Significance
Animal influenza viruses continue to challenge human public health; surveillance of these viruses and evaluation of their pandemic potential are important for future influenza pandemic preparedness. Pigs are intermediate hosts for novel influenza generation and transfer to humans. Two lineages of H1N1 swine influenza viruses (SIVs), classical H1N1 SIVs and Eurasian avian-like H1N1 (EAH1N1) SIVs, have been circulating in pigs since 1918 and 1979, respectively. The classical H1N1 SIVs emerged in humans as a reassortant and caused the 2009 H1N1 influenza pandemic. Here, we found that, after long-term evolution in pigs, the EAH1N1 SIVs have obtained the traits to cause a human influenza pandemic.
Keywords: swine influenza, H1N1, Eurasian lineage, evolution, pandemic potential
Abstract
Pigs are important intermediate hosts for generating novel influenza viruses. The Eurasian avian-like H1N1 (EAH1N1) swine influenza viruses (SIVs) have circulated in pigs since 1979, and human cases associated with EAH1N1 SIVs have been reported in several countries. However, the biologic properties of EAH1N1 SIVs are largely unknown. Here, we performed extensive influenza surveillance in pigs in China and isolated 228 influenza viruses from 36,417 pigs. We found that 139 of the 228 strains from pigs in 10 provinces in China belong to the EAH1N1 lineage. These viruses formed five genotypes, with two distinct antigenic groups, represented by A/swine/Guangxi/18/2011 and A/swine/Guangdong/104/2013, both of which are antigenically and genetically distinct from the current human H1N1 viruses. Importantly, the EAH1N1 SIVs preferentially bound to human-type receptors, and 9 of the 10 tested viruses transmitted in ferrets by respiratory droplet. We found that 3.6% of children (≤10 y old), 0% of adults, and 13.4% of elderly adults (≥60 y old) had neutralization antibodies (titers ≥40 in children and ≥80 in adults) against the EAH1N1 A/swine/Guangxi/18/2011 virus, but none of them had such neutralization antibodies against the EAH1N1 A/swine/Guangdong/104/2013 virus. Our study shows the potential of EAH1N1 SIVs to transmit efficiently in humans and suggests that immediate action is needed to prevent the efficient transmission of EAH1N1 SIVs to humans.
Pigs play a pivotal role in the ecology of influenza A viruses, being regarded as intermediate hosts for the generation of novel and potentially dangerous influenza viruses for humans. Cellular receptors containing α-2,3–linked sialic acids (Sias) (avian-like receptors) and α-2,6–linked Sias (human-like receptors) in the pig trachea favor the productive replication of viruses from both the avian and mammalian lineages (1). Influenza viruses of the subtypes H1N1, H1N2, and H3N2 are circulating in pigs globally (2). Two lineages of H1N1 swine influenza viruses (SIVs), classical H1N1 SIVs and Eurasian avian-like H1N1 (EAH1N1) SIVs, have been circulating in pigs since 1918 and 1979, respectively (3, 4). The classical H1N1 SIVs emerged in humans as a reassortant (2009/H1N1) and caused the 2009 H1N1 influenza pandemic (5). The EAH1N1 SIVs have been detected in pigs in many Eurasian countries (6) and have caused several human infections in European countries and also in China (7–11), where a fatal case was reported (11). EAH1N1 SIVs are reported to be most prevalent in pigs that have been brought into Hong Kong since 2005 (12). However, the evolution and biologic properties of the EAH1N1 SIVs are largely unknown.
China is the largest pork-producing country in the world. Pigs in China are not vaccinated against influenza, and therefore, influenza viruses can spread freely once they are introduced into pig herds. In this study, we performed active surveillance in pigs and found that the EAH1N1 SIVs are predominant in the pig population in China; we further found that the EAH1N1 SIVs pose an imminent threat with regard to their ability to cause a human influenza pandemic.
Results
Surveillance of SIVs in China.
Nasal swabs were collected from 36,417 pigs in slaughterhouses and on farms in 24 provinces in China from August 2010 to March 2013 (SI Appendix, Table S1); 228 SIVs were isolated from these samples, including 180 H1N1, 44 H1N2, 2 H3N2, and 2 H9N2 SIVs. Partial sequence analysis of the hemagglutinin (HA) and neuraminidase (NA) genes of the 180 H1N1 SIVs further classified them as 139 EAH1N1, 39 2009/H1N1-like, and two classical H1N1 SIVs (SI Appendix, Table S1). EAH1N1 SIVs was detected in ten provinces (SI Appendix, Table S1 and Fig. S1). The 2009/H1N1 and H1N2 SIVs were detected in four provinces, respectively, and the classical H1N1, H3N2, and H9N2 SIVs were each detected in only one province (SI Appendix, Table S1). These results indicate that the EAH1N1 is the predominant SIV circulating in pigs in China.
Genetics of EAH1N1 SIVs.
