strain, headache behind eyes symptoms). Our research and the Norwegian studies do not easily fit within either pathway. Aaras and colleagues have suggested a third pathway – a conjoint relationship between musculoskeletal symptoms and visual symptoms (Aaras et al., 1998, 2001). Lie and Watter (1987) suggested that visual symptoms are a determinant of musculoskeletal health. Epidemiological research has found a relationship between eye-level computer monitor heights and neck discomfort (Bergqvist et al., 1995). Human factors research has shown a strong interaction between viewing distance and angle and cervical posture (Burgess-Limerick et al., 2000). Visual health is likely the result of managing competing visual and biomechanical task demands (Wolkoff et al., 2003). Given that both interventions resulted in reductions in both musculoskeletal and visual symptoms, this would seem to be a fruitful area of continued investigation.
The lack of a training-only group effect was unexpected when the study started. The training discussed reducing or eliminating direct and indirect glare by moving the monitor or adjusting the window blinds, managing visual distance and viewing angle, monitor placement, exercises to reduce eyestrain, eye exams and considering appropriate eyeglass prescriptions. Perhaps the difficulty of moving a monitor within the workspace and the difficulty managing cables are barriers not prevented by chair adjustment. The absence of a training-only group effect supports implementing training in conjunction with highly adjustable office furniture and equipment to reduce visual symptoms (Robson et al., 2009).
The lack of randomization and a chair-only control group are limitations. A range of individual-level covariates was measured and only a few were identified as confounders thus the groups were considered comparable. No differences were found in supervisory unit level policies and practices that could support or inhibit ergonomic behaviors (Robertson et al., 2008). Therefore, the observed differences are not due to organizational context. Employing a chair-only group, in theory, would allow disentangling the chair effect from the training effect, but it would be expensive to implement and given the multiple adjustments required to effectively use the chair, it was considered unethical to have a chair-only group.
Nonparticipation or loss to follow-up could affect the ability to make unbiased conclusions (Shadish et al., 2002). It is unlikely in this case due to the high levels of retention and similarities between the remaining participants and those lost to follow-up.
Finally, this research was conducted in a public sector organization in the United States. It is unknown whether the multi-component intervention would have the same effects in a private sector organization. Clearly, further research is needed to extend the generalizability of the findings.
Our research, coupled with Norwegian studies, suggests both medical and office ergonomic interventions may improve visual health and potentially productivity. Further intervention research is needed to support these findings and provide the knowledge base for occupational safety and health practice.
Acknowledgments
This research was funded by grants from Steelcase, Inc. to the University of Texas, The Upjohn Research Institute, York University and Health and Work Outcomes and through the support of the Liberty Mutual Research Institute for Safety. Cammie Chaumont Menéndez was supported by NIOSH Occupational Injury Prevention Training Grant T42 0H008421.
References
- Aaras A, Horgen G, Bjorset H, et al. Musculoskeletal, visual and psychosocial stress in VDU operators before and after multidisciplinary ergonomic interventions. Appl. Ergon. 1998;29:335–354. doi: 10.1016/s0003-6870(97)00079-3. [DOI] [PubMed] [Google Scholar]
