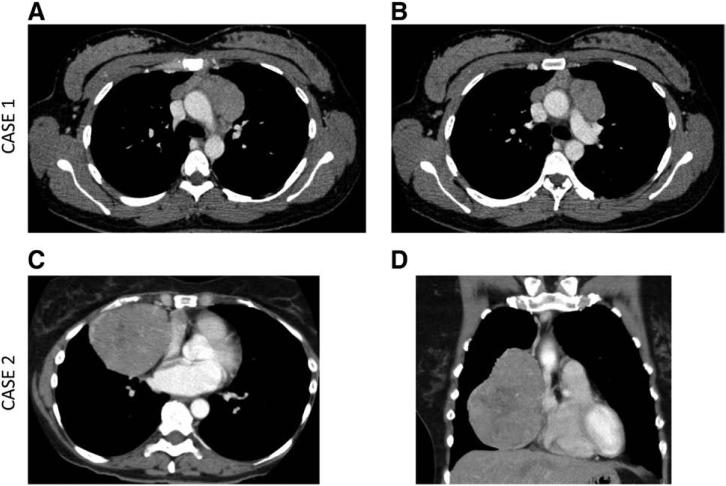
We describe the first cases in the literature, to our knowledge, of pruritus as a paraneoplastic symptom of thymoma. The first case is a 36-year-old woman who developed significant generalized pruritus without rash during her second pregnancy, which did not resolve after delivery and which was recalcitrant to topical steroids, antihistamines, and dry skin care. An extensive pruritus laboratory workup was performed and was negative (Table 1). A chest computed tomography (CT) performed 14 months after the onset of pruritus demonstrated a 7.5 × 4.3 cm anterior mediastinal mass that infiltrated the mediastinal fat and abutted the great vessels (Fig. 1A and B; Table 2). CT-guided fine needle aspiration of the mass and a repeat core biopsy was nondiagnostic but consistent with thymic sampling. Immunohistochemistry for Hodgkin's disease (HD) was negative. Based on the very high clinical suspicion of thymoma, she underwent three cycles of neoadjuvant cisplatin, cyclophosphamide, and doxorubicin chemotherapy with good response. Her pruritus resolved 3 days after her first cycle. She had a complete thymectomy, and final pathology demonstrated a Masaoka-Koga stage II World Health Organization type B2 thymoma. The patient is undergoing surveillance, without recurrence of disease or pruritus, now 2 years postoperatively.
TABLE 1.
Evaluation of Pruritus
| Evaluation | Case 1 | Case 2 |
|---|---|---|
| Distribution of pruritus | Generalized but most bothersome on bilateral lower extremities and hands and feet | Generalized but most bothersome on upper extremities and back |
| Interventions attempted | No resolution after a normal vaginal delivery No improvement with antihistamines, topical moisturizers, or topical steroids |
None |
| Constitutional symptoms, including fevers, night sweats, unintentional weight loss >10% | None | None |
| Physical examination, including skin, lymph node, liver/spleen examination | Normal | Normal |
| Thyroid-stimulating hormone | Normal | N/A |
| Complete blood count + differential | Normal | Normal |
| Serum chemistry/renal function | Normal | Normal |
| Serum liver function tests | Normal | N/A |
| Serum lactate dehydrogenase | Normal | N/A |
| Serum erythrocyte sedimentation rate and C-reactive protein | Normal | N/A |
| Other autoimmune work-upa | N/A | Negative |
| Hepatitis B + C panel | Negative | N/A |
| Other infectious work-upb | Negative | N/A |
| Right upper quadrant ultrasound | Normal, no cholelithiasis | N/A |
| Change in medications | No | No |
Case 2 had the following autoimmune workup: antinuclear antibody, rheumatoid factor, cyclic citrullinated peptide antibody IgG, anti-neutrophil cytoplasmic antibody, myeloperoxidase antibody, proteinase-3 antibody, SCL-70 antibody, Sjogren's screen (anti-SS-A/Ro and anti-SS-B/La antibodies).
