Abstract
Introduction:
A variety of factors have influenced the significant incidence of morbidity and mortality of acute poisoning and the timely recognition and properly management of critically ill poisoned patients is a key component. The aim of this study is to reveal the reasons for ICU admission of acutely poisoned patients, the main factors influencing the course and outcome of patients in relation with clinical approaches applied, available resources and infrastructure of treatment.
Materials and Methods:
This is a retrospective study based on most reachable variables extracted from patients’ medical records and ED registers of patients admitted at the medical ICU of “Mother Teresa” University Hospital in Tirana over two (2012-2013) years. Demography, time of exposure, etiology and circumstances of poisonings, assessment and treatment, reasons for ICU admission, course and outcome were duly obtained.
Results:
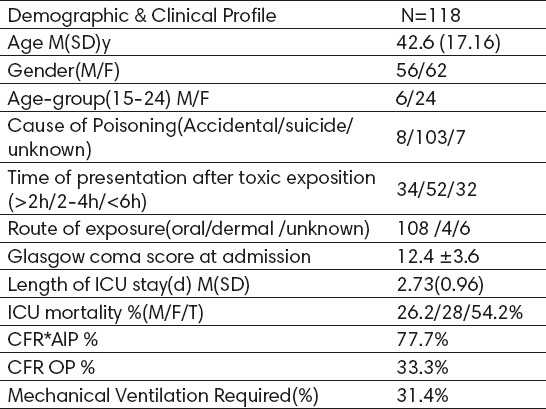
The number of ICU treated patients was 118, consisting in 47.4% (56) males and 52.5% (62) females which represented 10.2% of poisoned patients admitted during this two-year-period in ED and 9.2% of other etiology ICU admitted patients. Mean was 42.6 years for males, and 38 years for females. About 55.9% were urban residents and 44% rural ones. The elapsed time from toxic exposure to treatment initiation had varied between 2-6 hours, 44% arrived in the hospital <4 hours. The toxic exposures were intentional in 87.2% of cases, with a male:female ratio was 0.8:1. Agrochemicals such as Aluminum phosphide and organophosphates were involved in 77.1% of cases. Cardiovascular collapse and respiratory failure were the main clinical syndromes encountered. Mechanical ventilation was required in 31.4% of patients. The length of ICU stay was 2.73 (0.96) days and the mortality was 54.2%.
Conclusion:
This study evidenced that highly lethal toxicants used in poisoning acts such as agrochemicals, high rate of suicide, notwithstanding the infrastructure and resources available employed for ICU patients’ treatment, all had played a role in the very high rate of mortality in this cluster of patients.
Keywords: acute poisoning, intensive care unit, aetiology, severity of poisoning, mortality
1. INTRODUCTION
Acute poisonings represents a complex public health problem in many countries of the world (1-4). Their epidemiology, being accidental or intentional, varies among countries and changes over time (2). Deliberate self-poisoning (DSP) is the most common method of suicide attempt in developed countries, the most common type of deliberate self-harm and the third cause of injury-related fatalities (3). It accounts directly for 1% to 5% of medical admissions to hospital (4) and about 95% of poisonings (5). Pesticides and envenomations constitute a substantial rate of poisoned patients in developing countries as compared to prescription/recreational drugs in the developed world (5)..
Keeping information about acute poisonings updated is essential for the efficient use of resources, however, even in the countries where intoxications are reportable illnesses, this is related with the fragmented nature of case registration and reporting systems (6). While toxicants and their health impacts are countless, the specific, effective measures directed against the particular offending substance can be used to treat only a small minority of patients. Thus, the knowledge of the clinical features of poisoning through a systematic assessment permits early recognition and hospitalization of high-risk and critically ill poisoned patients (7). In this regard, poison information centers are cost-effective, especially among the patients admitted to hospital with less severe poisonings, since they can help with therapeutic decision-making and planning (6). In Albania, regardless the lack of studies and the scarcity of toxicological surveillance mechanisms, poisonings and deaths related to them are common. The aim of this study is to reveal the reasons for ICU admission of acute poisoned patients, the main factors influencing the course and outcome of patients in relation with clinical approaches applied and available resources and infrastructure of treatment.