- Aaras A, Horgen G, Bjorset H, et al. Musculoskeletal, visual and psychosocial stress in VDU operators before and after multidisciplinary ergonomic interventions. A 6 years prospective Study–part II. Appl. Ergon. 2001;32:557–559. doi: 10.1016/s0003-6870(01)00030-8. [DOI] [PubMed] [Google Scholar]
- Aaras A, Horgen G, Ro O, Loken E, Mathiasen G, Bjorset HH, Larsen S, Thoresen M. The effect of an ergonomic intervention on musculoskeletal, psychosocial and visual strain of VDT data entry work: the Norwegian part of the international study. Int. J. Occup. Saf. Ergon. 2005;11:25–47. doi: 10.1080/10803548.2005.11076627. [DOI] [PubMed] [Google Scholar]
- Amick BC, III, Roberston MM, DeRango K, et al. Effect of office ergonomics intervention on reducing musculoskeletal symptoms. Spine. 2003;28:2706–2711. doi: 10.1097/01.BRS.0000099740.87791.F7. [DOI] [PubMed] [Google Scholar]
- Bergqvist UD, Knave BG. Eye discomfort and work with visual display terminals. Scand. J. Work Environ. Health. 1994;20:27–33. doi: 10.5271/sjweh.1432. [DOI] [PubMed] [Google Scholar]
- Bergqvist UD, Knave BG, Voss M, et al. A longitudinal study of VDT work and health. Int. J. Hum. Comput. Interact. 1992;4:197–219. [Google Scholar]
- Bergqvist UD, Wolgast E, Nillson B, et al. Musculoskeletal disorders among visual display terminal workers, individual, ergonomic, and work organizational factors. Ergonomics. 1995;38:763–776. doi: 10.1080/00140139508925148. [DOI] [PubMed] [Google Scholar]
- Brewer S, Van Eerd D, Amick BC, III, et al. Workplace interventions to prevent musculoskeletal and visual symptoms and disorders among computer users, a systematic review. J. Occup. Rehabil. 2006;16:325–358. doi: 10.1007/s10926-006-9031-6. [DOI] [PubMed] [Google Scholar]
- Burgess-Limerick R, Mon-Williams M, Coppard VL. Visual display height. Hum. Factors. 2000;42:140–150. doi: 10.1518/001872000779656598. [DOI] [PubMed] [Google Scholar]
- Bush T, Hubbard R. Proceedings of the Human Factors and Ergo-nomics Society 43rd Annual Meeting. Houston, Texas: 1999. An evaluation of postural motions, chair motions and contact in four office seats. pp. 589–593. [Google Scholar]
- Collins MJ, Brown B, Bowman KJ, et al. Task variables and visual discomfort associated with the use of VDTs. Optom. Vis. Sci. 1991;68:27–33. doi: 10.1097/00006324-199101000-00005. [DOI] [PubMed] [Google Scholar]
- Dain SJ, McCarthy AK, Chan-Ling T. Symptoms in VDU operators. Am. J. Optom. Physiol. Opt. 1988;65:162–167. doi: 10.1097/00006324-198803000-00004. [DOI] [PubMed] [Google Scholar]
- Dainoff MJ, Happ A, Crane P. Visual fatigue and occupational stress in VDT operators. Hum. Factors. 1981;23:421–438. doi: 10.1177/001872088102300405. [DOI] [PubMed] [Google Scholar]
- Dainoff MJ, Aaras A, Horgen G, Konarska M, Larsen S, Thoresen M, Cohen BG, MEPS Study Group The effect of an ergonomic intervention on musculoskeletal, psychosocial and visual strain of VDT entry work: organization and methodology of the international study. Int. J. Occup. Saf. Ergon. 2005a;11:9–23. doi: 10.1080/10803548.2005.11076629. [DOI] [PubMed] [Google Scholar]
- Dainoff MJ, Cohen BG, Dainoff MH. The effect of an ergonomic intervention on musculoskeletal, psychosocial, and visual strain of VDT data entry work: the United States part of the international study. Int. J. Occup. Saf. Ergon. 2005b;11:49–63. doi: 10.1080/10803548.2005.11076630. [DOI] [PubMed] [Google Scholar]
- Daum KM, Clore KA, Simms SS, et al. Productivity associated with visual staring among computer users. Optometry. 2004;75:33–47. doi: 10.1016/s1529-1839(04)70009-3. [DOI] [PubMed] [Google Scholar]
