Abstract
Solitary fibrous tumors are well described in the pleura, but rare extra-pleural neoplasms have been reported. We describe a patient with a solitary left renal fibrous tumor who after undergoing a nephrectomy, presented 8 years later with a contralateral metachronous solitary fibrous tumor. Malignant metastatic extra-pleural solitary fibrous tumors are extremely rare, and to our knowledge, this is the first case of contralateral recurrence of solitary renal fibrous tumor. The patient underwent a robotic assisted partial nephrectomy of the right renal mass. Both tumors showed overlapping histopathology.
Keywords: Solitary fibrous tumor, Hemangiopericytoma, Metachronous metastasis, CD34
Abbreviations: Cr, creatinine; CT, Computerized Tomography; HPF, High Power Field; NCCN, National Comprehensive Cancer Network; SFT, solitary fibrous tumor
Introduction
Solitary fibrous tumors are most commonly described in the pleura but extra-pleural cases have been identified, rarely occurring in the kidney. Solitary fibrous tumors most commonly carry a benign course. Malignant cases are pathologically characterized by high cellularity, >10 mitotic figures per 10 HPF, pleomorphism, hemorrhage and necrosis and tend to metastasize and limit patient survival.1 Patients with benign lesions are usually cured by simple excision whereas only half of those with malignant tumors are cured this way.1
We present here the first case of contralateral recurrent malignant solitary fibrous tumor of the kidney.
Case presentation
A 49-year-old female who presented to our institution with vague abdominal pain, nausea, and a 15 lbs weight loss was found to have a 19 × 12 × 10 cm left enhancing renal mass with central necrosis and calcifications on abdominal CT scan (Fig. 1). The patient underwent left renal artery embolization by interventional radiology followed by a left radical nephrectomy with retroperitoneal lymphadenectomy. Pathologic evaluation revealed a 16 × 11 × 9 cm solitary fibrous tumor involving the perinephric soft tissue of the renal hilum, renal capsule, serosa of the ureter, and renal pelvis without lymphovascular invasion or nodal involvement (0 out of 35 lymph nodes). On immunohistochemical staining, the neoplastic cells were strongly positive for CD34 (>50%), and weakly focally positive for ER (10%), and PR (5%). They were negative for keratins AE1/AE3, CK 7, CK20, EMA, P63, CD10, HMB 45, Melan-A, and CD117. SMA showed focal positivity and the tumor had 5 mitoses per 10 HPF.
Figure 1.
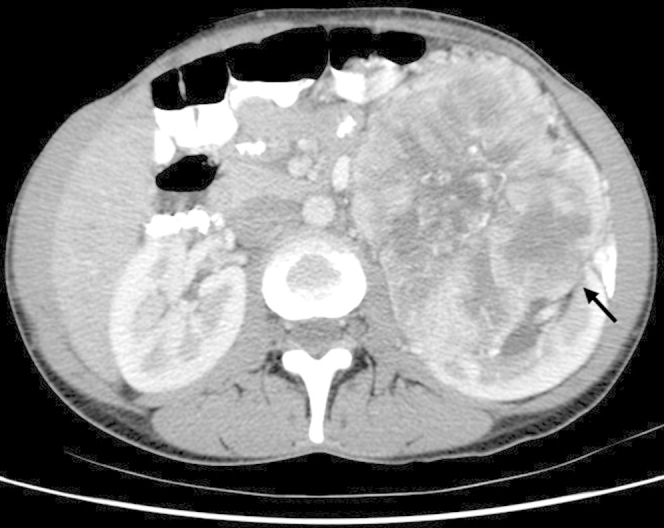
Large 12 cm × 10 cm enhancing left renal mass with central necrosis and calcification on initial presentation (black arrow).
Eight years after the initial operation, a follow up CT scan revealed a 4.3 cm exophytic, low complexity, enhancing solid mass with cystic and necrotic foci occupying the lower pole of the right kidney highly suspicious for malignancy (Fig. 2). A robotic assisted laparoscopic right partial nephrectomy was performed without complication. H&E staining showed a cellular spindle cell neoplasm with an elevated mitotic rate up to 6 mitoses in 10 HPF, significant cytologic atypia, and regions of necrosis. Immunohistochemistry revealed that tumor cells were positive for CD34 (∼10%), diffuse CD99 (Fig. 3), diffuse BCL-2 and vimentin. The case was compared to the prior contralateral renal tumor and showed overlapping histomorphology. Follow up CT imaging 18 months post-op revealed no evidence of tumor recurrence and renal function remained stable (Cr 1.07 mg/dL, GFR 58 mL/min/1.73 m2 based on MDRD).
