Abstract
Background
In the last few years, peritoneal dialysis (PD) catheter placement techniques and outcomes have become important because of the growing population of PD patients. Although there are a growing number of catheters placed by the minimally invasive Y-TEC peritoneoscopic technique, there are still limited data on outcomes for these catheters, especially those placed by a surgeon. We aimed to conduct a retrospective study of our experience with PD catheters placed by the Y-TEC peritoneoscopic technique in our institution.
Methods
We reviewed patients with peritoneoscopic PD catheter insertion over the last decade and described their complications and outcomes. In a secondary analysis, we compared the outcomes and complications of these catheters with those with open placement placed by the same surgeon.
Results
We had complete data on 62 patients with peritoneoscopic catheter placement during the study period. The mean age was 55 years, 48.4% were females and the most common cause of end-stage renal disease was diabetes mellitus (33%). Surgical complications were seen in only 6/62 (9.6%) and peritonitis in 16/62 (26%) of peritoneoscopic catheters. Most catheters were used after 2 months of placement, while 12.3% were used within 2 months. When compared with 93 patients with open placement of catheters as a secondary analysis, peritoneoscopic catheters were found to have a higher 2-year survival.
Conclusion
Our large series of peritoneoscopically placed catheters by a surgeon demonstrate low surgical complications and peritonitis rates as well as superior 2-year survival compared with open placement of catheters.
Keywords: CAPD, catheter, peritoneal dialysis, peritoneal membrane, peritoneoscopy
Introduction
Peritoneal dialysis (PD) has become a modality of choice for renal replacement therapy (RRT) for many end-stage renal disease (ESRD) patients requiring autonomy and having a busy lifestyle [1–6]. The PD catheter is the cornerstone of PD and its proper function and survival are crucial.
In the last few years, PD catheter placement techniques and outcomes have been the subject of several publications in the medical literature. Meta-analyses and systematic reviews have suggested that straight catheters tend to have less migration than coiled catheters [7–9]. Another important issue described in the recent literature is the improved results with fewer malfunctions and longer catheter survival found when performing the procedure with a classic laparoscopic technique using the several ports approach under general anesthesia [10]. However, there are still limited data on the outcomes of catheters placed by the minimally invasive Y-TEC peritoneoscopic technique. In the present study, we review our experience with these catheters over the past decade in a large population of PD patients. We also compared outcomes for these catheters with those placed by the classic open technique.
Materials and methods
Data collection
We performed a retrospective chart review of all ESRD patients who had a PD catheter inserted at Mount Sinai Hospital from 2004 to 2014. We only included the first instance of catheter placement for each patient. We performed a comprehensive chart review and abstracted demographics, comorbidities including diabetes mellitus and whether PD was the first RRT modality. We reviewed the operative notes and abstracted information on the surgical approach (peritoneoscopic versus open) and the time for first use after insertion. We also collected information on complications (mechanical/infectious/other), overall catheter survival and total time of follow-up (including when the patient discontinued PD due to inability/transplant/preference). The institutional review board of our institution approved the study.
Techniques of catheter implantation
Y-TEC peritoneoscopy technique
Under local anesthesia with mild sedation, a 2-cm paraumbilical paramedian incision is made in the skin and subcutaneous tissue, exposing the anterior rectus fascia. A 0 Prolene purse-ring stitch is placed in the fascia. Through the center of this purse-ring stitch, a Varis needle is introduced and 3 L of nitrous oxide is insufflated into the peritoneal cavity. This gas is used instead of CO2 because it is painless in the peritoneal cavity and allows for the procedure to be performed under local anesthesia. Once pneumoperitoneum is obtained, the Varis needle is removed and a Y-TEC trocar is introduced through the center of the purse ring. This trocar has a metallic cannula/peeling sheath that accepts the Y-TEC scope. Peritoneoscopy is done and the tip of the cannula/peeling sheath is directed toward the pelvis. The metallic cannula is removed, leaving the peeling sheath in place. The PD catheter, which is mounted on a rigid metallic rod, is introduced through the peeling sheath and as the catheter is being introduced, the rod is progressively removed. Before removing the peeling sheath, the distal Dacron cuff is forced into the rectal sheet. The purse-ring suture is tightened snugly around the catheter. The external side of the catheter is brought out through a small superior lateral skin opening, leaving the proximal Dacron cuff subcutaneously.
Open technique
Under general anesthesia, a 5–10 cm long paraumbilical paramedian incision is made in the skin and subcutaneous layers. The anterior rectus muscle fascia is opened in the same direction and extension. The muscle fibers are split, exposing the posterior fascia/peritoneal membrane. A 0 Prolene purse-ring stitch is placed in this layer and in the center of it, a small opening is made. The PD catheter is introduced through this opening, directing the tip of the catheter to the pelvic area. The distal Dacron cuff is positioned outside of the posterior fascia/peritoneal membrane and the purse-ring suture is tightly tied around the catheter. The anterior rectus fascia is closed with a continuous 0 Prolene suture. The catheter is exited through a small skin incision superior/lateral, leaving the proximal Dacron cuff in the subcutaneous layer.