2. MATERIALS AND METHODS
This is a retrospective descriptive review of intensive care unit patients. The study population consists of 118 patients admitted to ICU between January 1st, 2012 and December 31st, 2013. Patients were identified by using discharge diagnose codes ICD-9 (E 960–989.9) from hospital release registries, ED registers and patients records. According to the release diagnoses we tried to divide the cluster in eight groups. We considered tree variable groups: hosts characteristics (age, sex, residency pre-morbid status) data regarding aetiology and diagnosis, clinical assessment, laboratory investigation, if available, the results of any toxicology investigations or other imagery examinations, treatment data, time since exposure, severity, complications, length of hospital stay (LOS), critical care outcome and circumstances of exposures. Data analysis was carried out by using descriptive and inferential statistical methods: Frequency, percentage, mean and standard deviation (SD). A p-value of less than 0.05 was considered statistically significant. The only exclusions were patients under 14 years old, episodes where the poisoning considered chronic or related to alcohol or drug abuse, as well as patients who arrived dead to the ED.
3. RESULTS
Total amount of 5848 patients were presented at the medical ED, exposed to different toxic substances. 19.7% (1156) of patients were hospitalized, out of whom 10.2% (118) were transferred to the ICU, 83% (98) directly from ED. This number constituted only 9.2% of the total number of patients admitted to ICU with other critical illnesses. From ICU treated patients 47.4% (56) were male and 52.5% (62) female, with male/female ratio (0.9/1). The mean age±(SD) 42.6 (17.16), (14-82), for male patients 47.3 (16.26) and for female patients 38 (18.05). The age group 15-25 years old had the highest incidence with 25.4% of the total number of the patients, where 80% were female (Table 1). According to residency location, 55.9% of patients came from urban zones and 44% from rural ones. About 37.7% (44) of patients were transferred from other hospitals or emergency teams. The rest, about 62.3% (74) of them, reached hospital transferred by family members, police, bystanders or friends. The elapsed time from toxic exposure to treatment initiation had varied from >2 hour to <6 hour, where 44% arrived to hospital in less than 4 hours.
Table 1.
Division of patients according to age group
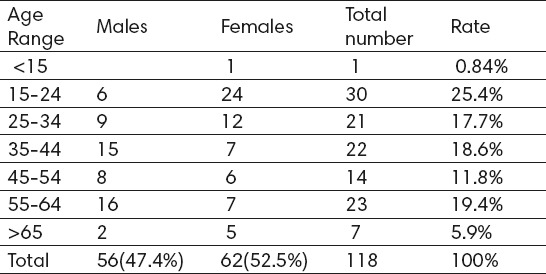
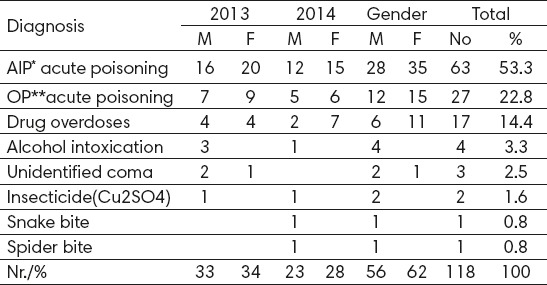
Table 2.
Division according to diagnosis, age and gender
The general management approach adopted at ED arrival was based on physiological abnormalities, resuscitation and risk assessment. Although not consistently evidenced, the system used for severity grading in ED presentation was Poisoning Severity Score (PSS) system introduced by Persson et al (15). Thus, 10.2% (118) of suspected or verified acute poisoned patients were arguably suffering moderate to severe poisoning and 83% of whom almost instantly were transferred to close ICU with severe poisonings. The time frame of patients transfer from ED to ICU had varied from immediately to less than one hour. In most of cases (70.8 %) in poisoning acts only one toxic agent was used, while in cases of pharmaceutical drugs overdoses more than one toxic agent was often used. The main route of exposure in 91.5% of patients was oral ingestion. And most of poisoning acts were committed in household environment.