Case 1 had toxoplasma, strongyloides, and quantiFERON-tuberculosis serologies sent.
FIGURE 1.
Computed tomography axial views of case 1 demonstrating abutment of proximal great vessels including aorta and pulmonary artery at different planes (A and B). Computed tomography (C) axial view and (D) coronal view of case 2 demonstrating indentation of the right atrium.
TABLE 2.
Characteristics of Cases
| Characteristic | Case 1 | Case 2 |
|---|---|---|
| Baseline CT imaging findings | 7.5 × 4.3 cm left anterior mediastinal lobulated, homogeneous mass Infiltrates the mediastinal fat Abuts mediastinal vessels (superior vena cava, descending aorta, and main pulmonary artery) |
9.2 × 7.7 × 11.7 cm right anteromedial mediastinal well-circumscribed, lobulated, heterogeneous mass Moderate indentation of the right atrium Abuts mediastinal vessels (aorta, superior vena cava) and right lung |
| Pre-surgical biopsy | Yes CT-guided FNA (nondiagnostic) CT-guided biopsy (nondiagnostic) |
Yes CT-guided biopsy (diagnostic for thymoma) |
| Clinical Masaoka-Koga stage | III | I or II |
| Neoadjuvant therapy | Yes CAP chemotherapy × 3 cycles |
No |
| Operative findings | Well-circumscribed main tumor mass towards the left of midline and a much smaller, apparently separate 2 cm well-circumscribed tumor mass to the right of midline | Encapsulated tumor Nodule palpated in right upper lobe |
| Type of resection | Median sternotomy approach: complete thymectomy and radical mediastinal dissection | Median sternotomy approach: complete thymectomy, radical mediastinal dissection, and wedge excision of RUL lung nodule |
| Pathologic Masaoka-Koga stage | II No clearly defined capsule -well-defined, discrete, microscopic foci of thymic tumor scattered throughout the surrounding mediastinal fat |
I Encapsulated tumor Wedge RUL biopsy showed an organizing pneumonia pattern |
| WHO type | B2 | AB |
| Resection statusa | R0 | R0 |
| Adjuvant therapy | None | None |
FNA, fine needle aspiration; CAP, cisplatin, cyclophosphamide, and doxorubicin; RUL, right upper lobe; WHO, World Health Organization.
Resection status: R0 = complete, R1 = microscopic, and R2 = macroscopic.
The second case is a 60-year-old woman who presented with 12 months of intermittent generalized pruritus without rash. A pruritus laboratory workup was negative (Table 1). A family history revealed HD in a maternal grandmother. A chest radiograph obtained routinely for work showed an anterior mediastinal mass. CT revealed a 9.2 × 7.7 × 11.7 cm mass, with indentation of the right atrium (Fig. 1C and D; Table 2). CT-guided core biopsy was consistent with thymoma. Clinically, she had a stages I or II thymoma and underwent a complete thymectomy. Final pathology demonstrated a Masaoka-Koga stage I World Health Organization type AB thymoma. Her pruritus resolved immediately after surgery. She is undergoing surveillance, without recurrence of disease or pruritus, now 2 years postoperatively.
DISCUSSION
To our knowledge, this is the first case report of generalized pruritus as a paraneoplastic symptom heralding the diagnosis of thymoma. Paraneoplastic pruritus develops before a clinically evident cancer, is not caused by direct effect of the tumor, and resolves after treatment.1 The most common malignancy associated with generalized pruritus is HD, where the prevalence rate is approximately 20% to 30%, and the severity of pruritus is associated with shorter survival.2 Generalized pruritus without rash can be associated with multiple systemic diseases including liver disease, end-stage renal disease, and as a paraneoplastic symptom of malignancies.1 The standard workup for generalized pruritus without rash (as reported in Table 1) includes evaluation of complete blood count with differential, liver function, renal function, and thyroid function and ruling out malignancy/lymphoma, viral infection (ie, HIV, hepatitis B/C), cholelithiasis, medication-related pruritus, and autoimmune conditions. Skin biopsy in the absence of a primary cutaneous lesion is nonspecific and is of low yield.