Statistical analysis
We summarized differences in continuous variables using mean/median values depending on their distribution and categorical variables using percentages. We utilized t-test/Wilcoxon rank-sum test for continuous and χ2 test for categorical variables to assess differences between patients who lost their catheters versus those who did not. As a secondary analysis, we analyzed the independent effect of the peritoneoscopic versus open placement technique using Cox proportional hazard modeling after adjusting for demographics and comorbidities. We censored follow-up time at death, transfer to hemodialysis (with a functioning PD catheter) or loss to follow-up. We constructed Kaplan–Meier curves to plot catheter survival over the follow-up period. We used a two-tailed P-value ≤0.05 to determine statistically significant differences. All statistical analyses were performed using STATA 12 SE (StataCorp, College Station, TX, USA).
Results
Baseline characteristics
From February 2004 to June 2014, a total of 155 ESRD patients had their first PD catheters inserted at the Icahn School of Medicine at Mount Sinai. Table 1 summarizes patients' baseline characteristics both overall as well as stratified by the type of catheter placement. The mean age was 55 years, 51% were males and 63.2% of patients were white. Diabetes mellitus was the most common cause of ESRD in our population, followed by hypertension and chronic glomerulonephritis/HIV-associated nephropathy (HIVAN). PD was the first modality of RRT in 103 (66.5%) patients. In 130 (83.9%) patients, catheters were used after 2 months of insertion, whereas in 19 (12.3%) patients, catheters were used <2 months, mostly in the setting of urgent-start PD. Three catheters had primary nonfunction, one was never used because the patient expired 5 days after PD catheter placement and one was never used because the patient was never started on PD. With the exception of lower body mass index in patients with peritoneoscopic placement, there were no significant differences in baseline characteristics by catheter placement technique.
Table 1.
Baseline characteristics of patients overall and stratified by catheter loss (n = 155)
| Overall | Patients with Y-TEC peritoneoscopic catheter placement (n = 62) | Patients with open catheter placement (n = 93) | P-value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 55.1 (17.1) | 56.5 (17.9) | 54.2 (16.6) | 0.42 |
| Male, n (%) | 79 (51) | 36 (59) | 42 (45.2) | 0.09 |
| Race, n (%) | 0.39 | |||
| White | 98 (63.2) | 36 (59) | 58 (62.4) | 0.68 |
| African American/other | 57 (36.8) | 24 (41) | 35 (37.6) | |
| Body mass index, median (IQR) | 26 (23–30) | 25 (22–28) | 27.5 (24–32) | 0.02 |
| Cause of ESRD, n (%) | 0.10 | |||
| Diabetes | 50 (32.3) | 13 (21.3) | 37 (39.8) | |
| Hypertension | 35 (22.6) | 18 (29.5) | 16 (17.2) | |
| Glomerulonephritis/HIVAN | 37 (23.9) | 17 (27.9) | 20 (21.5) | |
| Other | 33 (21.3) | 14 (21.5) | 20 (21.5) | |
| PD as first modality | 103 (66.5) | 42 (67.7) | 60 (64.5) | 0.58 |
| Time to first use, n (%) | 0.10 | |||
| ≥2 months | 130 (83.9) | 48 (77.4) | 82 (88.1) | |
| <2 months | 19 (12.3) | 10 (16.1) | 9 (9.7) | |
| Unknown/never used | 6 (3.8) | 4 (6.5) | 2 (2.2) | |
| Prior abdominal surgery, n (%) | 3 | 0 (0) | 3 (3.2) | 0.17 |
Other causes of ESRD included interstitial nephritis (n = 2), amyloidosis (n = 2), medication induced (n = 6), polycystic kidney disease (n = 5), congenital (n = 3), sickle-cell disease (n = 1), chronic rejection post-transplant (n = 1), acute kidney injury (n = 2) and unknown (n = 11).
IQR, interquartile range; HIVAN, HIV-associated nephropathy.
Complications and outcomes
The infectious and noninfectious complications of patients with catheters placed by Y-TEC peritoneoscopic techniques are shown in Table 2. The most common infectious complication was peritonitis, which occurred in 26% of patients. The most common noninfectious complication was scrotal leak, occurring in 4.8% of patients. There were no complications of hernias or catheter migration seen in the Y-TEC peritoneoscopically placed catheters. During follow-up, 8 (13%) patients lost their catheters. The most common reason for catheter loss was peritonitis in three patients. Other causes included mechanical dysfunction in two patients, abdominal wall leak in one patient and pleuroperitoneal fistula in one patient. One patient had a malposition; however, a new catheter was placed immediately. When comparing survival of Y-TEC placed catheters with those placed by open technique in a secondary analysis, although this difference was not statistically significant (Table 2).