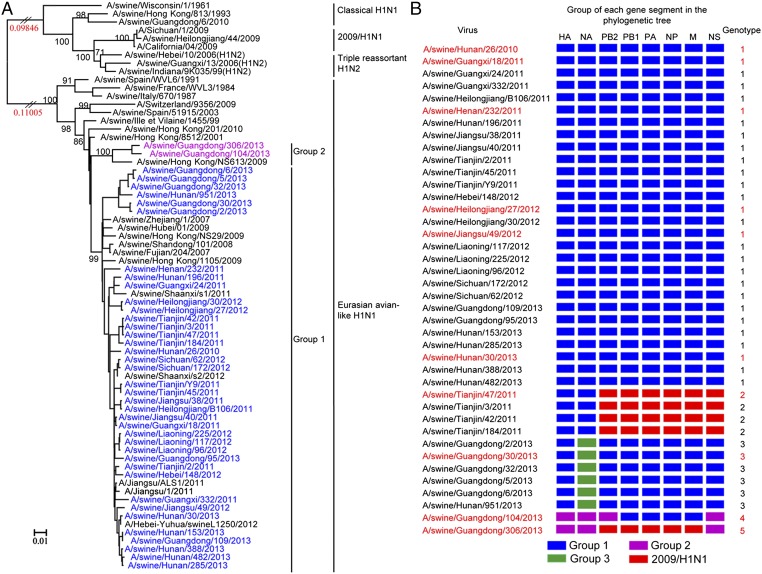
We fully sequenced the genome of 40 representative EAH1N1 SIVs that came from different farms. The HA gene of the 40 SIVs shared 92.7–100% identity at the nucleotide level and formed two phylogenetic groups (Fig. 1A). The NA gene of these SIVs shared 91.1–100% identity at the nucleotide level and formed three phylogenetic groups (SI Appendix, Fig. S2A).
Fig. 1.
Genetic relationships among the HA genes and genotype evolution of EAH1N1 SIVs. (A) Phylogenetic tree of HA. The unrooted tree was based on nucleotides 33–1733. Sequences of viruses with names in black were downloaded from available databases; viruses with names in colors were sequenced in this study. Scale bar indicates the number of nucleotide substitutions per site. (B) Genotypes of the EAH1N1 SIVs. The eight gene segments are indicated at the top of each bar. The colors of the bars represent the groups in the trees of Fig. 1A and SI Appendix, Fig. S2. Viruses shown in red were selected for all other tests.
The six internal genes of the EAH1N1 SIVs showed distinct diversity, with the basic polymerase 2 (PB2), PB1, acidic polymerase (PA), nucleoprotein (NP), matrix (M), and nonstructural protein (NS) genes of the 40 viruses sharing 82.9–100%, 84.1–100%, 83.7–100%, 82.4–100%, 93.6–100%, and 80.1–100% identity, respectively, at the nucleotide level. The PB2 and NS genes each formed three groups (two of which originated from EAH1N1 and the third from 2009/H1N1) in the phylogenetic trees (Fig. 1B and SI Appendix, Fig. S2 B and G), and the PB1, PA, NP, and M genes each formed two groups (one of which originated from EAH1N1 and the other from 2009/H1N1) in their phylogenetic trees (Fig. 1B and SI Appendix, Fig. S2 C–F).
On the basis of this genomic diversity, we divided these EAH1N1 SIVs into five genotypes (Fig. 1B). The SIVs in genotypes 2 and 5 bear six and five internal genes, respectively, from 2009/H1N1 viruses (Fig. 1B). The two SIVs in genotypes 4 and 5 have NS genes derived from the North American H1N2 triple reassortant SIVs rather than from the EAH1N1 SIVs (SI Appendix, Fig. S2G). The genotype 1 SIVs were detected in 10 provinces, whereas the viruses in genotypes 2, 3, 4, and 5 were only detected in one or two provinces (Fig. 1B).
To understand the biologic properties of these EAH1N1 SIVs, we selected 10 strains (red text in Fig. 1B), including six SIVs of genotype 1 and one SIV from each of genotypes 2, 3, 4, and 5, and tested their antigenic properties, receptor-binding preference, virulence, and transmissibility in mammals.
Antigenic Analysis.
The antigenic match between a vaccine and the circulating viruses is one of the most important factors in determining the efficacy of the vaccine. When the prevalent human influenza viruses show a greater than fourfold difference in hemagglutination inhibition (HI) assay titer from the vaccine strain, the immunity induced by the vaccine does not prevent the circulation of such viruses in humans (13). We therefore selected ferret antisera against 2009/H1N1 virus A/Sichuan/1/2009 (SC/1/09), which is from the current H1N1 human influenza vaccine lineage, and against A/swine/Guangxi/18/2011 (SW/GX/18/11) and A/swine/Guangdong/104/2013 (SW/GD/104/13), which contain the HA of group 1 and 2, respectively, for antigenic analysis.
