Summary
Background
In this paper the clinical and radiological features of three cases with paratesticular fibrous pseudotumor were presented after a retrospective analysis of medical archives of our hospital.
Case Report
Each of the three cases had unilateral, multiple nodular lesions with smooth borders accompanied by a hydrocele. On sonographic examination, the lesions showed echogenicity similar to, or slightly lower than, the testis, and the two large lesions had posterior acoustic shadowing. Color Doppler ultrasound examination of two cases showed intralesional vascularity of mild-to-moderate degree. All lesions appeared hypointense compared to testicular tissue on T1W and T2W magnetic resonance images. Moderate-to-high enhancement was observed in the diffuse pattern after intravenous injection of contrast material. An intraoperative pathological examination was performed and local excision carried out in all three cases.
Conclusions
Fibrous pseudotumor is a rare benign paratesticular lesion, which can be confused with malignant masses. Imaging procedures play an important role in correct diagnosis. Unfamiliarity with imaging findings of paratesticular fibrous pseudotumor may eventuate in an unnecessary orchiectomy.
MeSH Keywords: Magnetic Resonance Imaging; Multidetector Computed Tomography; Scrotum; Ultrasonography; Ultrasonography, Doppler, Color
Background
Fibrous pseudotumor is a non-neoplastic disease characterized by benign fibroinflammatory proliferation of paratesticular tissues, which presents with one or more nodular mass lesions [1,2]. Although tunica vaginalis is the most commonly involved tissue (75%), tunica albuginea, epididymis, and spermatic cord may also be involved [2]. This disorder affects a wide range of ages, ranging from 7 to 95 years [1].
Since the affected persons typically present with firm scrotal masses, these lesions may clinically be confused with malignancies. Therefore, many cases with this condition are operated with radical orchiectomy despite the benign nature of the disease [2,3]. Although physicians have long been familiar with this condition, there is a fairly limited number of reports regarding its radiological imaging properties. In this case series we aimed to demonstrate the ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI) features of benign paratesticular fibrous pseudotumors.
Case Reports
Case one
A 58-year-old man with a history of urinary bladder tumor was detected to have palpable firm masses in his left scrotum. A sonographic examination revealed an isoechoic solid nodule with posterior acoustic shadowing measuring 5.5×4.5 mm in the neighborhood of the left testicle. Additionally, there were also flat nodular lesions measuring 7×3 mm, 3×2.5 mm, and 2.5×2 mm on the anterior scrotal wall, which originated from the tunica vaginalis (Figure 1). Furthermore, mild hydrocele accompanied the lesions. Color Doppler US (CDUS) examination showed that the lesions showed no or weak vascularity. Three tunica vaginalis lesions and the lesion adhering to the testis were excised with a left high inguinal and scrotal incision and sent for frozen examination. The operation was terminated when the pathology report identified a fibrous pseudotumor.
Figure 1.

An ultrasound image shows a mild hydrocele with several soft-tissue nodules arising from the tunica vaginalis (arrow heads) and a solid mass (asterisk) adjacent to the testis. Note that the mass is isoechoic compared with the testis and shows posterior acoustic shadowing. T=testis.
Case two
A 42-year-old man presented with a left scrotal swelling for 4 months. On physical examination a mobile and firm mass was palpated adjacent to the lower pole of the left testis. A sonographic examination revealed a solid mass lesion with a smooth contour and an ovoid morphology, which measured 20×17 mm and had a posterior acoustic shadowing adjacent to the lower pole of the left testis (Figure 2A, 2B). The patient had two additional nodular tunica vaginalis lesions measuring 3×2 mm and 2.5×2 mm. There was also a mild hydrocele on the left side. A scrotal MRI examination with contrast revealed that the lesion adjacent to the left testis appeared markedly hypointense on T2W series while it appeared mildly hypointense compared to testis on T1W series (Figure 2C). The post-contrast images showed mild heterogeneous contrast uptake. A CT examination with contrast obtained for another reason demonstrated diffuse contrast uptake of mild-to-moderate degree (Figure 2D). Samples were obtained from the lesions via left inguinal incision, and sent for frozen section. When pathology examination identified benign features, the operation was finished by complete excision of all lesions.
Figure 2.
(A) Longitudinal panoramic view of scrotal ultrasonography demonstrates a heterogeneous well-circumscribed hypoechoic mass (asterisk) in the infratesticular region. E=epididymis, T=testis. (B) The mass shows prominent posterior shadowing (arrows). (C) An axial T2-weighted MR image depicts a markedly hypointense nodular lesion. It is surrounded by a high-signal-intensity hydrocele. (D)Two nodular lesions (arrowheads) with moderate contrast enhancement are seen in an abdominopelvic CT scan.
