Abstract
Urothelial carcinomas are the fourth most common tumors in men. Upper tract urinary carcinomas (UTUCs) are uncommon and represent only 5–10% of urothelial carcinomas.1 Metastatic testicular cancers are rare and primary tumor sources are the prostate, lung, and gastrointestinal tract. We report the first case of testicular metastasis 2 years after initial curative surgery for a high-grade UTUC, all other reported cases weren't proceed by curative surgery.3
Keywords: Testicular, Metastasis, Urothelial, Carcinoma
Introduction
Urothelial carcinomas are the fourth most common tumors in men. Upper tract urinary carcinomas (UTUCs) are uncommon and represent only 5–10% of urothelial carcinomas.1 The testicular metastases are quite common, but rarely of urothelial origin, and such cancers are determined incidentally in orchidectomy or autopsy specimens.2 Primary tumors known to metastasize in the testes include, in order of frequency: prostate, lung, digestive tract, melanoma and renal tumor.
Only 2 cases of testicular urothelial metastasis have been reported, however with synchronous primary urothelial cancer.3
We report the first case of testicular metastasis of a UTUC, 2 years after curative surgery by nephroureterectomy.
Case report
A 70 year old man presented in 2011 with gross hematuria in our outpatient clinic. Cystoscopy showed two papillary lesions of 5 mm in the left retromeatal region as well as a sessile bladder lesions of 5 mm of the posterior bladder wall. After complete resection, histology showed an low grade urothelial papillary carcinoma stage pTa.
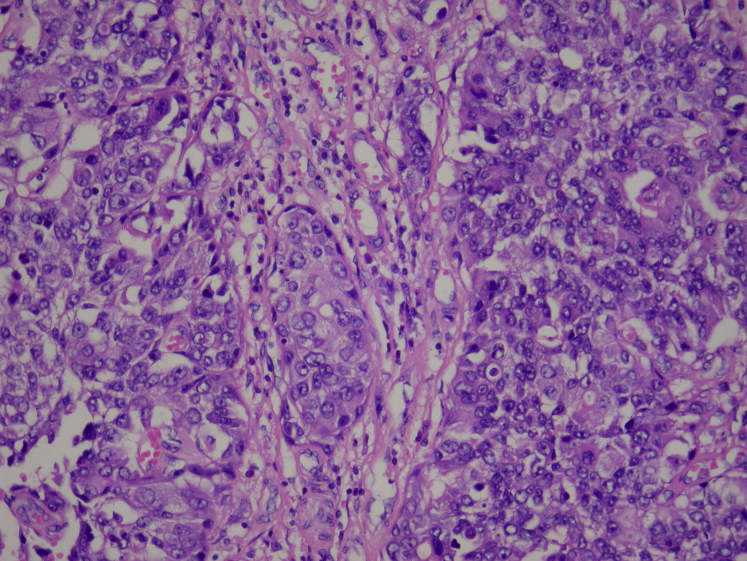
During follow-up, the patient presented 2 years later left kidney pain with gross hematuria. CT-scan showed a highlighting central tissue lesion of 4.2 × 4.1 × 4 cm in the left kidney (Fig. 1), raising the differential diagnosis of urothelial carcinoma versus renal carcinoma. A nephroureterectomy is realized in July 2013 and pathology showed a caliceal high-grade papillary urothelial carcinoma infiltrating the renal parenchyma of 2.5 × 2.4 × 4.4 cm. Pathological stage was a pT3 cN0 cM0 R0 carcinoma (Fig. 2).
Figure 1.

CT-scan showing a central tissue lesion in the left kidney.
Figure 2.
Histopathology of the left kidney showing a high-grade urothelial carcinoma.
In July 2015, the patient was readdressed by his urologist after treating a chronic left orchi-epididymitis, resistant to several antibiotic treatments. The patient reported chronic left testicular pain without any other symptoms. Physical examination showed a fixed painful testis with an induration of the whole spermatic cord.
CT-scan revealed an inflammation of the testis and spermatic cord without any lymph node nor secondary lesions (Fig. 3).
Figure 3.

Inflammation of the left spermatic cord.
The indication for orchiectomy is retained.