The antiserum against SC/1/09 cross-reacted with the EAH1N1 SIVs bearing the HA of group 1 and 2 with titers four- to eightfold and 64–128-fold, respectively, lower than the homologous titer. The antiserum against SW/GX/18/11 reacted well with the EAH1N1 SIVs bearing the HA of group 1, but its cross-reactive titers with 2009/H1N1 and the EAH1N1 SIVs bearing the HA of group 2 were fourfold and 32–128-fold, respectively, lower than the homologous titer. The antiserum against SW/GD/104/13 reacted well with the EAH1N1 SIVs bearing the HA of group 2, but its cross-reactive titers with the EAH1N1 SIVs bearing the HA of group 1 and with 2009/H1N1 were 32–64-fold and 128-fold, respectively, lower than the homologous titer (Table 1). We found 23 amino acid differences in the HA antigenic sites among these viruses (SI Appendix, Table S2). Which amino acid contributes to these observed antigenic differences has yet to be determined. Our results indicate that the EAH1N1 SIVs formed two distinct antigenic groups and both groups show a striking antigenic difference from the 2009/H1N1 virus.
Table 1.
Antigenic analysis of the EAH1N1 SIVs
| Virus | HA group | Ferret antisera | ||
| SC/1/09 | SW/GX/18/11 | SW/GD/104/13 | ||
| SC/1/09 | 2009/H1N1 | 1280 | 320 | 10 |
| SW/GX/18/11 | 1 | 320 | 1280 | 20 |
| SW/GD/104/13 | 2 | 10 | 40 | 1280 |
| Test viruses | ||||
| SW/HuN/26/10 | 1 | 160 | 640 | 40 |
| SW/TJ/47/11 | 1 | 320 | 320 | 20 |
| SW/HeN/232/11 | 1 | 320 | 640 | 40 |
| SW/HLJ/27/12 | 1 | 320 | 1280 | 40 |
| SW/JS/49/12 | 1 | 160 | 640 | 40 |
| SW/HuN/30/13 | 1 | 160 | 1280 | 20 |
| SW/GD/30/13 | 1 | 320 | 640 | 20 |
| SW/GD/306/13 | 2 | 20 | 10 | 640 |
Ferrets were inoculated intranasally with 106 EID50 of the indicated virus, and sera were collected 3 wk postinoculation. Homologous titers are underlined and bolded.
Receptor-Binding Preference.
We tested the receptor-binding specificity of the EAH1N1 SIVs by using a solid-phase binding assay with four different glycans as described previously (14, 15). The SC/1/09, and an H5N1 virus, A/duck/Anhui/1/2006, were included for comparison. The SC/1/09 and all 10 EAH1N1 SIVs bound to α-2,6–linked Sias with high affinity and to α-2,3–linked Sias with very low affinity (SI Appendix, Fig. S3 A–J and L), whereas the H5N1 virus bound to α-2,3–linked Sias with high affinity and to α-2,6–linked Sias with very low affinity (SI Appendix, Fig. S3K). These results indicate that the EAH1N1 SIVs preferentially bind to the human-type receptor.
Replication and Virulence in Mice.