Figure 2.
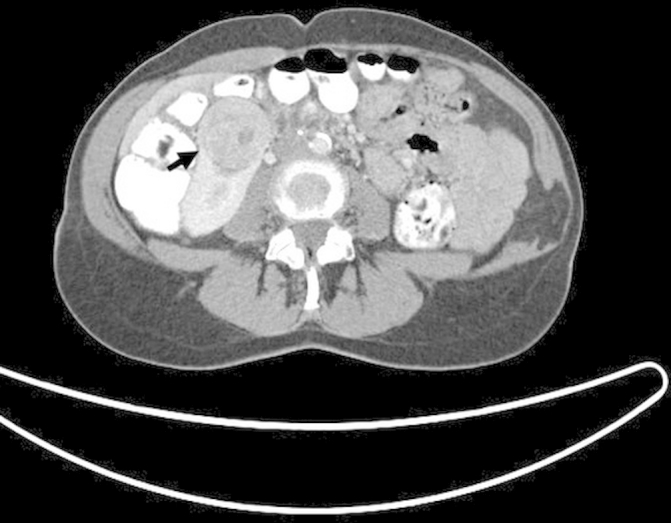
Eight years post left radical nephrectomy with new 4.3 cm enhancing right renal mass with necrotic foci (black arrow).
Figure 3.
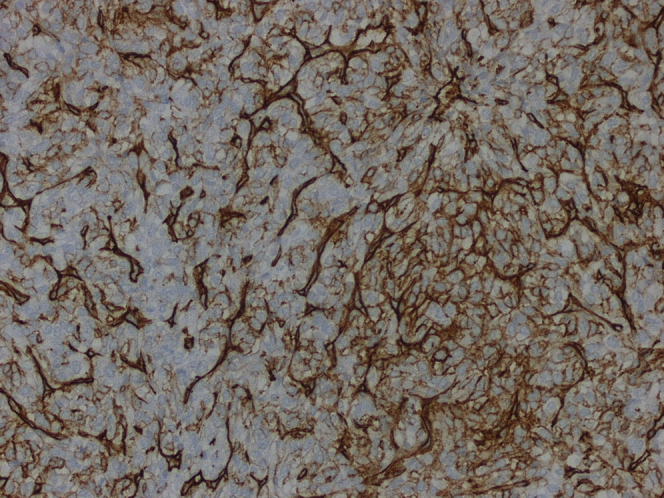
Histopathology of the resected metachronous right kidney lesion revealing spindle cell architecture, cytological atypia, and diffuse CD 99 staining on immunohistochemistry consistent with malignant SFT.
Discussion
Solitary fibrous tumors, also known as hemangiopericytomas, are usually benign and arise from mesenchymal spindle cells typically from the pleura. Extra-pleural sites have been described and the behavior of these SFTs can be unpredictable and may arise in different parts of the body with the first renal site reported by Gelb et al in 1996.2 While close to 50 cases of renal SFT are described in literature, malignant disease still remains extremely rare with only 8 other cases described, and none to our knowledge presented with metachronous spread to the contralateral kidney (Table 1).
Table 1.