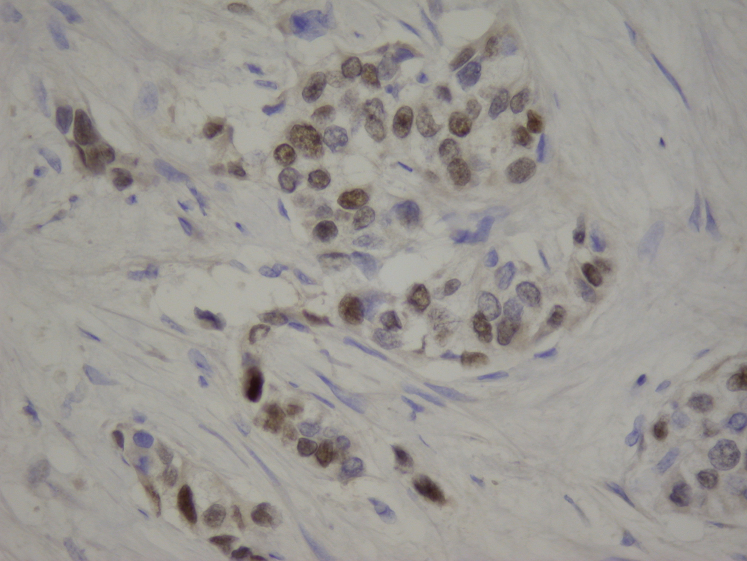
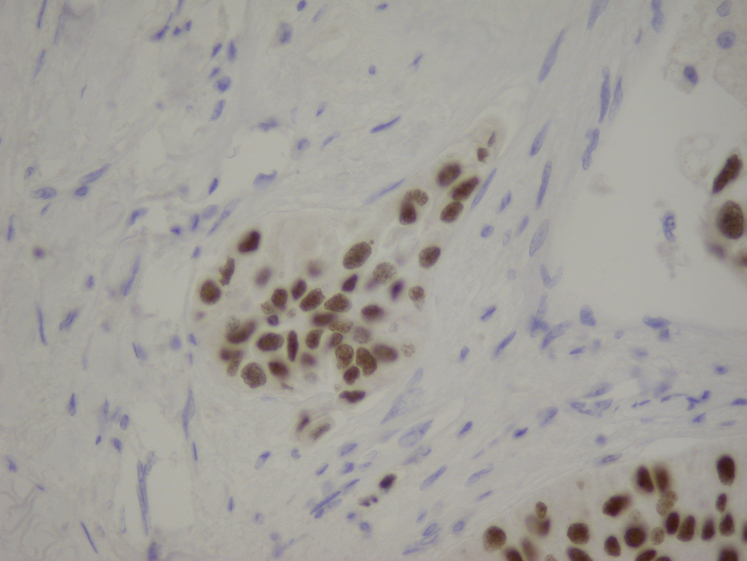
Pathology returned positive for a testicular metastasis of the known urothelial carcinoma (histological characteristics were similar to those of the nephrectomy in 2013), infiltrating the epididymis and the base of the spermatic cord with many lymphovascular invasions as well as perineural engainments in the testicular parenchyma and the spermatic cord, reaching the surgical margin at the spermatic cord. The markers p63 and Gata 3 were positive (Figure 4, Figure 5).
Figure 4.
P63 positive.
Figure 5.
Gata 3 positive.
We completed examination with a Pet-CT who showed many hypermetabolic lesions in the lungs, adrenal gland, liver, intra-peritoneal spermatic cord and the penis posing the indication of a palliative chemotherapy.
Discussion
Metastatic testicular tumors are very rare. Our case is the first describing a testicular metastasis of a urothelial UTUC after initial curative surgery. The most common pathway of tumor spread in urothelial carcinoma is the lymphovascular system.
In this case, we can see that the renal tumor as well as the metastasis were both on the left side without any positive lymph node on the CT-scan, opening the hypothesis that the dissemination was done through the vascular system.
Conclusion
Monitoring of patients with urothelial carcinoma is important and any atypical evolution must quickly been completed by additional examinations. For this patient, the management was probably too late, especially because a potential testicular metastasis of his urothelial carcinoma was not the first assumption.
Conflict of interest
There is no conflict of interest.
References
- 1.Ther Adv Urol. 2011 April;3(2):69–80. doi: 10.1177/1756287211403349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eble J.N., Sauter G., Epstein J.I., Sesterhenn I.A., World Health Organization Classification of Tumours . 1st ed. IARC Press; Lyon, France: 2004. Pathology and Genetics of Tumours of the Urinary System and Male Genital Organs. [Google Scholar]
- 3.Case Rep Urol. 2014;2014 Article ID 759858, 3 pages. [Google Scholar]