- DeRango K, Amick BC, III, Robertson MM, et al. The Productivity Consequences of Two Ergonomic Interventions. Institute for Work and Health; Toronto, Ontario: 2003. Working Paper Series, #222. [Google Scholar]
- Faiks F, Allie P. Supporting the torso through seated articulation.. Proceedings of the Human Factors and Ergonomics Society 43rd Annual Meeting; Houston, Texas. 1999. pp. 574–578. [Google Scholar]
- Horgen G, Aaras A, Thoresen M. Will visual discomfort among visual display unit (VDU) users change in development when moving from single vision lenses to specially designed VDU progressive lenses? Optom. Vis. Sci. 2004;81:341–349. doi: 10.1097/01.opx.0000134908.44145.49. [DOI] [PubMed] [Google Scholar]
- Horgen G, Aaras A, Dainoff MJ, Konarska M, Thoresen M, Cohen B, MEPS Study Group A cross-country comparison of short- and long-term effects of an ergonomic intervention on musculoskeletal discomfort, eyestrain and psychosocial stress in VDT operators: selected aspects of the international project. Int. J. Occup. Saf. Ergon. 2005;11:77–92. doi: 10.1080/10803548.2005.11076632. [DOI] [PubMed] [Google Scholar]
- Jainta S, Jaschinski W. Fixation disparity, binocular vergence accuracy for a visual display at different positions relative to the eyes. Hum. Factors. 2002;44:443–450. doi: 10.1518/0018720024497736. [DOI] [PubMed] [Google Scholar]
- Jaschinski W, Heuer H, Kylian H. Preferred position of visual display relative to the eyes, a field study of visual strain and individual differences. Ergo-nomics. 1998;41:1634–1649. doi: 10.1080/001401398186586. [DOI] [PubMed] [Google Scholar]
- Ketola R, Toivonen R, Hakkanen M, Luukkonen R, Takala EP, Viikari-Juntura E, Expert Group Effects of ergonomic intervention in work with video display units. Scand. J. Work Environ. Health. 2002;28:18–24. doi: 10.5271/sjweh.642. [DOI] [PubMed] [Google Scholar]
- Knave BG, Wilbon RI, Voss M, et al. Work with video display terminals among office employees, subjective status and discomfort. Scand. J. Work Environ. Health. 1985;11:457–486. doi: 10.5271/sjweh.2200. [DOI] [PubMed] [Google Scholar]
- Konarska M, Wolska A, Widerszal-Bazyl M, Bugajska J, Roman-Liu D, Aaras A. The effect of an ergonomic intervention on musculoskeletal, psychosocial, and visual strain of VDT data entry work: the Polish part of the international study. Int. J. Occup. Saf. Ergon. 2005;11:65–76. doi: 10.1080/10803548.2005.11076631. [DOI] [PubMed] [Google Scholar]
- Kuorinka I, Forcier L. Work Related Musculoskeletal Disorders (WMSDs), A Reference Book for Prevention. Taylor and Francis; UK: 1995. [Google Scholar]
- Lie J, Watter RG. Occulomotor factors in the aetiology of occupational cervichobrachial disease (OCD). Eur. J. Appl. Physiol. 1987;56:151–156. doi: 10.1007/BF00640638. [DOI] [PubMed] [Google Scholar]
- MLwiN [software] Version 1.10. Multilevel Models Project Institute of Education. London: 2001. [Google Scholar]
- Mocci F, Serra A, Corrius GA. Psychological factors and visual fatigue in working with video display terminals. Occup. Environ. Med. 2001;58:267–271. doi: 10.1136/oem.58.4.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academy of Sciences . Video Displays, Work, and Vision. National Academy Press; Washington, DC.: 1983. [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health . Potential Health Hazards of Video Display Terminals (Publication No. 81-129) Cincinnati, OH.: 1981. [Google Scholar]
- National Research Council and Institute of Medicine . Musculoskeletal Disorders and the Workplace, Low Back and Upper Extremities. National Academy Press; Washington, DC.: 2001. [PubMed] [Google Scholar]
- Ostberg O. CRTs pose health problems for operators. Int. J. Occup. Health Saf. 1975:24–52. [PubMed] [Google Scholar]