Thymomas are frequently associated with autoimmune conditions and paraneoplastic syndromes including myasthenia gravis and pure red cell aplasia.3 Paraneoplastic skin conditions associated with thymoma that have been reported include mixed connective tissue disease, dermatomyositis, systemic lupus erythematous, acrokeratosis, pemphigus, and lichen planus, which each have an associated clinically apparent rash.4
Thymoma is the most common neoplasm of the anterior mediastinum and represents 20% of anterior mediastinal tumors.5 However, the differential diagnosis of an anterior mediastinal mass includes teratoma, seminoma, lymphoma, and also nonmalignant conditions. An anterior mediastinal mass in a patient with generalized pruritus is more likely to be attributed to HD than thymoma. Given the significant upfront treatment differences between HD and thymoma, making the distinction between these two tumors is critical. The differential diagnosis of generalized pruritus in association with an anterior mediastinal mass should also include thymoma.
ACKNOWLEDGMENTS
This work was conducted with support from the TL1 Clinical Research Training Program of the Stanford Clinical and Translational Science Award to Spectrum (NIH TL1 TR 001084; S.K.P.); Stanford Cancer Institute Fellowship Award (S.K.P.); and the National Institutes of Health (K12 CA 138464; J.W.R.).
Footnotes
Disclosures: Dr. Padda (money paid to institution: TL1 Clinical Research Training Program of the Stanford Clinical and Translational Science Award to Spectrum [NIH TL1 TR 001084] and Stanford Cancer Institute Fellowship Award), Dr. Riess (money paid to institution: KL2CTSC award), and Dr. Wakelee (money paid to institution: AstraZeneca). Financial disclosures outside of this submitted work: Dr. Loo (money paid to institution: grants from Varian Medical Systems, RaySearch; money paid to author: Varian Medical Systems for educational symposium lecture and patent coinventor of Stanford patent licensed to Varian Medical Systems); Dr. Neal (money paid to author: consultancy to Clovis Oncology; grants paid to author and/or institution Genentech/Roche, Merck, ArQule, Novartis, Exelixis, Boehringer Ingelheim, Nektar); Dr. Riess (money paid to author: consultancy to Celgene, general education lecture for Celgene/Genentech; money paid to institution: Bonnie J. Addario Lung Cancer Foundation, NIH K12 Career Development Award grants); Dr. Shrager (money paid to author: consultancy to Maquet Inc. Carefusion Inc.; money paid to institution: Varian grants); and Dr. Wakelee (money paid to institution: consultancy to Peregine and grants from Novartis, BMS, Clovis, Xcovery, Celgene, Roche/Genentech, Medimmune, and Pfizer). The following authors have no disclosures: Dr. Hardy, Dr. Liang, Pagtama, Dr. Schwartz, Holmes Tisch, and Dr. Kwong.
REFERENCES
- 1.Yosipovitch G. Chronic pruritus: a paraneoplastic sign. Dermatol Ther. 2010;23:590–596. doi: 10.1111/j.1529-8019.2010.01366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubenstein M, Duvic M. Cutaneous manifestations of Hodgkin's disease. Int J Dermatol. 2006;45:251–256. doi: 10.1111/j.1365-4632.2006.02675.x. [DOI] [PubMed] [Google Scholar]
- 3.Evoli A, Lancaster E. Paraneoplastic disorders in thymoma patients. J Thorac Oncol. 2014;9(9 Suppl 2):S143–S147. doi: 10.1097/JTO.0000000000000300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tormoehlen LM, Pascuzzi RM. Thymoma, myasthenia gravis, and other paraneoplastic syndromes. Hematol Oncol Clin North Am. 2008;22:509–526. doi: 10.1016/j.hoc.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest. 2005;128:2893–2909. doi: 10.1378/chest.128.4.2893. [DOI] [PubMed] [Google Scholar]