We investigated the virulence in mice of the EAH1N1 SIVs as described previously (16). The 10 EAH1N1 SIVs replicated in the lungs of mice, nine SIVs were detected in the nasal turbinate of mice, and two were also detected in the kidneys (SI Appendix, Fig. S4). No virus was detected in the spleen or brain of any mice. Mice infected with these SIVs lost 7–29.1% of their body weight, and two SIVs, A/swine/Guangdong/30/2013 (SW/GD/30/13) and A/swine/Guangdong/306/2013 (SW/GD/306/13), killed 40% and 60% of the mice, respectively (SI Appendix, Fig. S4).
Replication and Transmission of EAH1N1 SIVs in Ferrets.
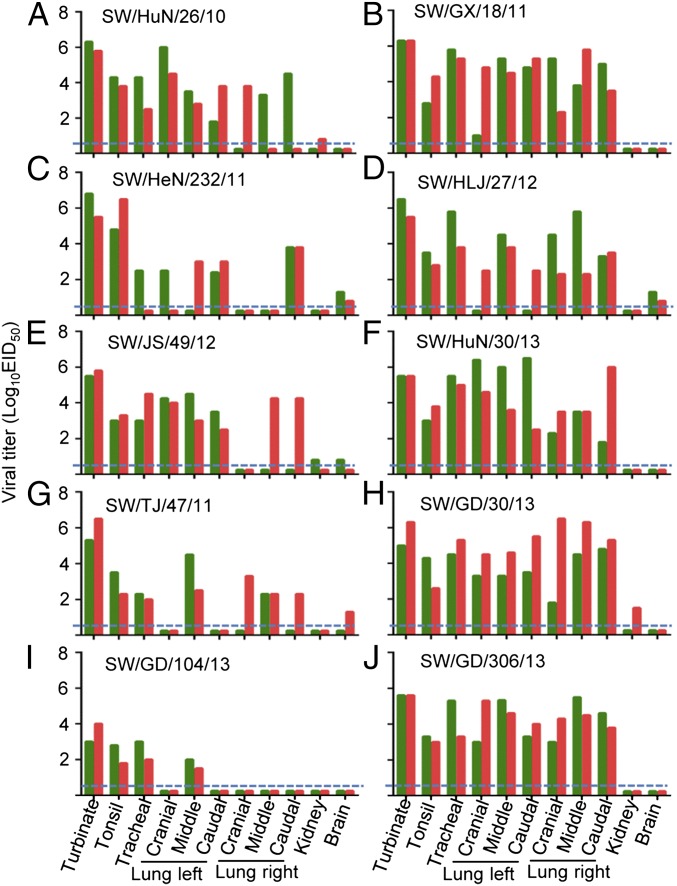
Two ferrets were inoculated intranasally (i.n.) with 106.0 50% egg infectious dose (EID50) of each virus, and organs from each ferret were collected on day 4 postinoculation (p.i.) for virus titration in eggs. All 10 of the viruses replicated in the nasal turbinate, tonsils, and trachea of the ferrets (Fig. 2). Virus was detected in all lung lobes of the ferrets inoculated with six of the viruses (Fig. 2 A, B, D, F, H, and J) but was not detectable in some of the lung lobes of ferrets inoculated with the other four viruses (Fig. 2 C, E, G, and I). Virus was detected in the kidneys of one ferret inoculated with A/swine/Hunan/26/2010 (SW/HuN/26), A/swine/Jiangsu/49/2012 (SW/JS/49/12), and SW/GD/30/13 (Fig. 2 A, E, and H). Virus was also detected in the brain of one ferret in each of the groups that were inoculated with SW/JS/49/12 and A/swine/Tianjin/47/2011 (SW/TJ/47/11) (Fig. 2 E and G) and in two ferrets in each of the groups that were inoculated with A/swine/Henan/232/2011 (SW/HeN/232/11) and A/swine/Heilongjiang/27/2012 (SW/HLJ/27/12) (Fig. 2 C and D).
Fig. 2.
Replication of EAH1N1 SIVs in ferrets. Ferrets (n = 2 per group) were inoculated i.n. with 106.0 EID50 of each virus, and the indicated organs from each ferret were collected on day 4 p.i. for virus titration in eggs. Each color bar represents the virus titer from an individual animal. The dashed blue lines indicate the lower limit of detection. (A) SW/HuN/26/10, (B) SW/GX/18/11, (C) SW/HeN/232/11, (D) SW/HLJ/27/12, (E) SW/JS/49/12, (F) SW/HuN/30/13, (G) SW/TJ/47/11, (H) SW/GD/30/13, (I) SW/GD/104/13, and (J) SW/GD/306/13.
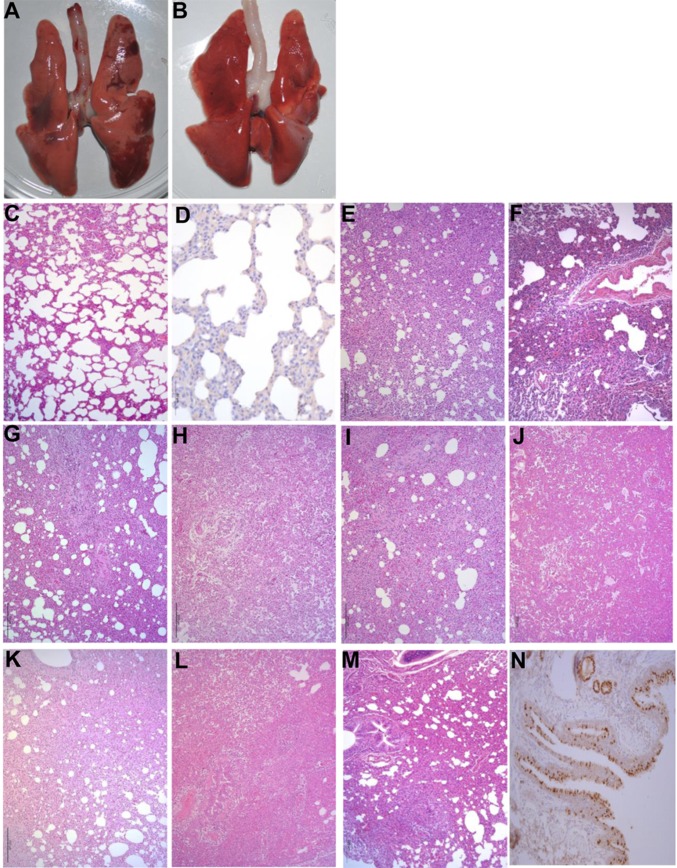
Macroscopic lesions were observed in the lungs of ferrets inoculated with all of the SIVs, except for those inoculated with SW/GD/104/13 (Fig. 3 A and B). Pathological studies indicated that most of the lungs showed mild damage after infection with SW/GD/104/13 (Fig. 3C), and viral antigen was not detected (Fig. 3D). By contrast, the lungs of the other nine virus-infected ferrets showed severe bronchopneumonia (Fig. 3 E–M), and viral antigen was detected in the epithelial cells of the bronchus and alveoli (Fig. 3N).
Fig. 3.