Table 2.
Infectious and noninfectious catheter complications with associated catheter loss
| Total, n | Patients with Y-TEC peritoneoscopic catheter placement (n = 62), n (%) | Patients with open catheter placement (n = 93), n (%) | P-value | |
|---|---|---|---|---|
| Infectious complications | ||||
| Only peritonitis | 55 | 16 (26) | 39 (42) | 0.05 |
| Exit site infection | 27 | 10 (16.1) | 17 (18.3) | 0.45 |
| Tunnel infection | 11 | 3 (5) | 8 (8.6) | 0.80 |
| Noninfectious complications | ||||
| Scrotal leak | 7 | 3 (4.8) | 4 (4.3) | 0.34 |
| Hernias | 3 | 0 (0) | 3 (3.2) | 0.55 |
| Catheter migration | 2 | 0 (0) | 2 (2.2) | 0.90 |
| Subcutaneous hematoma | 2 | 1 (1.6) | 1 (1.1) | 0.54 |
| Adhesions | 2 | 1 (1.6) | 1 (1.1) | 0.54 |
| Omental adherence | 2 | 1 (1.6) | 1 (1.1) | 0.54 |
| Pleuroperitoneal fistula | 1 | 0 (0) | 1 (1.1) | 0.90 |
In a secondary analysis, comparing the survival of Y-TEC-placed catheters with those placed by the open technique, there was no difference in hazard ratios in catheter survival after adjusting for demographics, diabetes status and the number of previous catheter placements for overall follow-up. However, at 2 years of follow-up, open placement of catheters had a higher adjusted hazard ratio for catheter loss compared with Y-TEC peritoneoscopic placement [2.53 (95% CI 0.98–6.68), P = 0.06], which was close to statistical significance (Table 3.) This is likely since a majority of catheters were lost within 24 months, with the mean time to catheter loss being 18 months. The Kaplan–Meier curves for time to catheter loss are shown in Figure 1.
Table 3.
Multivariable Cox proportional hazards for catheter loss
| Hazard ratio (95% CI) | P-value | |
|---|---|---|
| Peritoneoscopic placement | 1 (Ref) | NA |
| Open placement | 2.53 (0.98–6.68) | 0.06 |
| Age | 0.99 (0.96–1.02) | 0.79 |
| Female | 1 (Ref) | |
| Male | 1.02 (0.42–2.46) | 0.82 |
| White | 1 (Ref) | NA |
| African/American or other | 0.65 (0.25–1.72) | 0.39 |
| Diabetes mellitus | 1.06 (0.41–2.71) | 0.91 |
| Body mass index | 1.07 (0.99–1.16) | 0.08 |
Fig. 1.
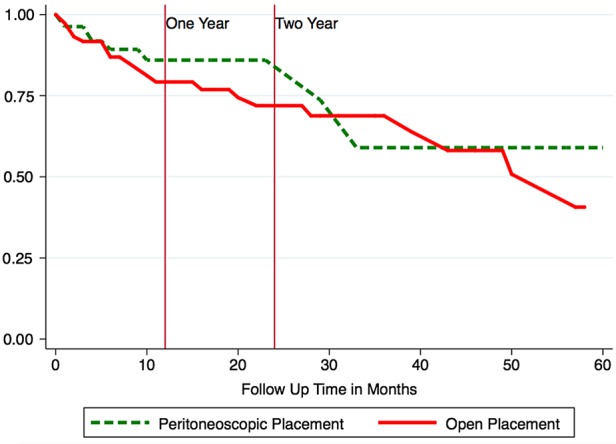
Catheter cumulative survival stratified by placement technique. This figure shows Kaplan–Meier curves for catheter loss by catheter placement technique. The solid red line denotes open placement of catheters, while the dotted green line denotes peritoneoscopic placement over the follow-up period in months. The two vertical maroon lines denote time intervals of 1 and 2 years of follow-up.
Discussion
In this article we present one of the largest series of Y-TEC peritoneoscopically placed PD catheters by a surgeon. We report an overall catheter survival rate comparable with previous reports of laparoscopic or open placement [8, 11–13], with an average of 80% survival at 2 years. Gadallah et al. [12] showed that a peritoneoscopically placed catheter (using Y-TEC) had fewer complications and higher survival rates compared with those placed by an open technique. A recent meta-analysis showed that peritoneoscopically placed catheters had a better 1-year survival and also less catheter migration than those placed via an open approach [10]. We also observed catheter leak occurring in 4.9% of patients, which is much lower than previously described [11, 14]. Also, our rate of mechanical complications was 11%, compared with 17.8% in a recent study by Ouyang et al. [8]. Our report shows that Y-TEC peritoneoscopically placed catheters had a low complication rate and a similar survival rate compared with those placed surgically by an open technique.