- Psihogios JP, Sommerich CM, Mirka GA, Moon SD. A field evaluation of monitor placement effects in VDT users. Appl. Ergon. 2001;32:313–325. doi: 10.1016/s0003-6870(01)00014-x. [DOI] [PubMed] [Google Scholar]
- Rasbash J, Browne W, Goldstein H, et al. A User's Guide to MLwiN. University of London Press; 2000. [Google Scholar]
- Reinicke S, Weisman G, Stifter A, Pope MH. Effects of seating posture on pressure distribution in office seating.. Proceedings of the 19th Annual Meeting of the Human Factors Association of Canada; Richmond (Vancouver), British Columbia. 1986. pp. 11–13. [Google Scholar]
- Robertson MM, Amick BC, III, DeRango K, et al. The impact of an office ergonomics training on worker knowledge, behavior and musculoskeletal risk.. Proceedings of the 6th International Scientific Conference on Work with Display Units; Berchtesgaden, Germany. ERGONOMIC Institut für Arbeit-und Sozialforschung Forschungsgesellschaft mbH; 2002. pp. 376–378. [Google Scholar]
- Robertson M, Amick B, Rooney T, DeRango K, Bazanni L. Organizational practices and policies, results from an office ergonomic field intervention study.. Proceedings of the 9th International Symposium on Human Factors in Organizational Design and Management; 2008. CD ROM. [Google Scholar]
- Robertson MM, Amick BC, III, DeRango K, Rooney T, Bazzani L, Harrist RH, Moore A. The effects of an office ergonomics training and chair intervention on worker knowledge. Behav. Musculoskelet. Risk Appl. Ergon. 2009;40:124–135. doi: 10.1016/j.apergo.2007.12.009. [DOI] [PubMed] [Google Scholar]
- Robson LS, Stephenson CM, Schulte P, Amick BC, III, Irvin EL, Eggerth DE, Chan S, Bielecky AR, Wang AM, Heidotting TL, Peters RH, Clarke JA, Cullen K, Rotunda CJ, Grubb PL. A Systematic Review of the Effectiveness of Occupational Health and Safety Training. Institute for Work and Health; Toronto, Canada: 2009. [DOI] [PubMed] [Google Scholar]
- Rocha LE, Debert-Riberiro M. Working conditions, visual fatigue and mental health among systems analysts in Sao Paulo, Brazil. Occup. Environ. Med. 2004;61:24–32. [PMC free article] [PubMed] [Google Scholar]
- Salibello C, Nilsen E. Is there a typical VDT patient? A demographic analysis. J. Am. Optom. Assoc. 1995;66:479–483. [PubMed] [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-experimental Designs for Generalized Causal Inference. Houghton Mifflin Company; Boston: 2002. [Google Scholar]
- Smith MJ, Cohen BGF, Stammerjohn LW., Jr. An investigation of health complaints and job stress in video display operations. Hum. Factors. 1981;23:387–400. doi: 10.1177/001872088102300402. [DOI] [PubMed] [Google Scholar]
- Sommerich C, Joines S, Psihogios J. Effects of computer monitor viewing angle and related factors on strain, performance, and preference outcomes. Hum. Factors. 2001;45:39–55. doi: 10.1518/001872001775992480. [DOI] [PubMed] [Google Scholar]
- StataCorp, Stata [software] Release 7.0. Stata Corporation; College Station, TX.: 2001. [Google Scholar]
- Taptagaporn S, Saito S. Visual comfort in VDT operation, physiological resting states of the eye. Ind. Health. 1993;31:13–28. doi: 10.2486/indhealth.31.13. [DOI] [PubMed] [Google Scholar]
- Taptagaporn S, Sotoyama M, Saito S, et al. Visual comfort in VDT workstation design. J. Hum. Ergol. 1995;24:84–88. [PubMed] [Google Scholar]
- Thomson D. Eye problems and visual display terminals – the facts and the fallacies. Ophthalmic Physiol. Opt. 1998;18:111–119. [PubMed] [Google Scholar]
- Wolkoff P, Skov P, Franck C, et al. Eye irritation and environmental factors in the office environment-hypotheses, causes and a physiological model. Scand. J. Work Environ. Health. 2003;29:411–430. doi: 10.5271/sjweh.748. [DOI] [PubMed] [Google Scholar]