Lung lesions caused by EAH1N1 SIVs in ferrets. Macroscopic lesions in the lungs and focal consolidations in dark red were observed in the lobes of ferrets inoculated with all of the EAH1N1 viruses (A; the image is from an SW/HuN/30/13-inoculated ferret), except for SW/GD/104/13, which did not cause obvious macroscopic lesions in the lungs of ferrets (B). Only mild histopathological changes were observed in the lungs of SW/GD/104/13-inoculated ferrets (C) (H&E staining), and viral antigen was not detected (D) (immunohistochemical staining), whereas the lungs of ferrets inoculated with SW/HuN/26/10, SW/GX/18/11, SW/HeN/232/11, SW/HLJ/27/12, SW/JS/49/12, SW/HuN/30/13, SW/TJ/47/11, SW/GD/30/13, and SW/GD/306/13 viruses showed severe pathological lesions (E–M) (H&E staining). Viral antigen was detected in the epithelial cells of the bronchus and alveoli by means of immunohistochemical staining (N, from the lung sample of a ferret inoculated with SW/HuN/30/13 virus). Images C and E–M were taken at 100× magnification; images D and N were taken at 400× magnification.
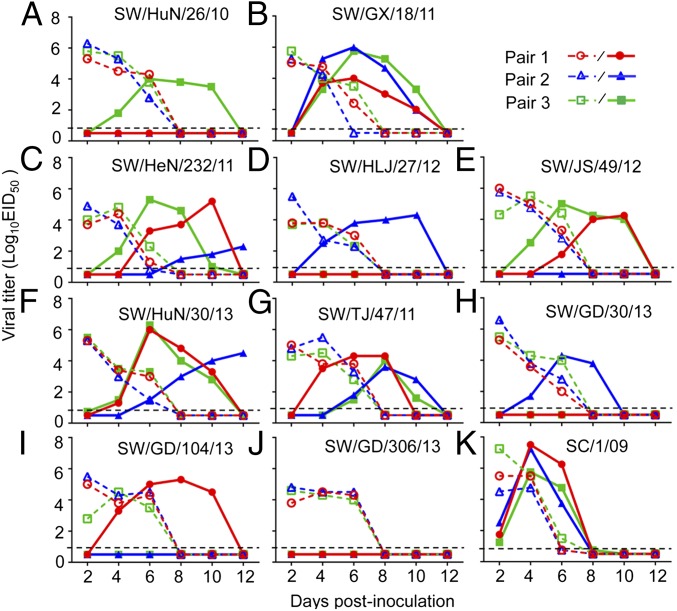
Respiratory droplet transmission was assessed in ferrets as described previously (15, 16). The highly transmissible SC/1/09 was included as a control (14, 17). Virus was detected in all of the directly infected animals (Fig. 4 A–K). In the exposed groups, virus was not detected in any of the animals exposed to the SW/GD/306/13-inoculated ferrets (Fig. 4J), but virus was detected in one ferret exposed to the ferrets that had been inoculated with SW/HuN/26/10, SW/HLJ/27/12, SW/GD/104/13, and SW/GD/30/13 (Fig. 4 A, D, H, and I) and in two ferrets exposed to the ferrets that had been inoculated with SW/JS/49/12 (Fig. 4E). Importantly, like the 2009/H1N1 SC/1/09 virus (Fig. 4K), four EAH1N1 SIVs—SW/GX/18/11, SW/HeN/232/11, A/swine/Hunan/30/2013 (SW/HuN/30/13), and SW/TJ/47/11—transmitted to all three exposed ferrets (Fig. 4 B, C, F, and G). The ferrets that were inoculated with these EAH1N1 SIVs experienced a 0.2–18.6% body weight loss, and the exposed ferrets lost up to 21% of their body weight (Table 2 and SI Appendix, Table S4). Seroconversion occurred in all of the virus-inoculated animals and in all exposed animals that were virus-positive (Table 2).
Fig. 4.
Respiratory droplet transmission of EAH1N1 SIVs in ferrets. Each line represents the virus titer from an individual animal. The dashed lines indicate the values from the inoculated animals; the solid lines indicate the values from the exposed animals. The dashed black lines indicate the lower limit of detection. (A) SW/HuN/26/10, (B) SW/GX/18/11, (C) SW/HeN/232/11, (D) SW/HLJ/27/12, (E) SW/JS/49/12, (F) SW/HuN/30/13, (G) SW/TJ/47/11, (H) SW/GD/30/13, (I) SW/GD/104/13, (J) SW/GD/306/13, and (K) SC/1/09.
Table 2.