Diagnosis was mainly based in the history of exposure acquired from the patient and any other involved persons, as well as on the suspected agents, the presumable quantity, time elapsed and other circumstantial evidences. In 39% (46) of cases, mainly in AlP, OP or other cases of acute poisonings, it was required the toxicological laboratory examination of biological samples. Positive laboratory results were confirmed in 23.6% of cases. In 12% of patients there were used bedside analytic tests (mostly substances of abuse), mainly in comatose patients, but their diagnostic value was not straightforward. Data on prior health status of patients were not consistently evidenced on patients’ files. In about 20.3% (24) of patients, there was information on mental health problems, mainly depressive and other affective disorders. According to circumstances and motivation for toxic exposures, there were notes where, in 87.2% of them, the subjects were self-poisoned in attempts for suicide, out of which 49.1% had committed suicide. The male: female ratio was 0.8:1. In 6.7% of cases, the exposure was accidental and in 5.9% of cases there were no confirmed notes (Table 3). There were no cases involving homicide poisoning. In 2013 there were registered 70 (56.7%) patients, whereas in 2014, 48 (43.2%) of the total number of patients. The rate male: female was 0.97:1 in 2013 and 0.82:1 in 2014 and in total 0.9:1 Table 5 presents the main etiological factors related to treatment outcome. Aluminum Phosphide (A1P) with 53.3% followed by agrochemicals with 22.8%, drug overdoses 14.4% were the main etiological causes of poisonings. Regarding the doses of toxic agents used, though not precisely, tablets were swallowed in the cases of AlP where dose varied from 0.5gm to 9gm. This was also reachable in cases of pharmaceutical overdoses. The treatment delivered in ED was mainly symptomatic and supportive, based on vital signs’ stabilization, oxygen, ECG registration, fluid and electrolyte resuscitation, vasopressors and inotrope use. Specific measures such as antidotes (atropine, 100% oxygen, bicarbonate, Magnesium sulfate) were used in 29.5% of cases. The only decontamination technique used was gastric lavage applied in only 6.7% of patients. Since active carbon had not been available in the country’s market it was not neither used as a single dose, nor as a multiple one. The ICU treatment was also supportive and symptomatic. It was based mainly on vasopressors and inotropes, IV liquids, electrolytes, bicarbonate, magnesium, antacids and PPI and cortisones administrations. Close vital signs monitoring, EKG, and bedside imaging examinations, ultrasonography, chest x-ray graph in 13.5%, head CT in 5.9% of cases and 2.5% IMR (head, thorax) were also performed for guiding treatment as well for ruling out other pathologies. Intubation and