Review of reported malignant renal SFT s/p nephrectomy
| Case | Reference | Year | Age | Sex | Size (cm) | Outcome |
|---|---|---|---|---|---|---|
| 1 | Fine et al3 | 2006 | 76 | M | 12 | Persistent disease |
| 2 | Magro et al | 2008 | 34 | F | 9 | Disease free |
| 3 | Marzi et al | 2011 | 72 | F | 19 | Unknown |
| 4 | Hsieh et al | 2011 | 50 | F | 9 | Disease free |
| 5 | De Martino et al | 2012 | 68 | F | 7 | Disease specific death |
| 6 | Cuello & Brugés | 2012 | 49 | F | 9.8 | Stable disease |
| 7 | Sasaki et al4 | 2013 | 48 | M | 28 | Disease free |
| 8 | Mearini et al | 2014 | 19 | F | 17 | Disease free |
Solitary fibrous tumor of the kidney has been described as originating from the renal capsule, and thus sarcomatoid RCC is often in the differential.5 Immunohistochemically, SFT stain positive for CD34 in a majority of the cases (sensitivity >90%), BCL-2 in about 50% of the time, and vimentin in 20%.3 However, with malignant transformation, SFT may lose CD34 expression and staining as described by Sasaki, et al in which the primary resected renal tumor stained CD34 positive, but negative in the distant metastatic liver site and weakly positive in the pleural site.3
Pathophysiologic mechanisms for malignant transformation of SFT have been postulated in literature but difficult to prove due to lack of large scale studies. The two ideas proposed are 1) de novo occurrence and 2) dedifferentiation from pre-existing benign SFT.3 Because our case shows a decrease in the CD34 staining while remaining morphologically similar in the recurrent contralateral tumor compared to the original lesion, sarcomatous dedifferentiation is a feasible mechanism of transformation.
Given the findings in the recurrent right side tumor of hypercellularity, pleomorphism, and 6 mitoses/10 HPF in our case, this tumor fulfills most criteria for malignant SFT (high cellularity, pleomorphism, dedifferentiation, mitosis >4 per 10 HPF, size exceeding 10 cm, and abnormal sites of presentation for pleural and extra-pleural malignant solitary fibrous tumors).1 SFTs are also known to occur in unusual visceral sites such as pancreas, prostate, spermatic cord and diaphragm with similarly unusual metastatic spread described to omentum, peritoneum, subcutaneous tissues and colonic mesentery.4 In a series of 79 patients with SFTs (pleural and extra-pleural), 16 patients (20%) had malignant components. None of these patients were described as having multi-focal primary SFTs.4 Therefore, it does not appear that a subset of patients exist with a genetic predisposition to recurrent primary SFT. Given the similar histomorphology of the original tumor and contralateral recurrence, the size of the original tumor increasing the risk of metastasis and the propensity of SFTs to spread to unusual sites, we believe this case to be consistent with a metastasis and less likely to represent multi-focal tumor.
Conclusion
In summary, we report a case of isolated recurrent malignant SFT arising in the right kidney 8 years after nephrectomy for SFT of the contralateral side likely representing metastatic spread. Metachronous lesions of solitary fibrous tumors suggest malignant potential in a tumor otherwise considered to be benign in majority of cases. These findings may play significant impact in patient management as providers should council patients with high risk pathologic features as to the need for surveillance. Based on findings from our study as well as prior case reports, we propose for SFTs meeting malignant criteria, a surveillance protocol similar to the current NCCN guidelines for other renal malignancies – at minimum a yearly clinical evaluation with chest and abdominal axial imaging. With reports describing malignant recurrence of SFTs anywhere from 8–20 years from initial diagnosis, we propose continuing follow up long term. Malignant SFT cases are rare and future studies will be necessary to elucidate follow up guidelines for surveillance.
Conflict of interest
The authors of this case report declare that they have nothing to disclose and no conflict of interests. No outside financial support was received for the preparation of this case report.
References
- 1.England D.M., Hochholzer L., McCarthy M.J. Localized benign and malignant fibrous tumors of the pleura. A clinicopathologic review of 223 cases. Am J Surg Pathol. 1989;13(8):640–658. doi: 10.1097/00000478-198908000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Gelb A.B., Simmons M.L., Weidner N. Solitary fibrous tumor involving the renal capsule. Am J Surg Pathol. 1996;20:1288–1295. doi: 10.1097/00000478-199610000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Sasaki H., Kurihara T., Katsuoka Y. Distant metastasis from benign solitary fibrous tumor of the kidney. Case Rep Nephrol Urol. 2013;3(1):1–8. doi: 10.1159/000346850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gold J.S., Antonescu C.R., Hajdu C. Clinicopathologic correlates of solitary fibrous tumors. Cancer. 2002;94(4):1057–1068. [PubMed] [Google Scholar]
- 5.Fine S.W., McCarthy D.M., Chan T.Y. Malignant solitary fibrous tumor of the kidney: report of a case and comprehensive review of the literature. Arch Pathol Lab Med. 2006;130:857–861. doi: 10.5858/2006-130-857-MSFTOT. [DOI] [PubMed] [Google Scholar]