Replication, virulence, and transmission of EAH1N1 SIVs in ferrets
| Virus (genotype) | Maximum body temperature increase, °C | Maximum body weight loss, % | Seroconversion (HI antibody titer range) | |||
| Inoculated | Exposed | Inoculated | Exposed | Inoculated | Exposed | |
| SW/HuN/26/10 (1) | 2.2 | 1.4 | 0.8 | 5.6 | 3/3 (640–1280) | 1/3 (1280) |
| SW/GX/18/11 (1) | 1.7 | 0.9 | 17.9 | 21.0 | 3/3 (1280–2560) | 3/3 (640-5120) |
| SW/HeN/232/11 (1) | 1.9 | 1.2 | 18.6 | 14.0 | 3/3 (1280–2560) | 3/3 (1280–2560) |
| SW/HLJ/27/12 (1) | 1.0 | 0.6 | 15.2 | 11.7 | 3/3 (1280) | 1/3 (2560) |
| SW/JS/49/12 (1) | 2.1 | 1.2 | 5.6 | 12.3 | 3/3 (1280–2560) | 2/3 (1280) |
| SW/HuN/30/13 (1) | 1.5 | 1.2 | 3.4 | 9.4 | 3/3 (2560–5120) | 3/3 (1280–5120) |
| SW/TJ/47/11 (2) | 1.4 | 1.0 | 12.9 | 7.1 | 3/3 (1280) | 3/3 (640–1280) |
| SW/GD/30/13 (3) | 1.0 | 0.5 | 3.2 | 4.6 | 3/3 (1280) | 1/3 (640) |
| SW/GD/104/13 (4) | 1.0 | 0.6 | 1.8 | 1.0 | 3/3 (1280) | 1/3 (1280) |
| SW/GD/306/13 (5) | 1.6 | 0.6 | 10.3 | 0.0 | 3/3 (320–1280) | 0/3 |
| SC/1/09 (2009/H1N1) | 2.2 | 2.3 | 10.1 | 21.2 | 3/3 (320–1280) | 3/3 (640–1280) |
Data shown are from the animal in that group with the maximum body temperature increase or maximum body weight loss. The data for all of the animals in each group are reported in SI Appendix, Table S4. Seroconversion was confirmed from ferret serum that was collected on day 21 postinoculation.
Human Immunity to the EAH1N1 Viruses.
Serum HI antibody titers of 40 (18, 19), or microneutralization (MNT) antibody titers of 40 in children or at least 80 in adults, are associated with no less than a 50% reduction in risk of infection or disease with influenza viruses in human populations (20). To investigate whether humans have any existing immune protection against the EAH1N1 SIVs, we tested sera collected from children (<10 y old, n = 55), adults (25–53 y old, n = 52), and elderly adults (≥60 y old, n = 52), against three viruses (SC/1/09, SW/GX/18/11, and SW/GD/104/13) for both HI and MNT antibodies as described previously (20, 21). We found that only 9.1%, 5.5%, and 0% of the children; 7.7%, 11.5%, and 3.8% of the adults; and 1.9%, 3.8%, and 0% of the elderly adults had HI antibody titers ≥40 to SC/1/09, SW/GX/18/11, and SW/GD/104/13, respectively (SI Appendix, Table S5). In addition, 12.7%, 3.6%, and 0% of the children had MNT antibody titers ≥40, and 1.9%, 0%, and 0% of the adults and 0%, 13.4%, and 0% of the elderly adults had MNT antibody titers ≥80 to SC/1/09, SW/GX/18/11, and SW/GD/104/13, respectively (SI Appendix, Table S5). These results indicate that the preexisting immunity in the human population may not be able to prevent the spread of the EAH1N1 SIVs.
Discussion
Here, we detected different subtypes of SIVs in pigs in China from 2010 to 2013 and found that the predominant strains are the EAH1N1 SIVs, which have evolved into five different genotypes through accumulated mutations or the acquisition of different internal gene segments from viruses in other lineages. We further determined that the EAH1N1 SIVs have formed two distinct antigenic groups and exhibit markedly different antigenicity from that of the 2009/H1N1 pandemic virus. Most importantly, we found that these SIVs preferentially or exclusively bind human-like receptors and that some of them can transmit efficiently between ferrets by respiratory droplet.
Several amino acid changes in PB2 are important for the replication or virulence of influenza viruses in mammals (22–30). A detailed comparison of the amino acid differences among the EAH1N1 SIVs indicated that all of these viruses have mammalian-adapting mutations in their PB2 genes (SI Appendix, Table S3). Therefore, although the EAH1N1 viruses do not cause severe disease in pigs and have different replication and virulence phenotypes in animal models, they may be able to replicate well and possibly cause appreciable disease in humans, as observed during the 2009/H1N1 influenza pandemic (31).
The human influenza vaccination coverage in China is less than 2% (32). Although we cannot attribute the seropositivity of humans against H1N1 viruses to vaccination or natural infection, the overall seropositive rate to the EAH1N1 SIVs in humans is low. Two doses of the seasonal trivalent inactivated influenza vaccine could not substantially improve the levels of cross-reactive antibodies to the EAH1N1 virus in humans (10). Thus, preexisting immunity in humans may not be sufficient to overcome EAH1N1 SIV infection.
Numerous studies have evaluated the pandemic potential of animal influenza viruses (14–17, 22, 33–39). Although H5N1 mutants and reassortants have been shown to be transmissible in ferrets or guinea pigs (14, 33, 35, 36), none of the naturally occurring H5N1 viruses is transmissible via respiratory droplet in these animal models. Certain H7N9 viruses are transmissible in ferrets (15, 40), but their circulation so far is geographically restricted. The Centers for Disease Control and Prevention in the United States developed a risk assessment tool to evaluate the pandemic potential of different influenza strains (41). By using this tool, we found that the EAH1N1 SIVs got the highest risk score among six different subtypes of viruses (SI Appendix, Table S6), suggesting that the EAH1N1 SIVs may pose the highest pandemic threat among the influenza viruses currently circulating in animals.