mechanical ventilation for airway protection, hypoventilation, or hypoxemia were required in 31.4% of patients. Hemodynamic instability, cardiogenic or vascular shock as well as heart rhythm and conduction disturbances were registered in 52.5% of patients, by dominating the clinical scenarios in this group of patients. The EKG registrations revealed rate and rhythm changes in about 28.3% of patients and myocardial fibrillation. Myocardial ischemic changes were present also in 18.6% of patients. Cardiogenic pulmonary edema was mostly registered in acute AlP poisoned patients caused by complex path physiologic mechanisms involving myocardium and vascular system, yet to be fully explained. Electrolytic and acid-basic disturbances associated with acidosis, and electrolyte disbalance were evidenced in 58% of patients cluster. Decreased consciences or coma, on average ± SD(12.4 ±3.6) as a direct effect of toxic agents or as a complication were registered in 51% of patients. Among invasive procedures applied were central veins catheterization and PCV measurements. The only specific antidotes used in ICU were atropine, Magnesium sulphate, and sodium bicarbonate and oxygen. The main ICU complications were tracheal stricture consisting in 1.7%, bacterial pneumonias in 3.3%, and neuropathies with 0.8%. The direct cause of death in 62% of patients, was multi organ failure, with cardiac and vascular shock, accompanied by respiratory and renal failure mainly in AlP poisonings and in organic phosphorus (OP) poisonings. Deep coma with cerebral edema and hydro electrolytic and acid basic disorders, were also evidenced in this case series. Length of ICU stay was 2.73 (0.96), it was longer in OP poisonings with 4.08 (2.56) days and shorter in the AlP poisoning patients with 2.06 (3.01) days (Table 6). The cluster mortality rate was 54.2% with a male: female ratio of 1:1.06. The main poisoning agent was AlP with 53.3% (63) of this cluster of patients and 41.5% of deaths list (group CFR 77.7%). OP pesticides were the second most important toxic agents involved with 22.8% of ICU poisoned patients and 14% of total deaths (group CFR 50%). Drug overdoses with 15.2% and 3.1% of deaths whereas CFR was 6.2%. Alcohol intoxications, unidentified coma and insecticides with snake and spider bite closed the lists of toxicants involved in acute critically ill poisonings. There was a slight difference according to average age and mortality rate among male and female population, which require more in depth analysis.
Table 3.
Source of information on cause poison exposure
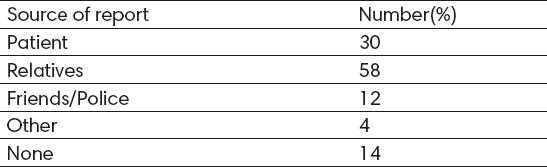
Table 4.
Classification according to intent of exposure
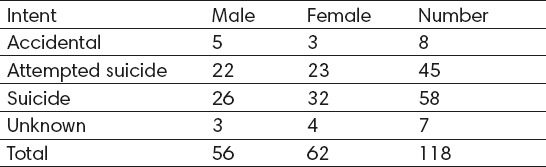
Table 5.
Patients outcome according to suspected diagnosis. *Aluminum Phosphide; **Organophosphates
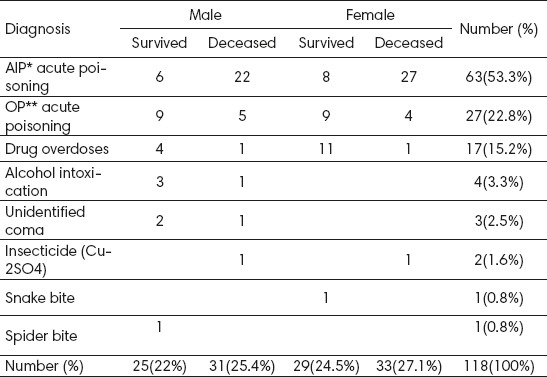
Table 6.