Case three
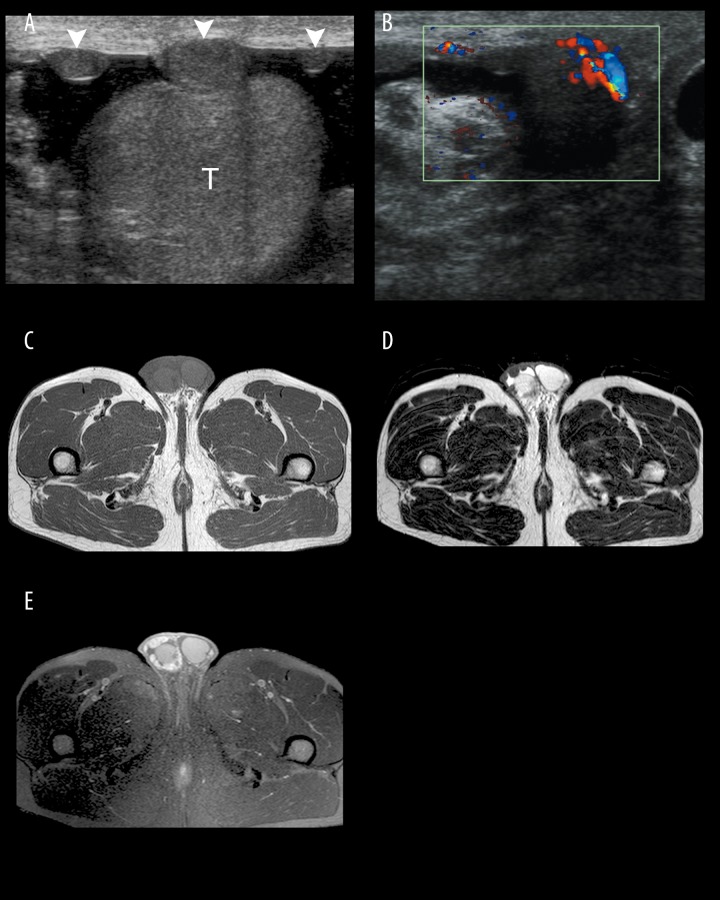
A 32-year-old man presented with right scrotal swelling for 6 months. His physical examination was notable for tiny subcutaneous nodularities in the right scrotum. A scrotal US examination showed mild hydrocele and multiple solid nodular lesions, with the largest measuring 16×9.5 mm, which originated from the tunica vaginalis and appeared slightly hypoechoic compared with the testis (Figure 3A). CDUS examination characterized vascularity of moderate degree in the lesions (Figure 3B). MR examination showed that all lesions had a hypointense appearance compared with the testis on both T1W and T2W series (Figure 3C, 3D). On postcontrast images all lesions were characterized by marked diffuse contrast uptake (Figure 3E). The late images taken 10 minutes later showed that the staining of the lesions persisted, albeit to a weaker degree. The pathology examination of the sample obtained at the operation identified benign fibrotic tissue fragments, and the operation was thus terminated after the lesions were excised with some tunica tissue.
Figure 3.
(A) An ultrasound image of the right scrotum reveals nodular lesions (arrowheads) projecting off the tunica vaginalis of the anterior wall into the scrotal fluid. T=testis. (B) Increased vascularity is seen around the pedicle of the dominant nodule on a color Doppler image. Axial MR images show multiple small nodular lesions, which are hypointense on T1-weighted image (C) and markedly hypointense on T2-weighted image (D); on contrast-enhanced image (E), the lesions have more intense enhancement than the normal testis.
Discussion
Fibrous pseudotumor is a rare form of paratesticular mass lesions. This lesion was identified in only 7 (6 of them were orchiectomized) of 114 cases with paratesticular mass lesions reported by Williams et al. [4]. The etiopathogenesis of this entity is still debated. However, it is widely believed that it develops in response to trauma, infections, and inflammatory hydrocele [5]. Approximately half of all cases are accompanied by a hydrocele, while 30% of them had a history of trauma or epididymoorchitis [6].
Most patients present with a painless scrotal swelling [1,5]. On physical examination these lesions are palpated as solitary or multiple painless, firm masses [6]. Histopathologically, they are characterized by dense hyalinized fibrous tissue, and dispersed collagen fibrils and proliferated fibroblasts. There may also exist dispersedly distributed inflammatory cells. Finally, granulation tissue and foci of calcification may co-exist with other findings [2,6].
The sonographic examination of the lesions shows varying echogenities depending on fibrous content and cellular amount, calcification, gross morphological character, and the involved organ. Posterior shadowing may also exist in non-calcified lesions. Such a finding suggests the existence of dense fibrotic tissue within a lesion. We observed posterior shadowing without calcification in the larger lesions of two of our cases. However, focal calcific areas were noted in the microscopic examination of our second case. CDUS may reveal mild-to-moderate vascularity within a lesion [7]. While we observed weak vascularity in our first case, there was a more prominent vascularity in our third case. It has been reported that these lesions appear as soft tissue masses showing mild contrast uptake in abdominopelvic CT examinations [3]. We, on the other hand, observed heterogeneous contrast uptake of moderate degree in the lesion of our second case.