Methods
This study was carried out in accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the Ministry of Science and Technology of China (42). The protocols were reviewed and approved by the Committee on the Ethics of Animal Experiments of the Harbin Veterinary Research Institute of the Chinese Academy of Agricultural Sciences. All experiments with live H1N1 viruses were conducted within the enhanced animal biosafety level 2-plus facilities in the Harbin Veterinary Research Institute of the Chinese Academy of Agricultural Sciences. The researchers who work with mice and ferrets wear N95 masks and disposable overalls; they shower on exiting the facility.
The detailed methods for this study are provided in SI Appendix.
Supplementary Material
Acknowledgments
We thank Susan Watson for editing the manuscript and the Consortium for Functional Glycomics (Scripps Research Institute) for providing the glycans. This work was supported by the National Natural Science Foundation of China (31302108 and 31521005), the Food and Agriculture Organization of the United Nations (CHN/2013/001/LOA), and the Japan Initiative for Global Research Network on Infectious Diseases from the Japan Agency for Medical Research and Development.
Footnotes
Conflict of interest statement: Y.K. has received speaker’s honoraria from Toyama Chemical and Astellas Inc.; has received grant support from Chugai Pharmaceuticals, Daiichi Sankyo Pharmaceutical, Toyama Chemical, Tauns Laboratories, Inc., and Otsuka Pharmaceutical Co., Ltd; and is a founder of FluGen.
Data deposition: Virus sequence data from this study were deposited in the Global Initiative on Sharing Avian Influenza Data database http://platform.gisaid.org/ (accession nos. EPI554268–EPI554539).
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1522643113/-/DCSupplemental.
References
- 1.Ito T, et al. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J Virol. 1998;72(9):7367–7373. doi: 10.1128/jvi.72.9.7367-7373.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown IH. The epidemiology and evolution of influenza viruses in pigs. Vet Microbiol. 2000;74(1-2):29–46. doi: 10.1016/s0378-1135(00)00164-4. [DOI] [PubMed] [Google Scholar]
- 3.Shope RE. Swine influenza: I. Experimental transmission and pathology. J Exp Med. 1931;54(3):349–359. doi: 10.1084/jem.54.3.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pensaert M, Ottis K, Vandeputte J, Kaplan MM, Bachmann PA. Evidence for the natural transmission of influenza A virus from wild ducts to swine and its potential importance for man. Bull World Health Organ. 1981;59(1):75–78. [PMC free article] [PubMed] [Google Scholar]
- 5.Garten RJ, et al. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325(5937):197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vincent A, et al. Review of influenza A virus in swine worldwide: A call for increased surveillance and research. Zoonoses Public Health. 2014;61(1):4–17. doi: 10.1111/zph.12049. [DOI] [PubMed] [Google Scholar]
- 7.de Jong JC, et al. Isolation of swine-like influenza A(H1N1) viruses from man in Switzerland and The Netherlands. Ann Inst Pasteur Virol. 1988;139(4):429–437. doi: 10.1016/s0769-2617(88)80078-9. [DOI] [PubMed] [Google Scholar]
- 8.Myers KP, Olsen CW, Gray GC. Cases of swine influenza in humans: A review of the literature. Clin Infect Dis. 2007;44(8):1084–1088. doi: 10.1086/512813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang H, et al. Human infection from avian-like influenza A (H1N1) viruses in pigs, China. Emerg Infect Dis. 2012;18(7):1144–1146. doi: 10.3201/eid1807.120009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang DY, et al. Human infection with Eurasian avian-like influenza A(H1N1) virus, China. Emerg Infect Dis. 2013;19(10):1709–1711. doi: 10.3201/eid1910.130420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Qi X, et al. Antigenic and genetic characterization of a European avian-like H1N1 swine influenza virus from a boy in China in 2011. Arch Virol. 2013;158(1):39–53. doi: 10.1007/s00705-012-1423-7. [DOI] [PubMed] [Google Scholar]
- 12.Vijaykrishna D, et al. Long-term evolution and transmission dynamics of swine influenza A virus. Nature. 2011;473(7348):519–522. doi: 10.1038/nature10004. [DOI] [PubMed] [Google Scholar]
- 13.Smith DJ, et al. Modeling the effects of updating the influenza vaccine on the efficacy of repeated vaccination. Int Congr Ser. 2001;1219:655–660. [Google Scholar]
- 14.Zhang Y, et al. H5N1 hybrid viruses bearing 2009/H1N1 virus genes transmit in guinea pigs by respiratory droplet. Science. 2013;340(6139):1459–1463. doi: 10.1126/science.1229455. [DOI] [PubMed] [Google Scholar]
- 15.Zhang Q, et al. H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science. 2013;341(6144):410–414. doi: 10.1126/science.1240532. [DOI] [PubMed] [Google Scholar]
- 16.Li X, et al. Genetics, receptor binding property, and transmissibility in mammals of naturally isolated H9N2 avian influenza viruses. PLoS Pathog. 2014;10(11):e1004508. doi: 10.1371/journal.ppat.1004508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang Y, et al. Key molecular factors in hemagglutinin and PB2 contribute to efficient transmission of the 2009 H1N1 pandemic influenza virus. J Virol. 2012;86(18):9666–9674. doi: 10.1128/JVI.00958-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Jong JC, et al. Haemagglutination-inhibiting antibody to influenza virus. Dev Biol (Basel) 2003;115:63–73. [PubMed] [Google Scholar]