The Core Demographic and Clinical Data *CFR: Case Fatality Ratio
4. DISCUSSION
In this retrospective study we presented a demographic, etiologic and clinical profile of acute poisoning patients treated in ICU, mostly of whom intentionally were exposed with a variety of highly lethal toxicants followed by a striking high mortality rate, presenting so a “suicide cluster”. About 47.4% were male as in previous studies (8, 9). The age group 15-25 years old had the highest incidence with 25.4% of the total number of the patients, where 80% were female. In almost the same proportion was the age distribution in studies of Clark et al (1). In our study, about 55.9% of patients come from urban zones and 44% from rural ones similar with other studies (10). About 60% of study subjects lived in rural areas in the report of Sharma et al (11). According to Daly et a (12) acute poisoning is a dynamic medical illness that represents an acute exacerbation of a chronic underlying psychosocial disorder. In this context, the majority of the subjects enrolled in this study, namely 87.2%, attempted suicide whereas 56.3% of them committed. There were no cases involving homicidal poisoning. The victims of suicide are a heterogenic population regarding suicide methods, psychiatric diagnoses, age, and socio-economic context, which represent a series of possible influences over suicide mortality.. In this report it was difficult however, to evaluate the personal and socio-cultural contributory factors for selfpoisoning acts, so, the reason why the victims of this study chose self-poisoning with different toxicants over other suicide means, requires further analysis. The main route of exposure, with 91.5% of this group of patients was oral poison ingestion, in the meantime in 5% of poisoning cases the information was missing. Regarding the place of poisoning, the information existed for 82% of patients and they occurred at home. Home was the place where 84.9% of accidents occurred following the report of Mucci et al (8). Considering that 62.3% of patients in this study were referred by family members, police or friends mainly implied that post toxic exposures, general and specific measures offered, were inadequate or missing. Even in hospital or ED transferred patients, the level and quality of delivered care, albeit not consistently evidenced, greatly varied from simple measures to advanced cardiac and respiratory life support in few cases. Liisanantti et al (13) reported that most of the deaths from acute drug poisoning occurred outside the hospital environment, and the proportion of patients treated by ambulance services or solely on emergency departments varied, depending on the area, from 20%-80%. Concerning this fact, it was difficult however in this study to get insight on the pre-hospital morbidity and mortality of acute poisoning patients. About 19.7% patients searching help for suspected or verified acute poisonings were admitted to hospital, 10.2% of whom in ICU. Clark et al (1) found that self-poisoning accounts for about 4% of admissions to ICU. Intensive care was required for 3.7-40% of patients hospitalized due to drug poisoning and the highest rates of intensive care are in the Nordic countries, with the highest rate, 40%, in Oslo, Norway (13). The rate of poisoned patients that require ICU treatment varied from 3% to 15.7% (1).
Alapat et al (14), reported that the management of toxicity in critical care requires significant effort by the clinician to recognize and rapidly evaluate patients in order that focused therapies may be instituted. Although in this cluster of patients the basis for the discerning the critically ill poisoned patients was Poisoning Severity Score (PSS), Persson et al (15), the decision taking for ICU transfer was further facilitated by multidisciplinary team consultations (mainly clinical toxicologists, intensivists and other emergency medicine physicians). Based on this approach about 83% of patients since their presentation to ED were considered severely or moderately poisoned and were transferred to ICU in less than one hour. Mégarbane et al (16) reported that poisoning should be considered as severe if life-threatening symptoms occur, the patient has been exposed to a large amount of toxicant requiring a close monitoring and the patient is more vulnerable (co-morbidities, elderly or infants). However the relationship between the level of abnormality in physiological values and the associated increase in risk is generally not linear and scoring systems are designed to describe severity of illness and probability of death in groups of patients, not individual patients. The diagnosis of acute poisoning in this report was based on clinical approach. In 11.8% of patients, the history was not conclusive. In this group of patients, the toxicology laboratory investigations were required in many individual cases, but the clinical utility was minimal owing to scarce quantity probes available, lack of communication and protocols. Urine bedside drug screens in our study were carried in 12% of patients. These screens were necessary in the evaluation of the 10% of patients from whom anamneses could not be obtained and in the patients with suicidal drug use from whom the anamneses were unreliable (12). The release diagnoses, as with risk for bias were based on ICD-9 classification. We made the classification of the etiological agents in eight groups (Table 4), where agrochemicals represented 76.2% of all toxic agents responsible for critically ill poisoned patients such as AlP and OP, that mostly determined the morbidity and mortality of ICU patients. Among the various causes of poisonings, pesticides are the most common cause of self-poisoning worldwide with the proportion ranging from 4% in the European region to over 50% in the Western Pacific region. Our country, as part of the European region, in this report certainly represented an exception. Quite different were the results in reports (17) where in accidental or deliberate poisoning exposures the commonly used agents were psychotropic medical drugs. Benzodiazepine, alcohol, tricyclic antidepressants, and carbon monoxide were the four most common poisons encountered, whereas caustic agents and household products were the prevalent causes of intoxications. Although prompt administration of activated charcoal and improved pre-hospital care may improve outcomes, these important measures lacked in our study. Only after arrival in ED or ICU, the gastric lavage was applied in 6.7% of cases. Use of active carbon or other decontamination techniques, as well as their extracorporeal elimination or neutralization were almost anecdotic. Gastric lavage and activated charcoal was administered to 50.7% patients in the report of Koylu et al (18), and it was carried out in 31.5% of patients whereas hemodialysis and hemoperfusion were performed in 2.1% of the patients (13). The report of Exiara et al (10) reported that antidote were administrated in 32.7% of patients, whereas Müller et al (6) reported that as a consequence of recent improvements in symptom oriented intensive care medicine, the use of certain antidotes that carry the risk of severe complications must be re-evaluated.