MRI is the most valuable diagnostic tool that assumes a vital role in the differentiation of paratesticular fibrous pseudotumors from malignant conditions. These lesions have an intermediate-to-low signal intensity on T1W series whereas they have low signal intensity on T2W series [1]. Contrast uptake may be missing in postcontrast images. However, when contrast uptake is observed, it is rather mild. [1,2]. While fibrous pseudotumor shows a slow but sustained contrast uptake pattern (similar to other fibrotic tissue lesions), the amount of contrast uptake shows variation [8]. On the other hand, it has been reported that MR could also be utilized in the postoperative follow-up of these cases [7]. The MR imaging findings of our two cases were compatible with the literature data. The second case had mild-to-moderate contrast uptake while the third case had diffuse, marked contrast uptake.
Since fibrous pseudotumors are benign lesions, local excision is preferred over radical orchiectomy in their management [2,6]. In cases with a high clinical suspicion of malignancy, or in cases where fibrotic tissue diffusely occupies testicular tissue (fibromatous periorchitis), orchiectomy can be selected as the surgical procedure. Despite being controversial, some authors have reported that intraoperative frozen section examinations may guide operators for testis-conserving surgery [9]. The intraoperative pathology examination usefully guided the operation and local excisions were carried out in all of our three cases. These lesions are typically cured after surgical excision. However, recurrences have been reported, albeit extremely rare [7].
Conclusions
Fibrous pseudotumor is a rare cause of benign paratesticular mass lesions, which can be confused with malignant lesions. It should be kept in mind that the most typical imaging finding of these lesions is the prominently low signal intensity on T2W MRI images. It is of vital importance that radiologists should be well aware of the imaging features of this condition and properly guide clinicians. In addition, frozen section during operation is beneficial to avoid an unnecessary orchiectomy.
Footnotes
Statement
The authors have no financial, commercial or other conflicts of interest to declare.
References
- 1.Woodward PJ, Schwab CM, Sesterhenn IA. From the archives of the AFIP: extratesticular scrotal masses: radiologic-pathologic correlation. Radiographics. 2003;23(1):215–40. doi: 10.1148/rg.231025133. [DOI] [PubMed] [Google Scholar]
- 2.Akbar SA, Sayyed TA, Jafri SZ, et al. Multimodality imaging of paratesticular neoplasms and their rare mimics. Radiographics. 2003;23(6):1461–76. doi: 10.1148/rg.236025174. [DOI] [PubMed] [Google Scholar]
- 3.Kim KH, Sung DJ, Han NY, et al. Immunoglobulin G4-related paratesticular fibrous pseudotumor and retroperitoneal fibrosis: a case report. Urol Int. 2015;94(3):369–72. doi: 10.1159/000362215. [DOI] [PubMed] [Google Scholar]
- 4.Williams G, Banerjee R. Paratesticular tumors. Br J Urol. 1969;41:332–39. doi: 10.1111/j.1464-410x.1969.tb11893.x. [DOI] [PubMed] [Google Scholar]
- 5.Miyamoto H, Montgomery EA, Epstein JI. Paratesticular fibrous pseudotumor: a morphologic and immunohistochemical study of 13 cases. Am J Surg Pathol. 2010;34(4):569–74. doi: 10.1097/PAS.0b013e3181d438cb. [DOI] [PubMed] [Google Scholar]
- 6.Grebenc ML, Gorman JD, Sumida FK. Fibrous pseudotumor of the tunica vaginalis testis: imaging appearance. Abdom Imaging. 1995;20(4):379–80. doi: 10.1007/BF00203377. [DOI] [PubMed] [Google Scholar]
- 7.Germaine P, Simerman LP. Fibrous pseudotumor of the scrotum. J Ultrasound Med. 2007;26(1):133–38. doi: 10.7863/jum.2007.26.1.133. [DOI] [PubMed] [Google Scholar]
- 8.Cassidy FH, Ishioka KM, McMahon CJ, et al. MR imaging of scrotal tumors and pseudotumors. Radiographics. 2010;30(3):665–83. doi: 10.1148/rg.303095049. [DOI] [PubMed] [Google Scholar]
- 9.Parker PM, Pugliese JM, Allen RC., Jr Benign fibrous pseudotumor of tunica vaginalis testis. Urology. 2006;68(2):427.e17–9. doi: 10.1016/j.urology.2006.02.034. [DOI] [PubMed] [Google Scholar]