With regards to the type of catheter used, a recent systematic review and meta-analysis by Hagen et al. [9] favored survival of straight versus coiled PD catheters. Since all of our patients, except one, had coiled PD catheters, we are unable to compare differences in outcome between the two types of catheters. However, the fact that we did not find differences in outcome in our catheters compared with other published experiences with a greater use of straight catheters suggests that coiled catheters might be as safe.
A majority of the PD catheters in the USA are placed by surgeons and by an open or laparoscopic technique. The peritoneoscopic technique has the advantage that it is done under local sedation, as opposed to a laparoscopic approach that is done with general anesthesia. Moreover, this technique allows acute use of the catheter as opposed to laparoscopy, which requires a healing time of at least 2 weeks. This report provides evidence that peritoneoscopically placed PD catheters could be utilized as a procedure of choice among surgeons providing access for PD.
In summary, this decade-long, single-center experience with peritoneoscopically placed PD catheters by a surgeon demonstrated similar catheter survival rates but lower mechanical complications rates compared with previous reported studies using open or laparoscopic placement. Also of interest, coiled PD catheters showed no significant difference in outcome compared with straight catheters.
Conflict of interest statement
The authors report no conflict of interest. The results presented in this article have not been published previously in whole or in part, except in abstract format.
References
- 1.Fenton SS, Schaubel DE, Desmeules M, et al. Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. Am J Kidney Dis 1997; 30: 334–342 [DOI] [PubMed] [Google Scholar]
- 2.Vonesh EF, Snyder JJ, Foley RN, et al. The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int 2004; 66: 2389–2401 [DOI] [PubMed] [Google Scholar]
- 3.Merkus MP, Jager KJ, Dekker FW, et al. Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. The Necosad Study Group. Am J Kidney Dis 1997; 29: 584–592 [DOI] [PubMed] [Google Scholar]
- 4.Coles GA, Williams JD. What is the place of peritoneal dialysis in the integrated treatment of renal failure? Kidney Int 1998; 54: 2234–2240 [DOI] [PubMed] [Google Scholar]
- 5.Rubin HR, Fink NE, Plantinga LC, et al. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA 2004; 291: 697–703 [DOI] [PubMed] [Google Scholar]
- 6.Saxena R. Peritoneal dialysis: a viable renal replacement therapy option. Am J Med Sci 2005; 330: 36–47 [DOI] [PubMed] [Google Scholar]
- 7.Xie J, Kiryluk K, Ren H, et al. Coiled versus straight peritoneal dialysis catheters: a randomized controlled trial and meta-analysis. Am J Kidney Dis 2011; 58: 946–955 [DOI] [PubMed] [Google Scholar]
- 8.Ouyang C-J, Huang F-X, Yang Q-Q, et al. Comparing the incidence of catheter-related complications with straight and coiled Tenckhoff catheters in peritoneal dialysis patients—a single-center prospective randomized trial. Perit Dial Int 2015; 35: 443–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hagen SM, Lafranca JA, IJzermans JNM, et al. A systematic review and meta-analysis of the influence of peritoneal dialysis catheter type on complication rate and catheter survival. Kidney Int 2014; 85: 920–932 [DOI] [PubMed] [Google Scholar]
- 10.Hagen SM, Lafranca JA, Steyerberg EW, et al. Laparoscopic versus open peritoneal dialysis catheter insertion: a meta-analysis. PLoS One 2013; 8: e56351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh N, Davidson I, Minhajuddin A, et al. Risk factors associated with peritoneal dialysis catheter survival: a 9-year single-center study in 315 patients. J Vasc Access 2010; 11: 316–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gadallah MF, Pervez A, el-Shahawy MA, et al. Peritoneoscopic versus surgical placement of peritoneal dialysis catheters: a prospective randomized study on outcome. Am J Kidney Dis 1999; 33: 118–122 [DOI] [PubMed] [Google Scholar]
- 13.Medani S, Hussein W, Shantier M, et al. Comparison of percutaneous and open surgical techniques for first-time peritoneal dialysis catheter placement in the unbreached peritoneum. Perit Dial Int 2015; 35: 576–585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Al-Hwiesh AK. Percutaneous versus laparoscopic placement of peritoneal dialysis catheters: simplicity and favorable outcome. Saudi J Kidney Dis Transpl 2014; 25: 1194–1201 [DOI] [PubMed] [Google Scholar]