- 19.Potter CW, Oxford JS. Determinants of immunity to influenza infection in man. Br Med Bull. 1979;35(1):69–75. doi: 10.1093/oxfordjournals.bmb.a071545. [DOI] [PubMed] [Google Scholar]
- 20.Hancock K, et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med. 2009;361(20):1945–1952. doi: 10.1056/NEJMoa0906453. [DOI] [PubMed] [Google Scholar]
- 21.Rowe T, et al. Detection of antibody to avian influenza A (H5N1) virus in human serum by using a combination of serologic assays. J Clin Microbiol. 1999;37(4):937–943. doi: 10.1128/jcm.37.4.937-943.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gao Y, et al. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathog. 2009;5(12):e1000709. doi: 10.1371/journal.ppat.1000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293(5536):1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 24.Li Z, et al. Molecular basis of replication of duck H5N1 influenza viruses in a mammalian mouse model. J Virol. 2005;79(18):12058–12064. doi: 10.1128/JVI.79.18.12058-12064.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Steel J, Lowen AC, Mubareka S, Palese P. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 2009;5(1):e1000252. doi: 10.1371/journal.ppat.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bussey KA, Bousse TL, Desmet EA, Kim B, Takimoto T. PB2 residue 271 plays a key role in enhanced polymerase activity of influenza A viruses in mammalian host cells. J Virol. 2010;84(9):4395–4406. doi: 10.1128/JVI.02642-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fan S, et al. Novel residues in avian influenza virus PB2 protein affect virulence in mammalian hosts. Nat Commun. 2014;5:5021. doi: 10.1038/ncomms6021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gabriel G, et al. The viral polymerase mediates adaptation of an avian influenza virus to a mammalian host. Proc Natl Acad Sci USA. 2005;102(51):18590–18595. doi: 10.1073/pnas.0507415102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mehle A, Doudna JA. Adaptive strategies of the influenza virus polymerase for replication in humans. Proc Natl Acad Sci USA. 2009;106(50):21312–21316. doi: 10.1073/pnas.0911915106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yamada S, et al. Biological and structural characterization of a host-adapting amino acid in influenza virus. PLoS Pathog. 2010;6(8):e1001034. doi: 10.1371/journal.ppat.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chowell G, et al. Severe respiratory disease concurrent with the circulation of H1N1 influenza. N Engl J Med. 2009;361(7):674–679. doi: 10.1056/NEJMoa0904023. [DOI] [PubMed] [Google Scholar]
- 32.Feng L, et al. Seasonal influenza vaccine supply and target vaccinated population in China, 2004-2009. Vaccine. 2010;28(41):6778–6782. doi: 10.1016/j.vaccine.2010.07.064. [DOI] [PubMed] [Google Scholar]
- 33.Herfst S, et al. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336(6088):1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tumpey TM, et al. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315(5812):655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 35.Imai M, et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486(7403):420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen LM, et al. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology. 2012;422(1):105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yen HL, et al. Hemagglutinin-neuraminidase balance confers respiratory-droplet transmissibility of the pandemic H1N1 influenza virus in ferrets. Proc Natl Acad Sci USA. 2011;108(34):14264–14269. doi: 10.1073/pnas.1111000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pascua PN, et al. Virulence and transmissibility of H1N2 influenza virus in ferrets imply the continuing threat of triple-reassortant swine viruses. Proc Natl Acad Sci USA. 2012;109(39):15900–15905. doi: 10.1073/pnas.1205576109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pearce MB, et al. Pathogenesis and transmission of swine origin A(H3N2)v influenza viruses in ferrets. Proc Natl Acad Sci USA. 2012;109(10):3944–3949. doi: 10.1073/pnas.1119945109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Watanabe T, et al. Characterization of H7N9 influenza A viruses isolated from humans. Nature. 2013;501(7468):551–555. doi: 10.1038/nature12392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Trock SC, Burke SA, Cox NJ. Development of framework for assessing influenza virus pandemic risk. Emerg Infect Dis. 2015;21(8):1372–1378. doi: 10.3201/eid2108.141086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ministry of Science and Technology of China (2013) Guide for the Care and Use of Laboratory Animals of the Ministry of Science and Technology of China (Central People's Government of the People's Republic of China, Beijing), 2nd Ed. Available at www.gov.cn/gongbao/content/2011/content_1860757.htm. Accessed December 23, 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.