Length of ICU stay was longer in OP poisonings with 4.08 (2.56) days and shorter in the AlP poisoning patients with 2.06 (3.01) days (Table 6). This was in an average of 3.5 days; with 85% of the victims passing away during the first twenty-four hours. Intubation and mechanical ventilation for airway protection, hypoventilation, or hypoxemia with different regimes was required in 31.4% of patients, meantime, the rate of mechanical ventilation requirement varied from 4.4%-79.5% of ICU patients (1, 8, 10).
The main poisoning agent were AlP involved in 53.3% of patients and 76.5% of deaths list with a CFR 77.7%. The majority of deaths were caused also by AlP (11). OP pesticides were the second most important agent with 22.8% of ICU poisoned patients and 14% of total deaths and CFR 50%. Both chemical groups in this study, such as AlP and different types of OP agents had caused the majority of morbidity (76.2%) and mortality (90.6%) in this two-year-period. OP pesticide were also responsible for the majority of deaths in most cases, particularly those from rural areas (11). In the study of Avsarogullari et al (8) it was reported that the majority of acute poisoning cases (68%) pharmaceutical drugs were involved, but pesticides with 9.3 % of cases have caused 40% of deaths. The high incidence of mortality encountered in ICU patients is related with inherent lethality of toxic agents involved, but it may also be related to sub-optimal treatment and management. In our study we also found that drug overdoses even in cases where there were used poly- pharmacy caused only 3.1% of death toll and CFR was 6.2%, in the meantime the CFR for AlP was 77.7%.
The hospital mortality rate of patients with acute drug poisonings is reported to be 0.2–5.8%(8,10). About 90.2 % of deaths in this study were caused by self poisoning with agrochemicals such as AlP and OP. These findings were similar with other author’s findings where these toxic agents were mainly responsible for the morbidity and mortality (11, 19). There was a slight female incidence in morbidity and mortality, but its role in treatment outcome along with the place of residence and age of patients require further evaluation if they ever had an impact in treatment’s outcome. However, as other authors have noted, age becomes a predictor of mortality in cases of acute poisoning.
5. CONCLUSIONS
Severe clinical presentations associated with a very high mortality were among others related to the free access for highly lethal toxicants chosen (AlP OP and other agrochemicals). The lack of a consistent poison information and scarce or insufficient use of specific antidotes and necessary resources had played an important role as well. The reduction of these preventable loses in human life requires a proper and further strategy for suicide prevention and more effective management of highly lethal agrochemicals through strict control and better legislation.
Footnotes
CONFLICT OF INTEREST: NONE DECLARED.
REFERENCES
- 1.Clark D, Murray DB, Ray D. Epidemiology and outcomes of patients admitted to critical care after selfpoisoning. 2011;12(4) [Google Scholar]
- 2.Bailey G, Wisniacki F. One Year of Deliberate Self-poisoning Presentations at a West London Emergency Department. The West London Medical Journal. 2014;6(1):33–44. [Google Scholar]
- 3.Cretikos MA, Parr MJA. Drug Related Admissions to Intensive Care: The Role of Illicit Drugs and Self Poisoning Critical Care and Resuscitation. 2003;5:253–257. [PubMed] [Google Scholar]
- 4.Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: Systematic review. BMC Public Health. 2007;7:357. doi: 10.1186/1471-2458-7-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murali R, Bhalla A, Singh D, Singh S. Acute pesticide poisoning:15 years experience of a large North-West Indian hospital. Clin Toxicol (Phila) 2009 Jan;47(1):35–38. doi: 10.1080/15563650701885807. [DOI] [PubMed] [Google Scholar]
- 6.Müller D, Desel H. Common causes of poisoning-etiology, diagnosis, and treatment. Dtsch Arztebl Int. 2013;110(41):690–700. doi: 10.3238/arztebl.2013.0690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma BR, Relhan N, Gupta N, Singn H. Trends of Fatal Poisonings in Northern India.A ten-year Autopsy Analysis. Journal of Pharmacology and toxicology. 2007;2(4):350–358. [Google Scholar]
- 8.Mucci N, Alessi M, Binetti R, Magliocchi MG. Profilo delle intossicazioni acute in Italia. Analisi dei dati registrati dai Centri antiveleni. Ann Ist Super Sanita. 2006;42(3):268–270. [PubMed] [Google Scholar]
- 9.Cook R, Allcock R, Johnston M. Self-poisoning: current trends and practice in a U.K. teaching hospital. ClinMed. 2008;8(1):37–40. doi: 10.7861/clinmedicine.8-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Exiara T, et al. A Prospective Study of Acute Poisonings in a Sample of Greek Patients. Cent Eur J Public Health. 2009;17(3):158–160. doi: 10.21101/cejph.a3522. [DOI] [PubMed] [Google Scholar]
- 11.Sharma A, Pandit V. Importance of Poison Information Center and Role of a Pharmacist in Management of Poisoning. IJPTP. 2014;5(1):905–909. [Google Scholar]
- 12.Daly FFS, Little M, Murray L. A risk assessment based approach to the management of acute poisoning. Emerg Med J. 2006;23:396–399. doi: 10.1136/emj.2005.030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liisanantti J. Acute drug poisoning: outcome and factors affecting outcome. Acta Univ Oul D 1154. 2012 [Google Scholar]
- 14.Alapat PM, Zimmerman JL. Toxicology in the critical care unit. Chest. 2008;133:1006–1013. doi: 10.1378/chest.07-1840. [DOI] [PubMed] [Google Scholar]
- 15.Persson H, Sjöberg G, Haines J, Pronczuk de Garbino J. Poisoning Severity Score: Grading of acute poisoning. J Toxicology–Clinical Toxicology. 1998;36:205–213. doi: 10.3109/15563659809028940. [DOI] [PubMed] [Google Scholar]
- 16.Mégarbane B. Toxidrome-based Approach to Common Poisonings. Asia Pac J Med Toxicol. 2014;3:2–12. [Google Scholar]
- 17.Boyle JS, Bechtel LK, Holstege CP. Management of the critically poisoned patient. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine. 2009;17:29. doi: 10.1186/1757-7241-17-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frithsen IL, Simpson W. Recognition and Management of Acute Medication Poisoning. American Family Physician. 2010;81(3):65. [PubMed] [Google Scholar]
- 19.Koylu R, et al. The Experiences in a Toxicology Unit: A Review of 623 Cases. J Clin Med Res. 2014;6(1):59–65. doi: 10.4021/jocmr1687w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sulaj Z, Drishti A, Çeko I, Gashi A, Vyshka G. Fatal aluminum phosphide poisonings in Tirana (Albania), 2009 - 2013 DARU. Journal of Pharmaceutical Sciences. 2015;23:8. doi: 10.1186/s40199-015-0090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


